Hospitalisation of older adults with a chronic conditions is associated with higher risk of nosocomial infections, delirium, falls, functional decline and even early mortality (Richardson 2006; Sharek et al. 2011; Shepperd et al. 2017; Sprivulis et al. 2006; Vasilevskis et al. 2012). Hospital‐at‐Home (HaH) interventions provide acute care treatments of a predetermined duration in the patient's home as an alternative to traditional hospital care. These interventions could shorten a hospital stay by enabling an early discharge or even becoming a complete substitution for hospital care. This would allow for continuity of acute care at home over a proscribed period of time (Gonçalves‐Bradley et al. 2017; Shepperd et al. 2016; Shepperd and Iliffe 1998). HaH interventions were developed to minimise, or even avoid, the potential iatrogenic effects of hospitalisation, improve patient and caregiver satisfaction, and reduce healthcare costs (Leong, Lim, and Lai 2021). There is growing evidence from systematic reviews demonstrating the effectiveness of HaH interventions on patient outcomes with lower mortality, reduced readmissions and lengths of stay, lower risk of long‐term care admission, lower depression and anxiety reduced costs, and improved patient satisfaction (Arsenault‐Lapierre et al. 2021; Caplan et al. 2012; Conley et al. 2016; Leong, Lim, and Lai 2021). Patients with chronic diseases who presented to emergency departments and then received HaH interventions had lower risks of readmission and long‐term admission. They also showed lower rates of depression and anxiety than patients who had received inpatient care (Arsenault‐Lapierre et al. 2021). Moreover, a meta‐analysis and a scoping review showed that patients and caregivers had positive perceptions and experiences with HaH services (Chua et al. 2022; Wang, Stewart, and Lee 2024).
Older people with chronic conditions are prone to multiple specialist follow‐ups, thereby generating significant care fragmentation (Le Couteur, Flicker, and Hilmer 2022; Sadler et al. 2023). Care fragmentation leads to adverse health outcomes and undermines patient's care experiences (Duan‐Porter et al. 2020), and contributes also to risks of medication errors (Daunt, Curtin, and O'Mahony 2023; Squires et al. 2020). Deficiencies in prioritising patient‐centred care and in the multidisciplinary continuity of care have, nevertheless, been identified (Wang, Stewart, and Lee 2024). In fact, the complex needs of an older people with multiple chronic conditions cannot be adequately addressed by a single healthcare professional; they require coordination and multidisciplinary collaboration (Araujo de Carvalho et al. 2017; Larsen, Broberger, and Petersson 2017). Thus, the World Health Organization recommends implementing integrated care models that ensure the continuity of care for older people with chronic conditions and minimise the fragmentation of care (World Health Organization 2017). Care coordination supported by nurses in an integrated healthcare model is effective for older people (Prajankett and Markaki 2021). Nurse‐led intervention models demonstrated improved patient outcomes in terms of care coordination (Gabbard et al. 2021; McParland, Johnston, and Cooper 2022), primary and secondary prevention and management of chronic diseases (Beks et al. 2023), hospital admissions (Imhof et al. 2012), emergency room visits (Counsell et al. 2007), mortality (Dorr et al. 2008), physical functioning, nutritional status and quality of life (Kasa et al. 2023).
Although recent decades have seen considerable scientific research on providing HaH interventions for older people with chronic conditions, there has been comparatively little investigation of those interventions specifically led by nurses. A literature and bibliometric search examining published articles in Medline Ovid SP up to February 21, 2024, using the search string in Appendix, comparing published studies involving HaH interventions in general and nurse‐led interventions in HaH for older adults with chronic conditions showed a lack of published research on the impact of nurse‐led interventions models in HaH (Figure 1).
FIGURE 1.
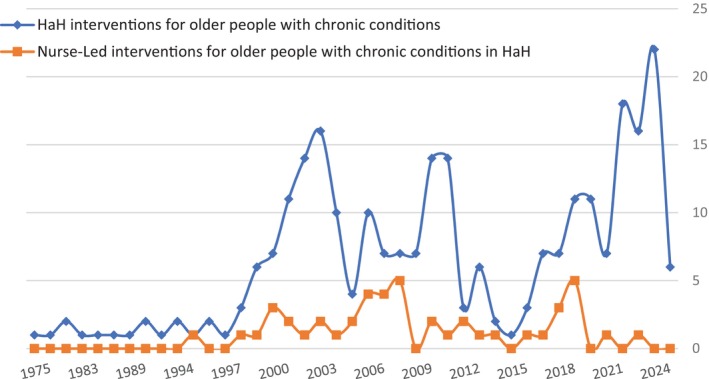
Medline database publications (since inception) examining HaH interventions and nurse‐led HaH interventions for older people with chronic conditions. Medline equations.
It is important that future nursing research should focus on highlighting the role and impact of nurse‐led interventions in HaH on the outcomes of older people and caregivers but also on health systems. Moreover, the effectiveness of nurse‐led models in this domain requires rigorous evaluation through retrospective, prospective and interventional studies. This will enhance our understanding and increase our knowledge of HaH care options that can be proposed to older people with chronic conditions. It will also give policymakers and healthcare institutions arguments for expanding efficient, home‐based, person‐centred care for this population.
Author Contributions
R.A. contributed to the design, data analysis and writing the article. P.D., H.V. and P.L. supervised, corrected and contributed to the editing of this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgements
The authors express their gratitude to Cécile Jaques, medical librarian, for her help in our literature search.
Medline Search String
1—HaH interventions for older people with chronic conditions:
(“Home Care Services, Hospital‐Based”/OR ((“hospital based” ADJ4 home) OR “hospital at home” OR “home hospital*”).ab,ti,kf.) AND (exp Aged/ OR exp. Geriatrics/ OR Geriatric Nursing/ OR multiple chronic conditions/ OR exp. comorbidity/ OR (elder* OR senior* OR geriatr* OR ((aged OR old*) ADJ2 (adult* OR patient* OR person* OR people)) OR multimorbidity or “multi‐morbidity” or “multi morbidity” or multimorbidities or “multi‐morbidities” or “multi morbidities” or multimorbid or “multi‐morbid” or “multi morbid” or comorbidity or “co‐morbidity” or “co morbidity” or comorbidities or “co‐morbidities” or “co morbidities” or comorbid or “co‐morbid” or “co morbid” or “multiple chronic conditions” or “multiple chronic illnesses” or “multiple chronic diseases” or “multiple conditions” or “multiple illnesses” or “multiple diseases” or “multiple diagnoses” or “morbidity pattern” or “morbidity patterns” or polymorbidity or “poly‐morbidity” or “poly morbidity” or polymorbidities or “poly‐morbidities” or “poly morbidities” or polypathology or “poly‐pathology” or “poly pathology” or polypathologies or “poly‐pathologies” or “poly pathologies” or pluripathology or “pluri‐pathology” or “pluri pathology” or multipathology or “multi‐pathology” or “multi pathology” or multipathologies or “multi‐pathologies” or “multi pathologies” or “multiple pathologies” or “disease cluster” or “disease clusters”).ab,ti,kf.).
2—Nurse‐led HaH interventions for older people with chronic conditions:
(“Home Care Services, Hospital‐Based”/OR ((“hospital based” ADJ4 home) OR “hospital at home” OR “home hospital*”).ab,ti,kf.) AND (exp Aged/ OR exp. Geriatrics/ OR Geriatric Nursing/ OR multiple chronic conditions/ OR exp. comorbidity/ OR (elder* OR senior* OR geriatr* OR ((aged OR old*) ADJ2 (adult* OR patient* OR person* OR people)) OR multimorbidity or “multi‐morbidity” or “multi morbidity” or multimorbidities or “multi‐morbidities” or “multi morbidities” or multimorbid or “multi‐morbid” or “multi morbid” or comorbidity or “co‐morbidity” or “co morbidity” or comorbidities or “co‐morbidities” or “co morbidities” or comorbid or “co‐morbid” or “co morbid” or “multiple chronic conditions” or “multiple chronic illnesses” or “multiple chronic diseases” or “multiple conditions” or “multiple illnesses” or “multiple diseases” or “multiple diagnoses” or “morbidity pattern” or “morbidity patterns” or polymorbidity or “poly‐morbidity” or “poly morbidity” or polymorbidities or “poly‐morbidities” or “poly morbidities” or polypathology or “poly‐pathology” or “poly pathology” or polypathologies or “poly‐pathologies” or “poly pathologies” or pluripathology or “pluri‐pathology” or “pluri pathology” or multipathology or “multi‐pathology” or “multi pathology” or multipathologies or “multi‐pathologies” or “multi pathologies” or “multiple pathologies” or “disease cluster” or “disease clusters”).ab,ti,kf.) AND (Primary Nursing/ OR Practice Patterns, Nurses'/ OR exp. Nurse Practitioners/ OR nurse specialists/ or nurse clinicians/ OR Advanced Practice Nursing/ OR exp. Nurses/ OR exp. Nursing/ OR exp. Nurse's Role/ OR exp. Nursing Care/ OR exp. Case Management/ or exp. Case Managers/ OR (apn OR apns OR acnp OR acnps OR cnss OR “specialized nurse*” OR “advanced practice nurs*” OR “advanced practitioner nurs*” OR “advanced practice registered nurs*” OR “advanced practice rn” OR “advanced practice rns” OR “advanced practitioner rn” OR “advanced practitioner rns” OR “advanced practice gerontological nurs*” OR “advanced nurs*” OR “nurse practitioner*” OR “nursing practitioner*” OR “practitioner nurse*” OR “nurse clinical practitioner*” OR “nurse specialist*” OR “nursing specialist practitioner*” OR “specialist practitioner district nurs*” OR “specialist practitioner nurs*” OR “advanced nursing” OR “consultant nurse*” OR “nurse consultant*” OR ((comanage* OR “co manage*”) ADJ3 (physician OR gp OR nurse OR nurses)) OR “primary nurse*” OR nurse‐led OR nurse‐delivered OR nurse‐coordinated OR nurse‐managed OR nurse‐driven or “nurse based intervention” or “nurse‐based intervention” or “primary nursing” or “nurse practitioner” or “nurse practitioners” or “practitioner nurse” or “practitioner nurses” or “advanced practice nurse” or “advanced practice nursing” or “advanced practice nurses” or “nurse specialist” or “nurse specialists” or “specialist nurse” or “specialist nurses” or “specialist nursing” or “nurse clinician” or “nurse clinicians” or “nurse consultant” or “nurse consultants” or “consultant nurse” or “consultant nurses” or ((“case manager” or “case‐manager” or “case management” or “case‐management”) and (nurse or nurses or nursing))).ab,ti,kf.).
Funding: The authors received no specific funding for this work.
Data Availability Statement
All data are available upon request to the authors.
References
- Araujo de Carvalho, I. , Epping‐Jordan J., Pot A. M., et al. 2017. “Organizing Integrated Health‐Care Services to Meet Older People's Needs.” Bulletin of the World Health Organization 95, no. 11: 756–763. 10.2471/BLT.16.187617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsenault‐Lapierre, G. , Henein M., Gaid D., Le Berre M., Gore G., and Vedel I.. 2021. “Hospital‐At‐Home Interventions vs in‐Hospital Stay for Patients With Chronic Disease Who Present to the Emergency Department.” JAMA Network Open 4, no. 6: e2111568. 10.1001/jamanetworkopen.2021.11568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beks, H. , Clayden S., Shee A. W., Binder M. J., O'Keeffe S., and Versace V. L.. 2023. “Evaluated Nurse‐Led Models of Care Implemented in Regional, Rural, and Remote Australia: A Scoping Review.” Collegian 30, no. 6: 769–778. 10.1016/j.colegn.2023.05.004. [DOI] [Google Scholar]
- Caplan, G. A. , Sulaiman N. S., Mangin D. A., Aimonino Ricauda N., Wilson A. D., and Barclay L.. 2012. “A Meta‐Analysis of “Hospital in the Home”.” Medical Journal of Australia 197, no. 9: 512–519. 10.5694/mja12.10480. [DOI] [PubMed] [Google Scholar]
- Chua, C. M. S. , Ko S. Q., Lai Y. F., Lim Y. W., and Shorey S.. 2022. “Perceptions of Hospital‐At‐Home Among Stakeholders: A Meta‐Synthesis.” Journal of General Internal Medicine 37, no. 3: 637–650. 10.1007/s11606-021-07065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley, J. , O'Brien C. W., Leff B. A., Bolen S., and Zulman D.. 2016. “Alternative Strategies to Inpatient Hospitalization for Acute Medical Conditions: A Systematic Review.” JAMA Internal Medicine 176, no. 11: 1693–1702. 10.1001/jamainternmed.2016.5974. [DOI] [PubMed] [Google Scholar]
- Counsell, S. R. , Callahan C. M., Clark D. O., et al. 2007. “Geriatric Care Management for Low‐Income Seniors—A Randomized Controlled Trial.” JAMA 298, no. 22: 2623–2633. 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- Daunt, R. , Curtin D., and O'Mahony D.. 2023. “Polypharmacy Stewardship: A Novel Approach to Tackle a Major Public Health Crisis.” Lancet Healthy Longevity 4, no. 5: e228–e235. 10.1016/S2666-7568(23)00036-3. [DOI] [PubMed] [Google Scholar]
- Dorr, D. A. , Wilcox A. B., Brunker C. P., Burdon R. E., and Donnelly S. M.. 2008. “The Effect of Technology‐Supported, Multidisease Care Management on the Mortality and Hospitalization of Seniors.” Journal of the American Geriatrics Society 56, no. 12: 2195–2202. 10.1111/j.1532-5415.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- Duan‐Porter, W. , Ullman K., Majeski B., Miake‐Lye I., Diem S., and Wilt T. J.. 2020. Care Coordination Models and Tools: A Systematic Review and Key Informant Interviews. Washington DC: Department of Veterans Affairs (US). http://www.ncbi.nlm.nih.gov/books/NBK566155/. [PubMed] [Google Scholar]
- Gabbard, J. , Pajewski N. M., Callahan K. E., et al. 2021. “Effectiveness of a Nurse‐Led Multidisciplinary Intervention vs Usual Care on Advance Care Planning for Vulnerable Older Adults in an Accountable Care Organization.” JAMA Internal Medicine 181, no. 3: 1–9. 10.1001/jamainternmed.2020.5950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves‐Bradley, D. C. , Iliffe S., Doll H. A., et al. 2017. “Early Discharge Hospital at Home.” Cochrane Database of Systematic Reviews 2017, no. 6: CD000356. 10.1002/14651858.CD000356.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imhof, L. , Naef R., Wallhagen M. I., Schwarz J., and Mahrer‐Imhof R.. 2012. “Effects of an Advanced Practice Nurse in‐Home Health Consultation Program for Community‐Dwelling Persons Aged 80 and Older.” Journal of the American Geriatrics Society 60, no. 12: 2223–2231. 10.1111/jgs.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasa, A. S. , Drury P., Traynor V., Lee S.‐C., and Chang H.‐C.. 2023. “The Effectiveness of Nurse‐Led Interventions to Manage Frailty in Community‐Dwelling Older People: A Systematic Review.” Systematic Reviews 12: 182. 10.1186/s13643-023-02335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen, A. , Broberger E., and Petersson P.. 2017. “Complex Caring Needs Without Simple Solutions: The Experience of Interprofessional Collaboration Among Staff Caring for Older Persons With Multimorbidity at Home Care Settings.” Scandinavian Journal of Caring Sciences 31, no. 2: 342–350. 10.1111/scs.12352. [DOI] [PubMed] [Google Scholar]
- Le Couteur, D. G. , Flicker L., and Hilmer S. N.. 2022. “Geriatric Medicine and Health Care for Older People in Australia.” Age and Ageing 51, no. 3: afac001. 10.1093/ageing/afac001. [DOI] [PubMed] [Google Scholar]
- Leong, M. Q. , Lim C. W., and Lai Y. F.. 2021. “Comparison of Hospital‐At‐Home Models: A Systematic Review of Reviews.” BMJ Open 11, no. 1: e043285. 10.1136/bmjopen-2020-043285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McParland, C. , Johnston B., and Cooper M.. 2022. “A Mixed‐Methods Systematic Review of Nurse‐Led Interventions for People With Multimorbidity.” Journal of Advanced Nursing 78, no. 12: 3930–3951. 10.1111/jan.15427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prajankett, O. , and Markaki A.. 2021. “Integrated Older People Care and Advanced Practice Nursing: An Evidence‐Based Review.” International Nursing Review 68, no. 1: 67–77. 10.1111/inr.12606. [DOI] [PubMed] [Google Scholar]
- Richardson, D. B. 2006. “Increase in Patient Mortality at 10 Days Associated With Emergency Department Overcrowding.” Medical Journal of Australia 184, no. 5: 213–216. 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- Sadler, E. , Khadjesari Z., Ziemann A., et al. 2023. “Case Management for Integrated Care of Older People With Frailty in Community Settings.” Cochrane Database of Systematic Reviews 2023, no. 5: CD013088. 10.1002/14651858.CD013088.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharek, P. J. , Parry G., Goldmann D., et al. 2011. “Performance Characteristics of a Methodology to Quantify Adverse Events Over Time in Hospitalized Patients.” Health Services Research 46, no. 2: 654–678. 10.1111/j.1475-6773.2010.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd, S. , Cradduck‐Bamford A., Butler C., et al. 2017. “A Multi‐Centre Randomised Trial to Compare the Effectiveness of Geriatrician‐Led Admission Avoidance Hospital at Home Versus Inpatient Admission.” Trials 18, no. 1: 491. 10.1186/s13063-017-2214-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd, S. , and Iliffe S.. 1998. “The Effectiveness of Hospital at Home Compared With In‐Patient Hospital Care: A Systematic Review.” Journal of Public Health 20, no. 3: 344–350. 10.1093/oxfordjournals.pubmed.a024778. [DOI] [PubMed] [Google Scholar]
- Shepperd, S. , Iliffe S., Doll H. A., et al. 2016. “Admission Avoidance Hospital at Home.” Cochrane Database of Systematic Reviews 9: CD007491. 10.1002/14651858.CD007491.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprivulis, P. C. , Da Silva J.‐A., Jacobs I. G., Frazer A. R. L., and Jelinek G. A.. 2006. “The Association Between Hospital Overcrowding and Mortality Among Patients Admitted via Western Australian Emergency Departments.” Medical Journal of Australia 184, no. 12: 616. 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- Squires, A. , Ridge L., Miner S., McDonald M. V., Greenberg S. A., and Cortes T.. 2020. “Provider Perspectives of Medication Complexity in Home Health Care: A Qualitative Secondary Data Analysis.” Medical Care Research and Review 77, no. 6: 609–619. 10.1177/1077558719828942. [DOI] [PubMed] [Google Scholar]
- Vasilevskis, E. E. , Han J. H., Hughes C. G., and Ely E. W.. 2012. “Epidemiology and Risk Factors for Delirium Across Hospital Settings.” Best Practice & Research. Clinical Anaesthesiology 26, no. 3: 277–287. 10.1016/j.bpa.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X. , Stewart C., and Lee G.. 2024. “Patients' and Caregivers' Perceptions of the Quality of Hospital‐At‐Home Service: A Scoping Review.” Journal of Clinical Nursing 33: 817–838. 10.1111/jocn.16906. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2017. Integrated Care for Older People: Guidelines on Community‐Level Interventions to Manage Declines in Intrinsic Capacity. Geneva, Switzerland: World Health Organization. https://apps.who.int/iris/handle/10665/258981. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available upon request to the authors.


