Abstract
Purpose: To summarize scientific findings related to cancer patients undergoing chemotherapy infusions assisted by Immersive Virtual Reality (IVR). The study focused on the involvement of nurses, the sole healthcare professionals authorized to administer the chemotherapy infusion, and evaluated the extent to which IVR helped reduce anxiety and distress. Method: To conduct this review, various databases, including Medline (via Pubmed), Web of Science (WoS), CINAHL, Scopus, and Google Scholar were searched. The PRISMA guidelines were followed in accordance with the EQUATOR checklist. Results: Relevant articles were identified by searching for studies that explored the use of IVR to support cancer patients undergoing chemotherapy infusions, assessed their perceived anxiety and stress levels, and discussed the role of nurses in this context. A total of 23 papers were included in the review. Conclusions: Most of these studies indicated that using IVR to distract patients during chemotherapy infusions led to a reduction in anxiety and distress levels. This not only facilitated the nursing care process but also improved the patient’s compliance with the therapy regimen.
Keywords: Chemotherapy infusion, immersive virtual reality
Introduction
Currently, neoplasms are of significant concern due to their broad implications for health, psychological well-being, and economy. Despite advancements in early screenings [1-5], imaging, and precision medicine [6-8], the global incidence of cancer continues to rise and is projected to become the primary cause of mortality after 2030 [9]. Traditionally, a cancer diagnosis has been associated with end-of-life considerations, a perception that still persists for some patients. However, advancements in medical procedures and targeted therapies have extended survival for many individuals, for years and even decades. Although cancer is now classified as a chronic condition, it has introduced new challenges in terms of healthcare approaches and in addressing its social and emotional aftermath [10]. In light of this scenario, it becomes imperative to strengthen existing therapeutic strategies. Modern cancer treatments go beyond conventional methods, incorporating innovative approaches alongside established protocols (such as non-organ-specific drugs which have been used for years, but often with limited effectiveness). This expanded arsenal of chemotherapeutic agents, enabled by novel mechanisms of action, has improved treatment efficacy for specific cancers, including those affecting the colon, breast, stomach, ovaries, and lungs.
Anxiety is a complex emotional and psychological state, characterized by a subjective and unsettling apprehension concerning future events or potential threats, which can manifest as feelings of impending doom, tension, and physiological changes like heightened blood pressure [9]. Individuals suffering from anxiety and distress disorders often contend with recurring intrusive thoughts or concerns, alongside specific physical manifestations such as trembling, sweating, rapid heart rate, or dizziness [21,25]. Anxiety can be classified into two types: state anxiety, related to temporary conditions, and trait anxiety, which describes a more enduring disposition. Among cancer patients, anxiety intertwined with distress may arise from a multitude of factors, including reactions to the cancer diagnosis itself, intense pain, prolonged treatment regimens, side effects, and a sense of dependency or burden on others. Additionally, the struggle to control the adverse effects of cancer treatments contributes to this anxiety [12].
Distress is common among cancer patients, with prevalence rates ranging from 35% to 55%. Feelings of depression, sadness, and a lack of control over treatment decisions contribute to increased anxiety and distress levels, ultimately diminishing patients’ overall quality of life. The presence of distress, anxiety, and depression can exacerbate treatment-related side effects, compromise treatment effectiveness, and pose challenges for care management during chemotherapy infusion. Additionally, cancer patients undergoing chemotherapy face a plethora of stressors while receiving treatment, including the logistics of traveling to appointments, hospital transportation, the burden on caregivers, and apprehension about future outcomes [9,16,23]. Among various psychological interventions aimed at bolstering tolerance to chemotherapy, distraction emerges as a promising strategy. According to Lazarus and Folkman’s stress and coping model [15], individuals often adopt emotion-focused coping strategies when they perceive their ability to change a stressful situation as limited. These strategies include avoidance, minimizing the issue, distancing, selective attention, making favorable comparisons, and seeking positive or distracting aspects within negative circumstances. Distraction proves effective within this emotion-focused coping framework by diverting attention away from unpleasant stimuli toward more pleasant or engaging ones. Consequently, this redirection of focus contributes to the reduction of stress, distress, and anxiety [14,32].
Depression represents another significant psychological disorder often intertwined with distress and anxiety. Individuals with depression may experience not only a persistently low mood but also disrupted sleep patterns, changes in appetite, notable weight fluctuations, diminished interest or pleasure in daily activities, a pervasive lack of energy, difficulty concentrating, feelings of worthlessness, and recurrent thoughts of death or suicide [21].
In response to the challenges posed by distress and anxiety, patients and healthcare providers are increasingly recognizing the value of complementary and alternative medicine (CAM), particularly in light of the opioid epidemic, which has limited access to pain medications. Numerous cancer centers utilize distress screening tools as an initial measure to comprehend and enhance the overall quality of life for patients [18,23]. Over the years, health professionals have employed an array of strategies to address both the physical and psychological symptoms in patients. In the context of chemotherapy infusion, it is imperative for the healthcare team to acknowledge and address not just the biological impact of the disease, but also its psychosocial ramifications. The infusion process often evokes anxiety and fear, making it essential for professionals to manage these emotions based on their professional expertise. Inadequate handling of anxiety can potentially lead to the development of depression, dissatisfaction with treatments, and diminished adherence to the prescribed therapeutic regimen [10,15,19].
In this context, where the psychological management of cancer patients is crucial to improving treatment efficacy and quality of life, the advancement and integration of modern technology within healthcare present novel and minimally invasive avenues for addressing the array of symptoms and challenges associated with cancer. Notably, Virtual Reality (VR) has emerged as a potent supplementary tool in clinical medicine [22,29].
VR entails an interactive and computer-generated mode of diversion, where individuals engage as active participants within a virtual setting. The distinctive strength of VR lies in its capability to facilitate user interaction with simulated environments in ways that may be unattainable within the constraints of the physical world [17,23].
VR systems can be categorized into two main types: immersive (IVR) and non-immersive, with the level of immersion varying based on how disconnected the user is from the physical surroundings [24]. Non-immersive VR utilizes computer screens and input devices like joysticks and mice to create a virtual environment, enabling the user to engage with the virtual world while remaining connected to the external surroundings [11]. On the other hand, IVR employs a head-mounted display (HMD) to create a deep sense of immersion, facilitating exclusive 3D interaction between the user and the computer [17]. A HMD produces visual and auditory stimuli, and certain systems include motion sensor-equipped devices for the feet, enabling users to change scenes through simple foot movements. In some cases, advanced setups even allow users to experience scents through specialized mechanisms [26]. The cost of IVR has become more affordable over time, contributing to its broader adoption, and the necessary equipment is increasingly accessible [17,27]. VR technology has found applications in various medical fields, including surgery, rehabilitation, dentistry, neurology, and other clinical contexts. However, its application to patients undergoing chemotherapy presents several unresolved issues and aspects that have received limited attention in existing literature. This highlights the need for a scoping literature review to comprehensively address the concerns and controversies surrounding the use of VR technology in this specific setting. In the context of chemotherapy administration, the role of the nurse is uniquely critical. While physicians prescribe chemotherapy, the infusion itself is managed exclusively by nurses. No other healthcare professionals, including physicians, are authorized to perform this task. The use of IVR as a distraction to alleviate discomfort often coincides with the chemotherapy infusion, requiring the nurse’s physical presence. Therefore, the nurse not only administers the chemotherapy treatment but also ensures the proper execution of IVR protocols, serving as the primary guarantor of this process. This review aims to assess whether IVR can effectively reduce anxiety and distress in patients during chemotherapy infusions, and to explore the potential benefits this approach could offer to the nursing process.
Review question
Can IVR effectively reduce the levels of anxiety and distress experienced by patients undergoing chemotherapy infusion, and what are the potential benefits for the nursing process?
Methods
Protocol and registration
This scoping review was registered on Open Science Framework (OSF) platform (https://doi.org/10.17605/OSF.IO/K9N4V).
Eligibility criteria
We developed a research question for our review using the Population, Concept, Context (PCC) methodology (Table 1).
Table 1.
The Population, Concept, Context (PCC) instrument for the review of the literature
| COMPONENT | DESCRIPTION | DETAILS |
|---|---|---|
| Population | Adult patients with a histologically confirmed cancer diagnosis, undergoing chemotherapy. | Patients aged 18 and above, individuals receiving chemotherapy infusion as part of their cancer treatment. |
| Concept | The use of IVR as a distraction technique to reduce anxiety and distress. | IVR is used to reduce anxiety and distress levels during chemotherapy, with a focus on the role of nurses and healthcare professionals. |
| Context | The clinical setting of chemotherapy infusion, particularly in oncology departments. | Oncology departments where chemotherapy is administered, with involvement of nursing staff interacting with patients using IVR. |
Abbreviations: IVR: immersive virtual reality; PCC: Population, Concept, Context.
Inclusion and exclusion criteria
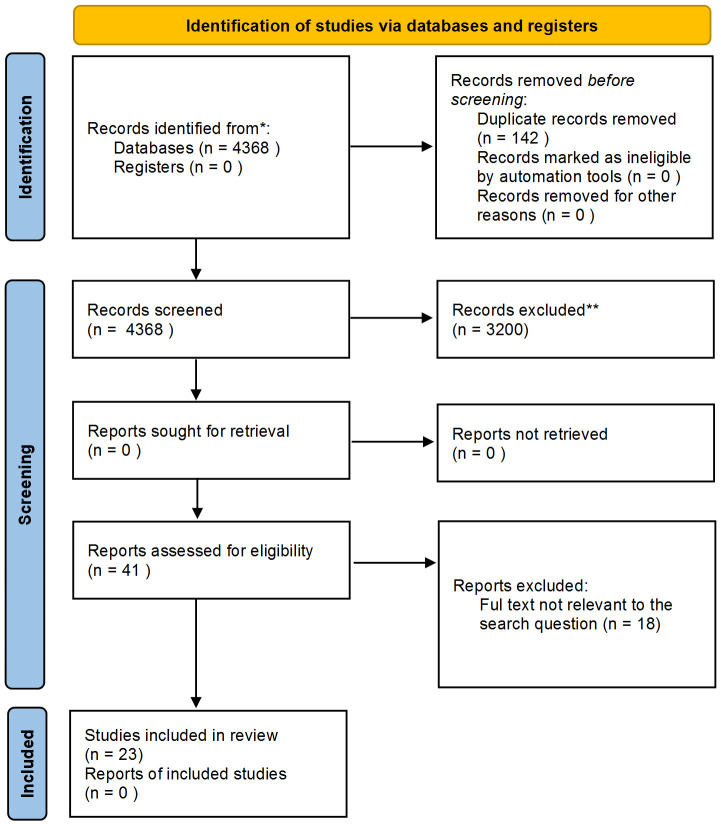
According to the EQUATOR checklist [28], the PRISMA guidelines were followed, as shown in Figure 1. Articles written in either English or Italian that met the following criteria were included in this review: 1. Cancer diagnosis clinically confirmed by histological examination; 2. Adult population ≥ 18 years; 3. Topic: IVR used as a distraction method during chemotherapy infusion to relieve patient anxiety and distress; 4. Articles available as full-texts.
Figure 1.
The PRISMA flow chart of the research.
Conversely, the studies that were excluded from the review satisfied the following criteria: 1. Studies involving the use of VR with non-oncology patients; 2. VR used for educational, training, or other purposes rather than a method of distraction; 3. Patients receiving VR during chemotherapy infusion to relieve pain from other medical procedures; 4. Pediatric and adolescent population.
Informational sources and search strategy
Our literature search covered databases such as MEDLINE (PubMed), Web of Science (WOS), Scopus, Google Scholar, and CINAHL (EBSCO). The search strategy incorporated both freetext and Medical Subject Headings (MeSH) terms, used individually and in combination with the Boolean operators AND and OR. Key terms such as ‘chemotherapy’, ‘nurse’, ‘virtual reality’, and ‘chemotherapy infusion’ (Table 2) were employed. An initial electronic search identified all articles relevant to the review’s objectives. Duplicate articles were removed, and the remaining ones were further evaluated. Two authors specifically reviewed the studies that potentially aligned with the research objective.
Table 2.
Key words combined with the Boolean operators
| Database | String | Limits | Results |
|---|---|---|---|
| Medline (Pubmed) | Search: ((virtual reality) AND (chemotherapy)) AND (nurse) | None | 10 |
| (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields]) AND (“chemotherapy s”[All Fields] OR “drug therapy”[MeSH Terms] OR (“drug”[All Fields] AND “therapy”[All Fields]) OR “drug therapy”[All Fields] OR “chemotherapies”[All Fields] OR “drug therapy”[MeSH Subheading] OR “chemotherapy”[All Fields]) AND (“nurse s”[All Fields] OR “nurses”[MeSH Terms] OR “nurses”[All Fields] OR “nurse”[All Fields] OR “nurses s”[All Fields]) | |||
| Medline (Pubmed) | Search: (chemotherapy infusion) AND (virtual reality) | None | 14 |
| (“chemotherapy s”[All Fields] OR “drug therapy”[MeSH Terms] OR (“drug”[All Fields] AND “therapy”[All Fields]) OR “drug therapy”[All Fields] OR “chemotherapies”[All Fields] OR “drug therapy”[MeSH Subheading] OR “chemotherapy”[All Fields]) AND (“infusate”[All Fields] OR “infusates”[All Fields] OR “infuse”[All Fields] OR “infused”[All Fields] OR “infuser”[All Fields] OR “infusers”[All Fields] OR “infuses”[All Fields] OR “infusing”[All Fields] OR “infusion”[All Fields] OR “infusions”[All Fields]) AND (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields]) | |||
| Medline (Pubmed) | Search: (chemotherapy) AND (virtual reality) | None | 261 |
| (“chemotherapy s”[All Fields] OR “drug therapy”[MeSH Terms] OR (“drug”[All Fields] AND “therapy”[All Fields]) OR “drug therapy”[All Fields] OR “chemotherapies”[All Fields] OR “drug therapy”[MeSH Subheading] OR “chemotherapy”[All Fields]) AND (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields]) | |||
| Scopus | Chemotherapy and virtual reality | None | 158 |
| Google Scholar | Nurse chemotherapy virtual reality | Research Articles | 1820 |
| CINAHL (through EBSCO Essential) | Chemotherapy and nurse and virtual reality | None | 2078 |
| Web of science (WOS) | Chemotherapy and virtual reality | None | 27 |
Results
A total of 4,368 records were identified through database searches. Prior to screening, 142 duplicate records were removed, resulting in 4,226 unique records for screening. The titles and abstracts of these 4,226 records were screened, leading to the exclusion of 3,200 records that were not relevant to the research question. Following this, 41 full-text reports were assessed for eligibility. During this assessment, 18 reports were excluded for various reasons: 15 were not relevant to the research question, and 3 did not have full-text available. Ultimately, 23 studies met the inclusion criteria and were included in the final analysis. The process of selecting sources of evidence is detailed in Figure 1, which presents the PRISMA flow diagram outlining the steps taken from identification to inclusion.
Characteristics of sources of evidence
This scoping review includes 23 studies, encompassing both observational studies and randomized controlled trials, each providing valuable insights into the use of IVR in managing anxiety and distress among patients undergoing chemotherapy infusion. The studies vary in design, with most employing descriptive observational methods to assess the impact of IVR on patient outcomes, while a smaller number use pre-post intervention designs to evaluate the effectiveness of IVR interventions.
The studies cover a range of patient populations, from paediatric to elderly cancer patients, and explore various aspects of IVR, including its role as a distraction tool, its impact on psychological well-being, and its potential to enhance the nursing process during chemotherapy.
Results of individual sources of evidence
Table 3 offers a detailed summary of the included studies, highlighting the authors, publication year, type of article, study population and main findings.
Table 3.
Studies included
| Author Year | Objective | Design | Sample | Results |
|---|---|---|---|---|
| Rutkowski 2021 [9] | To assess the effectiveness of a VR intervention in alleviating treatment-related anxiety and fatigue among cancer patients undergoing chemotherapy. | Descriptive observational | 453 patients receiving virtual reality and chemotherapy infusion | Drawing conclusions about the effectiveness of a virtual reality distractor for cancer patients is challenging due to the overall lack of methodological quality and statistical power observed in the current literature. |
| Schneider 2003 [16] | VR proves to be an effective distraction intervention in reducing pain levels associated with chemotherapy-related symptoms in older women with breast cancer. | Observational, pre-post | The implementation of a virtual reality distraction intervention was examined for its impact on the levels of suffering related to chemotherapy symptoms in a group of 16 women aged 50 and over. | There was a notable reduction in State Anxiety Inventory (SAI) scores immediately after chemotherapy treatments when participants engaged in VR (P = 0.10). |
| Ashley Verzwyvelt. 2021 [23] | VR has the potential to alleviate both the pain and distress experienced by cancer patients undergoing chemotherapy. | Observational, case-crossover | The study involved 33 participants diagnosed with breast, gynecological, gastrointestinal, pancreatic, and prostate cancers. | A significant majority, specifically 90.63% of the patients, expressed interest in understanding how nature could influence their health through the use of VR. |
| Wong 2021 [17] | The study aimed to evaluate the feasibility and acceptability of IVR as an intervention for relaxation and distraction, with the goal of reducing anxiety. | Observational, qualitative | Participants for the study will include both patients and their parents, as well as cancer nurses. Recruitment will take place at the oncology unit of a children’s hospital. | IVR enables patients to be completely engaged in an immersive environment, providing a distraction from noxious stimuli during chemotherapy. This engagement has the potential to reduce painful symptoms. |
| Birkhoff 2021 [30] | The study aimed to investigate the influence of a nursing intervention on anxiety levels and perceived self-efficacy. | Observational, descriptive | This study involved 35 cancer patients who were referred for their initial chemotherapy session. The participants were recruited from a large suburban cancer center in Newark, Delaware. | There was a significant decrease in anxiety levels, heart rate, and blood pressure from baseline to post-surgery. Additionally, perceived self-efficacy to cope increased significantly from baseline to the post-surgery assessment. |
| Janssen 2022 [27] | The objective was to investigate the feasibility and acceptability of utilizing VR for adult patients undergoing chemotherapy. | Observational, descriptive | The study included a total of 18 patients, with 5 of them taking part in semi-structured interviews. | Patients expressed that VR was beneficial in breaking up the monotony of their treatment. It offered an additional choice of activities alongside other recreational options. |
| Schneider 2011 [13] | The use of VR during chemotherapy resulted in an elapsed time compression effect. | Observational, descriptive | The study involved a combined sample of n = 137 participants diagnosed with breast, lung, or colon cancer. | In a forward regression model, three predictors - diagnosis, sex, and anxiety - accounted for a significant portion of the variability in the altered perception of time (F = 5.06, P = 0.0008). |
| Chirico 2020 [14] | Interventions that enhance treatment tolerance are pivotal for improving both the quality of life for patients and their adherence to therapies. | Observational, descriptive | Thirty patients were included in the VR group, 30 in the Music Therapy (MT) group, and 34 in the control group. | The VR group reported a mean post-operative anxiety score significantly lower than that of the control group (P = 0.001). The study results indicate that both VR and MT are beneficial interventions for alleviating anxiety. |
| Schneider 2007 [15] | The study aimed to investigate the use of VR as a distraction intervention to alleviate the discomfort of symptoms in adults undergoing chemotherapy treatments for breast, colon, and lung cancer. | Observational, crossover | A total of 123 adults underwent their initial chemotherapy treatments as part of the study. | Patients experienced an altered perception of time (P < 0.001) when using VR, confirming the distraction capacity of the intervention. The evaluation of the intervention revealed that patients found the head-mounted device easy to use, and 82% expressed a willingness to use VR again. |
| Scates. 2020 [31] | The utilization of VR as an alternative stress and pain relief therapy. | Observational, descriptive | The study involved 50 patients attending their regularly scheduled chemotherapy infusion sessions. | During data collection, the principal investigator observed the patients’ body language and facial expressions before, during, and after the VR experience. Although the patients reported feeling significantly less frustrated, the reduction in stress and pain was not statistically significant. |
| Oyama 2000 [26] | BSW has proven to be effective in reducing stress, improving mental well-being, and is suggested to aid in alleviating side effects and mental disorders in patients undergoing cancer chemotherapy. | Observational, case-control | The study included a total of 30 participants, comprising 6 males and 24 females. | Statistically significant reductions were observed in both fatigue and vomiting scores 3-5 days after chemotherapy (both P < 0.05), indicating noteworthy effects. The virtual reality system represents a novel therapeutic method that can be employed in palliative medicine. |
| Ioannou 2020 [19] | In recent years, VR has emerged as an intriguing alternative to traditional exposure-based therapies for various symptoms. | Observational, descriptive | A total of 882 titles and abstracts were reviewed, and 23 studies were included in the review. | This study contributes to the evidence indicating that distraction is an effective mechanism for managing symptoms. |
| Schneider 2004 [18] | The study aimed to explore the use of VR as an intervention through distraction to alleviate the discomfort of symptoms in women undergoing breast cancer chemotherapy. | Observational, cross-over | The study was conducted at the outpatient clinic of a global cancer center in the Midwest. The sample included 20 women aged between 18 and 55. | The primary research variables were symptom distress, fatigue, and anxiety. The results indicated significant decreases in symptom discomfort and fatigue immediately after chemotherapy treatments when women utilized the virtual reality intervention. |
| Bani 2018 [12] | The study aimed to assess the effectiveness of immersive VR as a distraction technology in reducing pain and anxiety among breast cancer patients. | Observational, randomized control | The study included a sample of 80 female patients diagnosed with breast cancer, recruited from a cancer center in Jordan. | The utilization of immersive VR as an adjuvant to surgery has been found to be more effective than morphine alone in alleviating pain and anxiety. Additionally, VR is considered a safe intervention compared to pharmacological treatments. |
| O’Gara 2022 [24] | VR integrates relaxation and compassionate mental health training to assess acceptability and feasibility in an oncological context. It also evaluates the impact on physical and psychological well-being as well as quality of life. | Observational, pre-post | 20 participants | There is a statistically significant difference in mean scores for EDA at mid-session and post-session compared to pre-session (1.658, 4.973) = 13.364, P < 0.05. There has been a statistically significant reduction in stress levels from baseline to the third session. |
| Keener. 2018 [10] | The purpose of this article was to ascertain the effectiveness of standardized and digitally registered education as an alternative teaching method. | Descriptive, observational | Utilizing a pre/post-test design, the study involved 92 patients who received registered instruction. | The digitally recorded educational method has led to a significant decrease in anxiety and an increased retention of knowledge. |
| Garcia 2014 [20] | Anxiety is among the most prevalent symptoms reported by patients undergoing their initial chemotherapy treatment. | Descriptive, observational | Ten articles were identified as pertinent to the clinical question, and they underwent evaluation for quality and methodological rigor. | Educating patients by nurses before their initial chemotherapy infusion in a tranquil environment proves to be the most effective approach. Strengthening the integration of successful patient education programs contributes to holistic care by placing greater emphasis on the psychosocial aspects of oncology. |
| Pourmand 2017 [29] | IVR simulations have the potential to enhance pain management by reducing the patient’s perception of both pain and anxiety. | Descriptive, observational | The search terms used resulted in 97 potential articles, and after screening, 45 articles were identified as meeting the study criteria and were consequently included in this review. | VR is poised to revolutionize the current approach to pain management, medical training, neurocognitive diagnosis, and physical rehabilitation. |
| Zeng 2019 [22] | The use of VR interventions on health-related outcomes in cancer patients. | Descriptive, observational | A total of 6 empirical studies met the eligibility criteria. | The study investigates the effectiveness of virtual reality-based interventions in cancer rehabilitation. |
| Zeng 2018 [21] | While existing evidence supports the use of VR in treating mental disorders, it remains uncertain whether IVR exercises would be beneficial for mental health. | Descriptive, observational | Four studies documented significant improvements in anxiety and depression measures following immersive IVR exercise. | The results indicate a preference for IVR exercise in alleviating symptoms of anxiety and depression. |
| Zasadzka 2021 [11] | IVR can provide women with breast cancer a secure environment for implementing various interventions. | Descriptive, observational | The initial search yielded a total of 144 records, and after applying the review criteria, 11 articles were identified and selected for analysis. | IVR can positively impact both mental and physical functions, such as alleviating anxiety during oncotherapy. |
| Leggiero 2020 [32] | VR has the potential to alleviate some of the negative aspects of the disease by allowing individuals to escape into environments where they can experience more positive thoughts and emotions. | Descriptive, observational | 721 patients across all the literature reviewed, from combined clinical study data. | The results of this review suggest that virtual reality can be used as an innovative delivery system. |
| Burrai 2023 [33] | Review of the literature, aiming to evaluate the effectiveness of VR in reducing anxiety, fatigue, and pain in patients undergoing chemotherapy, providing evidence to inform clinical decision-making. | Descriptive, observational | An overall sample of 459 patients. | The quality of the evidence is very low, and the strength of the recommendation is weak. Additional research holds significant potential to reduce uncertainty regarding the effects of VR during chemotherapy. |
Abbreviations: BC: breast cancer; BSW: wellness system in bed; EDA: electro dermal activity; IVR: virtual reality immersive; MT: music-therapy; SAI: state anxiety Inventory; VR: virtual reality; HDM: head-mounted device.
Overall, VR has proven to be an effective distraction tool in a range of medical and nursing procedures. Some studies describe VR as immersive, interactive, and capable of engaging multiple senses simultaneously, allowing individuals to experience auditory cues and tactile sensations corresponding to visual images, with a positive effect on typical symptoms related to chemotherapy such as anxiety, nausea and vomiting, even in paediatric patients [17]. VR can be non-immersive, where users maintain communication with the external world and healthcare personnel. Alternatively, it can be fully immersive (IVR), where users are completely engrossed in the virtual environment. This immersion is achieved through a HDM that projects images accompanied by sounds corresponding to the virtual scenario [19,31,32].
IVR does not require prior practice before its use in clinical settings [19]. The headset offers a secluded and isolated environment, allowing individuals to disconnect and focus on the virtual world presented to them [13,15,16,18]. Some studies suggest that the Bedside Wellness (BSW) system is effective in reducing stress, enhancing mental well-being and potentially alleviating side effects and mental disorders in patients undergoing cancer chemotherapy through the use of VR [26]. In [16], participants were randomly assigned to two groups: one group received the VR distraction intervention during chemotherapy, while the other group, serving as the control, received no distraction intervention. A paired t-test analysis revealed a significant reduction in State Anxiety Inventory (SAI) scores (P = 0.10) among participants who engaged in VR.
Several randomized pre- and post-intervention studies [FARE RIFERIMENTO A 9, 12, 14] have explored the efficacy of Immersive VR compared to pharmacological approaches in chemotherapy settings. Immersive and interactive VR has proven to be a valuable tool for distraction, aimed at mitigating chemotherapy-related anxiety, distress, and negative mood states among a cohort of Italian breast cancer patients. This study has also compared the effects of VR with those of music therapy (MT) [14]. In one study [24], salivary cortisol testing was conducted to assess the efficacy of IVR, obtaining statistically significant results.
Anxiety and distress are common responses to cancer diagnosis and are natural reactions to stressful situations. Preparing for chemotherapy can be especially anxiety-provoking for first-time patients who do not know what to expect [CITARE 30 e 32, LEGGIERO che ho reinserito]. Reference [30] describes a pilot study using a single-group experimental design to assess the feasibility of a personalized Immersive VR educational video for patients undergoing chemotherapy for the first time. Levels of anxiety and distress before chemotherapy treatment can significantly impact a patient’s empowerment and readiness for treatment; by using IVR, patients had the opportunity to visualize the chemotherapy process, including pre- and post-treatment stages, as experienced by others who had already undergone similar treatments.
The findings of a study involving 33 patients who underwent IVR during chemotherapy infusion [23] indicate that the patients experienced reduced heart rate, blood pressure, and stress levels after each biophilic intervention, whether in the physical presence of nature (Green Therapy) or through IVR. Patients described the experience as “fun” and “pleasant” when they were in the Green Therapy or VR room, as opposed to the control room.
The Safe-Space study was developed to assess the acceptability and feasibility of an IVR intervention that integrated relaxation and compassionate mental training in an oncology setting [24]. The study aimed to evaluate the impact of the intervention on physical and psychological well-being as well as quality of life. Mental well-being demonstrated improvement after each of the three intervention sessions compared to control sessions (IVR1 P ≤ 0.01; IVR2 P ≤ 0.01; IVR3 P ≤ 0.01).
Some literature reviews [22,29,32] provide data that strongly support the hypothesis that IVR simulations can improve pain management and especially decrease the anxiety and distress that subjects present before entering the health care facilities where they receive treatment. IVR can have a positive effect on mental and physical functions, such as relieving anxiety during oncotherapy, pain syndrome, and improving quality of life [11]. A recent review [33], however, takes a more critical and cautious stance, concluding that the evidence remains limited and further research is necessary before the effects of VR during chemotherapy are fully understood and can be recommended.
Discussion
Summary of evidence
Nurses, drawing on their expertise, have long employed various strategies to manage the diverse physical and psychological symptoms experienced by patients during chemotherapy infusion. This includes a holistic approach that addresses not only the biological effects of the disease but also its psychosocial implications [15,19]. In cancer care, the management of anxiety can be approached through both pharmacological and non-pharmacological means. This review aimed to explore the potential benefits of integrating IVR for cancer patients undergoing chemotherapy infusion, focusing on reducing anxiety and distress levels, while enhancing the proactive role of nurses.
While pharmacological treatments, such as the use of benzodiazepines to address anxiety and distress, may be effective, they often carry side effects and entail risks of addiction and interactions with chemotherapy drugs. As a result, non-pharmacological interventions can be safer alternatives. These interventions encompass a spectrum of techniques, including deep breathing exercises, imagery, relaxation practices, and the utilization of distraction. Notably, contemporary clinical approaches underscore the significance of non-pharmacological methods within nursing care, promoting patient recovery by enhancing social, cognitive, and emotional functions [CITARE 12].
Chemotherapy nurses play a crucial role in educating both patients and their families about cancer and its treatment. Due to their frequent interactions with patients, nurses have a central role in offering education and support [20]. In outpatient settings, the task of preparing patients for their initial chemotherapy treatment can be challenging, as a large amount of information needs to be conveyed in a short time. Moreover, patients often experience anxiety and an overwhelming sense of apprehension, particularly during the first infusion, which can hinder their ability to retain crucial information [10,20].
IVR is a sophisticated computer-simulated technique that engages multiple senses, allowing individuals not only to see but also to hear and feel stimuli within a simulated environment delivered through a head-mounted device. This technology offers a seamless and natural experience by projecting captivating scenarios that capture the user’s attention. The immersive nature of IVR minimizes distractions by external factors, and its intuitive HDM requires no prior training before being used in clinical settings [19].
In this scoping review, we identified 23 studies investigating the use of IVR in managing anxiety and distress among patients undergoing chemotherapy infusion. The included studies, published between 2000 and 2023, feature a variety of research designs, including observational studies and randomized controlled trials. Our findings highlight a growing interest in the potential of IVR as an effective tool for alleviating psychological distress and improving the overall patient experience during chemotherapy. Additionally, the evidence suggests that IVR may support the nursing process by enhancing patient engagement and reducing the perceived burden of treatment.
In various studies, the application of VR for patients undergoing chemotherapy infusion, particularly during initial sessions, has been shown to reduce fear and anxiety associated with the treatment process. As a result, patients have reported greater satisfaction, which, in turn, facilitates the nurse’s implementation of the nursing process [17]. The use of IVR has allowed patients to immerse themselves in diverse nature-themed environments, fostering an appreciation for nature’s beauty and engendering a sense of calmness. This approach has also reduced apprehension about chemotherapy appointments and increased feelings of tranquility during nursing procedures [23].
An intriguing example involves the creation of a 3D video using IVR technology to illustrate a “typical” day of a patient receiving chemotherapy infusion. This visual depiction, which involves collaboration between physicians and nurses, helps patients understand the therapeutic process and alleviate negative emotions. As a result, this approach contributes to a more favorable acceptance of the therapy and a subsequent reduction in anxiety and distress levels [30].
Compared to previous activities such as reading, using laptops, playing smartphone games, or even sleeping during chemotherapy sessions, the introduction of IVR scenarios made a notable difference in patients’ experiences. IVR scenarios evoked smiles and sparked interest, inducing a sense of relaxation, while also altering patients’ perception of time. Since clinical factors such as anxiety and distress can influence the perception of time, the IVR-enhanced infusion sessions appeared to reduce the patients’ perception of time [13,27].
The administration of chemotherapy drugs requires complex nursing care, where the nurse must understand and manage various drug prescriptions, infusion rates, and the routine administration of therapies to address side effects, such as antiemetics and pain relief medications. For patients experiencing heightened tension, effectively coping with treatment and cooperating with the healthcare team, particularly the nurse, can become challenging, complicating the procedures. IVR has shown promise in addressing this issue by reducing anxiety, which leads to a reduced perception of symptoms such as pain and nausea. This, in turn, contributes to an overall improvement in the quality of complex nursing care [15].
Several studies underscore the crucial role of nurses in preparing patients for chemotherapy drug administration, which is often performed through peripheral or central venous access (such as Porth Cath, PICC, or midline catheters). This procedure can evoke anxiety and apprehension in the patient. The studies indicate that with effective information dissemination and the utilization of IVR technology, a stronger therapeutic alliance can be established. Consequently, this approach leads to a reduction in anxiety and distress levels experienced by patients [18,27,31].
To provide a comprehensive view, it is important to acknowledge the negative experiences associated with the application of IVR during chemotherapy. Semi-structured interviews with patients highlighted both the effectiveness and some drawbacks of IVR in the context of drug treatment. One significant challenge identified was the time constraints faced by nurses who were already heavily engaged in various responsibilities such as drug preparation, administration, and management. These time constraints hindered their ability to operate the necessary displays for IVR use, leading to unfavorable implications for nursing care [27].
Furthermore, the use of IVR headsets can introduce technical challenges that impact nursing care quality. Issues such as mask discomfort, low audio volume, and suboptimal image clarity have been reported by nurses during the infusion process. These technical difficulties not only pose the risk of compromising the professionalism of nursing care but also introduce the potential for distractions that could result in errors [31].
In a different study, some patients reported a sense of discomfort during IVR sessions. Specifically, participants indicated that the IVR intervention failed to alleviate anxiety and distress as expected, and instead evoked feelings of compassion for their own condition [24]. This highlights the complexity of individual responses to IVR and underscores the need for a balanced consideration of its potential benefits and limitations in different patient scenarios.
Limitations
The limitations of this review include the scarcity of scientific literature, in particular the lack of large, randomized, blinded studies focusing on the role of nurses in managing cancer patients undergoing chemotherapy infusion with IVR. Few studies in fact described the specific scenarios during these treatments or assessed whether distraction effectively reduces anxiety and distress in patients and how nurses’ work might have benefited from this approach. Additionally, none of the studies included in this review reported long-term patient outcomes.
Conclusions
Reviewing the limited available literature indicates that IVR can reduce distress and anxiety in patients undergoing chemotherapy infusion. Distraction through HDM with headphones and complete isolation from the outside world benefits nursing procedures during drug treatment, helping patients manage treatment with reduced distress and anxiety. The review suggests that further research with larger samples is needed to better understand the benefits of using IVR not only in oncology but also in other clinical settings, especially in the Italian context.
Disclosure of conflict of interest
None.
References
- 1.De Nunzio G, Conte L, Lupo R, Vitale E, Calabrò A, Ercolani M, Carvello M, Arigliani M, Toraldo DM, De Benedetto L. A new berlin questionnaire simplified by machine learning techniques in a population of italian healthcare workers to highlight the suspicion of obstructive sleep apnea. Front Med (Lausanne) 2022;9:866822. doi: 10.3389/fmed.2022.866822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conte L, De Nunzio G, Lupo R, Mieli M, Lezzi A, Vitale E, Carriero MC, Calabrò A, Carvello M, Rubbi I, Federico M. Breast cancer prevention: the key role of population screening, breast self-examination (BSE) and technological tools. Survey of Italian women. J Cancer Educ. 2023;38:1728–1742. doi: 10.1007/s13187-023-02327-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conte L, Lupo R, Lezzi A, Paolo V, Rubbi I, Rizzo E, Carvello M, Calabrò A, Botti S, De Matteis E, Massafra R, Vitale E, De Nunzio G. A nationwide cross-sectional study investigating adherence to the Mediterranean diet, smoking, alcohol and work habits, hormonal dynamics between breast cancer cases and healthy subjects. Clin Nutr Open Sci. 2024;55:1–19. [Google Scholar]
- 4.Conte L, Lupo R, Sciolti S, Lezzi A, Rubbi I, Botti S, Carvello M, Fanizzi A, Massafra R, Vitale E, De Nunzio G. Exploring the landscape of breast cancer prevention among chinese residents in Italy: an in-depth analysis of screening adherence, breast self-examination (BSE) practices, the role of technological tools, and misconceptions surrounding risk factors and symptoms. Int J Environ Res Public Health. 2024;21:308. doi: 10.3390/ijerph21030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cortesi L, Galli GR, Domati F, Conte L, Manca L, Berio MA, Toss A, Iannone A, Federico M. Obesity in postmenopausal breast cancer patients: it is time to improve actions for a healthier lifestyle. The results of a comparison between two Italian regions with different “presumed” lifestyles. Front Oncol. 2021;11:769683. doi: 10.3389/fonc.2021.769683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tafuri B, Conte L, Portaluri M, Galiano A, Maggiulli E, De Nunzio G. Radiomics for the discrimination of infiltrative vs in situ breast cancer. Biomed J Sci Tech Res. 2019;24:17890–17893. [Google Scholar]
- 7.Conte L, Rizzo E, Grassi T, Bagordo F, De Matteis E, De Nunzio G. Artificial intelligence techniques and pedigree charts in oncogenetics: towards an experimental multioutput software system for digitization and risk prediction. Computation. 2024;12:47. [Google Scholar]
- 8.Conte L, Tafuri B, Portaluri M, Galiano A, Maggiulli E, De Nunzio G. Breast cancer mass detection in DCE-MRI using deep-learning features followed by discrimination of infiltrative vs. in situ carcinoma through a machine-learning approach. Appl Sci. 2020;10:6109. [Google Scholar]
- 9.Rutkowski S, Czech O, Wrzeciono A, Kiper P, Szczepańska-Gieracha J, Malicka I. Virtual reality as a chemotherapy support in treatment of anxiety and fatigue in patients with cancer: a systematic review and meta-analysis and future research directions. Complement Ther Med. 2021;61:102767. doi: 10.1016/j.ctim.2021.102767. [DOI] [PubMed] [Google Scholar]
- 10.Keener KA, Winokur EJ. Digitally recorded education: effects on anxiety and knowledge recall in patients receiving first-time chemotherapy. Clin J Oncol Nurs. 2018;22:444–449. doi: 10.1188/18.CJON.444-449. [DOI] [PubMed] [Google Scholar]
- 11.Zasadzka E, Pieczyńska A, Trzmiel T, Hojan K. Virtual reality as a promising tool supporting oncological treatment in breast cancer. Int J Environ Res Public Health. 2021;18:8768. doi: 10.3390/ijerph18168768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care. 2019;17:29–34. doi: 10.1017/S1478951518000639. [DOI] [PubMed] [Google Scholar]
- 13.Schneider SM, Kisby CK, Flint EP. Effect of virtual reality on time perception in patients receiving chemotherapy. Support Care Cancer. 2011;19:555–564. doi: 10.1007/s00520-010-0852-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chirico A, Maiorano P, Indovina P, Milanese C, Giordano GG, Alivernini F, Iodice G, Gallo L, De Pietro G, Lucidi F, Botti G, De Laurentiis M, Giordano A. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J Cell Physiol. 2020;235:5353–5362. doi: 10.1002/jcp.29422. [DOI] [PubMed] [Google Scholar]
- 15.Schneider SM, Hood LE. Virtual reality: a distraction intervention for chemotherapy. Oncol Nurs Forum. 2007;34:39–46. doi: 10.1188/07.ONF.39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneider SM, Ellis M, Coombs WT, Shonkwiler EL, Folsom LC. Virtual reality intervention for older women with breast cancer. Cyberpsychol Behav. 2003;6:301–307. doi: 10.1089/109493103322011605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong CL, Li CK, Choi KC, So WKW, Kwok JYY, Cheung YT, Chan CWH. Effects of immersive virtual reality for preventing and managing anxiety, nausea and vomiting among paediatric cancer patients receiving their first chemotherapy: a study protocol for an exploratory trial. PLoS One. 2021;16:e0258514. doi: 10.1371/journal.pone.0258514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneider SM, Prince-Paul M, Allen MJ, Silverman P, Talaba D. Virtual reality as a distraction intervention for women receiving chemotherapy. Oncol Nurs Forum. 2004;31:81–88. doi: 10.1188/04.ONF.81-88. [DOI] [PubMed] [Google Scholar]
- 19.Ioannou A, Papastavrou E, Avraamides MN, Charalambous A. Virtual reality and symptoms management of anxiety, depression, fatigue, and pain: a systematic review. SAGE Open Nurs. 2020;6:2377960820936163. doi: 10.1177/2377960820936163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcia S. The effects of education on anxiety levels in patients receiving chemotherapy for the first time: an integrative review. Clin J Oncol Nurs. 2014;18:516–521. doi: 10.1188/14.CJON.18-05AP. [DOI] [PubMed] [Google Scholar]
- 21.Zeng N, Pope Z, Lee JE, Gao Z. Virtual reality exercise for anxiety and depression: a preliminary review of current research in an emerging field. J Clin Med. 2018;7:42. doi: 10.3390/jcm7030042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeng Y, Zhang JE, Cheng ASK, Cheng H, Wefel JS. Meta-analysis of the efficacy of virtual reality-based interventions in cancer-related symptom management. Integr Cancer Ther. 2019;18:1534735419871108. doi: 10.1177/1534735419871108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ashley Verzwyvelt L, McNamara A, Xu X, Stubbins R. Effects of virtual reality v. biophilic environments on pain and distress in oncology patients: a case-crossover pilot study. Sci Rep. 2021;11:20196. doi: 10.1038/s41598-021-99763-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Gara G, Murray L, Georgopoulou S, Anstiss T, Macquarrie A, Wheatstone P, Bellman B, Gilbert P, Steed A, Wiseman T. SafeSpace: what is the feasibility and acceptability of a codesigned virtual reality intervention, incorporating compassionate mind training, to support people undergoing cancer treatment in a clinical setting? BMJ Open. 2022;12:e047626. doi: 10.1136/bmjopen-2020-047626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schneider SM, Hood LE. Virtual reality: a distraction intervention for chemotherapy. Oncol Nurs Forum. 2007;34:39–46. doi: 10.1188/07.ONF.39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oyama H, Kaneda M, Katsumata N, Akechi T, Ohsuga M. Using the bedside wellness system during chemotherapy decreases fatigue and emesis in cancer patients. J Med Syst. 2000;24:173–82. doi: 10.1023/a:1005591626518. [DOI] [PubMed] [Google Scholar]
- 27.Janssen A, Fletcher J, Keep M, Ahmadpour N, Rouf A, Marthick M, Booth R. Experiences of patients undergoing chemotherapy with virtual reality: mixed methods feasibility study. JMIR Serious Games. 2022;10:e29579. doi: 10.2196/29579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pourmand A, Davis S, Lee D, Barber S, Sikka N. Emerging utility of virtual reality as a multidisciplinary tool in clinical medicine. Games Health J. 2017;6:263–270. doi: 10.1089/g4h.2017.0046. [DOI] [PubMed] [Google Scholar]
- 30.Birkhoff SD, Waddington C, Williams J, Verucci L, Dominelli M, Caplan R. The effects of virtual reality on anxiety and self-efficacy among patients with cancer: a pilot study. Oncol Nurs Forum. 2021;48:431–439. doi: 10.1188/21.ONF.431-439. [DOI] [PubMed] [Google Scholar]
- 31.Scates D, Dickinson JI, Sullivan K, Cline H, Balaraman R. Using nature-inspired virtual reality as a distraction to reduce stress and pain among cancer patients. Environ Behav. 2020;52:895–918. [Google Scholar]
- 32.Leggiero NM, Armstrong TS, Gilbert MR, King AL. Use of virtual reality for symptom management in solid-tumor patients with implications for primary brain tumor research: a systematic review. Neurooncol Pract. 2020;7:477–489. doi: 10.1093/nop/npaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burrai F, Sguanci M, Petrucci G, De Marinis MG, Piredda M. Effectiveness of immersive virtual reality on anxiety, fatigue and pain in patients with cancer undergoing chemotherapy: a systematic review and meta-analysis. Eur J Oncol Nurs. 2023;64:102340. doi: 10.1016/j.ejon.2023.102340. [DOI] [PubMed] [Google Scholar]