Abstract
Objectives: To construct a three-dimensional visualized model of the sacral nerve canal, and understand its structure and angles. Methods: This was a retrospective study including 20 patients undergoing computerized tomography (CT) scanning of the sacrum. Consecutive CT images in Dicom format were directly imported into Mimics software. The images were edited selectively and repaired by hole procession. The sacral nerve canal was removed and a three-dimensional visualized model was acquired. The cylinder model was established to simulate axial images of the sacral nerve foramen. The angles of this cylinder in different conditions were measured and recorded. Results: A three-dimensional visualized model of the sacral nerve canal was successfully constructed, by which the space occupied and course of the sacral nerve canal were directly displayed. The angle between the anterior and posterior sacral nerve canals in the left sacrum 1 was 94.10°±3.72°, while on the right side it was 93.21°±4.19°. The angles between the vertical line and the cross-sectional plane in axial position of the left and right sacral nerve foramens were 26.27°±3.75° and 26.66°±2.65°, respectively. The angles between the vertical line and the sagittal plane in axial position of the left and right sacral nerve foramens were 46.24°±4.24° and 47.74°±5.32°, respectively. No significant differences were found (all P>0.05). Conclusions: A three-dimensional visualized model of the sacral nerve canal was established based on CT images using the Mimics software. This can reflect the morphologic features and course of the sacral nerve canal accurately, directly, and comprehensively.
Keywords: Sacral nerve canal, sacral fractures, computerized tomography, three-dimensional visualized model
Introduction
Sacral fractures have been reported to account for approximately 20%-30% of pelvic fractures, and 22%-60% of sacral fractures are accompanied by neurologic symptoms [1,2]. When the sacrum is subjected to strong violence, it easily fractures and loses symmetry, resulting in deformation and narrowing of the sacral foramen, sacral nerve compression, and further corresponding functional disorders [3].
In clinical practice, sacral fracture combined with sacral nerve injury is a common and serious trauma. Currently, surgery is still the main treatment method. Therefore, mastering the space occupation and course of the sacral nerve canal can enable doctors to have a more thorough understanding of the sacral nerve for surgeries such as sacral fracture fixation and sacral nerve decompression [4]. Currently, there are two methods for observing the course of the anterior and posterior branches of the sacral nerve within the sacral nerve canal: cadaver dissection and imaging anatomy. The sacral nerve canal is a sealed canal within the sacrum. If cadaver dissection is used to determine the exact position of the sacral nerve canal in the sacrum, it is necessary to perform operations such as dissection, observation, measurement, and casting of the sacral nerve canal, which undoubtedly increase the difficulty of experimental research [5]. The number of corpses used in such study was relatively large. Moreover, the sources of corpses were limited and the cost of corpses was relatively high, all of which affect the development of cadaver dissection research [6]. Computerized tomography (CT) workstations can perform three-dimensional reconstruction of the pelvis and sacrum, with clear reconstructed images which show the location and characteristics of fractures and display the shape of the sacral foramen. Whether bone blocks are embedded in the sacral foramen can be determined through layer scanning [7]. However, CT scan is mainly used to diagnose and observe surface conditions, and it is not an accurate reflection of the internal spaces and structural characteristics of the sacral nerve canal [8].
Thus, this study established a three-dimensional visualized digital model of the sacral nerve pathway in the sacrum, which is most prone to nerve damage in fractures, through the Materialise’s interactive medical image control system (Mimics) software. Mimics is a three-dimensional digital interactive medical image control system and a three-dimensional image generation and editing software developed by Materialise in Belgium. Mimics inputs various scanning data (such as CT and magnetic resonance imaging (MRI) data) and converts them into accurate three-dimensional digital models for anatomic teaching, surgical simulation, and finite element research. Mimics quickly converts scanning data into formats for computer-aided design (CAD) and finite element analysis (FEA). Then these data are output for rapid prototyping manufacturing (RPM), CAD, computer aided analysis (CAE), computer aided manufacturing (CAM), and FEA. Mimics can provide an efficient material allocation method based on grayscale values, which can accurately assign materials to three-dimensional models. The course of the sacral nerve canal pathway was observed and the angle between the anterior and posterior sacral nerve canals was measured. The three-dimensional visualized digital model was intuitive and easy to observe, helping surgeons deepen their understanding of the space occupation and course of the sacral nerve canal in the sacrum.
The aims of this study were as follows: (1) exploring the reconstruction and visualization methods of a three-dimensional digital model of the sacral nerve canal; (2) understanding the structure of the sacral nerve canal and the angle between the anterior and posterior sacral nerve canals in Sacrum 1 (S1), helping surgeons to enhance their understanding of the space occupied by the sacral nerve canal, and providing a basis for the diagnosis and treatment of sacral fractures and sacral nerve injuries; (3) enriching the clinical research methods by providing an effective reference for the projection angle of the sacral nerve canal during the surgery, and improving the accuracy of screw placement in sacral fracture and sacral nerve decompression surgeries.
Materials and methods
Subjects
This was a retrospective study. The image data of patients who underwent the scanning of sacral bones for physical examination in CT room of The Third Hospital of Hebei Medical University from May 2012 to October 2012 were collected. This study was approved by the Ethics Committee of The Third Hospital of Hebei Medical University (No. 2012-014). Inclusion criteria: (1) Patient’s age ranged from 18 to 65 years old; (2) Patients underwent the CT scanning using Siemens 64 slice spiral CT machine; (3) The scanning area should include lumbar vertebrae 5 (L5) to sacral vertebrae 2 (S2). Exclusion criteria: (1) The age was not between 18 and 65 years old; (2) Patients were diagnosed as having injuries such as sacral or sacroiliac joint fractures and dislocations; (3) Patients had concomitant diseases such as rheumatism, tuberculosis, tumors, and ankylosing spondylitis; (4) Patients had anatomical variations such as spina bifida and lumbosacral transitional vertebrae. According to the inclusion and exclusion criteria, a total of 20 patients were selected. The general information of these patients is shown in Table 1.
Table 1.
General information of patients in this study
| Data | Values |
|---|---|
| Subjects (Number) | 20 |
| Gender | |
| Male | 10 |
| Female | 10 |
| Age (years) | 44.0±2.6 |
| BMI (kg/m2) | 22.1±1.4 |
| Hypertension [Number (%)] | 4 (20%) |
| Diabetes mellitus [Number (%)] | 5 (25%) |
| Hyperlipidemia [Number (%)] | 4 (20%) |
Examination equipment
SIEMENS 64 slice spiral CT (SIEMENS, Germany), SIEMENS 64 slice spiral CT workstation, Picture Archiving and Communication Systems (PACS), personal PC hardware platform (CPU: Intel Pentium Duo Core E7500 2.93G. Motherboard chipset: Intel G41. Memory: 4096M, DDR2800MHz module. Hard disk: 500G. Graphics card: Intel GMA X4500, dynamic shared memory. Display: 19.0 inch of Samsung S19A330BW. Display performance: 1440 × 900 pixels), personal PC operating platform Windows XP, and a three-dimensional reconstruction visualization software Interactive Medical Image Control System Mimics 10.01 (Materialise, Belgium) were used.
Methods
Outcome measures
The main outcome measures included the angles between the anterior and posterior sacral nerve canals, the angles between the vertical line and the sagittal plane in axial position of the left sacral nerve foramen, and the angles between the vertical line and the cross-sectional plane in axial position of the left sacral nerve foramen. The secondary outcome measures included axial images of the sacral nerve foramen and the observations of the sacral nerve canal in the three-dimensional visualized model.
Scanning conditions
SIEMENS 64 slice spiral CT was applied for continuous scanning with a scanning angle of 0°. Scanning conditions were as follows: tube voltage: 120 kV, tube current: 150 mA, slice thickness: 5.0 mm, 512 × 512 matrix.
Data storage
The continuous cross-sectional CT images in the CT workstation were copied to compact disc in the form of DICOM. The complete CT image data from 20 patients were obtained.
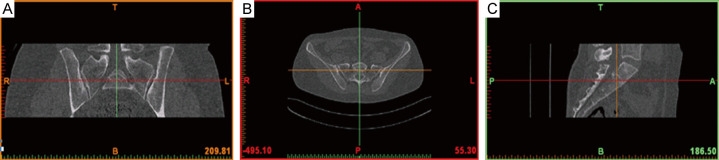
Importing cross-sectional images into the Mimics software
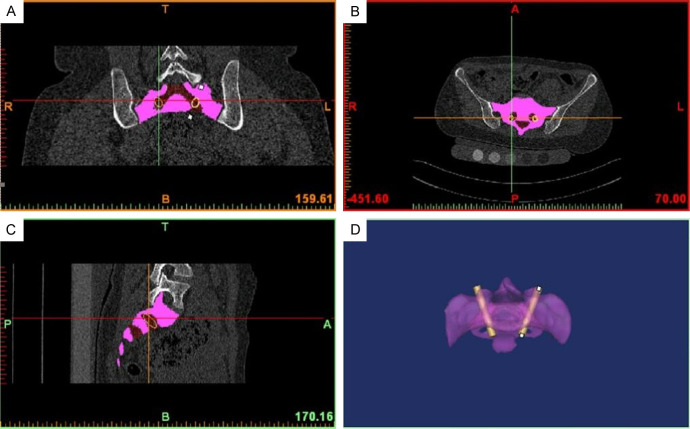
In a personal computer system, continuous cross-sectional pelvic images in the form of DICOM were imported into the Mimics software (version 10.01) [9]. The up and down, left and right, and front and back directions of the body position were defined, and then two-dimensional images of the cross-sectional, coronal, and sagittal planes were displayed, as shown in Figure 1.
Figure 1.
Determination of orientation of the two-dimensional image. A: The cross-sectional plane. B: The coronal plane. C: The sagittal plane.
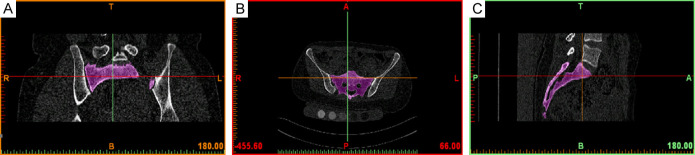
Image edition and hole processing
The “Thresholding” in the Segmentation Menu was adjusted [10]. A standard human bone threshold (CT value between 226-2498 Hu) was defined as the “Mask” range. The “Region Growth” tool was used to segment the bones. The “Edit Mask” was used to erase excessive structures such as bilateral sacroiliac joints and lumbar vertebrae, retaining only the sacrum. The images were edited and underwent hole processing, and then the irrelevant edge clutter and redundant data were deleted, as shown in Figure 2.
Figure 2.
Bilateral conjunction of the sacroiliac joint erased by the Edit Masks. A: The cross-sectional plane. B: The coronal plane. C: The sagittal plane.
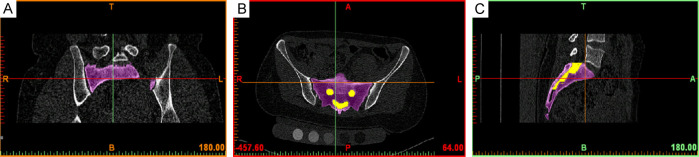
Drawing of the sacral nerve canal
The “Dynamic Region Growth” tool in the “Segmentation Menu” was selected to segment the bones, and the “Edit Masks” was used to draw the sacral nerve canal layer by layer, as shown in Figure 3.
Figure 3.
Rendering of the sacral nerve canal. A: The cross-sectional plane. B: The coronal plane. C: The sagittal plane.
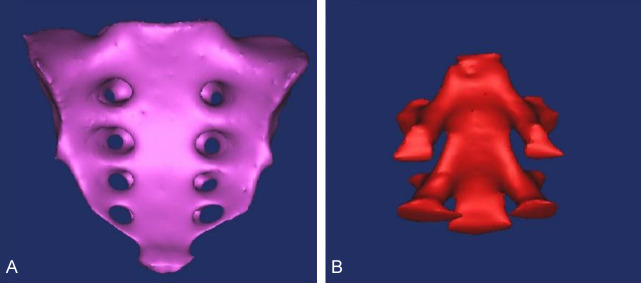
Reconstruction of the three-dimensional visualized model of the sacrum and sacral nerve canal
The “Calculate 3D from Masks” in the Segmentation Menu was used to select the corresponding mask, and the “Quality” was performed through the “Optimal*” calculation method. After running these settings, the three-dimensional model of the sacrum and sacral nerve canal were reconstructed, as shown in Figure 4.
Figure 4.
Three-dimensional reconstruction of the sacrum and sacral nerve canal. A: Sacrum. B: Sacral nerve canal.
Simulation of axial images of the sacral nerve foramen
The “Draw Cylinder” option in Med CAD was selected and a cylindrical model was established. The simulation was placed between the anterior and posterior foramens of the spinal nerve S1, as shown in Figure 5.
Figure 5.
Simulation of cylinder model. A: Cross-sectional plane. B: Coronal plane. C: Sagittal plane. D: Cylinder model.
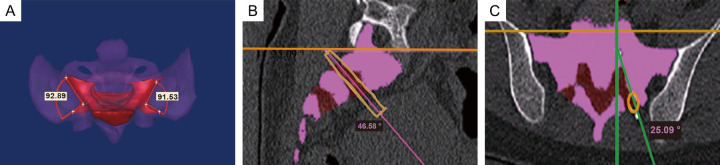
Record and measurement
In the tools of the Mimics software, the 3D angle measurement tool was selected. In the 3D visualized model of the sacral nerve canal, with the outer edge of the anterior and posterior foramens of the sacral nerve canal in the sacrum 1 as the reference, the angle between the anterior and posterior sacral nerve canals in the sacrum 1 was measured through the 3D method, as shown in Figure 6A. Using the perpendicular line of the scanning bed as a reference, the angles between the centerline of the simulated cylindrical model and the perpendicular line of the bed surface in both the sagittal and cross-sectional planes were measured, as shown in Figure 6B and 6C.
Figure 6.
Measurement of angles. A: Angles between the anterior and posterior sacral nerve canals. B: Angles in the sagittal plane. C: Angles in the cross-sectional plane.
Statistical analysis
SPSS software (version 13.0) was used to perform statistical analysis on the measured data. The measured data were presented as mean ± standard deviation. The counted data were presented as percentages/number. Normality tests were performed for all of the data. If the data conformed to a normal distribution, a paired t-test was conducted for comparison between the left and right sides. If the data did not conform to a normal distribution, non-parametric tests were conducted for comparison between the left and right sides. P<0.05 indicated a significant difference.
Results
Axial images of the sacral nerve foramen
The three-dimensional visualized model of the sacral nerve canal showed that the anterior and posterior sacral nerve canals were not completely regular straight canals, and the anterior sacral foramen was much larger than the posterior sacral foramen. Although the angles between the anterior and posterior sacral nerve canals were obvious, the cylindrical model could pass through the posterior sacral foramen directly from the inner side of the anterior sacral foramen. The occupation of the cylindrical model was adjusted layer by layer in the cross-sectional, coronal, and sagittal scanning images, so that the cylindrical model passed through the center of the posterior nerve foramen of the sacrum 1 anterogradely from the inner side of the anterior nerve foramen of the sacrum 1. This position was defined as the axis of the sacral nerve foramen, as shown in Figure 6.
Observation of the sacral nerve canal in the three-dimensional visualized model
A three-dimensional visualized model of the sacrum and sacral nerve canal was established, which intuitively displayed the occupation and course of the sacral nerve canal in the sacrum bone. The continuation of the sacral intervertebral foramen formed the anterior and posterior sacral nerve canals, which ran from the intervertebral foramen to the outer lower part of the anterior and posterior sacra, respectively, and were gradually expanded, forming a leaky bucket shape. The posterior sacral nerve canal had a shorter course and smaller diameter than the anterior sacral nerve canal.
Measurements of angles
As shown in Table 2, the angles between the anterior and posterior sacral nerve canals in the left sacrum 1 were 93.89°, 91.71°, 96.21°, 92.89°, 99.46°, 88.20°, 93.66°, 91.86°, 88.69°, 99.44°, 96.60°, 94.26°, 101.95°, 94.19°, 89.80°, 89.46°, 96.27°, 96.38°, 95.17°, and 91.84°, respectively, with an average value of 94.10°±3.72°. The angles between the anterior and posterior sacral nerve canals in the right sacrum 1 were 98.01°, 91.53°, 98.41°, 86.04°, 86.00°, 92.40°, 96.36°, 91.47°, 92.47°, 90.15°, 93.73°, 99.18°, 92.65°, 93.26°, 96.32°, 99.84°, 92.66°, 92.00°, 85.84°, and 95.92°, respectively, with an average value of 93.21°±4.19°. There were no statistically significant differences between the left and right sides. The angles between the vertical line and the sagittal plane in axial position of the left sacral nerve foramen were 49.52°, 43.19°, 45.94°, 46.94°, 46.45°, 37.55°, 52.85°, 44.07°, 44.08°, 43.09°, 38.55°, 51.00°, 48.95°, 52.47°, 41.45°, 48.41°, 46.58°, 51.09°, 47.60°, and 45.09°, respectively, with an average value of 46.24°±4.24°, and those in axial position of the right sacral nerve foramen were 39.08°, 49.09°, 51.55°, 50.39°, 54.41°, 50.31°, 51.26°, 52.14°, 43.48°, 53.13°, 39.96°, 56.60°, 44.28°, 46.89°, 49.82°, 37.31°, 50.15°, 44.99°, 42.20°, and 47.70°, respectively, with an average value of 47.74°±5.32°. No significant differences were found between the left and right sides. The angles between the vertical line and the cross-sectional plane in axial position of the left sacral nerve foramen were 19.04°, 27.95°, 20.80°, 31.69°, 27.50°, 23.27°, 28.94°, 26.20°, 27.65°, 33.93°, 22.61°, 24.93°, 25.82°, 26.15°, 24.69°, 22.10°, 26.32°, 25.09°, 31.84°, and 28.88°, respectively, with an average value of 26.27°±3.75°, and those in the axial position of the right sacral nerve foramen were 30.26°, 23.84°, 24.08°, 27.17°, 29.73°, 28.57°, 26.22°, 25.64°, and 24.78°, respectively, with an average value of 26.66°±2.65°. No significant differences were observed between the left and right sides.
Table 2.
Measurements of different angles in sacrum 1
| Subjects (Number) | Angle 1 | Angle 2 | Angle 3 | |
|---|---|---|---|---|
| Left side | N=20 | 94.10°±3.72° | 26.27°±3.75° | 46.24°±4.24° |
| Right side | N=20 | 93.21°±4.19° | 26.66°±2.65° | 47.74°±5.32° |
| t value | - | 0.623 | 0.341 | 0.969 |
| P value | - | 0.541 | 0.737 | 0.345 |
Note: Angle 1 referred to the angle between the anterior and posterior sacral nerve canals. Angle 2 referred to the angle between the vertical line and the cross-sectional plane in axial position of the left sacral nerve foramen. Angle 3 referred to the angle between the vertical line and the sagittal plane in axial position of the sacral nerve foramen.
Discussion
The sacral nerve canal is considered a sealed canal within the sacrum. Many discussions and clinical studies regarding surgical approaches have focused on how to avoid iatrogenic injury of the sacral nerve. Some studies reported that the incidence of intraoperative sacral nerve damage was 2%-18% [11]. Regardless of the surgical fixation methods, closed reduction or open reduction, it is particularly important to determine the safety zone and nerve course to avoid iatrogenic injury. Previous studies had mostly focused on establishing three-dimensional models of bone structures [12]. Contrary to most previous studies on the construction of three-dimensional models using CT workstations or dissection of the sacral nerve canal [13,14], this study established a three-dimensional visualized model of the sacral nerve canal through the CT thin layer scanning technology, direct reading of images in the format of Dicom, and application of the Mimics software. Mimics is a highly integrated and user-friendly three-dimensional image generation and editing software, which can input various scanning data such as CT and MRI, establish three-dimensional models for editing, and then output data in general formats for CAD, FEA, and rapid prototyping [15,16]. The large-scale conversion and processing operations for scanning data can be performed on a personal computer. This construction method based on CT images using the Mimics software has two advantages in contrast to previous methods: use of models with high precision and fast running speed [16,17], which were also observed in this study. Also, some studies reported that the method used in this study could generate raw data required for nearly prefect reconstruction, greatly reducing human error in the process of modeling and preventing the loss of raw data [18]. This method can read hundreds of images in a very short time, making the conversion of raw CT image data very fast, and eliminating the need for manual determination of node coordinates and other processing during modeling [19].
The space occupation and course of the sacral nerve canal are very important for surgical decompression for sacral nerve injury [20]. Percutaneous sacroiliac screw insertion, as the main treatment method for sacral fractures, has become widely used due to its good biomechanical stability and minimally invasive technique. However, improper placement, direction, or length of sacroiliac screws can lead to iatrogenic neurovascular or organ damage [21]. The anatomic and imaging studies on the safety of sacroiliac screw insertion were based on the fact that sacroiliac screws cannot enter the sacral nerve canal. The study on the relationship between the anterior sacral foramen and corresponding sacral nerve roots in sacrum bones [22] showed that from S1 to S4, the sacral nerve areas at the entrance of the sacral intervertebral foramen accounted for approximately 40%, 30%, 20%, and 15% of the anterior sacral foramen area, respectively. The sacral nerve areas at the outlet of the anterior sacral foramen accounted for 30%, 20%, 15%, and 15% of the anterior sacral foramen area, respectively. The shape of the entrance to the sacral intervertebral foramen was approximately oval, while that of the outlet was nearly circular. At the entrance to the sacral intervertebral foramen, the cross-sectional areas of the S2, S3, and S4 nerves accounted for approximately 70%, 25%, and 10% of the S1, while at the outlet of the anterior sacral foramen, they accounted for 75%, 30%, and 15% of the S1. Therefore, it can be inferred that the superior sacral nerve root is relatively more susceptible to injury during sacral fractures. In this study, the three-dimensional visualized model had good morphology and structure, both of which could be qualitatively and quantitatively observed. Moreover, this model had a realistic shape and obvious anatomic landmarks, realistically and vividly reflecting the spatial anatomic structure and relationships between various structures. It could be displayed in different colors and dynamically, and it also could be observed in multiple directions such as by zooming in, zooming out, and rotating. In this study, the self-contained measurement tools were allowed to perform two-dimensional measurements in the cross-sectional, sagittal, and coronal planes, as well as three-dimensional measurements of the reconstructed model. The digital reconstruction could intuitively and accurately reflect the structural characteristics of the sacrum and sacral nerve canals. This study not only established a three-dimensional visualized model of the sacral nerve canal, enabling clinical doctors to understand the course of the sacral nerve, but also measured the angels between axial position of the sacral nerve foramen (S1) and perpendicular line of the scanning bed surface through simulation of the cylinder model, guiding the projection angle of the C-arm bulb tube. The clinical significances of this study lies in reducing the omission of clinical diagnosis of sacral fractures combined with sacral nerve injury, strengthening the in-depth research regarding the concept of minimally invasive surgery, and fostering safer and more scientific surgical design, which are similar to other studies [23,24].
There were some limitations in this study. First, although the three-dimensional reconstruction and visualization of the sacrum and sacral nerve canal were performed and the course and angle of the sacral nerve canal in sacrum 1 were described and observed, the study results should be further used to simulate surgery through auxiliary design tools (CAD) and other software and then verified by cadaver dissection to gradually improve the preoperative design, so as to greatly improve the safety and surgical implementation of this technology. Second, measurement was performed on the axial position of the sacral nerve foramen, but an effective clinical radiological verification was not conducted, which should be further investigated in future studies. Third, the establishment of this model and the measurement of test indicators were all manually operated by one person alone, which might introduce subjectivity. Fourth, the number of patients in this study was relatively small, and the study results should be confirmed byfurther research using larger sample sizes to obtain more accurate reference values.
In summary, the three-dimensional visualized model of the sacral nerve canal was firstly established through the Mimics software, which had the physical characteristics of a real object, and comprehensively, accurately, and intuitively reflected the morphological characteristics of the sacral nerve canal, with high authenticity. By measuring the angles between the anterior and posterior sacral nerve canals, as well as between the perpendicular line of bed surface and the axial image of the sacral nerve foramen in the sagittal and cross-sectional planes, it helps surgeons to understand the space occupation and course of the sacral nerve canals in clinical practice. The perspective angle of the sacral nerve foramen in axial images is also proposed to improve the accuracy of operations such as sacral fracture screw insertion and sacral nerve decompression surgery.
Disclosure of conflict of interest
None.
References
- 1.Barber LA, Katsuura Y, Qureshi S. Sacral fractures: a review. HSS J. 2023;19:234–246. doi: 10.1177/15563316221129607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gutierrez-Gomez S, Wahl L, Blecher R, Olewnik L, Iwanaga J, Maulucci CM, Dumont AS, Tubbs RS. Sacral fractures: an updated and comprehensive review. Injury. 2021;52:366–375. doi: 10.1016/j.injury.2020.11.015. [DOI] [PubMed] [Google Scholar]
- 3.Chandra V, Wajswol E, Shukla P, Contractor S, Kumar A. Safety and efficacy of sacroplasty for sacral fractures: a systematic review and meta-analysis. J Vasc Interv Radiol. 2019;30:1845–1854. doi: 10.1016/j.jvir.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Li J, Yu XK, Dong XM, Guo L, Li XF, Tian W. The clinical value of using magnetic resonance contrast-enhanced three-dimensional nerve view in the diagnosis and management of sacral fracture accompanied by sacral plexus injury. Technol Health Care. 2022;30:1407–1415. doi: 10.3233/THC-213543. [DOI] [PubMed] [Google Scholar]
- 5.Zhu L, Zhou ZB, Shen D, Chen AM. Ipsilateral S2 nerve root transfer to pudendal nerve for restoration of external anal and urethral sphincter function: an anatomical study. Sci Rep. 2019;9:13993. doi: 10.1038/s41598-019-50484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuruc R, Haviarova Z, Halgas F, Sidlo J, Matejcik V. Extraordinary features of the intraspinal extradural and intradural nerve root courses. Neuro Endocrinol Lett. 2019;40:29–36. [PubMed] [Google Scholar]
- 7.Suzuki N, Kotani T, Sunami T, Sakashita K, Okuwaki S, Ohyama S, Iwata S, Iijima Y, Sakuma T, Akazawa T, Inage K, Shiga Y, Minami S, Ohtori S. Anatomical analysis of the S1 neural foramen using three-dimensional computed tomography imaging: insights for effective S1 nerve root block. World Neurosurg. 2024;181:e459–e467. doi: 10.1016/j.wneu.2023.10.082. [DOI] [PubMed] [Google Scholar]
- 8.Kamran H, Bitaraf M, Tanhaeivash R, Kajbafzadeh AM. Three-dimensional computed tomography scan of the pelvic bone in isolated epispadias: analysis before surgical correction. Urology. 2023;180:235–241. doi: 10.1016/j.urology.2023.05.050. [DOI] [PubMed] [Google Scholar]
- 9.Li J, Zhao LJ, Zheng MZ, Gan KF, Chen YL, Feng ZX, Pan LX, Xu JX, Fan TD, Chen JY, Zhao FD. Comparative study between 3D guide plate assisted and free-hand insertion of anterior cervical transpedicular screw. Zhongguo Gu Shang. 2021;34:45–50. doi: 10.12200/j.issn.1003-0034.2021.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Nasrulloh AV, Wilson I, Geenen C, Habib M, Obara B, Steel DHW. Macular hole morphology and measurement using an automated three-dimensional image segmentation algorithm. BMJ Open Ophthalmol. 2020;5:e000404. doi: 10.1136/bmjophth-2019-000404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu T, Cheng XL, Qu Y, Dong RP, Kang MY, Zhao JW. Computer navigation-assisted minimally invasive percutaneous screw placement for pelvic fractures. World J Clin Cases. 2020;8:2464–2472. doi: 10.12998/wjcc.v8.i12.2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W, Han J, Xin Q, Liu Q, Feng C, Liu Y, Zhang D. Finite element mechanical analysis of ipsilateral approach and contralateral approach in unilateral bilateral endoscopic spine surgery. J Orthop Surg Res. 2023;18:979. doi: 10.1186/s13018-023-04476-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steinke H, Saito T, Kuehner J, Reibetanz U, Heyde CE, Itoh M, Voelker A. Sacroiliac innervation. Eur Spine J. 2022;31:2831–2843. doi: 10.1007/s00586-022-07353-1. [DOI] [PubMed] [Google Scholar]
- 14.Agarwal P, Nivasarkar S, Agrawal N, Bajaj J, Parihar V, Yadav YR, Sharma D. Cadaveric study to assess the feasibility of S1 neurectomy and contralateral S1 transfer for spastic hemiparesis. J Orthop. 2022;31:99–102. doi: 10.1016/j.jor.2022.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.You YH, Zhao D, Huang QB, Lu JZ. Application of Mimics Medical 21.0 Software in thoracoscopic anatomical sublobectomy. Minerva Surg. 2022;77:221–228. doi: 10.23736/S2724-5691.21.08927-9. [DOI] [PubMed] [Google Scholar]
- 16.Sheikhi M, Haghighat A, Lourizadeh N, Tavangar H, Aryaee P. Evaluation of the effect of direct sinus lift surgery on maxillary sinus volume by Mimics software. Natl J Maxillofac Surg. 2023;14:198–207. doi: 10.4103/njms.njms_155_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang C, Song C, Wang D, Gao T, Li J, Yang D, Liu C, Du Y, Zhang K. Digitally driven surgical guide planning. J Clin Pediatr Dent. 2024;48:128–137. doi: 10.22514/jocpd.2024.014. [DOI] [PubMed] [Google Scholar]
- 18.Rahmatian M, Jafari Z, Moghaddam KN, Dianat O, Kazemi A. Finite element analysis of fracture resistance of mandibular molars with different access cavity designs. J Endod. 2023;49:1690–1697. doi: 10.1016/j.joen.2023.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Nair GR, Senthil Kumar MS. Evaluation of orbital volume in unilateral orbital fracture using computed tomography. Natl J Maxillofac Surg. 2022;13:223–228. doi: 10.4103/njms.njms_379_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Li S, Wang Y, Shang A. Functional, morphological and molecular characteristics in a novel rat model of spinal sacral nerve injury-surgical approach, pathological process and clinical relevance. Sci Rep. 2022;12:10026. doi: 10.1038/s41598-022-13254-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han X, Cao Z, Zhao K, Sun Z, Ma Y, Yin Q. Optimal insertion positions of anterior-posterior orientation sacroiliac screw. Eur Spine J. 2023;32:1383–1392. doi: 10.1007/s00586-023-07568-w. [DOI] [PubMed] [Google Scholar]
- 22.Hendrickson WK, Amundsen CL. Sacral neuromodulation: sacral anatomy and optimal lead placement. Int Urogynecol J. 2021;32:2545–2547. doi: 10.1007/s00192-020-04615-8. [DOI] [PubMed] [Google Scholar]
- 23.Gu Y, Lv T, Jiang C, Lv J. Neuromodulation of the pudendal nerve assisted by 3D printed: a new method of neuromodulation for lower urinary tract dysfunction. Front Neurosci. 2021;15:619672. doi: 10.3389/fnins.2021.619672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu Z, Jiang Y, Mu W, Li W, Zhang G, Jiang S, Xu P. Electrophysiological, biomechanical, and finite element analysis study of sacral nerve injury caused by sacral fracture. Front Bioeng Biotechnol. 2022;10:920991. doi: 10.3389/fbioe.2022.920991. [DOI] [PMC free article] [PubMed] [Google Scholar]