Abstract
Background Despite global awareness of the impacts of climate change on human health, assessment of resident physicians’ confidence in environmental health is limited. Lack of confidence in explaining environmental health topics can affect both patient education and advocacy efforts.
Objective To determine how confident resident physicians are in their environmental health training and their ability to explain climate health topics.
Methods An online survey was distributed to internal medicine residents at a large university-affiliated program in 2023. Self-perceived confidence levels in explaining various environmental health topics to a peer were measured using a Likert scale (from 1=not confident at all, to 5=completely confident) and a subsequent rank-order analysis of the response means.
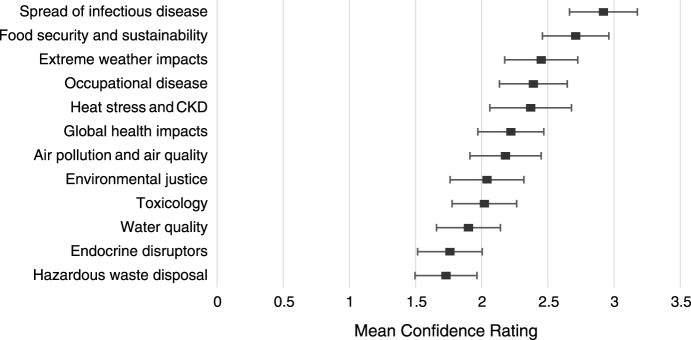
Results The response rate was 56% (62 out of 110 residents). A mean confidence score of 2.22 was reported on all topics, with hazardous waste (m=1.73), endocrine disruptors (m=1.76), water quality (m=1.9), toxicology (m=2.02), and environmental justice (m=2.04) representing lowest scores. Highest mean scores were reported in food security (m=2.71) and emerging infectious disease (m=2.92). Twenty-seven of 62 (44%) residents reported no confidence at all in their ability to discuss environmental justice concepts, with 17 of 62 (27%) reporting slight confidence in doing so.
Conclusions Physician trainees report low confidence levels regarding their ability to explain multiple environmental topics to their peers. Forty-four of 62 (71%) residents report either no or slight confidence in their ability to explain environmental justice to a colleague.
Introduction
The effects of climate change on human health are pronounced, yet their inclusion in graduate medical education (GME) is minimal. Multiple medical societies have released position statements calling for curricular standards for environmental justice.1-4 After medical knowledge is obtained, trainees must build confidence in effectively translating knowledge into actionable recommendations.5 Yet, how internal medicine residents assess their own understanding regarding environmental health is unknown. Trainee confidence in explaining health topics extends to the frequency and quality of patient counseling and advocacy efforts.6 Therefore, residents’ perceived confidence in environmental health topic discussion is an underexplored gap in environmental health education.
Our study aims to bridge this gap by examining self-reported confidence of internal medicine residents in explaining environmental health concepts to a colleague. This understanding will pave the way for curricular development at our institution that aligns with medical societies’ calls for environmental justice education.
Methods
Setting and Participants
Eligible participants included postgraduate year (PGY) 1, 2, and 3 internal medicine residents at a university program in the US South (N=110 residents). This group included categorical (n=84) and preliminary (n=26) residents.
Data Collection
We developed the survey instrument used in this study by first interviewing clinicians and researchers with prominent interest in environmental health (online supplementary data 1). Key themes were delineated using rapid qualitative analysis and refined via expert review and revision (online supplementary data 2). Some topics, such as air pollution and quality, were considered sufficiently related to measure as one concept. Survey questions were created that assessed residents’ baseline confidence in explaining environmental health topics to a peer, drawing upon Bandura’s model of self-efficacy to understand self-perceived readiness to do so.7 A Likert scale was utilized to gauge confidence, with options ranging from “not confident at all” to “completely confident.” The survey questions designed at our institution have no prior validity evidence, but are modeled on prior scales of self-efficacy predicting clinical performance.8
The survey was deployed through Qualtrics (Silver Lake LLC), an online survey platform, via institutional email address 4 times between February and July 2023. The survey instrument collected demographic data and forced responses on self-reported confidence across 12 environmental health topics (online supplementary data 3). On repeat survey distribution every 6 weeks, participants were asked not to complete the survey if they had done so previously.
Outcomes Measured
The primary outcome was residents’ self-perceived confidence in explaining environmental health topics to a peer.
Analysis of Outcomes
The raw data was imported into SPSS statistical software (SPSS Inc). Each content area was stratified by response mean on the Likert scale to rank-order topics from lowest to highest confidence.9 A 2-tailed student’s t test was performed between PGY-1 and PGY-2-3 resident confidence ratings of each topic. A one-way analysis of variance (ANOVA) was performed between the overall means of each content area. An adjustment for multiple comparisons was made using the Bonferroni method.
The current study was deemed exempt by the University of Texas at Austin Institutional Review Board.
Results
The survey response rate was 56% (62 out of 110 residents). Of 84 categorical residents, 55 responded (66% response rate); of these, 14 out of 26 PGY-1 residents responded (54%). Seven out of 26 preliminary PGY-1 residents responded (27%). The overall response rate for PGY-1s was 40% (21 of 52), while the response rate for all upper-level (PGY-2 and PGY-3) residents was 71% (41 of 58). PGY-1 interns comprised 21 of the 62 responses (34% of the sample). The survey did not distinguish between PGY-2 and PGY-3 residents, who comprised 66% (41 of 62) of the sample.
Overall, residents had a lower mean self-reported confidence score in the topics of hazardous waste disposal, endocrine disruptors, water quality, toxicology, and environmental justice (Figure). Residents reported highest confidence in food security and infectious disease topics. There is a significant gap in resident confidence between explaining the 5 lowest-rated topics and 2 highest-rated topics (online supplementary data 4).
Figure.
Graph of Mean Confidence Scores With 95% Confidence Intervals Across All Internal Medicine Residents
Abbreviation: CKD, chronic kidney disease.
PGY-1 residents had a lower mean self-reported confidence score across all topics compared to PGY-2 and PGY-3 residents, with lowest reported confidence in the topics of endocrine disruptors, hazardous waste disposal, heat stress and kidney disease, extreme weather impacts, and air pollution and air quality. The only topics where PGY-1 confidence was significantly higher than their PGY-2 and PGY-3 peers were toxicology and environmental justice (Table).
Table.
Mean Confidence Results Stratified by Postgraduate Year
| Environmental Health Topics | PGY-1 | PGY-2 and PGY-3 | All Residents | 95% Confidence Interval |
|---|---|---|---|---|
| Hazardous waste disposal | 1.45 | 1.87 | 1.73 | 1.50-1.96 |
| Endocrine disruptors | 1.39 | 1.95 | 1.76 | 1.52-2.00 |
| Water quality | 1.97 | 1.86 | 1.90 | 1.66-2.14 |
| Toxicology | 2.30 | 1.88 | 2.02 | 1.78-2.26 |
| Environmental justice | 2.24 | 1.94 | 2.04 | 1.76-2.32 |
| Air pollution and air quality | 1.93 | 2.31 | 2.18 | 1.91-2.45 |
| Global health impacts | 2.06 | 2.30 | 2.22 | 1.97-2.47 |
| Heat stress and kidney disease | 1.47 | 2.83 | 2.37 | 2.06-2.68 |
| Occupational disease | 2.12 | 2.53 | 2.39 | 2.13-2.65 |
| Extreme weather impacts | 1.87 | 2.75 | 2.45 | 2.17-2.73 |
| Food security and sustainability | 2.43 | 2.85 | 2.71 | 2.46-2.96 |
| Spread of infectious disease | 2.28 | 3.25 | 2.92 | 2.66-3.18 |
| Overall mean | 2.01 | 2.32 | 2.22 | 1.96-2.48 |
Abbreviation: PGY, postgraduate year.
Across all core topic areas, one-third (21 of 62) of residents report themselves as “not confident at all” in explaining at least one environmental health topic, with less than 2% (1 of 62) reporting “complete confidence” in any domain (online supplementary data 5). Seventy-one percent (44 of 62) of residents feel “not confident at all” or “slightly confident” in their ability to discuss environmental justice concepts (online supplementary data 6).
Discussion
These results suggest that internal medicine residents at our institution have low confidence in explaining environmental health topics to a peer, which extends to reduced confidence engaging in health policy advocacy10 and may further extend to effective counseling of patients.6 Furthermore, when individuals rate their confidence, they may be indirectly indicating their level of comfort with subject knowledge. While self-reported confidence is not a measure of knowledge, other studies have shown self-reported confidence to be associated with both legislative policy involvement10 and frequency of discussions with patients on environmental exposures.11 Therefore, the measured confidence levels may provide insight into their understanding of these topics and their readiness to communicate this information in multiple settings.
To our knowledge, this study is the first assessment of resident confidence in explaining environmental health topics to a peer. A survey of medical students revealed a similarly low sense of preparedness regarding discussing environmental health with colleagues or patients.12 Resident physicians who are less comfortable discussing health topics with peers are less likely to describe advocacy as a core component of their professional identity.13 To align with medical society calls for environmental justice education, curricula specifically focused on confidence-building can directly impact skill acquisition in community advocacy.14 Additionally, a multiprogram survey suggested that confidence answering environmental patient queries is directly correlated with frequency of patient counseling.11 A national toolkit for pediatric trainees successfully increased both resident confidence and frequency of environment-related patient counseling.15 Studies of practicing clinicians link lack of GME training to lack of confidence in counseling patients on prenatal environmental exposures.16 Increased resident confidence may be associated with improved patient outcomes, highlighting the use of results for targeted curricular intervention.17 PGY-1 residents reporting higher confidence in environmental justice and toxicology may be related to increasing medical school curricula integrating social determinants of health with the environment.12
One limitation of our study was the single site of study and single specialty investigated. Additionally, because the response rate did not reach a representative sample size (margin of error 8.26%), results may not accurately represent all eligible residents. Some respondents may have been more likely to respond due to personal interest. Another limitation was the use of self-perceived confidence rather than perceived or objective knowledge. Survey terminology may have altered results; for example, “environmental inequity” versus “environmental justice” may induce different responses. Some topics, such as food security and sustainability, were presented as double-barreled concepts, so it is unclear if there are significant differences between them. Potential ambiguity surrounding topic label interpretation might have introduced unintended variation in responses.
Future directions include measuring resident confidence and frequency of patient counseling after curricular intervention.
Conclusions
Internal medicine residents self-report low confidence in explaining environmental health concepts to peers, especially within environmental justice.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Trisha Parekh, DO, MSPH, for designing and contributing to the air pollution and air quality curricular content, Kathryn Pelch, PhD, for designing and contributing to the endocrine disruptors and toxicology curricular content, Kristin Mondy, MD, for designing and contributing to the spread of infectious disease curricular content, Parker Hudson, MD, MPH, for his guidance on survey design and curriculum implementation, and Landon Chambers, MSBA, for his statistical analysis support and review.
Editor’s Note
The online supplementary data contains the survey used in the study, further data from the study, and a visual abstract.
Author Notes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
This work was previously presented at the virtual Baylor College of Medicine Health Equity Summer Research Summit, May 2023.
References
- 1.Crowley R, Mathew S, Hilden D;, Health and Public Policy Committee of the American College of Physicians Environmental health: a position paper from the American College of Physicians. Ann Intern Med . 2022;175(11):1591–1593. doi: 10.7326/m22-1864. [DOI] [PubMed] [Google Scholar]
- 2.Ahdoot S, Pacheco SE;, Council on Environmental Health Global climate change and children’s health. Pediatrics . 2015;136(5):e1468-84. doi: 10.1542/peds.2015-3233. [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists Addressing Climate Change: Position Statement. Published 2021. Accessed August 26, 2024. https://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2021/addressing-climate-change.
- 4.Bush T, Jensen WA, Katsumoto TR. U.S. medical organizations and climate change advocacy: a review of public facing websites. BMC Public Health . 2022;22(1):1950. doi: 10.1186/s12889-022-14339-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capone V. Medical Communication Perceived Self-Efficacy (ME-CO) Scale: construction and validation of a new measuring instrument from a socio-cognitive perspective. Eur J Investig Health Psychol Educ . 2022;12(7):765–780. doi: 10.3390/ejihpe12070056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malatskey L, Bar Zeev Y, Tzuk-Onn A, Polak R. Lifestyle medicine course for family medicine residents: preliminary assessment of the impact on knowledge, attitudes, self-efficacy and personal health. Postgrad Med J . 2017;93(1103):549–554. doi: 10.1136/postgradmedj-2016-134726. [DOI] [PubMed] [Google Scholar]
- 7.Artino AR., Jr Academic self-efficacy: from educational theory to instructional practice. Perspect Med Educ . 2012;1(2):76–85. doi: 10.1007/s40037-012-0012-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheraghi F, Hassani P, Yaghmaei F, Alavi-Majed H. Developing a valid and reliable self-efficacy in clinical performance scale. Int Nurs Rev . 2009;56(2):214–221. doi: 10.1111/j.1466-7657.2008.00685.x. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan GM, Artino AR., Jr Analyzing and interpreting data from Likert-type scales. J Grad Med Educ . 2013;5(4):541–542. doi: 10.4300/jgme-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones HE, Manze M, Brakman A, Kwan A, Davies M, Romero D. Physician engagement in reproductive health advocacy: findings from a mixed methods evaluation of a leadership and advocacy program. BMC Med Educ . 2024;24(1):476. doi: 10.1186/s12909-024-05410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanborn M, Grierson L, Upshur R, et al. Family medicine residents’ knowledge of, attitudes toward, and clinical practices related to environmental health: multi-program survey. Can Fam Physician . 2019;65(6):e269–e277. [PMC free article] [PubMed] [Google Scholar]
- 12.Kligler B, Pinto Zipp G, Rocchetti C, Secic M, Ihde ES. The impact of integrating environmental health into medical school curricula: a survey-based study. BMC Med Educ . 2021;21(1):40. doi: 10.1186/s12909-020-02458-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vance M, Bui E, Shtasel D, Borba C. Health advocacy among resident physicians. MedEdPublish . 2019;8(1) doi: 10.15694/mep.2019.000029.1. [DOI] [Google Scholar]
- 14.Del Rosso CR, Grow M, McGeehan M. Efficacy of pediatric residency advocacy curriculum in improving skills and intent. Pediatrics . 2021;147(3_meetingabstract):42–42. doi: 10.1542/peds.147.3MA1.42. [DOI] [Google Scholar]
- 15.Goldman RH, Zajac L, Geller RJ, Miller MD. Developing and implementing core competencies in children’s environmental health for students, trainees and healthcare providers: a narrative review. BMC Med Educ . 2021;21(1):503. doi: 10.1186/s12909-021-02921-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stotland NE, Sutton P, Trowbridge J, et al. Counseling patients on preventing prenatal environmental exposures—a mixed-methods study of obstetricians. PLoS One . 2014;9(6):e98771. doi: 10.1371/journal.pone.0098771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Douthit NT, McBride CM, Townsley EC. Increasing internal medicine resident confidence in leading inpatient cardiopulmonary resuscitations and improving patient outcomes. J Med Educ Curric Dev . 2020;7:2382120520923716. doi: 10.1177/2382120520923716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.