Abstract
Objectives: To evaluate the clinical efficacy of the combination of acupuncture and medicine for vascular dementia (VD) treatment, and to analyze and summarize the relevant association rules. Methods: A systematic search of Chinese and English databases such as CNKI, VIP, Wanfang, Embase, PubMed, Cochrane Library, and Web of Science was performed along with a manual search to screen for randomized controlled trials that met the inclusion and exclusion criteria that were published over a period from January 1, 2000, to July 31, 2023. Literature quality assessment and meta-analysis were performed using the Cochrane Handbook for Systematic Reviews of Interventions and RevMan 5.4 to explore the efficacy of TCM-acupuncture combination therapy and conventional Western medical therapy for VD treatment, as well as assess relevant improvements in MMSE, ADL, and HDS scale scores. A study database was created by entering the required data into MS Excel. The PROSPERO registration number for this systematic evaluation is CRD42023458282. High-use-frequency drugs and acupoints were screened for by using frequency statistics, and the nature of their categories was recorded separately. The source database was then imported into SPSS (version 26.0.0.2) and IBM SPSS Modeler (version 18.0) to elucidate high-use-frequency TCM drugs and acupoints for VD treatment. Results: Eighteen randomized controlled clinical trials with a total of 1617 participants were finally included. The meta-analysis results suggested that treatment combining traditional Chinese medicine (TCM) with acupuncture performed better in terms of efficacy and clinical improvement of related outcome indicators [OR = 2.54, 95% CI (1.98, 3.26), P < 0.05]. Twenty-four prescription drug groups and 18 acupuncture prescriptions were extracted from the 18 included studies. The following results were obtained: (1) The drugs with the highest use frequency were Acori Tatarinowii Rhizoma, Glycyrrhizae Radix Et Rhizoma, and Salviae Miltiorrhizae Radix Et Rhizoma; high-use-frequency tonifying herbs; and sweet, warm, and liver meridian-attributing drugs. (2) The acupoints with the highest use frequency were Baihui, Sishencong, and Zusanli, often applied on the head, face, and Du meridian points, as well as on high-use-frequency crossing acupoints. (3) The high-use-frequency drugs and acupoints could be clustered into four categories each. (4) The strongest associations were noted for the drug pairs Polygalae Radix-Glycyrrhizae Radix Et Rhizoma and Polugoni Multiflori Radix-Acori Tatarinowii Rhizoma, as well as the acupoint pairs Sishencong-Baihui and Zusanli-Baihui. Conclusion: TCM drugs combined with acupuncture demonstrated considerable clinical efficacy for VD treatment. The TCM-based treatment of VD mostly starts from the liver meridian and the Du meridian, with the use of more sweet and warm herbs and crossing acupoints. The general principles of treatment include smoothening the flow of qi and blood, tonifying the liver and kidneys in TCM, and enhancing the patient’s mood and cognitive function.
Keywords: Vascular dementia, acupuncture combined with medicine, randomized controlled trial, meta-analysis, data mining
Introduction
Vascular dementia (VD) is a result of brain damage due to different types of vascular diseases, generally attributable to blood vessel stenosis or occlusion, injury-related brain hemorrhage, ischemia, or brain tissue death. Its overall presentation follows a chronic course, occurring suddenly with fluctuating or stepwise progression and severely affects patients’ quality of life [1]. VD is the second leading cause of dementia after Alzheimer’s disease [2]. VD prevalence varies widely [3], with epidemiologic surveys suggesting that VD prevalence in individuals aged > 65 years in Asia can range from 0.6% to 4.2% - accounting for 15%-40% of all patients with dementia [4]. A study estimated that 15.07 million individuals aged > 60 years in China have dementia, of which 3.92 million have VD [5].
Most neurological treatments for VD start with screening and confirmation of VD diagnosis, management of multiple risk factors, and symptomatic management of cognitive impairment [6]. Because drugs ideal for targeted VD treatment are unavailable, dementia drugs such as donepezil hydrochloride, memantine hydrochloride, and nimodipine are commonly used in the current clinical practice. However, these drugs have poor therapeutic efficacy and lead to adverse effects on the gastrointestinal tract, cardiovascular system, and neurological system [7].
In traditional Chinese medicine (TCM), VD is categorized as a cerebral disease, called dullness disease. Dr. Jie-Bin Zhang, a warm recuperation school doctor from the Ming dynasty of China, proposed this name for dementia and its clinical symptoms (e.g., speech inversion and excessive sweating), which are “all kinds of strange”. TCM scholars generally believe that the disease lies in the brain and that within the scope of TCM, the heart, liver, spleen, and kidney dysfunction is closely related to VD onset. In TCM theory, kidney deficiency and the resulting loss of cerebral nourishment often manifests clinically as forgetfulness, slowed thinking, weakness, depression, and other symptoms related to intelligence and spirituality. Phlegm, stasis, fire, and toxins are TCM pathogenic factors. These factors may be related to Western medicine’s understanding of the deposition of Aβ proteins and neurofibrillary tangles (NFTs); they produce a series of lesions, ultimately resulting in brain atrophy and disruption of neurological structure and function and consequently leading to cognitive deficits. At present, the main TCM methods for treating VD involve the use of TCM-acupuncture combinations. These combinations are receiving increasing attention because they may treat VD from its essence.
In this study, we summarize and review published studies related to TCM-acupuncture combinations for VD treatment and evaluate the combinations’ efficacy using meta-analysis. Data mining is used in many fields, such as mathematics and statistics, to elucidate the potential connections and development trends within a large amount of data. This method aids in identifying the correlation between individual data points and quantifying the incidence of each item in a database [8]. Association rule mining is an unsupervised machine learning technique [9], and an apriori algorithm is an association rule algorithm, which generates frequent data pairs based on its features. Cluster analysis, a multivariate analysis technique, is used to categorize samples into different groups [10]. TCM practitioners often adjust TCM drug types and dosages during clinical consultations. Nevertheless, they do not adjust prescriptions for some drugs commonly used for main symptoms. These drugs can be identified using data mining techniques. As such, data mining is one of the most appropriate research tools for data collection and statistical analyses in TCM-related clinical research. The results of statistical analysis and generalization of clinical selection of acupuncture points and TCM drugs through data mining may provide a reliable reference for subsequent clinical treatment of VD.
Sources and methods
Search strategy for literature identification
We searched Chinese databases such as CNKI, VIP, and Wanfang and English-language databases such as PubMed, Web of Science, Embase, and Cochrane Library for appropriate randomized controlled trials and integrated this search result with our manual search results. All searches were conducted by combining subject terms with free words: “vascular dementia”, “traditional Chinese medicine”, “acupuncture”, “randomized controlled trial”, “Chinese medicine”, “acupuncture”, “randomized controlled”, and “Vascular dementia”, “VD”, “VaD”, “Chinese herbal medicine”, and “acupuncture therapy”. “Moxibustion” and “randomized controlled trial” were specifically used as English-language search terms. No language restriction was imposed on the searched documents, and the search time range was from January 1, 2000, to July 31, 2023. For instance, the following is the search formula we used to search CNKI: SU = ‘vascular dementia’ AND SU = ‘Chinese medicine’ + ‘Traditional Chinese medicine’ + ‘Single formula’ + ‘Compound formula’ + ‘Combination of needle and medicine’ + ‘Acupuncture therapy’ + ‘Acupuncture and moxibustion’ AND SU = ‘Randomized controlled trial’ + ‘RCT’ + ‘Clinical’ + ‘Trial’ NOT SU = ‘Review’ + ‘Meta’ + ‘Randomized controlled trial’ + ‘Clinical’ + ‘Trial’ NOT SU = ‘Review’ + ‘Meta’ + ‘Trial’. ‘Meta’ + ‘Trial’ + ‘Progress’. This systematic evaluation program is registered in PROSPERO under the number CRD420234582.
Inclusion criteria
All randomized controlled trials were evaluated according to the following model of study participants, interventions, controls, and outcomes (PICO): (P) The study participants were included regardless of sex and age, and all met the clinical diagnostic criteria: the Draft Diagnostic Criteria for Vascular Dementia [11]; the U.S. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) [12]; or the NIH’s National Institute of Neurological Disorders and Stroke (NINDS) in conjunction with the International Association for Research in Neuroscience (AIREN); developed in 1993 [13]. The degree of cognitive impairment was determined using The Mini-Mental State Examination (MMSE), revised by Folstein et al. in 1975, and the Clinical Dementia Rating (CDR), revised by Morris in 1993 [14]; a CDR of 0, 0.5, 1.0, 2.0, and 3.0 indicates no, suspected, mild, moderate, and severe dementia, respectively. (I) The intervention consisted of an acupuncture-medicine combination for VD, which was particularly defined in this study as the combination of acupuncture therapy and herbal tonics. (C) The control group received conventional Western medicine treatment, including oral Western medicine, intravenous Western medicine, and other treatments. (O) The outcome measures included overall effectiveness rate, MMSE [15] (to check the degree of cognitive impairment of patients), Activity of Daily Living Scale (ADL) [16] (to assess the ability of patients to care for themselves), and Hasegawa Dementia Scale (HDS) (a relatively simple method for screening for dementia) as clinical endpoints. The included trials contained at least one of these indicators, with overall clinical effectiveness as the primary outcome indicator.
Exclusion criteria
(1) Nonrandomized controlled trials, animal studies, reviews, theoretical seminars, case reports, and other nature; (2) Inclusion of patients with comprehension disorders who cannot cooperate or patients with dementia due to other diseases, combined with other neurological deficits or combined with other difficult and severe diseases; (3) Studies with repeated publications or unclear outcome indicators; (4) Studies in which TCM was applied in addition to Western medicine to the treatment group.
Literature selection
To ensure study inclusion accuracy, two independent researchers selected the literature and extracted the data according to the unified inclusion and exclusion criteria and selection plan; a third researcher resolved any dispute related to literature selection. Search results from different databases were imported into Endnote (version 20.4) to remove duplicates; then, titles and abstracts were read to remove obvious irrelevancies. Finally, the full text of potentially eligible studies was read and cross-checked to obtain a final list of included studies.
Meta-analysis
Data extraction
We collected the following data according to the criteria of the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0) for the literature that meets the quality standards: (1) general literature information (i.e., title, first author, publication time, source of the literature), (2) study characteristics [i.e., patients (number of samples, grouping method, and baseline information), interventions, and observational indicators (total clinical effectiveness, MMSE, ADL, and HDS)], (3) trial design plan, and (4) shedding and return visits. Next, two researchers jointly checked the results to confirm the collected data’s accuracy.
Assessment of risk of bias in included studies
Two researchers independently used RevMan (version 5.4) to assess the risk of bias of the included randomized controlled trials according to the risk of bias evaluation form in the Cochrane Handbook [17]; if there was any disagreement, the final decision was made through discussion. The results of the quality assessment of the included literature were categorized as low, high, and uncertain risk according to the points assessed (randomized distribution, concealment and blinding settings, completeness of results, likelihood of incomplete reporting of study results, and other risks of bias); any disagreements during the process were agreed on in consultation with a third researcher.
Statistical analysis
All data were analyzed using RevMan (version 5.4) for information analysis, and different extraction modes were selected based on the data type. Subsequently, the heterogeneity of the included trials was analyzed using methods such as the χ2 test, with significance levels set at P = 0.100 and I2 = 50%. P > 0.10 and I2 ≤ 50% indicated no heterogeneity, and for such data, a fixed effects model was used. For the combined effects analysis of the source of heterogeneity, a random effects model was used, with statistical significance set at P < 0.05. Sensitivity analysis was used to evaluate the stability of our meta-analysis results, and the 95% confidence interval (CI) was recalculated by selecting studies with a lower risk of bias; if it was consistent with the original conclusion, it indicated that the results were stable, and vice versa. The included literature was evaluated using a funnel plot if there was a risk of publication bias or if more than 15 studies were included for the same outcome indicator.
Data mining
Data extraction
Prescription sources were identical to the sources of meta-analysis data, and the acupoints of TCM drugs used in the included studies; they were categorically entered into an MS Excel sheet to build a database and explore the laws of compounding. The naming of traditional Chinese medicines was unified according to the 2020 Chinese Pharmacopoeia [18]; for instance, Raw Dihuang was unified as Rehmanniae Radix according to the textbook Chinese Medicine published by China Traditional Chinese Medicine Press [19]. Next, the TCM category was determined, and acupoint names were unified and standardized according to Acupuncture and Moxibustion [20]; for instance, Renzhong and Juegu were standardized as Shuigou and Xuanzhong, respectively. The input and naming verification process was repeated to ensure data accuracy.
Statistical analysis
Frequency analysis was used to summarize the TCM drugs that met the criteria; TCM drugs with frequency ≥ 5 were considered high frequency. We used MS Excel to categorize and statistically analyze the characteristics of the high-use-frequency TCM drugs; for a TCM drug with multiple properties, all the properties were recorded, and SPSS (version 26.0.0.2) was used to perform clustering analysis and set the inter-group linkage and the interval of Pearson’s correlation measurement. The clustering maps and association rules were then analyzed using IBM SPSS Modeler (version 18.0). The Apriori operation node was run to establish a model and explore the pairing pattern of high-use-frequency TCM drugs, with the support level set at 30.0%, confidence level at 85.0%, and maximum number of antecedent terms at 2. Acupoints with a frequency of ≥ 3 were counted as common acupoints; their sites, attributed meridians, and specific acupoints were recorded, with the support level for the association rule analysis set at 40.0%, confidence level at 90.0%, and maximum number of antecedents at 2. The remaining analysis process was similar to that for TCM drugs.
Results
Literature selection
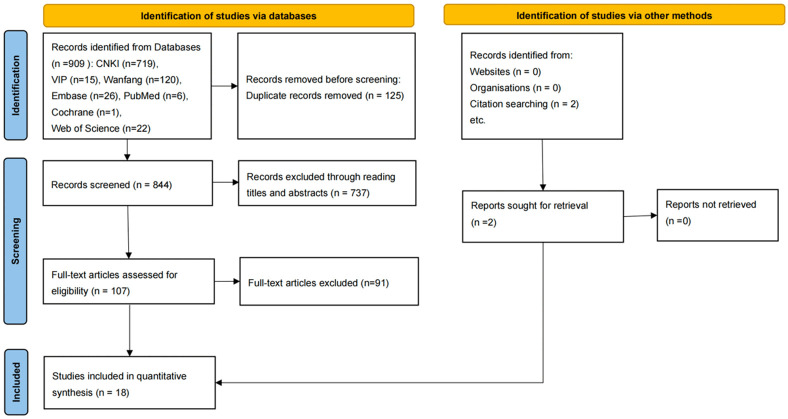
After the initial database and manual search, a total of 909 pieces of literature were obtained. After screening by two researchers according to the aforementioned criteria, 18 randomized controlled trials [21-38] were finally included (Figure 1).
Figure 1.
Flow of the study selection process.
Basic characteristics
All randomized controlled trials were in Chinese and included 1617 participants (n = 815 in treatment group and 802 in control group). The evaluation indexes used for dementia diagnosis in 17, 12, 10, and 5 trials were the overall clinical effectiveness rate, MMSE score, ADL scores, and HDS scores, respectively (Table 1).
Table 1.
Characteristics of included studies
| Reference | n | Age (years) | Sex (cases) | Interventions | Course (wk) | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| C | E | C | E | Female | Male | C | E | |||
| Feng et al. (2018) | 100 | 100 | 68±5 | 68±4 | 88 | 112 | Nimodipine | Gubentongqiao Decoction + Acupuncture | 24 | ① |
| Peng et al. (2013) | 60 | 60 | -- | -- | -- | -- | Donepezil Hydrochloride Tablets | Bushenhuoxuehuatan Recipe + Acupuncture | 8 | ① |
| Wang (2015) | 30 | 30 | 64.07±6.91 | 63.17±7.29 | 24 | 36 | Donepezil Hydrochloride Tablets | Yizhi Decoction + Acupuncture | 8 | ① ② ③ |
| Niu et al. (2016) | 22 | 22 | -- | -- | -- | -- | Piracetam Tablets | Bushenyizhi Recipe + Acupuncture | 8 | ① ② |
| Duan (2009) | 45 | 45 | 72.53±9.68 | 71.72±8.45 | 28 | 62 | Almitrine and Raubasine Tablets + Citicoline Injection | Yifeizengzhi Decoction + Acupuncture | 4.3 | ① ② ③ ④ |
| Li et al. (2012) | 30 | 30 | -- | -- | 26 | 34 | Piracetam Tablets | Yizhi Decoction + Acupuncture | 4 | ① |
| Huang et al. (2013) | 30 | 30 | -- | -- | 31 | 29 | Donepezil Hydrochloride Tablets | Yizhi Decoction + Acupuncture | 8 | ① ② ③ |
| Huang et al. (2020) | 35 | 35 | 67.42±3.21 | 68.54±3.01 | 30 | 40 | Donepezil Hydrochloride Tablets | Yinaozengzhi Decoction + Acupuncture | 1.4 | ② ③ |
| Shi et al. (2015) | 84 | 83 | 67.80±10.91 | 67.60±11.53 | 68 | 99 | Donepezil Hydrochloride Tablets | Huangdisan Granules + Western medicine placebo + Acupuncture | 12 | ① ② |
| Liu et al. (2011) | 20 | 20 | 42.60±10.20 | 44.20±10.60 | 10 | 30 | Folic acid + Vitamin B6 + Huperzine A Tablets | Bushenhuoxiequtan Recipe + Acupuncture | 4 | ① ② ③ ④ |
| Xing et al. (2007) | 25 | 25 | 68.70±4.49 | 66.95±6.80 | 23 | 27 | Piracetam Tablets | (TCM)Self-determined Formulas + Acupuncture | 12 | ① ② |
| Zheng et al. (2000) | 30 | 30 | -- | -- | 16 | 44 | Nimodipine | Fuyuan Decoction + Acupuncture | 8 | ① ④ |
| Wang (2012) | 36 | 40 | 76.18±9.34 | 75.20±9.16 | 23 | 53 | Cerebrolysin + Piracetam Tablets | Bushenkaiqiaohuoxiequtan Recipe + Acupuncture | 4 | ① ② ③ |
| Wang et al. (2013) | 30 | 30 | 72.53±9.68 | 70.72±8.45 | 27 | 33 | Piracetam Tablets | (TCM)Self-determined Formulas + Acupuncture | 12 | ① ② ③ ④ |
| Zhang et al. (2001) | 35 | 42 | 65.38±10.44 | 67.77±10.37 | 37 | 40 | Nimodipine + Piracetam Tablets | (TCM)Self-determined Formulas + Acupuncture | 8.6 | ① ② ③ ④ |
| Hu et al. (2015) | 100 | 103 | 69.55±5.84 | 71.68±5.35 | 89 | 129 | Donepezil Hydrochloride Tablets | (TCM)Self-determined Formulas + Acupuncture | 8 | ① ③ |
| Zheng et al. (2005) | 60 | 60 | 65.12±5.09 | 66.36±6.36 | -- | -- | Nimodipine + Piracetam Tablets + Almitrine and Raubasine Tablets | Huanglianwendan Decoction + Acupuncture | 8 | ① ② |
| Lu et al. (2013) | 30 | 30 | 66.00±8.00 | 69.00±9.00 | 26 | 34 | Huperzine A Tablets | Tongqiaohuoxie Decoction + Acupuncture | 4 | |
Notes: C = Control; E = Experiment; ① Clinical efficacy; ② MMSE; ③ ADL; ④ HDS.
Quality evaluation
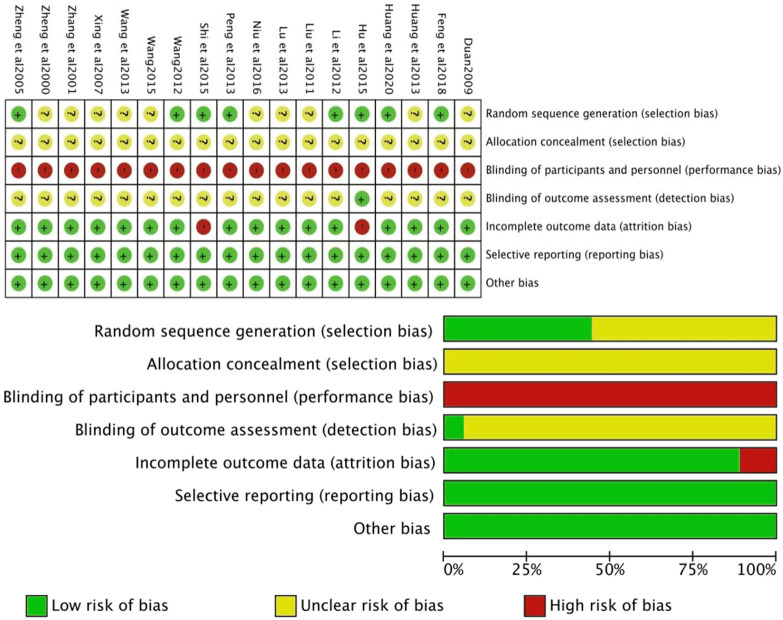
The quality of the included studies was evaluated using the Cochrane Risk of Bias Assessment tool (Figure 2).
Figure 2.
Risk of bias summary. Authors’ judgments about each risk of bias item for each included study are reviewed. “+” = low risk, “-” = high risk, “?” = unclear.
Meta outcome metrics analysis
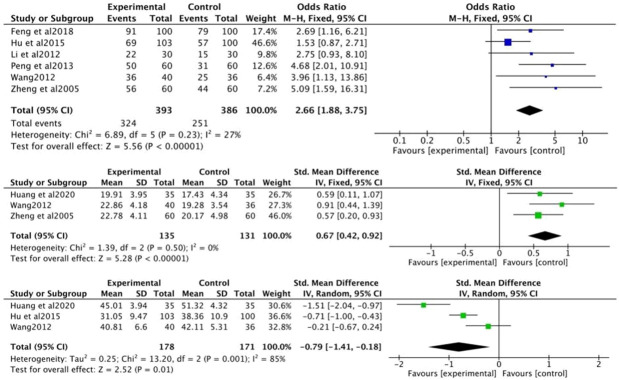
Clinical efficacy
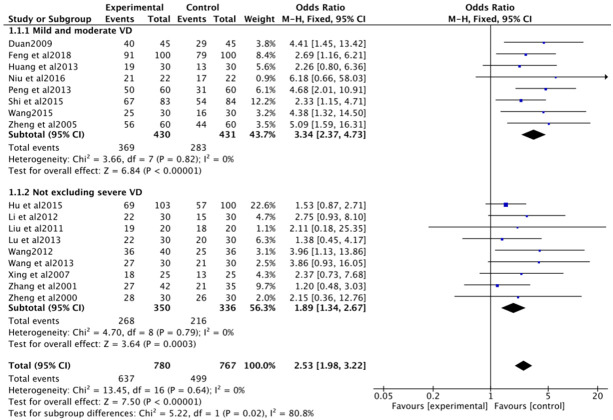
In total, 17 trials (n = 1547) analyzed the overall clinical efficacy rate as the outcome index. The heterogeneity test results demonstrated no heterogeneity (I2 = 0% < 50%, P > 0.10); therefore, a fixed effects model was used for analysis [OR = 2.54, 95% CI (1.98, 3.26), P < 0.05].
The study participants were divided into those with mild-to-moderate and those with no exclusion for severe VD; for both subgroups, the treatment group demonstrated better therapeutic efficacy than the control group, with the mild-to-moderate VD group [OR = 3.34, 95% CI (2.37, 4.73), P < 0.05] and those with no exclusion for severe VD [OR = 1.89, 95% CI (1.34, 2.67), P < 0.05] (Figures 3 and 4). The left-right asymmetry of the funnel plot suggested the presence of publication bias.
Figure 3.
Forest plot for effects of acupuncture plus TCM drugs on clinical efficacy of VD treatment using a fixed effects model.
Figure 4.
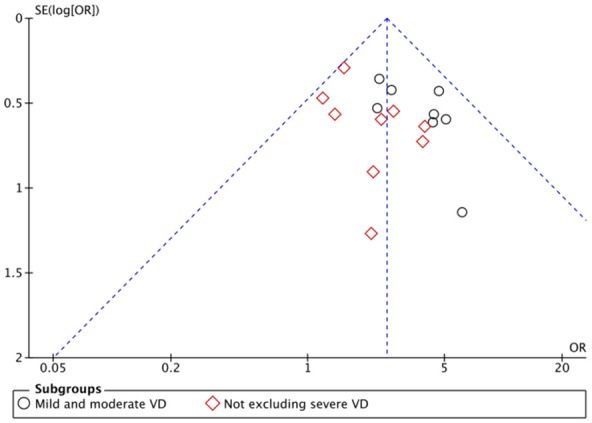
Funnel plot for publication bias of studies on the effects of acupuncture plus TCM drugs on clinical efficacy of VD treatment.
In summary, acupuncture-TCM drug combination therapy demonstrated better VD treatment efficacy than Western medicine; moreover, this efficacy was significantly better in patients with mild-to-moderate VD than in those with severe VD.
VD-related scales
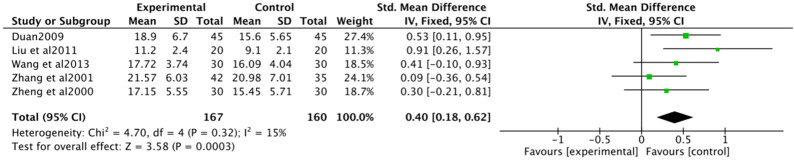
MMSE scores
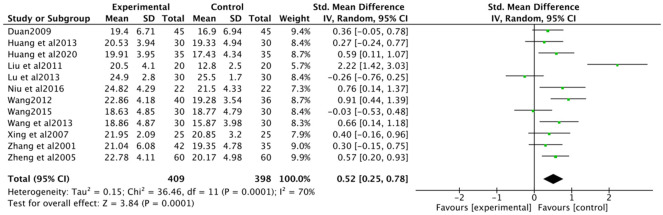
Twelve studies (n = 807) were included in this analysis. Heterogeneity was noted among these studies (I2 = 70%, P < 0.10); nevertheless, because of clinical homogeneity among these studies, we used a random-effects model [standard mean difference (SMD) = 0.52, 95% CI (0.25, 0.78), P < 0.05]. The statistically significant differences indicated that compared with the control group, the treatment group demonstrated a better improvement in the MMSE scores (Figure 5).
Figure 5.
Forest plot of the effects of acupuncture plus TCM drugs on the MMSE score using a random effects model. MMSE = Mini-Mental State Examination.
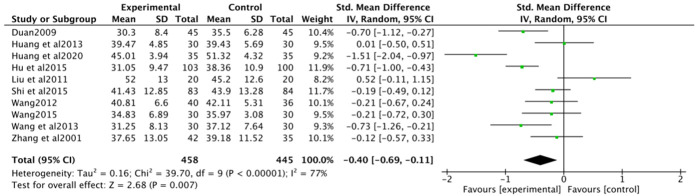
ADL scores
Ten studies (n = 903) were included in the analysis. Heterogeneity (I2 = 77%, P < 0.10), but clinical homogeneity among studies was examined, and a random effects model was chosen. The results showed [SMD = -0.40, 95% CI (-0.69, -0.11), P < 0.05], suggesting that the combination of acupuncture and medicine was effective in improving the ADL scores compared with the conventional Western medicine treatment, as shown in Figure 6.
Figure 6.
Forest plot of the effects of acupuncture plus TCM drugs on ADL scores using a fixed effects model. ADL = Activity of Daily Living Scale.
HDS scores
Five studies (n = 327) were included in this analysis. The studies did not demonstrate heterogeneity (I2 = 15% < 50%, P > 0.10); therefore, we used a fixed effects model. The results demonstrated a statistically significant difference [SMD = 0.40, 95% CI (0.18, 0.62), P < 0.05], indicating that the combination of acupuncture and TCM drugs demonstrated superior VD treatment efficacy in terms of the HDS scores compared with conventional Western medicine (Figure 7).
Figure 7.
Forest plot of the effects of acupuncture plus TCM drugs on HDS scores using a random effects model. HDS = Hasegawa Dementia Scale.
Sensitivity analysis
Sensitivity analysis was performed on the indicators for 10 or more included studies. After the exclusion of studies with no more than three low risks of bias, none of the results were changed, suggesting that the results were stable (Figure 8).
Figure 8.
Forest plot for sensitivity analysis of the effects of acupuncture plus TCM drugs on MMSE, ADL, and HDS scores.
Data mining results
Our meta-analysis of all 18 trials indicated that the efficacy indexes of the treatment groups were higher than those of the control groups. To further explore the use of medicines in the study and the pattern of the acupoints, we performed correlation analysis on TCM formulas and drugs used in the treatment group.
TCM drugs used for VD treatment
A total of 23 TCM formulas were extracted from the 18 included studies, which included a total of 59 TCM drugs; moreover, the cumulative frequency of TCM drug use was 206.
High-use-frequency TCM drugs and their properties
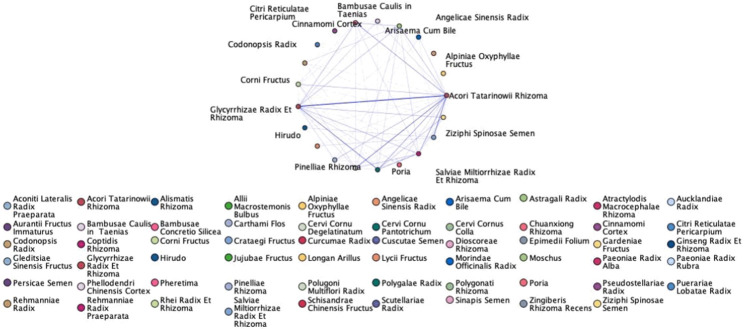
TCM drugs used at least five times were counted as high-use-frequency TCM drugs; 19 high-use-frequency TCM drugs were obtained. Top-three TCM drugs with the highest cumulative frequency in all prescriptions were Acori Tatarinowii Rhizoma (use frequency = 14, 60.87%), Glycyrrhizae Radix Et Rhizoma (use frequency = 12, 52.17%), and Salviae Miltiorrhizae Radix Et Rhizoma (use frequency = 11 times, 47.83%; Table 2). According to the efficacy of the TCM drugs involved in seven categories of TCM drugs, with a high frequency of tonifying herbs (48 times, 36.36%) and blood-activating herbs (26 times, 36.36%; Table 3). If a TCM drug had more than one property attributed to the meridian, all the properties were counted. Among the properties of the high-use-frequency drugs, warm (use frequency = 8, 47.06%) had the highest frequency; however, none had the heat property. Among the flavors of the high-use-frequency drugs, sweet (use frequency = 9, 34.62%) and bitter (use frequency = 6, 23.08%) had the highest frequency. Among the meridians of the high-use-frequency drugs, the meridians of the liver (use frequency = 9, 20.00%), heart meridian (use frequency = 8, 17.78%), and lungs (use frequency = 8, 17.78%) had the highest frequency (Figure 9).
Table 2.
Frequency of high-frequency herbal (≥ 5)
| Herbal | Frequency | Frequency distribution |
|---|---|---|
| Acori Tatarinowii Rhizoma | 14 | 60.87% |
| Glycyrrhizae Radix Et Rhizoma | 12 | 52.17% |
| Salviae Miltiorrhizae Radix Et Rhizoma | 11 | 47.83% |
| Chuanxiong Rhizoma | 9 | 39.13% |
| Polygalae Radix | 9 | 39.13% |
| Polugoni Multiflori Radix | 8 | 34.78% |
| Astragali Radix | 8 | 34.78% |
| Rehmanniae Radix Praeparata | 8 | 34.78% |
| Ziziphi Spinosae Semen | 7 | 30.43% |
| Lycii Fructus | 6 | 26.09% |
| Corni Fructus | 6 | 26.09% |
| Hirudo | 6 | 26.09% |
| Pinelliae Rhizoma | 6 | 26.09% |
| Codonopsis Radix | 6 | 26.09% |
| Poria | 6 | 26.09% |
| Arisaema Cum Bile | 5 | 21.74% |
| Bambusae Caulis in Taenias | 5 | 21.74% |
Table 3.
High frequency herbal classification
| Form | Herbal | Frequency | Frequency distribution |
|---|---|---|---|
| Tonifying herbs | Glycyrrhizae Radix Et Rhizoma, Astragali Radix, Rehmanniae Radix Praeparata, Polugoni Multiflori Radix, Codonopsis Radix, Lycii Fructus | 48 | 36.36% |
| Activating blood herbs | Salviae Miltiorrhizae Radix Et Rhizoma, Chuanxiong Rhizoma, Hirudo | 26 | 19.70% |
| Expectorant cough suppressant and anti-asthmatic herbs | Pinelliae Rhizoma, Arisaema Cum Bile, Bambusae Caulis in Taenias | 16 | 12.12% |
| Tranquilizer herbs | Polygalae Radix, Ziziphi Spinosae Semen | 16 | 12.12% |
| Resuscitation herbs | Acori Tatarinowii Rhizoma | 14 | 10.61% |
| Water wetting herbs | Poria | 6 | 4.55% |
| Astringent herbs | Corni Fructus | 6 | 4.55% |
Figure 9.
Properties, flavors, and attributes of high-use-frequency TCM drugs.
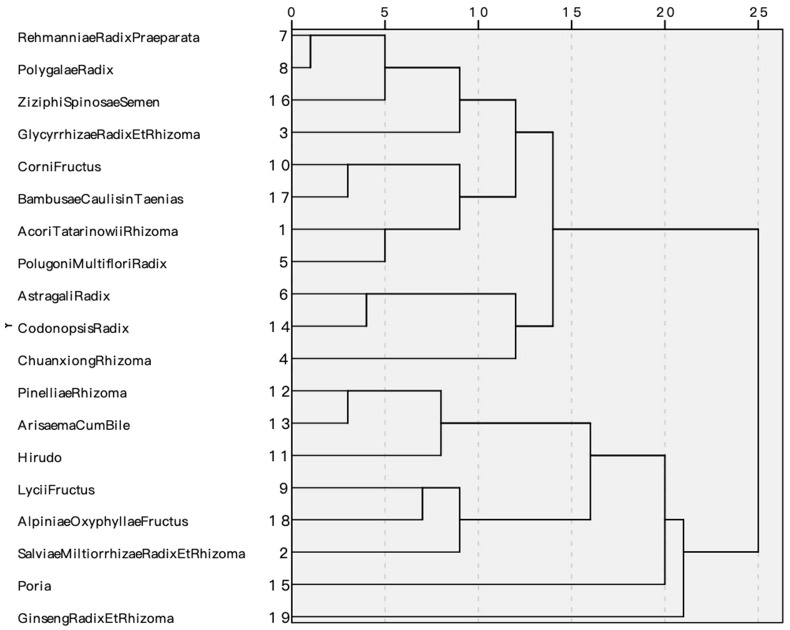
Clustering analysis of high-use-frequency TCM drugs
Clustering analysis of high-use-frequency drugs provided four categories (Figure 10): (1) Category 1: Rehmanniae Radix Praeparata, Polygalae Radix, Ziziphi Spinosae Semen, Chuanxiong Rhizoma; (2) Category 2: Pinelliae Rhizoma, Arisaema Cum Bile, Alpiniae Oxyphyllae Fructus, Salviae Miltiorrhizae Radix Et Rhizoma; (3) Category 3: Poria; (4) Category 4: Ginseng Radix Et Rhizoma.
Figure 10.
Clustering analysis of high-use-frequency herbals.
Analysis of association rules of TCM drugs for VD treatment
SPSS Modeler was used for the analysis of association rules. Apriori association rules were used for modeling, and the study extracted all the internal compatibility of TCM drugs, with the support set at 30%, confidence level at 85%, and maximum number of antecedent terms at 2. Of them, Polygalae Radix-Glycyrrhizae Radix Et Rhizoma and Acori Tatarinowii Rhizoma-Polugoni Multiflori Radix demonstrated the strongest correlation and highest frequency. Fourteen groups of core pairings were obtained (Table 4), and the noted drug associations are shown in Figure 11.
Table 4.
Association rule analysis of used herbals
| Entries | Antecedent | Percentage support | Percent confidence level |
|---|---|---|---|
| Glycyrrhizae Radix Et Rhizoma | Polygalae Radix | 39.13 | 88.889 |
| Polygalae Radix | Rehmanniae Radix Praeparata | 34.783 | 87.5 |
| Acori Tatarinowii Rhizoma | Rehmanniae Radix Praeparata | 34.783 | 87.5 |
| Acori Tatarinowii Rhizoma | Polugoni Multiflori Radix | 34.783 | 100 |
| Polygalae Radix | Ziziphi Spinosae Semen | 30.435 | 85.714 |
| Glycyrrhizae Radix Et Rhizoma | Ziziphi Spinosae Semen | 30.435 | 85.714 |
| Polugoni Multiflori Radix | Rehmanniae Radix Praeparata and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
| Glycyrrhizae Radix Et Rhizoma | Rehmanniae Radix Praeparata and Polygalae Radix | 30.435 | 85.714 |
| Acori Tatarinowii Rhizoma | Rehmanniae Radix Praeparata and Polygalae Radix | 30.435 | 85.714 |
| Polygalae Radix | Rehmanniae Radix Praeparata and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
| Rehmanniae Radix Praeparata | Polygalae Radix and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
| Astragali Radix | Chuanxiong Rhizoma and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
| Glycyrrhizae Radix Et Rhizoma | Chuanxiong Rhizoma and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
| Glycyrrhizae Radix Et Rhizoma | Polygalae Radix and Acori Tatarinowii Rhizoma | 30.435 | 85.714 |
Figure 11.
Association rule analysis of TCM drugs.
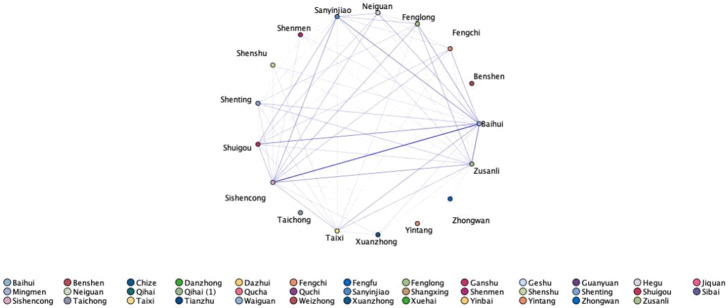
Use of acupoints for treating VDs
The 18 acupuncture prescriptions involved 37 acupoints, with a total frequency of 163. The total number of high-use-frequency acupoints with a frequency of ≥ 3 was 17, and their total use frequency was 133 (Figure 12).
Figure 12.
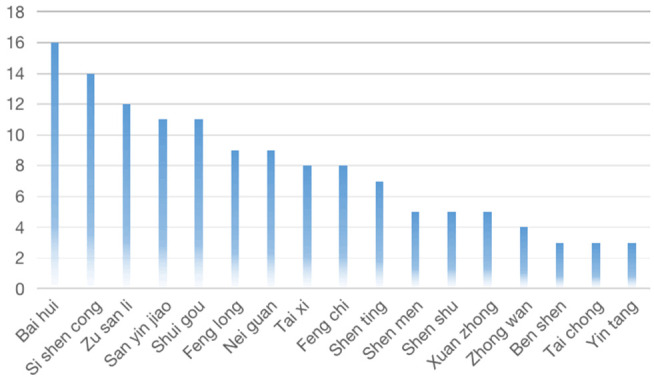
Frequency of high-use-frequency acupoints.
Acupoints and their properties
We summarized the acupoints according to the body parts attributable to the meridians and the specific points attributable to these meridians. The results demonstrated that the head and face were used 59 times (36.19%), with 9 acupoints, and the Du meridian was used 43 times (26.38%), with 8 acupoints. Moreover, the crossing acupoints were used the most frequently, with Sanyinjiao, Shuigou, and Neiguan being the main ones (Tables 5, 6 and 7). Most acupoints for VD are selected to be taken from the head and face, the directing vessel, and the crossing acupoints.
Table 5.
Statistics on the location of the used acupoints
| Position | Frequency | Acupoints (top three in frequency) |
|---|---|---|
| Head and face | 59 | Bai hui (16), Si shen cong (14), Shui gou (11) |
| Lower extremities | 52 | Zu san li (12), San yin jiao (11), Feng long (9) |
| Upper extremities | 21 | Nei guan (9), Shen men (5), He gu (2), Ji quan (2) |
| Neck | 13 | Feng chi (8), Da zhui (2), Tian zhu (2) |
| Chest and abdomen | 9 | Zhong wan (4), Qi hai (3), Guan yuan (1), Dan zhong (1) |
| Lumbar and back | 9 | Shen shu (5), Gan shu (2), Ge shu (1), Ming men (1) |
Table 6.
The attribution of used acupoints
| Meridians | Frequency | Number of Acupoints |
|---|---|---|
| Du meridian | 43 | 8 |
| Stomach meridian | 23 | 3 |
| Gallbladder meridian | 16 | 3 |
| Spleen meridian | 14 | 3 |
| Urinary bladder meridian | 12 | 6 |
| Ren meridians | 9 | 4 |
| Pericardium meridian | 9 | 1 |
| Kidney meridian | 8 | 1 |
| Heart meridian | 7 | 2 |
| Large intestinal meridian | 3 | 2 |
| Liver meridian | 3 | 1 |
| Lung meridian | 1 | 1 |
| Triple energizer meridian | 1 | 1 |
Table 7.
Statistics on specific acupoints
| Specific acupoint | Frequency | Number of Acupoints | Acupoints (top three in frequency) |
|---|---|---|---|
| Crossing acupoint | 69 | 11 | Bai hui (16), San yin jiao (11), Shui gou (11) |
| Luo-Connecting acupoint | 19 | 3 | Feng long (9), Nei guan (9), Wai guan (1) |
| Yuan-Source acupoint | 18 | 4 | Tai xi (8), Shen men (5), Tai chong (3) |
| Five Shu Points | 31 | 7 | Zu san li (12), Tai xi (8), Shen men (5) |
| The Lower He Sea acupoint | 12 | 1 | Zu san li (12) |
| The Eight Influential acupoint | 9 | 2 | Xuan zhong (5), Zhong wan (4) |
| Back-shu acupoint | 8 | 3 | Shen shu (5), Gan shu (2), Ge shu (1) |
| Front-mu acupoint | 1 | 1 | Guan yuan (1) |
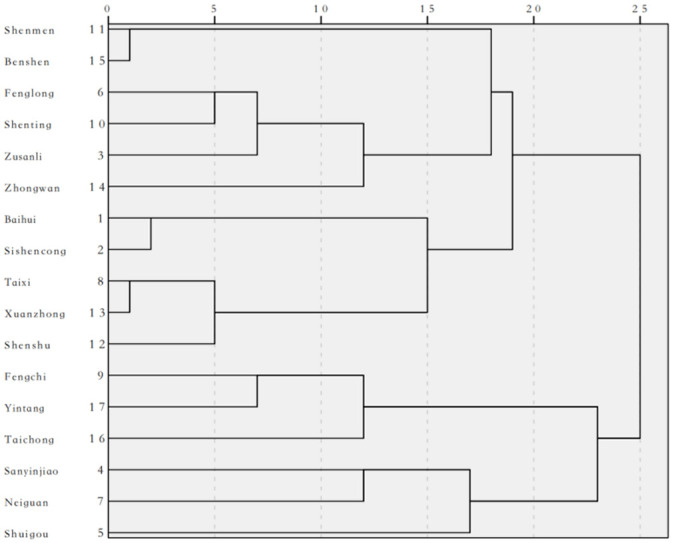
Clustering analysis of high-use-frequency acupoints
Clustering analysis of acupoints with high use frequency provided with four categories, Clustering analysis yielded four clusters (Figure 13): Category 1 included Shenmen, Benshen, Fenglong, Shenting, Zusanli, and Zhongwan; Category 2 included Baihui, Sishencong, Taixi, Xuanzhong, and Shenshu; Category 3 included Fengchi, Yintang, and Taichong; and Category 4 included Sanyinjiao, Neiguan, and Shuigou.
Figure 13.
Clustering analysis of high-use-frequency acupoints.
Association rule analysis of acupoints
The association rule analysis of acupoints used in acupuncture treatment VD was performed, with support set at 40%, confidence level at 90%, and maximum number of antecedent terms at 2. Thirteen association rules were obtained; the association network is shown in Figure 14, and the association rules are shown in Table 8.
Figure 14.
Association rule analysis of acupoints.
Table 8.
Association rule analysis of used acupoints
| Entries | Antecedent | Percentage support | Percent confidence level |
|---|---|---|---|
| Bai hui | Feng chi | 44.444 | 100 |
| Bai hui | Tai xi | 44.444 | 100 |
| Bai hui | Feng long | 50 | 100 |
| Bai hui | Si shen cong | 77.778 | 100 |
| Bai hui | Feng long and Zu san li | 44.444 | 100 |
| Bai hui | Feng long and Si shen cong | 44.444 | 100 |
| Bai hui | Shui gou and Si shen cong | 44.444 | 100 |
| Bai hui | San yin jiao and Si shen cong | 50 | 100 |
| Bai hui | Zu san li and Si shen cong | 50 | 100 |
| Bai hui | Zu san li | 66.667 | 91.667 |
| Bai hui | Shui gou | 61.111 | 90.909 |
| Bai hui | San yin jiao | 61.111 | 90.909 |
| Si shen cong | San yin jiao and Bai hui | 55.556 | 90 |
Discussion
Through meta-analysis of the included studies, we found that TCM-acupuncture combinations led to superior outcomes to Western medical therapy; the combinations also significantly improved the scores on the relevant scales. On further screening of TCM drugs and acupoints used in the study, we identified significant associations and formula patterns.
Comparison of the included studies
Therapeutic mechanisms for VD
Cerebral atherosclerosis is a major independent risk factor for VD. By reviewing literature published over the past 10 years, we found that the existing Western medical treatment mechanisms include the use of therapeutic modalities including cholinesterase inhibitors [39], antioxidant drugs, calcium antagonists, excitatory amino acid receptor antagonists [40], vasodilator drugs [41], hyperbaric oxygen, and rehabilitation. These mechanisms are aimed at preventing ischemia-induced necrosis of cerebral cells and softening of brain tissues via the pathways of microcirculation improvement, acetylcholine secretion promotion, neuroinflammatory process deceleration, and metabolism improvement. In clinical practice, this therapeutic approach has been noted to effectively improve the cerebrovascular status of patients, reflected by ADL and cognitive ability improvement, but not in patients who already have VD. Currently, commonly prescribed Western drugs are commonly associated with adverse reactions such as gastrointestinal symptoms such as diarrhea, nausea and vomiting, anorexia, neurological symptoms (e.g., hallucinations, dizziness, and headache), tremor, somnolence, and cardiovascular symptoms (e.g., low blood pressure, angina pectoris, and bradycardia) [13,42,43]. In addition, the treatment process leads to poor patient compliance due to a long treatment course, and the aforementioned adverse reactions lead to self-adjustment of drug dosage or discontinuation. As such, the patient’s condition often progresses to severe disease, imposing large physiological, psychological, and economic burdens on the patients and their families.
The 18th-century Chinese book on epidemic febrile diseases Wu Jutong Medical Cases - Stroke was the first to mention the term “prickly heat”, which considers that poststroke dementia often occurs due to the five viscera in TCM theory. These viscera are related to multiple risk factors for brain vascular diseases; kidney deficiency, phlegm, and blood stasis are crucial factors as well.
In TCM theory, the kidney essence, originating from parents, has the reproduction function and is the root of the brain marrow; it gradually decreases with age, leading to memory loss and ultimately dementia. Pathological changes such as synaptic damage occur in the early stage of VD; a relevant study [44] reported that the TCM concept of kidney tonic herbs affects brain-derived neurotrophic factor (BDNF). BDNF regulates hippocampal synaptic transmission and synaptic plasticity in kidney-deficient mice; this demonstrates the relevance of hippocampal neurons to the kidneys as defined by TCM. Scholars believe that brain marrow in TCM refers to the neurons and neurotrophic factors in the brain, as recognized by modern Western medicine, and that a decrease in neurotrophic factor levels and shrinkage of neurons with an increase in age can cause cognitive dysfunction.
In the lungs, spleen, and other internal organs, qi dysfunction leads to abnormalities in body fluid metabolism; this leads to the formation of phlegm turbid blockage of qi. Moreover, upward obstruction of the brain leads to dementia development. This process may be related to lipid metabolism disorders. In TCM theory, a greasy diet consumption leads to visceral dysfunction and phlegm accumulation; this is recognized in modern Western medicine as hyperlipidemia, where blood viscosity increases, leading to an increase in the coagulation state. Inflammatory responses lead to endothelial dysfunction, wall thickening, and increased plaque accumulation, slowing blood flow and altering vascular permeability; these eventually lead to platelet activation, thrombus formation, and blood vessel obstruction-consistent with blood stasis in TCM theory. Similarly, the metabolites of an inflammatory reaction can block the blood vessels and exacerbate vascular obstruction [45] such that repeated transient cerebral ischemia occurs in the parts of the cerebral cortex involved in cognitive functioning due to hypertension and small arteriosclerosis. Moreover, prolonged ischemic hypoperfusion leads to delayed neuron necrosis, followed by cognitive deficits.
Comparison of the included findings
In this study, we compared the VD treatment efficacy of acupuncture-medicine combination therapy with that of conventional Western medicine and explored the characteristics and pairing relationships of high-use-frequency drugs with acupoints statistically. In total, 18 papers were included and evaluated for different outcome indicators. In the 18 included studies, the participants’ disease diagnosis and outcome indicators were based on commonly used clinical criteria.
TCM drug use
Literature on TCM treatment of VD published over the past 5 years demonstrated a discrepancy in the results.
The TCM drugs commonly used in clinical practice are mainly sweet, bitter, and warm; they mostly belong to the liver and kidney meridians and include Acori Tatarinowii Rhizoma, Polugoni Multiflori Radix, and Glycyrrhizae Radix Et Rhizoma. In TCM theory, VD is related to the liver, and more closely related to the kidney. According to The Spiritual Pivot - The End and the Beginning, “Yin and Yang are both insufficient … can be placed on sweet medicines”, which suggests that sweet, warming, and tonic herbs can be used to treat a deficiency and bitter herbs can be used to strengthen the kidney yin while treating the liver and kidneys such that they nourish each other and restore each other’s functions.
The 2020 Chinese Pharmacopoeia [20] records the Polygalae Radix preparation method as follows: “Take Glycyrrhizae Radix Et Rhizoma, add appropriate amount of water to decoct the soup, remove the dregs, add clean Polygalae Radix, cook with mild fire until the soup is absorbed, take out, and dry it”. This method is the same as the one used in Lei Gong Gun Zhi Lun, aiming to reduce toxicity and increase the effect, tranquilizing the mind, benefitting the intellect, transporting the heart and kidneys, dispelling phlegm, and eliminating swelling. Acori Tatarinowii Rhizoma is acrid, bitter, and warm, belonging to the heart and stomach meridian and function; it can open the orifices and clear phlegm, wake up the spirit, and benefit wisdom. Polugoni Multiflori Radix is often used to treat vertigo, tinnitus, blood deficiency, and atrophy. Acori Tatarinowii Rhizoma-Polugoni Multiflori can act complementarily on the liver and kidneys, benefiting the essence and blood, tonifying the kidneys, and resolving phlegm. Modern pharmacological studies [46] have demonstrated that the active ingredients in Acori Tatarinowii Rhizoma-Polugoni Multiflori Radix, such as diphenyl glycosides and β-synephrine, can synergize with multiple targets and pathways and play a major role in the treatment of dementia-related therapies by inhibiting inflammatory responses.
Combined herb formulations, such as Yizhi drink and Shutiaoyizhi formula, include complexes that facilitate disease treatment. Our clustering analysis results suggested that the high-use-frequency TCM drugs could be categorized into four categories.
Category 1 includes Yizhi drink, Astragali Radix, Chuanxiong Rhizoma, and Codonopsis Radix, which act on the body’s qi and blood to make them flow and circulate smoothly. Moreover, the components of Suanzaoren soup are Ziziphi Spinosae Semen, Glycyrrhizae Radix Et Rhizoma, and Chuanxiong Rhizoma. Adding Acori Tatarinowii Rhizoma, Polygalae Radix, and Bambusae Caulis in Taenias to this soup can aid in calming the mind, reassuring the mind, and alleviating vexation. Moreover, Chuanxiong Rhizoma, Corni Fructus, Rehmanniae Radix Praeparata, and Polugoni Multiflori Radix can tonify the liver and kidneys - representing the basic pathogenesis in TCM theory.
Category 2 includes the additions to and subtractions from the Shutiaoyizhi formula. Pinelliae Rhizoma is used with Arisaema Cum Bile to remove dampness and resolve phlegm, whereas Salviae Miltiorrhizae Radix Et Rhizoma and Hirudo can invigorate blood circulation, expel blood stasis, open the orifices, and awaken the mind; Lycii Fructus and Alpiniae Oxyphyllae Fructus can nourish the liver and kidney.
In Categories 3 and 4, Poria and Ginseng Radix Et Rhizoma single medicines act as diuretics, seeping away dampness, tranquilizing the mind, and benefitting the intellect. In general, TCM treatment of VD often uses some herbs paired with each other, the components of which can regulate each other and act synergistically in the body. The overall treatment rules commonly used in clinical practice for treating VD obtained through literature search and screening are aimed at replenishing the qi, invigorating the blood, nourishing the liver and kidneys, and tranquilizing the spirit and mind.
Relevant TCM literature published so far has focused on only one syndrome; for instance, one study focused on blood stasis syndrome, the treatment of which is mainly based on blood activation and blood stasis elimination, supplemented by orifice opening, phlegm elimination, mind awakening, and liver and kidney nourishment. Nevertheless, by not restricting our study to a specific particular type of evidence, we could report on a wide range of treatments in the current study. Moreover, our conclusions here correspond to the initial analyses of TCM drugs and formulations.
Acupoint use
The most commonly selected acupuncture points selected clinically were on the head and the Vertical Chakra. VD affects the brain according to the principle of proximal point-taking. From the point of view of meridian circulation, the Du meridian starts from the Yu at the lower pole of the spine and ends at the Fengfu in the brain. In addition, the circulation of the directing vessel is also related to the kidneys; Su Wen - Bone Emptiness Theory states that “the directing vessel passes through the shoulder, holds the spine and arrives at the middle of the waist, and then enters through the brawn and connects to the kidneys”. In other words, the directing vessel connects the brain and kidneys by contacting the foot-sun bladder meridian and the foot-shaoyang kidney meridian. In addition, regulating the directing vessel aids in invigorating yang qi and improving the function of the brain. Acupuncture and moxibustion are good at dredging the meridians and regulating qi, and the junction point of all the meridians coordinates the whole body; this reflects the holistic concept of TCM.
Commonly used acupoint Baihui is the intersection of the three yangs of the hands and feet, the Du meridian, and the foot syncope meridian. The Du meridian is the main acupoint used for dementia, stroke, aphasia, insomnia, and amnesia treatment. Sishencong is an extra acupoint, mainly used to treat diseases such as epilepsy, stroke, and hemiplegia. Sishencong and Baihui can also wake up and open the mind. From the neuroanatomical point of view [47], acupuncture at Baihui can significantly improve glucose metabolism and blood flow in the cerebral cortex and the small cerebellum, and the Sishencong, adjacent to Baihui, demonstrates similar efficacy.
Clustering analysis yielded four clusters. Of them, Zusanli, Sanyinjiao, Neiguan, Shenmen, Fenglong, Taixi, Taichong, and Xuanzhong were located in the limbs; Zhongjiao was in the chest and abdomen; and Ren Yu (a distal point) in the lumbar back. Baihui, Sishencong, Shenting, Fengchi, Shuigou, Benshen, and Yintang are head and face acupoints, which are proximal; it is the method of distant and proximal matching points in acupuncture. Zusanli and Fenglong can regulate the spleen and stomach and replenish qi and blood. Shenting facilitates the convergence of qi and blood at the duking chakra. Benshen and Shenmen tranquilize the mind and wake up the brain. Baihui can tonify the kidneys and marrow, benefit the intellect, and wake the brain. Sishencong can calm the mind. Xuanzhong can open the meridians and activate the collaterals and channels. Shenshu and Taixi can nourish the kidney yin. Fengchi and Yintang can dispel wind, wake the brain, and open the mind. Taichong can increase the brain’s ability to rest the wind and open the channels. Sanyinjiao strengthens the spleen and dispels dampness. Neiguan can tranquilize the mind. Finally, Shuigou can awaken the mind and open the orifices.
We identified 13 groups of core acupoints. The group of Sishencong-Baihui is described above. Moreover, Zusanli-Baihui benefits qi and yang, invigorating the brain and benefitting the intellect.
Strengths and limitations of this study
Compared with similar studies registered with PROSPERO, our study included a longer timeframe, had more available outcome metrics, and reflected more perspectives on the effectiveness of different treatments. In addition, we did not limit the specific typology of patients when developing the inclusion and exclusion criteria; this allowed our results to include a more comprehensive classification of evidence types. The herbal efficacy percentage can also be used to suggest the current major evidence types for clinical VD and assist in VD management.
Previous studies [48-51] on the treatment of VD with Chinese medicine are mostly single interventions or specialized prescriptions, but VD has complex pathogenesis and clinical manifestations, so it is difficult to achieve the best therapeutic effect with a single treatment, and therefore we need to use a variety of measures to intervene. Acupuncture can stimulate the meridian qi, wake up the brain and open the mind, and the combination of acupuncture based on the identification of medication is the feature of our study, which is of great practical value and practical significance.
The current study has several limitations. First, in none of the included clinical trials, the control group received placebo acupuncture therapy. Considering the inherent nature of acupuncture therapy, it is difficult to ensure no to negligible therapeutic effects of an acupuncture technique. Therefore, detecting the differences in the therapeutic effects of acupuncture between the control and test groups, as well as blinding the physicians or participants, was difficult in most of the included studies. This may have increased the risk associated with literature inclusion and reduced the original research quality.
Second, the results for all treatment efficacy indicators demonstrated that the efficacy of acupuncture-TCM drug combinations led to improved VD treatment compared with conventional Western drugs; however, the risk of completeness bias of the outcome indicators may be high because all the included studies were conducted in China and because some of the included studies applied inadequate follow-up considerations.
In addition, patients with severe clinical dementia have difficulty understanding and accepting external information, demonstrate poor adherence to trials, and limit drug efficacy evaluation; therefore, future studies should consider recording detailed CDRs or MMSE scores when screening patients with VD and grouping them according to the degrees of their disease.
Finally, most of the evaluation indexes included in this study were scale scores, and the results obtained were considerably influenced by subjective factors related to physicians and patients and the basic cognitive levels of the subjects. To obtain more objective, accurate conclusions, VD biomarkers such as MRI, PET, amyloid β1-42 (Aβ1-42), phospho-tau (P-tau), and total tau (T-tau) may be included in future studies.
Practical implications of this study
The subgroup analysis of the total effective rate demonstrated that the combination of acupuncture and TCM drugs is more effective in the treatment of mild-to-moderate VD. However, elucidation of the principles and mechanisms of action shared by TCM drugs and acupoints is warranted to comprehensively understand the therapeutic advantages of combining TCM and acupuncture.
VD is covered by the broader category of vascular cognitive impairment (VCI), where patients commonly demonstrate the coexistence of vascular damage and neurodegeneration, both of which often progress to dementia [52].
Incomplete infarction due to repeated, chronic, or subclinical ischemia may be another major cause of ischemic brain injury. Brain injury location, number, and size determine whether dementia occurs and the extent of neurological and physical functioning it affects - suggesting that the focus of research should be shifted from alleviating VD symptoms to alleviating or preventing ischemic brain injury [53]. Preventing the onset of cardiovascular disease, pharmacological intervention for hypertension, and multifaceted modification of lifestyle habits may aid in achieving a reduction in dementia incidence among the population, as well as an improvement in cognitive functioning [54-56]. VD can be easily alleviated or prevented through early intervention, and it somewhat reflects the importance of this TCM principle: “preventing disease before it occurs and preventing changes in existing diseases” [57]. Therefore, VD treatment focuses on alleviating symptoms in the early stages of VD. To prevent VD, the popularization of healthy scientific lifestyles and the establishment of early screening mechanisms for risk factor-related diseases are warranted.
Acknowledgements
We would like to thank Dr. Rui-Dong Ge, Dr. Shan Jiang, and Dr. Dan-Tao Peng for their providing materials and technical assistance. The study was supported by two grants from the National High Level Hospital Clinical Research Funding (Nos. 2023-NHLHCRF-YSPY-01 and 2023-NHLHCRF-YYPPLC-TJ-19), and two grants from National Key Research and Development Program of China (Nos. 2022YFC2009700, 2022YFC2009706).
Disclosure of conflict of interest
None.
References
- 1.Standardization Project Team for the Guidelines for Clinical Application of Proprietary Chinese Medicines in the Treatment of Vascular Dementia. Clinical Application Guidelines for the Treatment of Vascular Dementia with Chinese Patent Medicines (2020) Chinese Journal of Integrated Traditional and Western Medicine. 2021;41:273–279. [Google Scholar]
- 2.O’Brien JT, Thomas A. Vascular dementia. Lancet. 2015;386:1698–1706. doi: 10.1016/S0140-6736(15)00463-8. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC, Sellke FW, Seshadri S American Heart Association Stroke Council, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on Cardiovascular Radiology and Intervention, and Council on Cardiovascular Surgery and Anesthesia. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu WX, Wang YJ. Epidemiology of vascular cognitive impairment in Asia. Chinese Journal of the Frontiers of Medical Science. 2020;12:1–8. [Google Scholar]
- 5.Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, Li Y, Li Y, Zhu M, Jiao H, Song Y, Shi Y, Zhang H, Gong M, Wei C, Tang Y, Fang B, Guo D, Wang F, Zhou A, Chu C, Zuo X, Yu Y, Yuan Q, Wang W, Li F, Shi S, Yang H, Zhou C, Liao Z, Lv Y, Li Y, Kan M, Zhao H, Wang S, Yang S, Li H, Liu Z, Wang Q, Qin W, Jia J COAST Group. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. 2020;5:e661–e671. doi: 10.1016/S2468-2667(20)30185-7. [DOI] [PubMed] [Google Scholar]
- 6.2024 Alzheimer’s disease facts and figures. Alzheimers Dement. 2024;20:3708–3821. doi: 10.1002/alz.13809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Das JM, Zito PM. Nimodipine. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 8.Bayardo RJ, Agrawal R. Mining the most interesting rules. ACM. 1999:145–154. [Google Scholar]
- 9.Agrawal R, Imielinski T. Mining association rules between sets of items in large databases. Washington D.C., USA: 1999. [Google Scholar]
- 10.Wu L, Liang W, Chen W, Li S, Cui Y, Qi Q, Zhang L. Screening and analysis of the marker components in ganoderma lucidum by HPLC and HPLC-MS(n) with the aid of chemometrics. Molecules. 2017;22:584. doi: 10.3390/molecules22040584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qian CY, Lu CZ, Wang XD. Draft diagnostic criteria for vascular dementia. Chin J Urol. 2002:57. [Google Scholar]
- 12.American Psychiatric Association. American Psychiatric Association: diagnostic and statistical manual of mental disorders. 2000 [Google Scholar]
- 13.Román GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, Amaducci L, Orgogozo JM, Brun A, Hofman A. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250–260. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 14.Gelb DJ, St Laurent RT. Clinical dementia rating. Neurology. 1994;44:1983–1984. doi: 10.1212/wnl.44.10.1983-a. [DOI] [PubMed] [Google Scholar]
- 15.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 16.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 17.Higgins JP, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Organized by the State Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China, Part Four, 2020 Edition. Beijing: China Pharmaceutical Science and Technology Press; 2020. [Google Scholar]
- 19.Peng C, Wang XG, Sun JN, Li CY, Miao MS, Hu YH, Cheng JY, Wei H, Ma J, Wang H, Wang XY, Wang RG. Pharmacology of Traditional Chinese Medicine New Century, 4th edition. Beijing: China Press of Traditional Chinese Medicine; 2016. [Google Scholar]
- 20.Zhao JP, Li Y, Chang XR, Ni GX, Cui J. Acupuncture and Moxibustion Undergraduate Traditional Chinese Medicine, 3rd edition. Beijing: People’s Medical Publishing House; 2016. [Google Scholar]
- 21.Feng MG, Liu CF, Chen L, Zheng G, Yang Q. Clinical study of Shuang Gu Yi Tong needling plus Chinese medication for vascular dementia. Shanghai J Acu-mox. 2018;37:982–986. [Google Scholar]
- 22.Liu Y, Wang DL. Clinical study on combined acupuncture and medicine in the treatment of vascular dementia due to kidney deficiency, phlegm and blood stasis. Guide of China Medicine. 2011;9:141–142. [Google Scholar]
- 23.Lu CJ, Zhou ZY, Liu GC, Lu JL, Wei BX, Wang JQ. Observation on the efficacy of combined use of acupuncture and medicine in the treatment of vascular dementia. Shanghai J Acu-mox. 2013;32:545–547. [Google Scholar]
- 24.Zhang ZZ, Zhou DA, Liu HL, Sheng L, Liu J. Clinical study on the treatment of vascular dementia with traditional Chinese medicine Shutiao Yizhi prescription and acupuncture Yuanshen prescription. Beijing Journal of Traditional Chinese Medicine. 2001:36–39. [Google Scholar]
- 25.Peng H, Li X, Liang L, Jiang XR. 60 cases of vascular dementia treated with kidney-tonifying, blood-activating and phlegm-resolving prescription plus Xingnao-kaiqiao acupuncture. Hunan Journal of Traditional Chinese Medicine. 2013;29:51–53. [Google Scholar]
- 26.Li SC, Li Y, Zhou YD. Clinical observation on the treatment of vascular dementia by combined acupuncture and Yi Zhi Yin. Journal of Clinical Acupuncture and Moxibustion. 2012;28:29–30. [Google Scholar]
- 27.Duan WY. Observation of combination of Yifei Zengzhi decoction and acupuncture - therapy on vascular dementia. Hebei J TCM. 2009;31:1768–1770. 1773. [Google Scholar]
- 28.Niu FJ, Ding SD, Huang XL, Shi DM. Observation on the effect of Xingnao Kaiqiao acupuncture combined with Bushen Yizhi prescription orally in the treatment of vascular dementia. Shandong Medical Journal. 2016;56:91–92. [Google Scholar]
- 29.Wang JX, Du NN. Clinical observation on traditional Chinese medicine and acupuncture on vascular dementia. Hubei Journal of TCM. 2013;35:3–4. [Google Scholar]
- 30.Wang QX. Clinical observation on the combination of acupuncture and medicine in the treatment of vascular dementia. Tianjin Journal of TCM. 2012;29:249–250. [Google Scholar]
- 31.Wang SN. Clinical observation on Xingnao Tiaoshen acupuncture combined with Yizhiyin in the treatment of vascular dementia. Heilongjiang Journal of TCM. 2014;43:59–60. [Google Scholar]
- 32.Shi JW, Jia YJ, Liu XX, Meng Y, Yu T, Han JX. Clinical effects of combination of acupuncture and medicine on treating moderate-mild vascular dementia. Journal of Nanjing University of TCM. 2015;31:206–209. [Google Scholar]
- 33.Hu YQ, Tang N, Wu L, Ling JH, Tan KW, Liang N, Lu CJ. Clinical observations on 110 cases of vascular dementia treated with traditional Chinese medicine comprehensive treatment programs. Journal of TCM. 2015;56:487–491. [Google Scholar]
- 34.Xing Y, Wang SX, Zhou ZK. Clinical observation on 50 cases of mild vascular dementia with phlegm obstruction type treated by combination of acupuncture and medicine. Heilongjiang Journal of TCM. 2007:40–41. [Google Scholar]
- 35.Zheng WL, Liu SX. Huanglian Wendan decoction combined with acupuncture to treat 60 cases of vascular dementia. Shanxi Journal of TCM. 2006:175–176. [Google Scholar]
- 36.Zheng L, Zhuang LX, Li YH. Observations on the curative effect of acupuncture and herbs on vascular dementia. Shanghai J Acu-mox. 2000:8–10. [Google Scholar]
- 37.Huang RF, Chen RH, Li XM, Guan WF, Guo F. Clinical effect of acupuncture combined with Yinao Zengzhi decoction in the treatment of vascular dementia after cerebral infarction. China Modern Medicine. 2020;27:71–73. [Google Scholar]
- 38.Huang ZK. Clinical observation on the treatment of acupuncture cooperate Yizhiyin in the treatment of obsessd with the vascular dementia phlegm turbidity resistance type. Acta Chinese Medicine and Pharmacology. 2013 [Google Scholar]
- 39.Liu Q, Wang XJ, Zhang ZC, Xue R, Li P, Li B. Neuroprotection against vascular dementia after acupuncture combined with donepezil hydrochloride: P300 event related potential. Neural Regen Res. 2016;11:460–464. doi: 10.4103/1673-5374.179059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ma X, Xu W, Zhang Z, Liu N, Yang J, Wang M, Wang Y. Salvianolic acid B ameliorates cognitive deficits through IGF-1/Akt pathway in rats with vascular dementia. Cell Physiol Biochem. 2017;43:1381–1391. doi: 10.1159/000481849. [DOI] [PubMed] [Google Scholar]
- 41.Paris D, Townsend KP, Humphrey J, Obregon DF, Mullan M. Statins inhibit Aβ-neurotoxicity in vitro and Aβ-induced vasoconstriction and inflammation in rat aortae. Atherosclerosis. 2002;161:293–299. doi: 10.1016/s0021-9150(01)00660-8. [DOI] [PubMed] [Google Scholar]
- 42.Wilcock GK, Black SE, Hendrix SB, Zavitz KH, Swabb EA, Laughlin MA Tarenflurbil Phase II Study investigators. Efficacy and safety of tarenflurbil in mild to moderate Alzheimer’s disease: a randomised phase II trial. Lancet Neurol. 2008;7:483–493. doi: 10.1016/S1474-4422(08)70090-5. [DOI] [PubMed] [Google Scholar]
- 43.Orgogozo JM, Rigaud AS, Stöffler A, Möbius HJ, Forette F. Efficacy and safety of memantine in patients with mild to moderate vascular dementia: a randomized, placebo-controlled trial (MMM 300) Stroke. 2002;33:1834–1839. doi: 10.1161/01.str.0000020094.08790.49. [DOI] [PubMed] [Google Scholar]
- 44.Sun LJ, Wang X, Wang XD, Zhang Q, Sun YR, Sun YG. Effect of kidney-supplementing TCM on brain-derived neurotrophic factor expresssion of rats with kidney-deficiency constitution. Chinese Journal of Information on TCM. 2015;22:64–66. [Google Scholar]
- 45.Hu WJ, Zhang BT, Wu R. The relationship between inflammatory injury, platelet activation and blood stasis syndrome. Journal of Nanchang University (Medical Science) 2012;52:81–83. 90. [Google Scholar]
- 46.Yang ML, Zhou XQ, Wu DH, Zhang YY, Zheng CX, Tong TH. Network pharmacology research and experimental calidation polygonimultiflori radix-acori Tatarinowii Rhizoma in Treating Alzheimer Disease. Chinese Journal of Information on TCM. 2021;28:36–41. [Google Scholar]
- 47.Lai XS, Huang Y, Tang AR, Tang CZ, Yang JJ, Li DJ, Zeng TJ, Zou YQ. Effects of acupuncture at Baihui point on brain functional imaging characteristics under pathological conditions. Journal of Guangzhou University of TCM. 2008:410–413. [Google Scholar]
- 48.Liu J, Gong J, Xu J, Fang M, Su M, Li W, Wu Y, Hui Y, He Y. Integrated network pharmacology and proteomic analyses of targets and mechanisms of Jianpi Tianjing decoction in treating vascular dementia. Evid Based Complement Alternat Med. 2023;2023:9021546. doi: 10.1155/2023/9021546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fan LL, Fang H, Zheng JY, Qiu YH, Wu GL, Cai YF, Chen YB, Zhang SJ. Taohong Siwu decoction alleviates cognitive impairment by suppressing endoplasmic reticulum stress and apoptosis signaling pathway in vascular dementia rats. J Ethnopharmacol. 2024;333:118407. doi: 10.1016/j.jep.2024.118407. [DOI] [PubMed] [Google Scholar]
- 50.Yang XN, Li CS, Chen C, Tang XY, Cheng GQ, Li X. Protective effect of Shouwu Yizhi decoction against vascular dementia by promoting angiogenesis. Chin J Nat Med. 2017;15:740–750. doi: 10.1016/S1875-5364(17)30105-X. [DOI] [PubMed] [Google Scholar]
- 51.Li N, Wang H, Liu H, Zhu L, Lyu Z, Qiu J, Zhao T, Ren H, Huang L, Chen S, Hu X, Zhou L. The effects and mechanisms of acupuncture for post-stroke cognitive impairment: progress and prospects. Front Neurosci. 2023;17:1211044. doi: 10.3389/fnins.2023.1211044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thal DR, Grinberg LT, Attems J. Vascular dementia: different forms of vessel disorders contribute to the development of dementia in the elderly brain. Exp Gerontol. 2012;47:816–24. doi: 10.1016/j.exger.2012.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chui H. Vascular dementia, a new beginning: shifting focus from clinical phenotype to ischemic brain injury. Neurol Clin. 2000;18:951–978. doi: 10.1016/s0733-8619(05)70234-6. [DOI] [PubMed] [Google Scholar]
- 54.Dodge HH, Chang CC, Kamboh IM, Ganguli M. Risk of Alzheimer’s disease incidence attributable to vascular disease in the population. Alzheimers Dement. 2011;7:356–360. doi: 10.1016/j.jalz.2010.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peters R, Beckett N, Forette F, Tuomilehto J, Clarke R, Ritchie C, Waldman A, Walton I, Poulter R, Ma S, Comsa M, Burch L, Fletcher A, Bulpitt C HYVET investigators. Incident dementia and blood pressure lowering in the hypertension in the very elderly trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7:683–689. doi: 10.1016/S1474-4422(08)70143-1. [DOI] [PubMed] [Google Scholar]
- 56.Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, Backman L, Hanninen T, Jula A, Laatikainen T, Lindstrom J, Mangialasche F, Paajanen T, Pajala S, Peltonen M, Rauramaa R, Stigsdotter-Neely A, Strandberg T, Tuomilehto J, Soininen H, Kivipelto M. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385:2255–2263. doi: 10.1016/S0140-6736(15)60461-5. [DOI] [PubMed] [Google Scholar]
- 57.Engelhardt E, Moreira DM, Laks J. Vascular dementia and the cholinergic pathways. Dement Neuropsychol. 2007;1:2–9. doi: 10.1590/S1980-57642008DN10100002. [DOI] [PMC free article] [PubMed] [Google Scholar]