Abstract
Objective: To explore whether there are correlations between loneliness, disease uncertainty, and perceived social support among elderly patients with digestive tract tumors. Method: A cross-sectional study was conducted on 149 patients with digestive tract tumors. A general information questionnaire, the Chinese version of the Cancer Patient Loneliness Scale, the Disease Uncertainty Scale, and the Perceived Social Support Assessment Scale were used. Results: The mean score on the Cancer Patient Loneliness Scale was 31.22±2.62 points; the mean score on the Disease Uncertainty Scale was 135.06±8.15 points; and the mean score on the Perceived Social Support Scale was 59.69±5.96 points. There was a positive correlation between loneliness and disease uncertainty (r=0.745, P<0.001), and there was a negative correlation between loneliness and perceived social support (r=-0.494, P<0.001). Conclusion: Disease uncertainty and social support directly predicted loneliness among elderly patients with digestive tract tumors. Social support partially mediated the relationship between loneliness and disease uncertainty, accounting for 57.20% of the total effect. Clinical medical staff need to devote more attention to elderly patients being treated for digestive tract tumors, and psychological interventions should be implemented to enhance social support from society and families, thereby reducing patients’ feelings of loneliness.
Keywords: Elderly digestive tract tumors, loneliness, illness, uncertainty, understanding, social support
Introduction
Recent studies have shown that the prevalence of elderly people experiencing symptoms of loneliness and anxiety is 38%, and the prevalence of elderly people experiencing depressive symptoms is 41% [1]. Loneliness is an unpleasant emotional experience that occurs naturally or is a subjective feeling that occurs due to insufficient social relationships. Loneliness is a common psychological problem among elderly people and has become a serious public health problem as well as a social problem. Psychological health issues such as loneliness and depression have gradually become important factors affecting the quality of life, happiness, social security and stability of elderly people.
According to the latest data from the International Agency for Research on Cancer, the number of new cancer cases worldwide reached 19.29 million in 2020; furthermore, the incidence rate of malignant digestive tract tumors among elderly people was expected to increase annually, and the incidence rate and mortality rate of digestive tract tumors were expected to rank among the top 10 worldwide [2]. As China gradually becomes an aging society, the incidence rate of cancer has increased, and malignant tumors have become a serious threat to the physical and mental health of Chinese residents. Gastrointestinal tumors, including liver cancer, gastric cancer, esophageal cancer, pancreatic cancer and colorectal cancer, are common malignant tumors in China and have high incidence rates and poor prognoses [3]. The series of adverse conditions experienced by elderly patients with malignant tumors, such as protective isolation, changes in body image, and stigmatization, can all induce feelings of loneliness among patients [4]. There are many clinical treatment methods for cancer, including surgery, radiotherapy, chemotherapy, molecular targeting, and immunotherapy. However, patients receiving treatment may experience feelings of loneliness and anxiety due to uncertainty related to treatment cycles, plans, and family and social support, thereby affecting the efficacy and outcomes of treatment. Previous research on patients with malignant tumors has mostly focused on anxiety, depression, fear, etc., and there has been a lack of attention devoted to loneliness [5]. Therefore, it is crucial to examine loneliness among elderly patients with digestive tract tumors.
Disease uncertainty refers to an emotion induced by a patient’s lack of understanding regarding disease-related issues, treatment and nursing measures, and disease outcomes [6]. Disease uncertainty can cause negative emotions such as loneliness and anxiety, thereby reducing patients’ psychological adaptability, decreasing their quality of life and seriously affecting their disease treatment progress and rehabilitation outcomes [7]. Since the 1980s, foreign countries have focused on exploring disease uncertainty. Previous investigations mainly focused on acute disease patients; however, after the 1990s, disease uncertainty among patients with malignant tumors could no longer be ignored [8].
Perceived social support refers to an individual’s subjective emotional experience and satisfaction regarding support and understanding from society [9]. Higher levels of social support can enhance a patient’s level of family intimacy and adaptability, this enabling the patients to experience more successful treatments and improving their self-efficacy [10]. Moreover, social support helps patients to engage in self-reflection; improve various unhealthy lifestyles; actively regulate their own thinking; practice emotional communication; improve daily life behaviors; reduce excessive stress reactions; and further enhance their immune function. Research by British scholar LeatM et al. [11] revealed that when medical staff provided more medical information-related support and emotional assistance to hospitalized malignant tumor patients, the patients exhibited benefits in terms of higher quality of life. The information and resources provided by medical staff (including information about tumor prevention and treatment, social psychology, etc.) are important sources of support to help malignant tumor patients survive long treatment cycles and to ensure their quality of life.
A review of the literature revealed that there is a lack of research on the correlation between loneliness, disease uncertainty, and perceived social support among elderly patients with digestive tract tumors. The aims of this study were to analyze the correlations among these three factors and to explore how social support can provide a basis for medical staff to alleviate disease uncertainty among elderly patients with digestive tract tumors, thereby improving patients’ loneliness and other types of stress and providing a reference for clinical intervention, disease diagnosis and disease treatment.
Data and methods
Research subjects
Convenience sampling was used to recruit 150 elderly patients with digestive tract tumors who were admitted to the Oncology Department of Anhui Zhongke Gengjiu Hospital from November 2023 to April 2024, including 103 males and 47 females. The patients were aged between 65 and 99 years, including 32 patients diagnosed with liver malignancy, 25 patients diagnosed with gastric malignancy, 26 patients diagnosed with esophageal malignancy, 54 patients diagnosed with colorectal malignancy, 11 patients diagnosed with pancreatic malignancy, and 2 patients diagnosed with gallbladder malignancy. The general and clinical information of patients was collected, and statistical analysis was conducted to examine the data. Informed consent was obtained from all participants.
Inclusion criteria
The inclusion criteria were as follows: (1) aged ≥65 years [12]; (2) diagnosed with digestive tract tumors via pathology, imaging, or other special auxiliary examinations; (3) underwent antitumor treatment; and (4) had clear thinking, good communication skills, could understand the content of the scale, and voluntarily agreed to participate in the study.
Exclusion criteria
The exclusion criteria were as follows: (1) patients who were critically ill or have other urgent and severe conditions that make it impossible to conduct a questionnaire survey; (2) patients who were diagnosed with non-gastrointestinal malignant tumors; (3) individuals with a history of mental illness or cognitive impairment who were unable to cooperate in completing this survey; and (4) patients who were taking anti-anxiety and depression medication.
Ethical statement
This study was approved by the hospital’s medical ethics committee, with ethics approval number Geng Medical Ethics Review Approval [2024] No. 21.
Sample size calculation
According to the simple formula for calculating sample size in the pilot study [13], the sample size should be equal to 5-10 times the number of variables. This survey included 26 variables, and thus, the sample size should have been between 130 and 260. A total of 150 questionnaires were distributed, and 149 were collected and found to be valid, thus yielding an effective rate of 99.33%.
Research tools
General and clinical data survey questionnaire
The researcher designed a questionnaire to assess general and clinical data. The general information included sex, age, occupation, smoking and drinking history, educational level, marital and child status, beliefs, monthly family income, and medical insurance settlement method. The clinical data included the patient’s diagnosis, knowledge about the condition, treatment methods, duration of illness, and TNM clinical stage.
Cancer Loneliness Scale (CLS)
The Cancer Loneliness Scale (CLS) was developed by Professor Adams in 2017 to assess loneliness among cancer patients. The CLS includes 7 items, with each item scored on a 5-point Likert scale. Scores of 1, 2, 3, 4, and 5 corresponded to “never”, “rarely”, “sometimes”, “often”, and “always”, respectively. Total scores on the CLS range from 7-35 points. Higher scores indicated more severe levels of loneliness. Scores ranging from 5-14 indicated low levels of loneliness, scores ranging from 15-27 indicated moderate levels of loneliness, and scores ranging from 28-35 indicated high levels of loneliness. The Cronbach alpha coefficient of the CLS was 0.94, indicating excellent internal consistency. The Chinese scholar Cui Haijuan translated this scale into Chinese in 2018, and the Cronbach alpha coefficient of the Chinese version of the CLS was 0.912. The Chinese version of the scale showed good reliability and validity.
Mishel’s Uncertainty in Illness Scale (MUISA)
The Mishel’s Uncertainty in Illness Scale (MUIS-A) is a self-report scale developed by the American nursing expert Professor Mishel in 1988. The Taiwanese researcher Xu Shulian et al. translated the MUIS-A [14] into Chinese and used it to measure the level of disease uncertainty in Chinese patients. The Chinese version of the MUIS-A exhibited good reliability and validity. The MUIS-A includes 33 items across four dimensions: uncertainty 13 items), complexity (8 items), information deficiency (7 items), and unpredictability (5 items). Each item is scored using a 5-point Likert scale. Scores of 1, 2, 3, 4, and 5 correspond to responses of “strongly disagree”, “disagree”, “unclear”, “agree”, and “strongly agree”, respectively. Items 6, 7, 10, 12, 20, 24, 26, 27, 29, 30, 31, and 32 are reverse-scored. The total score on the MUIS-A ranges from 33 to 165 points. A score ranging from 33-74 indicates a low level of disease uncertainty, a score ranging from 75-117 indicates a moderate level of disease uncertainty, and a score ranging from 118-165 indicates a high level of disease uncertainty. Therefore, higher scores indicate higher levels of disease uncertainty. The content validity of this scale is 0.86.
Perceived Social Support Scale (PSSS)
The Perceived Social Support Scale (PSSS) was developed by Zimet et al. [15] in 1988 and was translated into Chinese by Huang Li et al. The PSSS includes 12 items across three dimensions: family support, friend support, and other support. Each item is scores on a 7-point Likert scale ranging from 1 to 7 (“strongly disagree”, “strongly disagree”, “slightly disagree”, “neutral”, “slightly agree”, “strongly agree”, respectively). The total score ranges from 12 to 84 points. Scores of 36 points or below indicate a low level of social support; scores ranging from 37-60 points indicate a moderate level; of social support, and scores ≥61 points indicate a high level of social support. Therefore, higher scores indicate higher levels of perceived social support. The Cronbach alpha coefficient of the PSSS was 0.84.
Statistical methods
The survey data were analyzed via SPSSPRO statistical software. Descriptive statistics: Categorical data, such as general and clinical data, are expressed as frequencies and percentages. The Shapiro-Wilk test was used to examine the normality of the distributions of continuous variables such as disease uncertainty and perceived social support. The normality of the distributions were represented by X Ω±s. The scores on the CLS were found to be nonnormally distributed; however, the histogram basically showed a bell shape. Moreover, the coefficient of variation (cv) of the CLS was 0.084, which was less than 0.15, indicating a low probability of outliers in the current data. Therefore, the mean was used for descriptive analysis [16]. Nonparametric tests: For univariate analysis of elderly patients with gastrointestinal malignancies, the Mann-Whitney U test and Kruskal-Wallis H test were performed on binary and multiple independent variables, respectively. Generalized linear regression analysis was used to examine the impact of general and clinical characteristics on loneliness among elderly patients with gastrointestinal malignancies. Spearman’s correlation analysis was used to examine the correlations of loneliness with disease uncertainty and its four dimensions as well as with perceived social support and its three dimensions. P<0.05 or P<0.001 indicated statistical significance. Structural equation modeling was used to examine the mediating effect of perceived social support on the relationship between loneliness and disease uncertainty.
Results
General information and clinical data of patients
A total of 149 valid questionnaires were collected, thus yielding an effective response rate of 99.33%. The average age was 71.71±6.94 years, with 66 patients (44.30%) aged 65-69 years, 65 patients (43.62%) aged 70-79 years, 14 (9.40%) aged 80-89 years, and 4 (2.68%) aged ≥90 years. There were 102 males (68.46%) and 47 females (31.54%). Regarding medical insurance payment methods, 38 patients (25.51%) used provincial and municipal medical insurance, 103 patients (69.13%) used resident medical insurance, and 8 patients (5.36%) used self-funded medical insurance. Regarding disease treatment methods, 27 patients used one type (chemotherapy or radiotherapy) (18.12%), 101 patients used two types (chemotherapy + radiotherapy, chemotherapy + immunotherapy or targeted therapy) (67.79%), and 21 patients used three types (chemotherapy or radiotherapy + immunotherapy or targeted therapy) (67.79%). Regarding TNM clinical staging, 31 patients (20.81%) were in clinical stage I, 90 patients (60.40%) were in clinical stage II, and 28 patients (18.79%) were in clinical stage III. For specific details, please refer to Table 1.
Table 1.
General information on loneliness in elderly patients with digestive tract tumors: univariate analysis (n=149)
| Project | Number of cases | Percentage (%) | Loneliness score (x̅±S) | P | Cohen’s f/d |
|---|---|---|---|---|---|
| Age | 0.599 | 0.253 | |||
| 65-69 | 66 | 44.30 | 31.34±2.66 | ||
| 70-79 | 65 | 43.62 | 31.11±2.67 | ||
| 80-89 | 14 | 9.40 | 30.71±2.23 | ||
| ≥90 | 4 | 2.68 | 32.5±1.91 | ||
| Gender | 0.324 | 0.209* | |||
| Male | 102 | 68.46 | 31.04±2.70 | ||
| Female | 47 | 31.54 | 31.59±2.40 | ||
| Place of residence | 0.001 | 0.051 | |||
| Rural area | 61 | 40.94 | 32.39±2.20 | ||
| Town | 50 | 33.55 | 30.36±2.37 | ||
| City | 38 | 25.51 | 30.47±2.87 | ||
| Degree of education | 0.543 | 0.054 | |||
| Elementary school and below | 61 | 40.94 | 31.39±2.60 | ||
| Middle school | 44 | 29.53 | 31.20±2.31 | ||
| High school And vocational school | 33 | 22.14 | 31.03±3.14 | ||
| Junior college | 6 | 4.03 | 31.33±2.87 | ||
| Bachelor degree or above | 5 | 3.36 | 30.04±1.81 | ||
| Monthly Household income | 0.001 | 0.152 | |||
| <5000 yuan | 31 | 20.81 | 34.29±0.73 | ||
| 5000-10000 yuan | 90 | 60.40 | 31.3±1.78 | ||
| >10000 yuan | 28 | 18.79 | 27.57±1.31 | ||
| Marriage and child status | 0.001 | 0.137 | |||
| Married | 116 | 77.85 | 30.58±2.52 | ||
| Lose a spouse | 30 | 18.87 | 32.8±2.06 | ||
| Divorced | 3 | 3.28 | 33.33±0.58 | ||
| No children | 5 | 3.36 | 34.60±0.54 | ||
| Having children | 144 | 96.64 | 30.10±2.58 | ||
| Career | 0.978 | 0.003 | |||
| Farmer | 61 | 40.94 | 31.29±2.62 | ||
| Retire | 38 | 25.51 | 31.16±2.84 | ||
| Liberal professions | 50 | 33.55 | 31.22±2.50 | ||
| Payment Method | 0.001 | 0.128 | |||
| Employee medical insurance | 38 | 25.51 | 31.24±2.73 | ||
| Resident medical insurance | 103 | 69.13 | 30.84±2.40 | ||
| Self-funded | 8 | 5.36 | 35 | ||
| Belief | 0.608 | 0.049* | |||
| Have | 26 | 17.45 | 31.11±2.30 | ||
| Not have | 123 | 82.55 | 31.24±2.69 | ||
| Smoke | 0.348 | 0.204* | |||
| Have | 101 | 67.79 | 31.05±2.72 | ||
| Not have | 48 | 32.21 | 31.58±2.37 | ||
| Drink alcohol | 0.172 | 0.266* | |||
| Have | 92 | 61.74 | 31.95±2.77 | ||
| Not have | 57 | 38.26 | 31.64±2.32 | ||
| Disease diagnosis | 0.522 | 0.121 | |||
| Rectal malignant tumor | 30 | 20.13 | 31.1±2.72 | ||
| Colon malignant tumor | 23 | 15.43 | 31.39±2.19 | ||
| Gastric malignant tumor | 25 | 16.78 | 30.76±2.60 | ||
| Esophageal malignant tumor | 26 | 17.45 | 31.27±2.37 | ||
| Pancreatic malignant tumor | 11 | 7.38 | 31.45±3.32 | ||
| Liver malignant tumor | 32 | 21.48 | 31.68±2.76 | ||
| Gallbladder malignant tumor | 2 | 1.35 | 27.5±0.71 | ||
| Disease duration | 0.001 | 0.097 | |||
| <6 months | 59 | 39.60 | 29.38±2.58 | ||
| 6-12 months | 32 | 21.48 | 33.41±1.32 | ||
| 1-3 years | 30 | 20.13 | 32.33±1.79 | ||
| >3 years | 28 | 18.79 | 31.39±1.85 | ||
| Treatment methods | 0.528 | 0.021 | |||
| 1 type | 27 | 18.12 | 30.62±2.73 | ||
| 2 types | 101 | 67.79 | 31.32±2.58 | ||
| 3 types | 21 | 13.99 | 31.47±2.66 | ||
| Disease informed status | 0.001 | 0.141 | |||
| Completely unaware | 30 | 20.13 | 27.53±1.36 | ||
| Partially informed | 60 | 40.26 | 30.70±1.41 | ||
| Fully informed | 59 | 39.61 | 33.62±1.16 | ||
| TNM Clinical stages | 0.001 | 0.141 | |||
| Clinical stages I | 31 | 20.81 | 27.81±1.76 | ||
| Clinical stages II | 90 | 60.40 | 31.51±1.87 | ||
| Clinical stages III | 28 | 18.79 | 34.07±0.72 |
Cohen’s f/d.
Loneliness
The mean score on the CLS was 31.22±2.62 points, which indicates a high level of loneliness. There were 133 patients (89.26%) with high levels of loneliness and 16 patients (20.74%) with moderate levels of loneliness, as shown in Table 1.
Disease uncertainty
The mean score on the MUIS-A was 135.06±8.15 points, which indicated a high level of disease uncertainty. A total of 148 patients (99.33%) had a high level of disease uncertainty, whereas only 1 patient (0.67%) had a moderate level of disease uncertainty. See Table 2 for details.
Table 2.
Disease uncertainty and dimension scores of elderly patients with digestive tract malignant tumors (n=149)
| Project | Number of entries | Score (x̅±S) |
|---|---|---|
| Disease uncertainty | 33 | 135.06±8.15 |
| Ambiguity | 13 | 58.60±5.07 |
| Complexity | 7 | 27.49±2.84 |
| Inconsistency | 7 | 23.48±2.22 |
| Unpredictability | 6 | 25.03±2.17 |
Perceived social support
The mean score on the PSSS was 59.69±5.96 points, which indicates a moderate level of perceived social support. A total of 83 patients had a moderate level of perceived social support (55.70%), while 66 patients had a high level of perceived social support (44.30%). See Table 3 for details.
Table 3.
Perceived social support and dimension scores of elderly patients with gastrointestinal malignant tumors (n=149)
| Project | Number of entries | Score (x̅±S) |
|---|---|---|
| Perceived social support | 12 | 59.69±5.9 |
| Family support | 4 | 23.74±2.38 |
| Friend support | 4 | 18.21±2.39 |
| Other support | 4 | 17.99±2.34 |
Univariate analysis of loneliness
Univariate analysis was conducted with age, sex, place of residence, educational level, monthly family income, marital and child status, occupation, medical insurance payment method, religious beliefs, smoking history, alcohol consumption history, disease diagnosis, disease duration, treatment method, disease awareness, and TNM clinical stage as the independent variables and scores on the CLS as the dependent variable. The analysis revealed that marital and child status, family income, medical insurance payment method, duration of illness, place of residence, disease awareness, and TNM clinical stage were the main factors influencing loneliness (P<0.05). See Table 1 for details.
Multivariate analysis of loneliness
Multiple regression analysis was also conducted. The variables that were significant in the univariate analysis were entered in to the multiple regression model as predictors: the patient’s marital and child status, place of residence, family income, medical insurance payment method, duration of illness, disease awareness, and TNM clinical stage of the tumor. The dependent variable was the total score on the CLS. Each variable was assigned as follows: marital status: married, with children = 0, widowed, divorced = 1, no children = 2; monthly household income: >10000 yuan = 0, 5000-10000 yuan = 1, <5000 yuan = 2; medical insurance payment method: resident medical insurance = 0, provincial and municipal employee medical insurance = 1, self-funded = 2; disease duration: <6 months = 0, >3 years = 1, 1-3 years = 2, 6-12 months = 3; disease awareness: completely unaware = 0, partially aware = 1, completely aware = 2; TNM clinical staging of tumors: clinical stage I = 0, clinical stage II = 1, clinical stage III = 2; residence: urban = 0, urban = 1, rural = 2.
To examine the outcomes of the generalized linear regression model and to avoid the influence of multicollinearity on the model, an omnibus test was used to test the collinearity of the independent variables. The likelihood ratio chi square value range for this study was 276.075, with 7 degree of freedom and P<0.001, thus indicating the effectiveness of the applied model. The results revealed that marital and child status, family income, medical insurance payment method, duration of illness, disease awareness, and TNM clinical staging were significant predictors of loneliness among elderly patients with digestive tract tumors (P<0.05), whereas place of residence was not a significant predictor (P>0.05). See Table 4 for details.
Table 4.
Multivariate analysis of loneliness in elderly patients with digestive tract tumors during treatment (n=149)
| Parameter | Coefficient | Standard error | Wald value | P value | Lower limit of 95% confidence interval | Upper limit of 95% confidence interval |
|---|---|---|---|---|---|---|
| Constant | 27.0999 | 0.187 | 20932.854 | 0.001 | 26.732 | 27.466 |
| Monthly household income | 0.91 | 0.25 | 13.301 | 0.001 | 0.421 | 1.399 |
| Disease awareness | 1.728 | 0.202 | 73.039 | 0.001 | 1.332 | 2.124 |
| Disease duration | 0.216 | 0.094 | 5.282 | 0.022 | 0.032 | 0.4 |
| Marriage and child Status | 0.394 | 0.191 | 4.247 | 0.039 | 0.019 | 0.768 |
| Place of residence | 0.047 | 0.114 | 0.171 | 0.679 | 0.271 | 0.177 |
| Payment Method | 0.305 | 0.155 | 3.873 | 0.049 | 0.001 | 0.608 |
| TNM stages | 0.704 | 0.217 | 10.539 | 0.001 | 0.279 | 1.129 |
Correlation analysis of loneliness, disease uncertainty, and perceived social support
Spearman’s correlation analysis revealed that scores on the CLS were positively correlated with total scores on the MUIS-A as well as scores of its four dimensions (the r values were all positive, indicating positive correlations). Specifically, the correlation of CLS scores with the MUIS-A total score, the uncertainty dimension, the complexity of the disease dimension, and the unpredictability dimension were significant at P<0.001. Scores on the CLS were significantly negatively correlated with the total score of the PSS as well as scores on its four dimensions (the r values were all negative, indicating negative correlations) (P<0.001). See Table 5 for details.
Table 5.
Correlation analysis of loneliness, disease uncertainty, and perceived social support in elderly patients with digestive tract tumors (n=149)
| Project | Loneliness | uncertainty | Ambiguity | Complexity | Inconsistency | Unpredictability | Social support | Family support | Friend support | Other support |
|---|---|---|---|---|---|---|---|---|---|---|
| Loneliness | 1 | |||||||||
| Uncertainty | 0.745*** | 1 | ||||||||
| Ambiguity | 0.647*** | 0.792*** | 1 | |||||||
| Complexity | 0.57 *** | 0.704*** | 0.556*** | 1 | ||||||
| Inconsistency | 0.256** | 0.41*** | 0.071* | 0.054* | 1 | |||||
| Unpredictability | 0.215** | 0.464*** | 0.112* | 0.155** | 0.351*** | 1 | ||||
| Social support | -0.494*** | -0.407*** | -0.44*** | -0.328*** | -0.048* | -0.073* | 1 | |||
| Family support | -0.384*** | -0.311*** | -0.295*** | -0.253** | -0.038* | -0.085* | 0.79*** | 1 | ||
| Friend support | -0.416*** | -0.302*** | -0.365*** | -0.295*** | -0.048* | -0.008* | 0.834*** | 0.554*** | 1 | |
| Other support | -0.395*** | -0.361*** | -0.394*** | -0.216** | -0.114* | -0.118* | 0.772*** | 0.448*** | 0.572*** | 1 |
P<0.001;
P<0.05;
P>0.05.
Analysis of the mediating effect of perceived social support on the relationship between loneliness and disease uncertainty
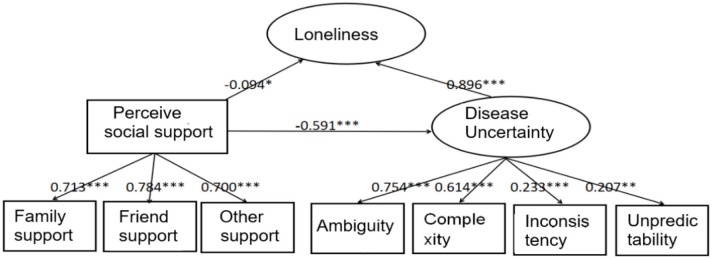
Structural equation modelling was performed using the SPSSPRO software, and path analysis was conducted with perceived social support as the mediating variable, disease uncertainty as the independent variable, and loneliness as the dependent variable. The corrected results indicated that the model had a good fit, and the results of the z test were also significant (P<0.001), further confirming the robustness of the model. The data analysis revealed that social support partially mediated the relationship between disease uncertainty and loneliness, with the mediator accounting for 57.20% of the total effect, which is [-0.094 + 0.596/-0.141 + (-0.56)] * 100%. For details, please refer to Figure 1.
Figure 1.
Structural model diagram for testing the mediating effect of loneliness, disease uncertainty, and perceived social support in elderly patients with digestive tract tumors during treatment.
Discussion
Status of loneliness in patients during treatment
The results of this study revealed that the mean score on the CLS among elderly patients receiving treatment for digestive tract tumors was 31.22±2.62 points, which indicated a high level of loneliness. A total of 111 patients (74.50%) scored above 30 points, while 38 patients (25.50%) scored between 25 and 30 points. This finding is consistent with the results of other scholars [17] and indicate that the patients in this study all experienced varying degrees of loneliness, with higher scores indicating stronger feelings of loneliness. Loneliness refers to an individual’s subjective feeling of being in a state of social isolation, often accompanied by feelings of isolation from others, isolation from society or a lack of contact with others or society [18]. Elderly patients with digestive tract tumors face greater difficulty and risks during treatment, higher mortality rates, low patient tolerance, multiple comorbidities, and weakened immune function. During treatment, side effects such as vomiting, leukopenia, pain, fever, diarrhea, and damage to the skin and important organs - especially side effects caused by chemotherapy, radiation therapy, or immune-targeted therapy - can lead to decreased compliance with treatment. Patients who experience these side effects are more prone to negative psychological emotions such as loneliness, anxiety, and fear. Researchers have reported that loneliness is also a mechanism by which social cognitive factors affect depression. Severe loneliness may eventually lead to depression [19], and some severely depressed patients may exhibit suicidal behavior, which in turn affects their survival.
Factors affecting loneliness during patient treatment
Influence of general and clinical data
This study revealed that marital and child status, family income, medical insurance payment method, disease awareness, disease course, and TNM clinical stage are the main factors affecting patients’ loneliness during treatment. Patients who are divorced, widowed, or childless in their marital and child status have a higher level of loneliness, which is consistent with the systematic evaluation results of Deckx et al. [20]. Spouses and children can accompany and take care of them carefully and can also provide spiritual or economic support in the selection of treatment plans, reducing patients’ worries and fears. The lower the family income is, the greater the degree of loneliness experienced by patients, which is consistent with the findings of other scholars [21]. Patients with low family income may experience self-blaming due to treatment costs, and some may voluntarily give up subsequent treatment and distance themselves from social interactions. Due to progress in cancer treatment, the cost of antitumor treatment has also increased, and the proportion of patients with out-of-pocket expenses is expected to increase. The reimbursement ratio of employee medical insurance is higher than that of resident medical insurance, and self-paying patients have the highest sense of loneliness. Patients are anxious about treatment costs, so they actively reduce social activities and develop feelings of loneliness. When patients are fully aware of their condition, their sense of loneliness is highest, and increased fear of death may exacerbate their loneliness. Clinical analysis of tumor TNM staging revealed that patients in the middle and late stages had higher levels of loneliness, lower survival rates and a tendency to develop a pessimistic and hopeless mentality, thus increasing their sense of loneliness [22]. The results of the disease course revealed that patients in the middle stage of the disease had a greater sense of loneliness. These patients may be worried about the recurrence and cost of the disease. As the disease progresses, their sense of loneliness decreases, which may be due to increased psychological resilience and confidence in treatment. Multivariate analysis revealed that the P value for residential areas was greater than 0.05, indicating a weak correlation. This finding may have been due to limitation with respect to sample characteristics or refinement of residential area classification.
Status of disease uncertainty during patient treatment
The overall uncertainty score of elderly patients with digestive tract malignant tumors surveyed in this study was high, with a mean MUIS-A score of 135.06±8.15 points. The lowest score was 114 points, and the highest score was 160 points. Disease uncertainty is closely related to psychological capital, implicit behavior, and cognitive abilities of patients [23]. Disease uncertainty among cancer patients mainly stems from their lack of clarity regarding how the disease will affect treatment efficacy and their quality of life. Many factors, such as the risk of disease recurrence and the pressure of multiple treatments during follow-up, can also cause patients to experience disease uncertainty.
Perceived social support during treatment
The mean scores on the PSSS was 59.69±5.96 points, with the scores ranging from 47 to 78 points. Perceived social support refers to an individual’s subjective perception and evaluation of support from various sources, such as family, others, and friends [24]. Perceived social support is the actual help provided by social interaction or relationships with individuals or the degree to which individuals perceive being loved, cared for, and attached to social groups [25]. Perceived social support is as an important modifiable psychological factor for individuals coping with stress, and it is regarded as a protective external resource [26]. Compared with general digestive tract tumor patients, elderly patients with malignant digestive tract tumors have a greater treatment response, more complications, older age, a higher mortality rate, and greater difficulty in treatment. During the treatment period, the economic burden is heavy, and greater social support promotes stronger self-management motivation in patients [27].
Correlation analysis between loneliness, disease uncertainty, and perceived social support
Spearman’s correlation analysis revealed that scores on the CLS were significantly correlated with disease uncertainty and its four dimensions, with correlation coefficients of 0.745, 0.647, 0.57 (P<0.001), 0.256, and 0.251 (P<0.01), respectively. Higher scores indicated higher levels of loneliness. The results of this study were consistent with the findings of other scholars [28]. Some patients lack knowledge about their diagnosis, treatment, and survival. Furthermore, adverse reactions to and complications from treatment can also lead to strong feelings of loneliness in patients. The negative impact of disease uncertainty on patients’ emotions not only interferes with their ability to search for information related to the disease but also leads to a decrease in patient compliance and a degradation of their role, resulting in the inability to continue treatment. The correlation coefficients between loneliness and social support as well as its three dimensions were -0.494, -0.384, -0.416, and -0.395, respectively (P<0.001). Higher scores on the PSSS indicated higher levels of perceived social support and thus lower levels of loneliness. Researchers have studied the correlation between perceived social support and psychological resilience among colorectal cancer patients [29]; a high level of perceived social support was shown to reduce adverse reactions, such as loneliness, depression, or fear, thereby significantly improving the self-regulation ability of cancer patients to combat the disease. The mediation analysis revealed that social support had a negative effect on loneliness (non-standardized coefficient = -0.141, standardized coefficient = -0.094). Social support can reduce feelings of loneliness; disease uncertainty significantly positively predicted loneliness (non-standardized coefficient = 0.596, standardized coefficient = 0.896), thus emphasizing the core role of disease uncertainty in exacerbating individual experiences of loneliness. When implementing interventions against loneliness, emphasis should also be placed on reducing disease-related uncertainty. Social support had a significant negative impact on disease uncertainty (non-standardized coefficient = -1.33, standardized coefficient = -0.591). This finding indicates that increasing social support can effectively reduce individuals’ uncertainty when facing diseases, further indicating that social support is an important resource for alleviating loneliness and uncertainty. Social support accounted for 57.20% of the total effect of disease uncertainty on loneliness, indicating that social support partially mediated the effect and is only one factor affecting disease uncertainty and loneliness rather than the only factor.
Summary
Owing to time and topic constraints, the design of this study was not detailed enough and was conducted at a single medical institution. Convenience sampling was also used, and the sample size was not large enough, which may have resulted in selection bias. The results are only applicable to elderly patients with digestive tract tumors who are receiving tumor treatment during hospitalization; therefore, the results may not be applicable to other tumor patients who are discharged after treatment is completed.
In summary, the negative emotions of loneliness in elderly patients with digestive tract tumors are closely related to disease uncertainty and perceived social support. There is currently no specific method for treating loneliness, and the main treatment methods are limited to alleviating patient symptoms and improving function. Malignant tumors are chronic diseases, and the correct model of the doctor-patient relationship should be a participatory approach [30]. The uncertainty of illness includes physiological, psychological, and spiritual aspects related to loneliness and depression. Therefore, medical staff should not only develop a correct comprehensive cancer treatment plan but also pay special attention to patients’ uncertainty of illness. Through the joint participation of doctors and patients in symptom management education, integrated medical and nursing management, and the development of other new treatment technologies, the level of patients’ disease uncertainty can be reduced, thereby improving treatment compliance, increasing comfort, reducing disease uncertainty, and mitigating loneliness and anxiety. With high levels of social support, especially from family members, patients can be full of hope and confidence in treatment, and they can also recover their physical strength quickly during the treatment cycle. Therefore, medical personnel should pay special attention to the psychological changes of patients during the treatment process; provide sufficient care and support; actively guide patients to make full use of external resources; help patients understand care from family, friends and other aspects; broaden patients’ networks, information and other support resources; enhance patients’ understanding of social support levels; and fully exert the power of patients’ inner positive beliefs, thereby reducing patients’ loneliness and disease uncertainty and achieving a good prognosis and recovery from the disease.
Acknowledgements
The work is supported by the 2024 Take-Off project of Shenzhen Hospital of Southern Medical University (No. 23H3ATF01); and Health Research Project of Anhui Province (AHWJ2023A20149).
Disclosure of conflict of interest
None.
References
- 1.Peng P, Hao Y, Liu Y, Chen S, Wang Y, Yang Q, Wang X, Li M, Wang Y, He L, Wang Q, Ma Y, He H, Zhou Y, Wu Q, Liu T. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2023;321:167–181. doi: 10.1016/j.jad.2022.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Z, Liu N, Sun M. Research progress of immunotherapy for gastric cancer. Technol Cancer Res Treat. 2023;22:153. doi: 10.1177/15330338221150555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ren L, Shen LL, Lu H, Wen X, Xu CJ. A study of grief experience interviews with family members of patients with advanced malignant tumors based on noninvasive death index monitoring. BMC Psychol. 2023;11:357. doi: 10.1186/s40359-023-01396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyu MM, Siah RC, Lam ASL, Cheng KKF. The effect of psychological interventions on fear of cancer recurrence in breast cancer survivors: a systematic review and meta-analysis. J Adv Nurs. 2022;78:3069–3082. doi: 10.1111/jan.15321. [DOI] [PubMed] [Google Scholar]
- 6.Mishel MH, Braden CJ. Finding meaning: antecedents of uncertainty in illness. Nurs Res. 1988;37:98–103. 127. [PubMed] [Google Scholar]
- 7.Massazza A, Kienzler H, Al-Mitwalli S, Tamimi N, Giacaman R. The association between uncertainty and mental health: a scoping review of the quantitative literature. J Ment Health. 2023;32:480–491. doi: 10.1080/09638237.2021.2022620. [DOI] [PubMed] [Google Scholar]
- 8.Parker PA, Davis JW, Latini DM, Baum G, Wang X, Ward JF, Kuban D, Frank SJ, Lee AK, Logothetis CJ, Kim J. Relationship between illness uncertainty, anxiety, fear of progression and quality of life in men with favourable-risk prostate cancer undergoing active surveillance. BJU Int. 2016;117:469–477. doi: 10.1111/bju.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senneseth M, Dyregrov A, Matthiesen SB, Pereira M, Hauken MA. Improving social network support for partners facing spousal cancer while caring for minors: four-month outcomes of a single-centre randomised controlled trial. Eur J Cancer Care (Engl) 2019;28:e12907. doi: 10.1111/ecc.12907. [DOI] [PubMed] [Google Scholar]
- 10.Sawma T, Choueiri P. The influence of family functioning on the severity of fear of cancer recurrence: a cross-sectional study in a sample of breast cancer survivors of Lebanese women. Eur J Oncol Nurs. 2022;60:102169. doi: 10.1016/j.ejon.2022.102169. [DOI] [PubMed] [Google Scholar]
- 11.Liu Q, Jin Y, Wang Y, Feng J, Qiao X, Ji L, Si H, Bian Y, Wang W, Yu J, Wang C. Association between self-efficacy and self-management behaviours among individuals at high risk for stroke: social support acting as a mediator. J Clin Nurs. 2023;32:71–82. doi: 10.1111/jocn.16191. [DOI] [PubMed] [Google Scholar]
- 12.Cohen G, Zalomonson S, Press Y. Prevalence of orthostatic hypotension in the unselected ambulatory population of persons aged 65 years old and above. Blood Press. 2015;24:298–305. doi: 10.3109/08037051.2015.1066998. [DOI] [PubMed] [Google Scholar]
- 13.Viechtbauer W, Smits L, Kotz D, Budé L, Spigt M, Serroyen J, Crutzen R. A simple formula for the calculation of sample size in pilot studies. J Clin Epidemiol. 2015;68:1375–1379. doi: 10.1016/j.jclinepi.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Massazza A, Kienzler H, Al-Mitwalli S, Tamimi N, Giacaman R. The association between uncertainty and mental health: a scoping review of the quantitative literature. J Ment Health. 2023;32:480–491. doi: 10.1080/09638237.2021.2022620. [DOI] [PubMed] [Google Scholar]
- 15.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 16.Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth. 2019;22:67–72. doi: 10.4103/aca.ACA_157_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pehlivan S, Ovayolu O, Ovayolu N, Sevinc A, Camci C. Relationship between hopelessness, loneliness, and perceived social support from family in Turkish patients with cancer. Support Care Cancer. 2012;20:733–739. doi: 10.1007/s00520-011-1137-5. [DOI] [PubMed] [Google Scholar]
- 18.Kraav SL, Awoyemi O, Junttila N, Vornanen R, Kauhanen J, Toikko T, Lehto SM, Hantunen S, Tolmunen T. The effects of loneliness and social isolation on all-cause, injury, cancer, and CVD mortality in a cohort of middle-aged Finnish men. A prospective study. Aging Ment Health. 2021;25:2219–2228. doi: 10.1080/13607863.2020.1830945. [DOI] [PubMed] [Google Scholar]
- 19.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21:140–51. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 20.Deckx L, van den Akker M, Buntinx F. Risk factors for loneliness in patients with cancer: a systematic literature review and meta-analysis. Eur J Oncol Nurs. 2014;18:466–477. doi: 10.1016/j.ejon.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Dahill A, Al-Nakishbandi H, Cunningham KB, Humphris GM, Lowe D, Rogers SN. Loneliness and quality of life after head and neck cancer. Br J Oral Maxillofac Surg. 2020;58:959–965. doi: 10.1016/j.bjoms.2020.04.041. [DOI] [PubMed] [Google Scholar]
- 22.Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, Sado M, Nakagawa A, Takahashi M, Hayashida T, Fujisawa D. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer-a randomized controlled trial. J Pain Symptom Manage. 2020;60:381–389. doi: 10.1016/j.jpainsymman.2020.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Rahimi Esbo S, Ghaffari F, Fotokian Z, Nikbakht HA, Saadati K. Development and psychometric evaluation of uncertainty about disease and treatment scale in hemodialysis patients: a sequential-exploratory mixed-method study. BMC Psychol. 2024;12:187. doi: 10.1186/s40359-024-01685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uchino BN, Baucom BRW, Landvatter J, de Grey RGK, Tacana T, Flores M, Ruiz JM. Perceived social support and ambulatory blood pressure during daily life: a meta-analysis. J Behav Med. 2022;45:509–517. doi: 10.1007/s10865-021-00273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen C, Sun X, Liu Z, Jiao M, Wei W, Hu Y. The relationship between resilience and quality of life in advanced cancer survivors: multiple mediating effects of social support and spirituality. Front Public Health. 2023;11:1207097. doi: 10.3389/fpubh.2023.1207097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan X, Huang H, Peng Q, Yu NX, Zhang Y, Ding Y, Wu H, Hao J, Lu G, Chen C. A meta-analysis on the relationship between posttraumatic growth and resilience in people with breast cancer. Nurs Open. 2023;10:2734–2745. doi: 10.1002/nop2.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lea S, Martins A, Morgan S, Cargill J, Taylor RM, Fern LA. Health care professional perceptions of online information and support for young people with cancer in the United Kingdom. Adolesc Health Med Ther. 2019;10:103–116. doi: 10.2147/AHMT.S211142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Song Z, Wei L, Liu Y, Bian J, Wang C, Wang S. The mediating role of psychological capital between post-traumatic growth and uncertainty in illness among patients with Parkinson’s disease. Geriatr Nurs. 2023;50:194–202. doi: 10.1016/j.gerinurse.2023.01.014. [DOI] [PubMed] [Google Scholar]
- 29.Çakir H, Küçükakça Çelik G, Çirpan R. Correlation between social support and psychological resilience levels in patients undergoing colorectal cancer surgery: a descriptive study. Psychol Health Med. 2021;26:899–910. doi: 10.1080/13548506.2020.1859561. [DOI] [PubMed] [Google Scholar]
- 30.Hopwood M. The shared decision-making process in the pharmacological management of depression. Patient. 2020;13:23–30. doi: 10.1007/s40271-019-00383-w. [DOI] [PMC free article] [PubMed] [Google Scholar]