Abstract
Objective: To investigate the preventive effect of upper limb functional exercise on venous thrombosis in patients undergoing peripherally inserted central catheter (PICC) placement. Methods: A retrospective analysis was conducted on 108 patients who underwent PICC placement in Suzhou High tech Zone People’s Hospital. The patients were divided into a control group (n=52) and an observation group (n=56) according to different treatment methods. The control group received upper limb functional exercise on the basis of routine treatment, while the observation group received rehabilitation exercises using an intelligent grip ball alongside the treatment administered to the control group. The incidence of catheter-related thrombosis, coagulation indicators, upper limb venous hemodynamic indicators, and compliance with functional exercise were compared between the two groups. Results: The incidence of catheter-related thrombosis was lower in the observation group compared with that in the control group (P=0.012). After treatment, improvements were observed in the coagulation indicators and upper limb venous hemodynamic indicators in both groups compared with pre-treatment levels. Moreover, post-treatment levels of these indicators were better in the observation group than in the control group (all P<0.05). The scores of the compliance questionnaire for functional exercise were higher in the observation group than those in the control group in various dimensions (all P<0.05). Lastly, patient satisfaction in the observation group was higher than that in the control group (P=0.032). Conclusion: Upper limb functional exercise combined with an intelligent grip ball can reduce the incidence of catheter-related thrombosis, improve coagulation function, increase compliance with functional exercise, and improve nursing satisfaction in patients with PICCs.
Keywords: Central venous catheter, venous thrombosis, upper limb functional exercise, intelligent grip ball, clinical efficacy
Introduction
There is currently a rising trend in the incidence rate of cancer, despite the fact that early screening and surgery can prolong the survival period of such patients. To enhance treatment outcomes, various clinical treatment methods are employed for tumors, including chemotherapy, immunotherapy, targeted therapy, and traditional Chinese medicine treatment [1,2]. Given that these treatments require intravenous infusion, peripherally inserted central catheters (PICCs) are currently the predominant option for infusion access over peripheral veins. PICCs offer several advantages over peripheral veins, including extended indwelling time, avoidance of repeated punctures, and the reduction of potential harm from prolonged infusion times and drug administration. Therefore, PICCs have become the first-line method for infusion [3,4].
Recent clinical data, however, indicated that PICCs were associated with certain complications, with catheter-related thrombosis being a prevalent and serious complication, occurring at a rate of approximately 4%. In cancer patients, the incidence rate of catheter-related thrombosis can be as high as 25% due to their hypercoagulable state. Therefore, effectively reducing catheter-related thrombosis is of great significance [5,6]. Upper limb functional exercise has been identified as an effective preventive measure with favorable clinical outcomes. However, it cannot effectively reduce the incidence of related complications. Infusion Nursing Society (INS) highlights the potential of functional exercise in preventing thrombosis in patients with PICC placement. Additionally, a study has revealed that hand grip exercises can promote venous blood circulation and reduce catheter-related complications [6]. However, routine clinical ball-holding exercise lacks diversity and presents a challenge in controlling grip strength. Moreover, the compliance of patients with PICC placement is generally poor. These factors limit the effect of functional exercise. Nevertheless, the gradual application of intelligent exercise management software holds significant promise in improving the compliance of patients with PICC placement and promoting regular exercise. In addition, intelligent grip balls have been found to significantly improve upper limb blood flow and reduce thrombus formation. However, there is limited research on preventing catheter-related thrombosis [7]. Based on this gap, this study aims to explore the effects of intelligent grip balls on blood flow and coagulation function, thereby comprehensively evaluating their preventive effects on catheter-related thrombosis.
Materials and methods
General data
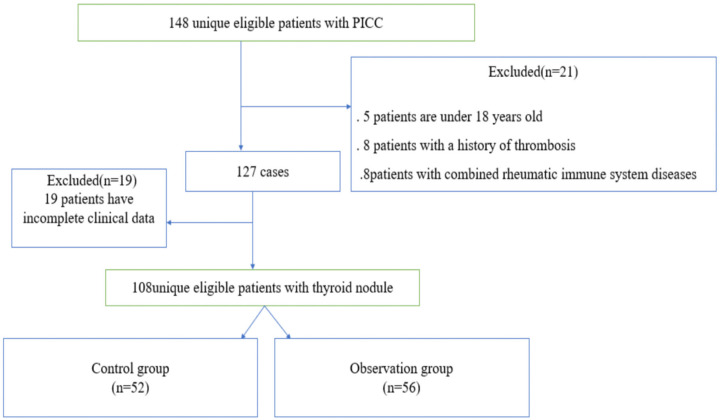
A retrospective analysis was conducted on 108 patients who underwent PICC placement in Suzhou High tech Zone People’s Hospital from January 2022 to December 2023. The patients were divided into a control group (n=52) and an observation group (n=56) according to different treatment methods. The patient selection process is shown in Figure 1. Patients were included if they: 1. were aged over 18; 2. underwent their first-time PICC insertion; 3. had complete medical records; 4. received the same style of a three-way valve; 5. experienced only one puncture. Patients were excluded if they: 1. were aged less than 18 years; 2. had a history of previous thrombosis; 3. were taking anticoagulants; 4. suffered from rheumatic immune system disorders; 5. were unable to move their upper limb due to any reasons; 6. had a history of neurological disorders or cognitive impairment; 7. had an expected survival period less than six months. This study was approved by the Ethics Committee of Suzhou High tech Zone People’s Hospital.
Figure 1.
Patient selection process.
Nursing methods
Nursing methods in the control group
Patients in the control group were provided with routine health guidance before discharge, including psychological counseling, PICC maintenance, daily life guidance during PICC placement, strategies for preventing PICC-related complications, skin care at the puncture site, dietary recommendations, exercise instructions, and appointment guidance. Patients and their families were educated on disease-related information and had their questions answered in detail. Patients also received upper limb exercises, including functional exercises. On days 1-3 after PICC placement, the patient used an electronic grip device (Xiangshan Hengqi EH101) for extension and flexion of the fingers and elbow with their affected limb positioned on the bed. On days 4-10, the patient’s affected limb was allowed to rest naturally or hang down, and arm swing exercises were performed from the shoulder (30° anteriorly, 10° posteriorly), guiding the affected limb in extension movements. The upper limb was extended to both sides, contracted, and extended again, gradually extending to the horizontal position. On days 11-20, patients engaged in assisted shoulder joint rotation exercises and were permitted to perform mild shoulder elevation exercises. During this period, they were prohibited from rapidly lifting, abducting, or vigorously shaking the affected limb, as well as sudden turning, excessive bending, high jumping, falling from heights, or bumping.
Nursing methods in the observation group
Patients in the observation group underwent grip ball training on the basis of routine exercises. The main steps included the establishment of a grip ball exercise group led by two specialist nurses. In addition, educational sessions were conducted by senior staff to highlight the significance of grip ball exercises in preventing PICC-related thrombosis and explain specific learning methods through department meetings, WeChat groups, face-to-face interactions, and online classrooms. Furthermore, patients were advised to maintain self-exercise diaries to enhance compliance. Junior staff were tasked with assisting patients in accurately understanding the exercise techniques. During the exercise, patients were instructed to keep their forearms in a neutral position, with the elbows bent at right angles to the upper arms, and to grip the ball in the following manner: squeeze the ball with force for 10 seconds, then rest for 10 seconds, and repeat this cycle at least 800 times daily. Additionally, the patients were also instructed to record their daily exercise regimen. If any abnormal conditions occurred during the exercise process, such as persistent or unrelieved pain in the limb where the catheter was placed, swelling at the catheter insertion site, catheter leakage, or fever, patients were instructed to promptly notify the nursing staff and, if necessary, seek medical attention at the hospital.
Observation indicators
Primary observation indicators
Information regarding pre- and post-treatment coagulation indicators and upper limb venous hemodynamic indicators of both groups were obtained from the electronic medical record system. The coagulation indicators include prothrombin time (PT), activated partial thromboplastin time (APTT), thrombin time (TT), tissue plasminogen activator (t-PA) level, fibrinogen (FIB), D-dimer, fibrinogen degradation products (FDP), and plasminogen activator inhibitor (PAI) levels. The upper limb venous hemodynamic indicators include peak systolic velocity (PSV), resistance index (RI), and blood flow velocity (Vm).
Secondary observation indicators
Compliance with functional exercise was assessed using a compliance table, which consists of four dimensions with a total of 16 items [8]. These dimensions are compliance with grip strength exercises, exercise monitoring compliance, active help-seeking compliance, and exercise precautions compliance. The scoring scale ranges from “impossible to do”, “occasionally done”, “basically done”, to “completely done”, with scores of 0, 1, 2, and 3 respectively. The total score is 50 points, where higher scores indicate better compliance. A satisfaction scale was employed for assessing nursing satisfaction, comprising four levels: very satisfied, satisfied, basically satisfied, and dissatisfied. The satisfaction rate was calculated as (very satisfied + satisfied + basically satisfied) individuals/total number of individuals × 100% [9].
Statistical methods
The data in this study underwent statistical analysis using SPSS 26.0 software. Measurement data were presented as mean ± standard error of the mean (SEM), and those normally distributed were analyzed utilizing t-test. Counting data were expressed as percentages and analyzed using Chi-square test. A significance level of P<0.05 was considered statistically significant.
Results
Comparison of baseline data between the two groups
There were no statistically significant differences between the two groups in terms of gender, age, course of disease, limb, and arm circumference (all P>0.05), indicating comparability (Table 1).
Table 1.
Comparison of general data between the two groups
| Gender (Male/female) | Age | Duration of disease (years) | Limb (left/right) | Arm circumference (cm) | |
|---|---|---|---|---|---|
| Observation group (n=56) | 36/20 | 41.2±2.8 | 7.3±2.1 | 31/25 | 26.5±3.4 |
| Control group (n=52) | 28/24 | 40.9±2.7 | 7.4±1.9 | 29/23 | 25.7±3.5 |
| χ2/t | 0.998 | 0.771 | 0.654 | 0.772 | 0.117 |
| P | 0.552 | 0.440 | 0.341 | 0.663 | 0.339 |
Comparison of the incidence of catheter-related thrombosis and related complications between the two groups
There were 4 cases of catheter-related thrombosis and 3 cases of complications (1 case each of dermatitis, phlebitis, and blood oozing) in the observation group, while in the control group, there were 12 cases of catheter-related thrombosis and 10 cases of complications (2 cases each of dermatitis; 4 cases each of phlebitis and blood oozing, respectively). Statistical analysis revealed a significantly lower incidence of catheter-related thrombosis in the observation group compared with that in the control group (P=0.011). Additionally, none of the patients showed obvious symptoms of thrombosis after active anticoagulant treatment, thus avoiding catheter removal (Table 2 and Figure 2).
Table 2.
Comparison of thrombus incidence between the two groups (n, %)
| Case | Thrombogenesis | |
|---|---|---|
| Observation group (n=56) | 56 | 4 (7.14) |
| Control group (n=52) | 52 | 12 (23.08) |
| χ2 | 6.478 | |
| P | 0.011 | |
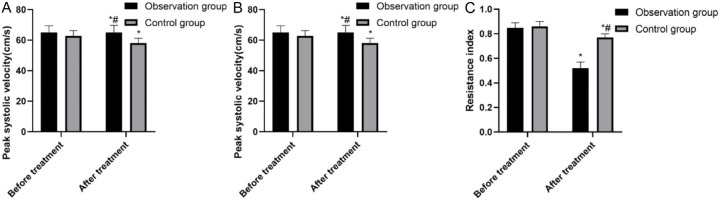
Figure 2.
Comparison of upper limb venous hemodynamics indicators between two groups before and after treatment. A. Peak systolic velocity; B. Blood flow velocity; C. Resistance index. *Compared with before treatment, P<0.005; #Compared with the control group after treatment, P<0.05.
Comparison of coagulation indicators between the two groups before and after treatment
There were no statistically significant differences in PT, APTT, TT, FIB, D-dimer, FDP, and PAI levels between the two groups prior to treatment. After treatment, PT, APTT, TT, and t-PA levels in both groups were significantly prolonged, whereas FIB, D-dimer, FDP, and PAI levels exhibited a significant decrease. Additionally, the levels of the above indicators in the observation group after treatment were significantly improved compared to those in the control group (all P<0.05) (Table 3).
Table 3.
Comparison of coagulation indicators between the two groups before and after treatment
| Time node | Observation group | Control group | t | P |
|---|---|---|---|---|
| PT | ||||
| Before treatment | 9.72±1.28 | 10.43±0.95 | 0.768 | 0.553 |
| After treatment | 13.26±0.88* | 12.27±0.76* | 1.551 | 0.043 |
| APTT | ||||
| Before treatment | 25.75±1.32 | 26.22±2.06 | 0.554 | 0.221 |
| After treatment | 29.79±2.85* | 28.84±2.15* | 1.669 | 0.037 |
| TT | ||||
| Before treatment | 15.83±0.96 | 15.78±0.85 | 0.883 | 0.602 |
| After treatment | 17.08±0.91* | 16.26±0.77* | 1.110 | 0.028 |
| FIB | ||||
| Before treatment | 4.26±0.55 | 4.31±0.69 | 0.772 | 0.523 |
| After treatment | 3.50±0.40* | 3.90±0.48* | 1.903 | 0.039 |
| D-dimer | ||||
| Before treatment | 233.27±49.53 | 241.22±58.83 | 0.904 | 0.821 |
| After treatment | 156.75±89.81* | 189.58±63.72* | 1.882 | 0.036 |
| FDP | ||||
| Before treatment | 3.58±0.53 | 3.63±0.69 | 0.762 | 0.541 |
| After treatment | 2.38±0.62* | 2.82±0.66* | 2.036 | 0.002 |
| t-PA | ||||
| Before treatment | 5.67±2.48 | 5.69±2.24 | 0.991 | 0.775 |
| After treatment | 7.17±2.74* | 6.49±2.74* | 3.440 | 0.017 |
| PAI | ||||
| Before treatment | 33.85±5.72 | 33.48±5.38 | 0.881 | 0.674 |
| After treatment | 27.98±4.25* | 32.18±4.86* | 6.433 | 0.002 |
Compared with before treatment, P<0.05;
PT, prothrombin time; APTT, activated partial thromboplastin time; TT, thrombin time; t-PA level, tissue plasminogen activator; FIB, fibrinogen; FDP, fibrinogen degradation products; PAI, plasminogen activator inhibitor.
Comparison of upper limb venous hemodynamic indicators between the two groups before and after treatment
There was a significant decrease in post-treatment PSV and RI in both groups, along with a significant increase in Vm compared with the pre-treatment levels (all P<0.05) (Figure 2).
Comparison of functional exercise compliance between the two groups
The scores of functional exercise compliance of patients in the observation group were significantly higher than those in the control group in all dimensions (all P<0.001) (Table 4).
Table 4.
Comparison of exercise compliance between the two groups
| Grip exercise | Exercise monitoring | Active help-seeking | Exercise precautions | Total | |
|---|---|---|---|---|---|
| Observation group (n=56) | 13.07±0.89 | 8.83±0.33 | 9.97±0.72 | 13.96±0.75 | 43.02±3.13 |
| Control group (n=52) | 9.98±0.67 | 6.31±0.65 | 6.93±0.5 | 7.84±0.87 | 20.07±6.84 |
| t | 15.662 | 14.117 | 12.440 | 13.002 | 19.112 |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Comparison of patient satisfaction between the two groups
The nursing score and patient satisfaction with nursing care in the observation group were significantly higher than those in the control group (Tables 5, 6).
Table 5.
Comparison of patient satisfaction between the two groups
| Very satisfied | Satisfied | Basically satisfied | Dissatisfied | |
|---|---|---|---|---|
| Observation group (n=56) | 36 | 10 | 7 | 3 |
| Control group (n=52) | 015792528 | 10 | 4 | 10 |
| χ2 | 4.901 | |||
| P | 0.027 | |||
Table 6.
Comparison of patient satisfaction scores between the two groups
| Knowledge | Skills | Attitudes | Appearances | Total | |
|---|---|---|---|---|---|
| Observation group (n=56) | 27.86±5.22 | 23.87±1.66 | 22.73±2.42 | 21.75±2.74 | 87.66±9.03 |
| Control group (n=52) | 21.66±5.33 | 17.73±4.36 | 16.57±5.03 | 17.06±5.20 | 73.05±10.12 |
| t | 3.596 | 6.882 | 5.867 | 6.365 | 7.645 |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Discussion
PICC is a medical procedure involving the insertion of a long catheter through a peripheral vein, usually the basilic vein or cephalic vein of the upper arm, and then advanced into a larger vein, typically a central vein. This technique has been in clinical use since late 1970s [10,11], and rapidly become the preferred venous access for various clinical scenarios, including long-term intravenous infusion, parenteral nutrition, chemotherapy, and intensive care, due to its unique advantages, such as being minimally invasive, easy to perform, and providing high patient comfort. However, thrombus formation after PICC insertion is a significant complication that cannot be ignored, as it can directly lead to PICC dysfunction [12,13]. The primary reasons contributing to the risk of thrombus formation after PICC placement include prolonged catheter retention in the vein and potential malpositioning, which may lead to changes in local hemodynamics and facilitate thrombus development. Thrombus formation poses a dual risk by potentially blocking the catheter to impede drug delivery, and by detaching and entering the bloodstream to cause severe complications like pulmonary embolism. Reducing the risk of thrombus formation involves precise measurement of the catheter length during PICC insertion to ensure proper placement and regular monitoring of catheter patency. Additionally, active functional exercise after placement also helps reduce thrombus formation [14,15].
Previous research has indicated that the incidence rate of PICC-related thrombosis ranges from 10% to 25%. In this study, the incidence rate in the control group was 23.07%, falling within the expected range. Notably, the incidence rate among patients in the observation group who engaged in exercises by using an intelligent ball was below 10% [16]. This result can be attributed to several factors. Regular exercise involving the ball in the limb where the catheter is inserted induces repetitive contractions and relaxations of the muscles in the upper arm, thereby enhancing venous flow velocity and volume. This mechanism creates an “artificial pump” effect, ultimately improving venous blood circulation in the affected limb. Furthermore, the act of gripping the ball can directly stretch the blood vessels of the limb with the PICC line, stimulating vascular endothelial cells and triggering the release of vasodilators including nitric oxide and thromboxane. These factors contribute to the dilation of blood vessels and an increase in blood volume, aligning with previous research findings [17,18].
We delved into the hemodynamic indicator of the PICC-inserted vein to enhance the tertiary prevention of venous thrombosis, building upon the premise that grip ball training can decrease the incidence of thrombosis. Studies have shown that after PICC placement, the vascular system is affected due to the special characteristics of the catheter materials. The central venous catheter is a long and thin tube that is typically inserted into a patient’s central vein, commonly the internal jugular vein, subclavian vein, or femoral vein, through a skin puncture [19]. This catheter is designed to come into direct contact with a significant volume of blood, facilitating rapid drug administration, precise monitoring of blood components, and effective nutritional support. However, upon insertion into the venous system of the human body, this small tube inevitably interacts directly with the blood, affecting blood flow. Specifically, the presence of the central venous catheter can alter the speed and direction of blood flow, particularly in the immediate vicinity of the catheter. This effect is primarily attributed to the catheter occupying space within the blood vessel and modifying the flow path of the blood, potentially resulting in decreased Vm and, in some instances, the development of a blood flow vortex [20]. The high tendency to thrombosis of the PICC-inserted vein is primarily due to several reasons. These include a decrease in average Vm, maximum flow rates, and vascular RI. The narrowing of the venous lumen of the catheter-inserted vein, as well as the characteristics of medications and tumor-related coagulation abnormalities, also contribute to this tendency [21,22]. Hence, it is crucial to effectively assess the hemodynamics of PICC-inserted vein to provide early detection of thrombosis. The analysis of the hemodynamics of the two groups demonstrated that after active upper limb functional exercise following PICC placement, both groups of patients showed significant improvements in coagulation indicators and hemodynamic parameters. Furthermore, the indicators of patients in the observation group were better than those in the control group, demonstrating that the intelligent grip ball can enhance the blood flow index of the catheter-inserted limb, thereby reducing the risk of thrombosis. The potential mechanism involves gripping the ball to boost the transit-time blood flow of PICC-inserted vessels, increase the flow velocity, and enhance PICC-related indicators due to the vein flexibility, which is consistent with previous research findings [23].
The concept of nursing satisfaction may appear simple, yet it contains intricate implications. It involves patients’ subjective feelings and evaluation of nursing service, as well as a multi-dimensional evaluation system [24,25]. Nursing satisfaction focuses on patients’ psychological experience, emotional response and satisfaction during care delivery, providing a comprehensive assessment of nursing services. Therefore, evaluating nursing satisfaction should consider not only the satisfaction of patients, but also the communication ability, professional skills, and attitude of nurses [26,27]. The results of this study showed that patients in the observation group, who underwent grip ball exercises, demonstrated significantly higher exercise compliance and nursing satisfaction compared with those in the control group. The lack of consistency and specificity in upper limb exercises after PICC placement in previous nursing activities may have contributed to suboptimal clinical intervention outcomes. Additionally, traditional upper limb exercises cannot effectively promote vascular patency due to inadequate intensity, force, and sustainability, failing to fundamentally address the risk of potential thrombosis caused by slow and insufficient blood flow. Grip balls can effectively address these shortcomings. They are cost-effective and user-friendly, offer high benefits, and save time. Furthermore, we proposed measures such as maintaining exercise diaries combined with online teaching to efficiently encourage patients to engage in uninterrupted exercises, achieving unexpected outcomes similar to “supervision”. This approach improves patients’ exercise enthusiasm and enhances their compliance. It also fosters better communication and deeper emotional bonds between medical staff and patients, ultimately improving nursing satisfaction. These results align with previous research findings [28-30].
In summary, upper limb exercises combined with intelligent grip balls can reduce the incidence of catheter-related thrombosis, improve coagulation function, enhance exercise compliance, and boost nursing satisfaction in patients with PICCs, justifying clinical recommendations. However, this is a single-center study with a small sample size, which necessitates large-sample, multi-center studies to confirm the clinical effects of grip ball intervention for upper limb venous thrombosis. Additionally, further studies are needed to maximize the clinical effect of grip balls.
Disclosure of conflict of interest
None.
References
- 1.Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, Sado M, Nakagawa A, Takahashi M, Hayashida T, Fujisawa D. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer-a randomized controlled trial. J Pain Symptom Manage. 2020;60:381–389. doi: 10.1016/j.jpainsymman.2020.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Greer JA, Jacobs JM, Pensak N, Nisotel LE, Fishbein JN, MacDonald JJ, Ream ME, Walsh EA, Buzaglo J, Muzikansky A, Lennes IT, Safren SA, Pirl WF, Temel JS. Randomized trial of a smartphone mobile app to improve symptoms and adherence to oral therapy for cancer. J Natl Compr Canc Netw. 2020;18:133–141. doi: 10.6004/jnccn.2019.7354. [DOI] [PubMed] [Google Scholar]
- 3.Hu Q, Su Y, Yan L. Effects of peripherally inserted central catheter (PICC) catheterization nursing on bloodstream infection in peripheral central venous catheters in lung cancer: a single-center, retrospective study. Comput Math Methods Med. 2022;2022:2791464. doi: 10.1155/2022/2791464. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Yavanoglu Atay F, Guran O, Sahin O, Cakmak F, Colak D, Mungan Akın İ. Pain during PICC insertion in preterm infants: the needle is not the only problem. J Matern Fetal Neonatal Med. 2023;36:2222205. doi: 10.1080/14767058.2023.2222205. [DOI] [PubMed] [Google Scholar]
- 5.Mielke D, Wittig A, Teichgräber U. Peripherally inserted central venous catheter (PICC) in outpatient and inpatient oncological treatment. Support Care Cancer. 2020;28:4753–4760. doi: 10.1007/s00520-019-05276-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zochios V, Umar I, Simpson N, Jones N. Peripherally inserted central catheter (PICC)-related thrombosis in critically ill patients. J Vasc Access. 2014;15:329–337. doi: 10.5301/jva.5000239. [DOI] [PubMed] [Google Scholar]
- 7.Swaminathan L, Flanders S, Horowitz J, Zhang Q, O’Malley M, Chopra V. Safety and outcomes of midline catheters vs peripherally inserted central catheters for patients with short-term indications: a multicenter study. JAMA Intern Med. 2022;182:50–58. doi: 10.1001/jamainternmed.2021.6844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ribeiro MM, Andrade A, Nunes I. Physical exercise in pregnancy: benefits, risks and prescription. J Perinat Med. 2021;50:4–17. doi: 10.1515/jpm-2021-0315. [DOI] [PubMed] [Google Scholar]
- 9.Omoronyia FR, Aina JO, Ogungbesan OO. Patient satisfaction with psychiatric nursing care: a survey in Calabar, Nigeria. J Psychosoc Nurs Ment Health Serv. 2020;58:50–55. doi: 10.3928/02793695-20200305-01. [DOI] [PubMed] [Google Scholar]
- 10.Moureau N. Hydrophilic biomaterial intravenous hydrogel catheter for complication reduction in PICC and midline catheters. Expert Rev Med Devices. 2024;21:207–216. doi: 10.1080/17434440.2024.2324885. [DOI] [PubMed] [Google Scholar]
- 11.Montanarella MJ, Agarwal A, Moon B. Peripherally Inserted Central Catheter (PICC) Line Placement. In: StatPearls. Treasure Island (FL) with ineligible companies. Disclosure: Ankit Agarwal declares no relevant financial relationships with ineligible companies. Disclosure: Brian Moon declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [PubMed] [Google Scholar]
- 12.Ma S, Shen C, Li Q, Yang H, Hu Y, Wei X, Liang T. Clinical factors of PICC-RVT in cancer patients: a meta-analysis. Support Care Cancer. 2023;31:393. doi: 10.1007/s00520-023-07855-8. [DOI] [PubMed] [Google Scholar]
- 13.Gao X, Mi X, Hou S, Kang C. Analysis of factors related to thrombosis in patients with PICC placements. Medicine (Baltimore) 2024;103:e37168. doi: 10.1097/MD.0000000000037168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu A, Liu X, Li Z, Lai C, Tan J. Effect of exercise therapy on PICC-associated venous thromboembolism: a meta-analysis. Phlebology. 2023;38:103–114. doi: 10.1177/02683555221149597. [DOI] [PubMed] [Google Scholar]
- 15.D’Arrigo S, Annetta MG, Musarò A, Distefano M, Pittiruti M. Secondary malposition of a PICC-port due to heavy physical exercise: a case report. J Vasc Access. 2023;24:507–510. doi: 10.1177/11297298211039445. [DOI] [PubMed] [Google Scholar]
- 16.Gale S. The evolving treatment landscape of pulmonary arterial hypertension. Am J Manag Care. 2021;27(Suppl):S42–S52. doi: 10.37765/ajmc.2021.88610. [DOI] [PubMed] [Google Scholar]
- 17.O’Brien MW, Shivgulam ME. Mechanistic, participant, and movement-related factors that contribute to low-flow-mediated constriction. Eur J Appl Physiol. 2023;123:2687–2697. doi: 10.1007/s00421-023-05332-y. [DOI] [PubMed] [Google Scholar]
- 18.Fujii N, McGarr GW, Notley SR, Boulay P, Sigal RJ, Amano T, Nishiyasu T, Poirier MP, Kenny GP. Effects of short-term heat acclimation on whole-body heat exchange and local nitric oxide synthase- and cyclooxygenase-dependent heat loss responses in exercising older men. Exp Physiol. 2021;106:450–462. doi: 10.1113/EP089025. [DOI] [PubMed] [Google Scholar]
- 19.Chen Q, Hu YL, Li YX, Huang X. Peripherally inserted central catheter placement in neonates with persistent left superior vena cava: report of eight cases. World J Clin Cases. 2021;9:7944–7953. doi: 10.12998/wjcc.v9.i26.7944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trinh HT, Nguyen TT, Nguyen TT. Cardiac tamponade due to pericardial effusion following peripherally inserted central catheter: a single-institution Case Series. Cureus. 2024;16:e56403. doi: 10.7759/cureus.56403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang D, Liao M, Chen J, Zhang X, Lu Y, Wang C. Application of nursing intervention based on intelligent grip strength system in patients with tumor PICC: a case-control study on promoting functional exercise and quality of life. Comput Math Methods Med. 2022;2022:8016567. doi: 10.1155/2022/8016567. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Taxbro K, Hammarskjöld F, Thelin B, Lewin F, Hagman H, Hanberger H, Berg S. Clinical impact of peripherally inserted central catheters vs implanted port catheters in patients with cancer: an open-label, randomised, two-centre trial. Br J Anaesth. 2019;122:734–741. doi: 10.1016/j.bja.2019.01.038. [DOI] [PubMed] [Google Scholar]
- 23.Kong S, Lee KS, Kim J, Jang SH. The effect of two different hand exercises on grip strength, forearm circumference, and vascular maturation in patients who underwent arteriovenous fistula surgery. Ann Rehabil Med. 2014;38:648–657. doi: 10.5535/arm.2014.38.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plevová I, Kachlová M, Jarošová D, Zeleníková R, Mynaříková E. Satisfaction with nursing care of hospitalized patients: a descriptive, cross-sectional, multicenter study. Med Pr. 2023;74:461–468. doi: 10.13075/mp.5893.01364. [DOI] [PubMed] [Google Scholar]
- 25.Fuseini AG, Bayi R, Alhassan A, Atomlana JA. Satisfaction with the quality of nursing care among older adults during acute hospitalization in Ghana. Nurs Open. 2022;9:1286–1293. doi: 10.1002/nop2.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alıcı CB, Koç Z. Quality of life and satisfaction affect individualized nursing care perceptions in intensive care. Psychol Health Med. 2020;25:148–159. doi: 10.1080/13548506.2019.1654110. [DOI] [PubMed] [Google Scholar]
- 27.Storm J, Chen HC. The relationships among alarm fatigue, compassion fatigue, burnout and compassion satisfaction in critical care and step-down nurses. J Clin Nurs. 2021;30:443–453. doi: 10.1111/jocn.15555. [DOI] [PubMed] [Google Scholar]
- 28.Gandolla M, Mariani C, Pozzi L, Mancini M, Foglia GM, Pedrocchi A. Hand grip support for rehabilitation and assistance: from patent to TRL5. IEEE Int Conf Rehabil Robot. 2022;2022:1–6. doi: 10.1109/ICORR55369.2022.9896562. [DOI] [PubMed] [Google Scholar]
- 29.Schranz C, Srivastava S, Seamon BA, Marebwa B, Bonilha L, Ramakrishnan V, Wilmskoetter J, Neptune RR, Kautz SA, Seo NJ. Different aspects of hand grip performance associated with structural connectivity of distinct sensorimotor networks in chronic stroke. Physiol Rep. 2023;11:e15659. doi: 10.14814/phy2.15659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cha RH, Lee GS, Yoo JY, Rhee OB, Jeon YD. Hand grip and leg muscle strength in hemodialysis patients and its determinants. J Korean Med Sci. 2021;36:e76. doi: 10.3346/jkms.2021.36.e76. [DOI] [PMC free article] [PubMed] [Google Scholar]