In a recent national survey, the prevalence of psychiatric disorder in children and adolescents in Great Britain was more than 9%.1 Parents and doctors commonly think that these disorders are transient, but longitudinal studies show otherwise.2 We followed up children from the national survey to examine persistence in a large sample of children in Britain.1
Participants, method, and results
The original survey studied a sample of 10 438 British children aged 5-15 years.1 We sent the parents of all children with a psychiatric disorder (936) and a third of those without a psychiatric disorder (3029) a questionnaire. It included the strengths and difficulties questionnaire, a well validated measure of childhood psychopathology and its impact on the child.3,4
A total of 73% of parents responded; most losses were non-contacts, not refusals. The response rate was lower among those with a child with a disorder than those without (66% v 76%). Non-responders at follow up had had significantly more symptoms initially (analysis of variance adjusting for initial diagnosis, F=39.9, 1 df, P<0.001: the mean symptom score for non-responders was greater, by 1.2, than for responders, matched by diagnosis). Responders' and non-responders' initial impact scores did not differ significantly. Overall, differential non-response will not have led us to overestimate the persistence of psychopathology.
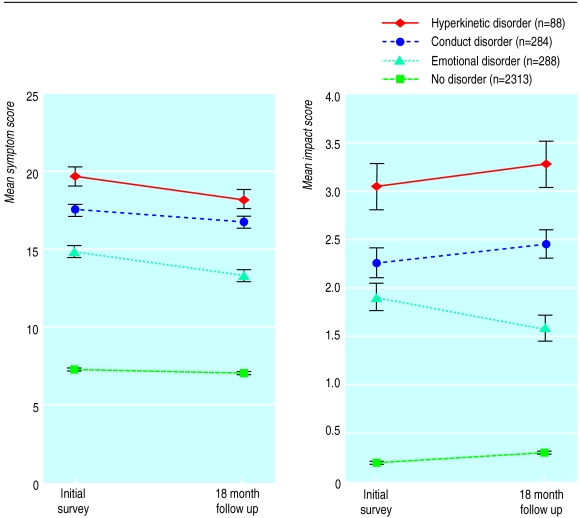
The figure shows symptom and impact scores in children initially diagnosed with hyperkinetic, conduct, emotional, or no disorder. We used paired t tests to test whether the changes in symptom and impact scores in children with hyperkinetic, conduct, emotional, or no disorder were significant. For conduct disorder, neither symptoms nor impact changed significantly. Symptoms (P<0.05) but not impact fell significantly in children with hyperkinesis. For emotional disorder, there were significant falls in both symptoms and impact (P<0.001 for both), though the follow up scores were still substantially greater than in the group with no initial disorder (P<0.001, independent samples t test).
We defined “caseness” from the combination of raised symptom (⩾14) and impact scores (⩾2).3 Caseness at follow up was considered informative for only the 86% (2487/2901) of participants in whom caseness was congruent with the initial psychiatric diagnosis. For example, when a child was initially diagnosed as having conduct disorder solely on the basis of symptoms reported by a teacher, and when the initial questionnaire, completed by the parents, described their child as normal, then the diagnosis (disorder present) and the caseness (negative) were not congruent. So, caseness was not considered informative at follow up, since the parent's answers to the questionnaire would probably not change whether or not the conduct disorder persisted or was resolved. Similarly, if the initial diagnosis of depression in a teenager was based on self reported symptoms (not reported by a parent), the follow up parent questionnaire is unlikely to be informative.
Caseness criteria at the 18 month follow up were met by 3% (67/2249) of children who did not initially have a psychiatric disorder, compared with 62% (147/238) of children who did (relative risk 20.7; 95% confidence interval 16.0 to 26.7). Persistence at 18 months varied with initial diagnosis: 36% (25/70) for children who had an emotional disorder initially, compared with 73% (122/168) for children with other disorders initially (mostly conduct and hyperkinetic disorders, sometimes with coexistent emotional disorders) (P<0.001, χ2 test).
Comment
Childhood psychopathology is often persistent, particularly among children with conduct disorder and hyperkinesis. Although emotional disorders have a better prognosis than conduct or hyperkinetic disorders, they are not always benign: their resolution over 18 months is far from complete, and recent work suggests an increased risk of similar disorders recurring in adulthood.2
Everyone in contact with children should take the symptoms of emotional distress, behavioural difficulty, and hyperactivity seriously, as they may impair the child's function and development and are unlikely to be transient. This is particularly important as evidence based interventions can alleviate distress and minimise the secondary handicap that results from disrupted education and impaired social development.5
Figure.
Mean symptom and impact scores initially and at 18 month follow up from the strengths and difficulties questionnaire, completed by parents, for children with and without initial psychiatric disorder
Footnotes
Funding. TF is funded by a Wellcome clinical training fellowship and the original surveys were funded by the Department of Health.
Competing interests: None declared.
References
- 1.Meltzer H, Gatward R, Goodman R, Ford T. Mental health of children and adolescents in Great Britain. Stationery Office: London; 2000. [DOI] [PubMed] [Google Scholar]
- 2.Harrington R. Developmental continuities and discontinuities. Br J Psychiatry. 2001;179:189–190. [Google Scholar]
- 3.Goodman R. The extended version of the strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–801. [PubMed] [Google Scholar]
- 4.Goodman R. Psychometric properties of the strengths and difficulties questionnaire (SDQ) J Am Acad Child Adolesc Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Graham P. Treatment interventions and findings from research: bridging the chasm in child psychiatry. Br J Psychiatry. 2000;176:414–419. doi: 10.1192/bjp.176.5.414. [DOI] [PubMed] [Google Scholar]