Abstract
Objective: To evaluate the impact of different surgical fixation sequences on ankle joint stability and functional recovery in patients with trimalleolar fractures. Methods: A retrospective analysis was conducted on the medical records of 144 patients with trimalleolar fractures treated at Xi’an International Medical Center Hospital. Among these, 78 patients underwent the fixation sequence of lateral malleolus-posterior malleolus-medial malleolus (Group A), while 66 patients underwent the sequence of posterior malleolus-lateral malleolus-medial malleolus (Group B). Perioperative parameters, including operation time, intraoperative blood loss, healing time, hospital stay, and treatment cost, were compared between the two groups. Patient recovery was assessed using the Radiographic Union Score for Hip (RUSH) and Visual Analogue Scale (VAS) at postoperative 3 months and Biard-Jackson scores at postoperative 3 and 12 months. Logistic regression analysis was used to identify risk factors influencing postoperative joint function recovery. The incidence of postoperative complications was also compared between the two groups. Results: Group A demonstrated significantly shorter operation time (P < 0.001) and reduced intraoperative blood loss (P < 0.001) compared to Group B. No significant differences were observed in healing time (P = 0.905), hospital stay (P = 0.374), or treatment cost (P = 0.454) between the two groups. Similarly, RUSH (P = 0.780) and VAS (P = 0.590) scores at post-operative 3 months showed no significant differences between the two groups. However, Group A exhibited significantly higher Biard-Jackson scores at postoperative 3 months compared to Group B (P < 0.001), with no significant difference noted at postoperative 12 months (P = 0.157). The overall incidence of complications did not differ significantly between the groups (P = 0.164). Independent risk factors for prognosis included the treatment plan (P = 0.025), body mass index (P = 0.042), distal tibiofibular injury (P = 0.002), and intraoperative blood loss (P = 0.021). Conclusion: Patients with trimalleolar fractures who underwent fixation in the sequence of lateral malleolus-posterior malleolus-medial malleolus showed improved ankle joint functional recovery at postoperative 3 months compared to those treated with the posterior malleolus-lateral malleolus-medial malleolus sequence. No significant differences were observed at postoperative 12 months. Operation time and intraoperative blood loss were critical factors influencing short-term recovery outcomes.
Keywords: Fracture fixation, trimalleolar fracture, ankle joint stability, ankle joint function
Introduction
Ankle joint, as the primary weight-bearing hinge joint in human body, plays a crucial role in maintaining structural stability and flexibility, essential for everyday activities such as walking [1]. In upright position, the entire body weight is concentrated on the ankle joint, creating significant localized stress. The ankle joint comprises the distal tibia, fibula, and talar dome, also known as the talocrural joint [2]. Stability is maintained by the bones themselves, along with the surrounding joint capsule and ligament system. The complex ligament system involves the medial deltoid ligament, lateral collateral ligaments, and the distal tibiofibular syndesmosis [3].
With the rapid urbanization, the diversification of transportation means, and the expansion of urban and rural road networks, the incidence of traffic accidents has increased correspondingly [4]. Ankle injuries resulting from high-energy traumas, such as car accidents and falls from heights, are also on the rise [5]. Among adults, ankle fractures are among the most frequent injuries, accounting for approximately 4% of all fractures [6]. Trimalleolar fractures, a severe type of ankle fracture involving the medial malleolus, fibula, and posterior lip of the distal tibia, are common intra-articular fractures in clinical settings [7]. Displaced fractures often cause ankle dislocation and foot rotational deformity, severely compromising the integrity, stability, and flexibility of the ankle joint, thereby affecting joint function [8].
The displacement of fracture ends significantly alters the normal structure of the ankle joint. Clinically, open reduction and internal fixation (ORIF) is a typical approach to achieve anatomical reduction of the fracture ends, restore the original tension of the damaged ligaments, and ultimately regain joint stability [9]. Due to the complex nature of ankle fractures, the treatment outcomes for trimalleolar fractures can vary greatly. Therefore, managing trimalleolar fractures remains a significant challenge in fracture treatment [10]. To restore the lost stability of the joint, the preferred treatment option for trimalleolar fractures is open reduction of the fracture ends, followed by internal fixation [11]. However, there is no consensus on the optimal sequence for reducing the medial, lateral, and posterior malleoli during surgery. Some researchers have noted that fixing the lateral malleolus first can hinder the reduction of the medial malleolus fragment, complicating proper fibula reduction and ultimately preventing accurate reduction of the posterior malleolus [12,13]. Some experts argue that reducing the posterior malleolus first can avoid these issues, as correctly reducing the posterior malleolus provides a stable anatomical reference for the fibula and medial malleolus, facilitating precise reduction. However, this approach also presents challenges, such as increased complexity, prolonged operation time, and increased blood loss [14]. Thus, each reduction sequence during surgery has its own advantages and disadvantages, with no established consensus.
This study aims to determine the most effective treatment approach for trimalleolar fractures by comparing the outcomes of two different reduction and fixation sequences: posterior malleolus-lateral malleolus-medial malleolus versus lateral malleolus-posterior malleolus-medial malleolus. The goal is to identify an optimal sequence to enhance surgical success and promote functional recovery for patients with trimalleolar fracture.
Methods and materials
Data collection
Medical records of patients with trimalleolar fractures treated at Xi’an International Medical Center Hospital between April 2019 and May 2023 were retrospectively reviewed. A total of 144 eligible cases were identified, with 78 patients underwent the fixation sequence of lateral malleolus-posterior malleolus-medial malleolus assigned to Group A and 66 patients underwent the fixation sequence of posterior malleolus-lateral malleolus-medial malleolus to Group B (Figure 1). The study was conducted with the approval from the Medical Ethics Committee of Xi’an International Medical Center Hospital.
Figure 1.
Case screening flowchart.
Inclusion and exclusion criteria
Inclusion criteria: Patients with ankle injury, presenting with swelling, deformity, or abnormal movement indicative of a fracture; Patients meeting the established diagnostic criteria for trimalleolar fractures, with imaging studies such as X-rays and CT scans confirmed significant displacement of the fracture ends, involving the medial, lateral, and posterior malleoli [2]; Patients with complete clinical data.
Exclusion criteria: Patients with open or pathological fractures, underlying joint diseases that could affect functional recovery (e.g., rheumatoid arthritis, purulent arthritis, gouty arthritis); Patients with concurrent malignant tumors; Pregnant women.
Surgical procedure
Patients were instructed to discontinue aspirin (Yunnan Baiyao Group Co., LTD., Sinopharm-approved H53021845) and other anticoagulants one week prior to surgery and underwent a comprehensive preoperative evaluation. Patients fasted for 6 hours before surgery, and prophylactic antibiotics were administered 30 minutes prior to surgery to mitigate the risk of infection.
Surgical steps for patients in Group A
Patients were placed in a lateral decubitus position for spinal anesthesia. An incision was made via a posterolateral approach to the fibula, and the skin, superficial fascia, and deep fascia were carefully dissected to protect the sural and superficial peroneal nerves. After exposing the fracture site, the lateral malleolus was first anatomically reduced and fixed with screws. The posterior malleolus was then exposed, reduced, and temporarily fixed with K-wires, followed by drilling and the insertion of a lag screw for stabilization. An appropriate reconstruction plate was selected and fixed under C-arm fluoroscopy guidance (Model: OEC Elite, Manufacturer: GE Healthcare). An arc-shaped incision was made along the medial side to expose the deltoid ligament and medial malleolus, which were then reduced and fixed with compression screws. Bone defects were filled with bone grafts to promote healing. Siemens Healthineers’ Multix Fusion Max X-rays confirmed the restoration of the ankle joint structure. The joint capsule and ligaments were repaired, and the incision was closed with the insertion of a drain.
Surgical steps for patients in Group B
In Group B, the reduction and fixation sequence was adjusted to posterior malleolus-lateral malleolus-medial malleolus. The surgical approach was the same as in Group A, with the posterior malleolus being reduced and fixed first, followed by the lateral and medial malleoli.
Postoperative management
Postoperatively, both groups received neutral plaster external fixation and were encouraged to perform toe flexion and extension exercises to promote circulation. Antibiotics were administered for 1 to 3 days postoperatively, along with medications to reduce swelling and promote bone healing. The plaster was removed 4 to 6 weeks postoperatively, and patients were instructed to perform ankle flexion and extension exercises. Monthly X-rays were conducted to monitor fracture healing. Weight-bearing walking was started at 8 to 12 weeks postoperatively, along with ankle function strengthening exercises. Internal fixation removal was planned for 8 to 12 months postoperatively, based on the patient’s recovery.
Clinical data collection
Clinical data were collected from electronic medical records, outpatient follow-up records, and follow-up visits. The data included age, gender, body mass index (BMI), fracture site, injury mechanism, fracture type, household income, residence, treatment cost, history of hypertension, history of diabetes, distal tibiofibular injury, operation time, intraoperative blood loss, healing time, hospital stay, treatment cost, Radiographic Union Score for Hip (RUSH), Visual Analogue Scale (VAS), Biard-Jackson score, and postoperative complications.
Functional scores
The RUSH score was used to assess fracture healing, primarily through radiographic examination, with scores ranging from 0 to 12, where higher score indicated better fracture healing [15].
The VAS score was used to assess pain levels. Patients marked their pain intensity on a straight line, yielding scores from 0 to 10, where higher score indicated more severe pain [16].
The Biard-Jackson score was used to assess ankle joint function, particularly after ankle fractures. This scoring system evaluates various aspects of the ankle joint, including pain, function, range of motion, and alignment, with scores ranging from 0 to 100 points, where higher score indicates better functional recovery [17].
Outcome measures
Primary outcomes
The study compared perioperative indicators between the two groups, as well as RUSH and VAS scores at postoperative 3 months. Additionally, Biard-Jackson scores at 3 and 12 months postoperatively were also compared between the two groups. Logistic regression analysis was conducted to identify risk factors influencing postoperative joint function (Biard-Jackson score).
Secondary outcomes
Baseline data were compared between the two groups, and the frequency of postoperative complications was analyzed.
Statistical analysis
Data were analyzed using SPSS 26.0 software, and images were rendered using GraphPad Prism 9.5.1. Quantitative data were tested for normality and homogeneity of variance. Normally distributed data were presented as mean ± standard deviation (SD). Independent sample t-tests were used for inter-group comparisons, and paired t-tests were used for intra-group comparisons. Non-normally distributed data were expressed as median (interquartile range) and compared using non-parametric tests. Categorical data were presented as n (%) and compared using chi-square tests. Binary logistic regression was used to analyze risk factors for postoperative joint function. The sample size calculation indicated that approximately 78 cases per group were required, with a total of 156 samples to meet a patient prevalence of 45%, significance level of 0.05, and test efficacy of 80%. A P-value of < 0.05 was considered statistically significant.
Results
Comparison of baseline data between the two groups
No significant differences were found between the two groups in terms of age (P = 0.329), gender (P = 0.337), BMI (P = 0.607), fracture site (P = 0.427), injury mechanism (P = 0.406), fracture type (P = 0.533), household income (P = 0.323), residence (P = 0.612), settlement method (P = 0.255), history of hypertension (P = 0.520), history of diabetes (P = 0.424), or distal tibiofibular injury (P = 0.654) (Table 1).
Table 1.
Comparison of baseline data between the two groups (n, %)
| Factors | Group A (n = 78) | Group B (n = 66) | χ2 Value | P Value |
|---|---|---|---|---|
| Age | ||||
| ≥ 45 years | 35 | 35 | 0.953 | 0.329 |
| < 45 years | 43 | 31 | ||
| Gender | ||||
| Male | 51 | 38 | 0.923 | 0.337 |
| Female | 27 | 28 | ||
| BMI | ||||
| ≥ 25 kg/m2 | 15 | 15 | 0.265 | 0.607 |
| < 25 kg/m2 | 63 | 51 | ||
| Fracture site | ||||
| Left | 35 | 34 | 0.632 | 0.427 |
| Right | 43 | 32 | ||
| Injury mechanism | ||||
| Low-energy injury | 48 | 45 | 0.69 | 0.406 |
| High-energy injury | 30 | 21 | ||
| Fracture type | ||||
| Supination-external rotation type | 58 | 52 | 0.388 | 0.533 |
| Pronation-external rotation type | 20 | 14 | ||
| Household income | ||||
| < 50,000 | 48 | 38 | 2.258 | 0.323 |
| 50,000-100,000 | 24 | 26 | ||
| > 100,000 | 6 | 2 | ||
| Residence | ||||
| Urban | 61 | 50 | 0.121 | 0.728 |
| Rural | 17 | 16 | ||
| Settlement method | ||||
| Insurance | 66 | 60 | 1.295 | 0.255 |
| Self-Pay | 12 | 6 | ||
| History of hypertension | ||||
| Yes | 15 | 10 | 0.415 | 0.52 |
| No | 63 | 56 | ||
| History of diabetes | ||||
| Yes | 9 | 5 | 0.64 | 0.424 |
| No | 69 | 61 | ||
| Distal tibiofibular injury | ||||
| Yes | 12 | 12 | 0.201 | 0.654 |
| No | 66 | 54 |
Note: BMI, body mass index.
Perioperative indicators
Comparison of perioperative indicators between the two groups revealed that the operation time and intraoperative bleeding were significantly lower in group A than in group B (both P < 0.001). However, there were no statistical differences in the healing time (P = 0.905), the length of hospitalization (P = 0.374), and the cost of treatment (P = 0.454) between the two groups (Table 2).
Table 2.
Comparison of perioperative indicators between the two groups (n, %)
| Indicator | Group A (n = 78) | Group B (n = 66) | Statistic Value | P Value |
|---|---|---|---|---|
| Operation time (min) | 51.49 (5.58) | 62.41 (8.61) | -8.848 | < 0.001 |
| Intraoperative blood loss (ml) | 149.44 (13.21) | 165.79 (18.94) | -5.902 | < 0.001 |
| Healing time (days) | 36.35 (6.38) | 36.47 (5.95) | -0.12 | 0.905 |
| Hospital stay (days) | 15.01 (2.92) | 15.53 (3.87) | -0.892 | 0.374 |
| Treatment cost (RMB) | 14948.76 (1822.67) | 15178.70 (1834.22) | -0.752 | 0.454 |
Comparison of healing and pain scores between the two groups
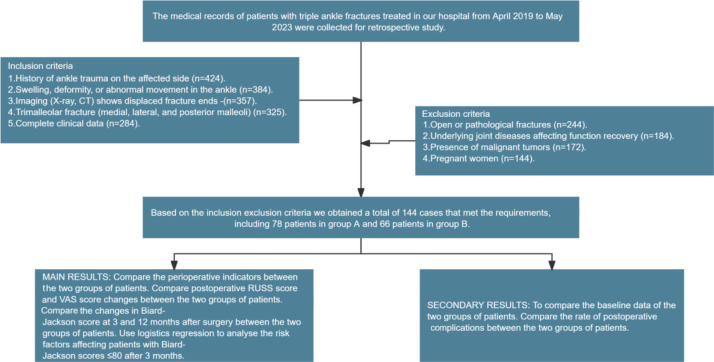
Fracture healing and pain levels were evaluated using the RUSH and VAS scores, respectively. Results showed no significant differences in RUSH scores (P = 0.780) or VAS scores (P = 0.590) between the two groups at 3 months postoperatively (Figure 2).
Figure 2.
Comparison of RUSH and VAS scores between the two groups. A. Comparison of RUSH scores at 3 months postoperatively between the two groups. B. Comparison of VAS scores at 3 months postoperatively between the two groups. Note: RUSH, radiographic union score for hip; VAS, visual analog scale; nsP > 0.05.
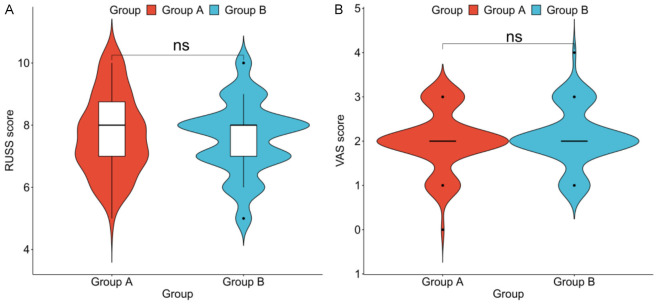
Comparison of postoperative Biard-Jackson scores between the two groups
Biard-Jackson scores were used to compare ankle joint function between the two groups. Group A had significantly higher Biard-Jackson scores at 3 months postoperatively compared to Group B (P < 0.001). However, there was no significant difference in Biard-Jackson scores between the two groups at 12 months postoperatively (P = 0.157, Figure 3).
Figure 3.
Comparison of Biard-Jackson scores between the two groups. A. Comparison of Biard-Jackson scores at 3 months postoperatively between the two groups. B. Comparison of Biard-Jackson scores at 12 months postoperatively between the two groups. Note: nsP > 0.05, and ***P < 0.001.
Comparison of postoperative complications between the two groups
The comparison of postoperative complications, including incision infection, internal fixation loosening and traumatic arthritis, showed no significant differences between the two groups (P > 0.05). Additionally, no significant difference was found in the overall incidence of complications between the two groups (P = 0.164, Table 3).
Table 3.
Comparison of incidence of postoperative complications between the two groups (n, %)
| Complication | Group A (n = 78) | Group B (n = 66) | χ2 Value | P Value |
|---|---|---|---|---|
| Incision infection | 1 (1.28%) | 2 (3.04%) | 0.537 | 0.464 |
| Internal fixation loosening | 0 (0.00%) | 1 (1.52%) | 1.19 | 0.275 |
| Traumatic arthritis | 1 (1.28%) | 2 (3.04%) | 0.537 | 0.464 |
| Total incidence | 2 (2.56%) | 5 (7.60%) | 1.942 | 0.164 |
Risk factors affecting short-term ankle joint function recovery
The study found that Group A had significantly higher Biard-Jackson scores at 3 months postoperatively compared to Group B, with no significant difference at 12 months. To further identify risk factors affecting short-term recovery, patients were divided into a poor recovery group (Biard-Jackson score ≤ 80) and a good recovery group (Biard-Jackson score > 80) based on their 3-month postoperative Biard-Jackson scores. Data categorization (Table 4) and univariate analysis identified several significant risk factors affecting patient prognosis, including the treatment plan (P < 0.001), BMI (P = 0.022), distal tibiofibular injury (P = 0.002), operation time (P < 0.001), and intraoperative blood loss (P < 0.001) (Table 5). Multivariate logistic regression analysis further confirmed that the treatment plan (P = 0.025), BMI (P = 0.042), distal tibiofibular injury (P = 0.002), and intraoperative blood loss (P = 0.021) were independent risk factors affecting the prognosis (Table 6).
Table 4.
Assignment table
| Factors | Assignment |
|---|---|
| Treatment plan | Group A = 1, Group B = 0 |
| Age | ≥ 45 years = 1, < 45 years = 0 |
| Gender | Male = 1, Female = 0 |
| BMI | ≥ 25 kg/m2 = 1, < 25 kg/m2 = 0 |
| Fracture site | Left = 1, Right = 0 |
| Injury mechanism | Low-energy injury = 1, High-energy injury = 0 |
| Fracture type | Supination-external rotation = 1, Pronation-external rotation = 0 |
| Household income | < 50,000 = 1, 50,000-100,000 = 2, > 100,000 = 3 |
| Residence | Urban = 1, Rural = 0 |
| Settlement method | Insurance = 1, Self-Pay = 0 |
| History of hypertension | Yes = 1, No = 0 |
| History of diabetes | Yes = 1, No = 0 |
| Distal tibiofibular injury | Yes = 1, No = 0 |
| Operation time | < 56.5 min = 1, ≥ 56.5 min = 0 |
| Intraoperative blood loss | < 166.5 ml = 1, ≥ 166.5 ml = 0 |
| Healing time | < 32.5 days = 1, ≥ 32.5 days = 0 |
| Hospital stay | < 14.5 days = 1, ≥ 14.5 days = 0 |
| Treatment cost | < 14,633 ¥ = 1, ≥ 14,633 ¥ = 0 |
| RUSH score | < 8.5 = 1, ≥ 8.5 = 0 |
| VAS score | < 2.5 = 1, ≥ 2.5 = 0 |
| 3-month prognosis | Biard-Jackson score ≤ 80 = 1, > 80 = 0 |
Note: BMI, body mass index; RUSH, radiographic union score for Hip; VAS, visual analog scale.
Table 5.
Univariate logistic analysis of factors affecting short-term prognosis
| Variable | Estimate | Std. Error | P | OR | 95% CI |
|---|---|---|---|---|---|
| Treatment plan | -1.758 | 0.368 | 0.000 | 0.172 | 0.082-0.349 |
| Age | 0.213 | 0.336 | 0.526 | 1.237 | 0.641-2.398 |
| Gender | -0.185 | 0.345 | 0.591 | 0.831 | 0.422-1.636 |
| BMI | 0.974 | 0.425 | 0.022 | 2.648 | 1.169-6.256 |
| Fracture site | 0.150 | 0.336 | 0.655 | 1.162 | 0.601-2.25 |
| Injury mechanism | -0.164 | 0.350 | 0.640 | 0.849 | 0.427-1.691 |
| Fracture type | 0.174 | 0.398 | 0.661 | 1.190 | 0.549-2.635 |
| Household income | -0.184 | 0.283 | 0.515 | 0.832 | 0.473-1.441 |
| Residence | -0.369 | 0.398 | 0.353 | 0.691 | 0.315-1.51 |
| Settlement method | 0.000 | 0.507 | 1.000 | 1.000 | 0.37-2.779 |
| History of hypertension | -0.022 | 0.443 | 0.961 | 0.978 | 0.403-2.327 |
| History of diabetes | -0.071 | 0.568 | 0.900 | 0.931 | 0.292-2.827 |
| Distal tibiofibular injury | 1.574 | 0.507 | 0.002 | 4.826 | 1.874-14.127 |
| Operation time | -1.564 | 0.361 | 0.000 | 0.209 | 0.101-0.419 |
| Intraoperative blood loss | -1.711 | 0.410 | 0.000 | 0.181 | 0.078-0.394 |
| Healing time | -0.228 | 0.372 | 0.539 | 0.796 | 0.38-1.641 |
| Hospital stay | -0.310 | 0.342 | 0.365 | 0.733 | 0.372-1.43 |
| Treatment cost | -0.229 | 0.339 | 0.499 | 0.795 | 0.407-1.543 |
| RUSH score | 0.368 | 0.411 | 0.371 | 1.444 | 0.652-3.309 |
| VAS score | 0.300 | 0.414 | 0.469 | 1.350 | 0.605-3.106 |
Note: BMI, body mass index; RUSH, radiographic union score for Hip; VAS, visual analog scale.
Table 6.
Multifactorial logistic analysis of factors affecting short-term prognosis
| Variable | Estimate | Std. Error | P | OR | 95% CI |
|---|---|---|---|---|---|
| Treatment plan | -1.119 | 0.498 | 0.025 | 0.327 | 0.12-0.861 |
| BMI | 1.047 | 0.516 | 0.042 | 2.850 | 1.054-8.079 |
| Distal tibiofibular injury | 1.794 | 0.587 | 0.002 | 6.015 | 1.991-20.409 |
| Operation time | -0.735 | 0.475 | 0.121 | 0.479 | 0.188-1.229 |
| Intraoperative blood loss | -1.126 | 0.488 | 0.021 | 0.324 | 0.122-0.838 |
Note: BMI, body mass index.
Discussion
In recent years, the critical role of the posterior malleolus in maintaining ankle stability has garnered increasing attention. The anatomical features of the posterior malleolus, including its lip-shaped projection, help stabilize the talus and prevent its posterior displacement. These features also increase the contact area, evenly distribute stress, and maintain overall body balance [18]. Additionally, the posterior malleolus serves as the attachment site for the posterior inferior tibiofibular ligament, contributing to the stability of the distal tibiofibular syndesmosis [19]. For fractures involving the posterior malleolus, direct fixation is generally preferred over ligament reconstruction or the use of lag screws, as restoring the anatomical position of the posterior malleolus is crucial for preserving ankle joint stability.
As an intra-articular fracture, the treatment of trimalleolar fractures requires precise anatomical reduction to prevent restricted joint movement and the development of post-traumatic osteoarthritis [20]. However, there is ongoing debate on the optimal reduction sequence for trimalleolar fractures, with different opinions among scholars [21,22]. Reducing the posterior malleolus first may facilitate accurate positioning of the fibula and reduce the number of reductions and intraoperative blood loss, while fixing the posterior malleolus first can help visualize the talocrural joint space after reducing the medial and lateral malleoli [23].
This study compared the outcomes of two surgical approaches for trimalleolar fracture treatment: lateral malleolus-posterior malleolus-medial malleolus (Group A) versus posterior malleolus-lateral malleolus-medial malleolus (Group B). The results showed no significant differences between the two groups in terms of healing time, hospital stay, treatment cost, 3-month RUSH scores, 3-month VAS scores, 12-month Biard-Jackson scores, and postoperative complications. These findings suggest that the uniformity of postoperative management and rehabilitation protocols resulted in similar healing environments and resource utilization across both groups. The comparable RUSH and VAS scores indicate that both surgical sequences are equally effective in restoring fracture stability and anatomical structure. The absence of significant differences in 12-month Biard-Jackson scores suggests that long-term functional recovery is likely influenced by postoperative rehabilitation and individual recovery factors rather than the surgical order itself.
Notably, Group A demonstrated significantly shorter operation duration, less intraoperative blood loss, and higher Biard-Jackson scores at 3 months postoperatively compared to Group B. These outcomes can be attributed to the initial reduction of the lateral malleolus, which provides better visualization and access to the posterior and medial malleolar fractures. This sequence establishes a stable reference point for the surgeon, reducing the need for adjustments during surgery, shortening the duration of the procedure, and minimizing blood loss, ultimately leading to a quicker recovery. Tian et al. [24] reported no differences in operation time or intraoperative blood loss between patients treated with posterolateral and posteromedial approaches for posterior malleolar fractures, aligning with our findings. Prioritizing lateral malleolus reduction appears to optimize the surgical process, enhance early functional recovery, and does not adversely affect long-term clinical outcomes.
Our study further revealed that Group A exhibited higher Biard-Jackson scores at 3 months postoperatively, with no significant differences at postoperative 12 months. This indicates that the initial reduction and fixation sequence significantly impacts short-term recovery but has a diminishing effect on long-term recovery. To identify factors affecting short-term recovery, patients were categorized into poor recovery (≤ 80) and good recovery (> 80) groups based on their 3-month Biard-Jackson scores. Multivariate logistic regression analysis identified the treatment plan, BMI, distal tibiofibular injury, and intraoperative blood loss as independent risk factors for short-term recovery. Notably, a higher BMI (≥ 25 kg/m2) was identified as a risk factor for poor recovery. Obese patients often face challenges such as poorer soft tissue conditions and increased surgical difficulty, complicating postoperative rehabilitation and adversely affecting short-term functional recovery [25]. For example, Xiao et al. [26] found that patients with ankle fracture wound complications had significantly higher BMI (28.84 ± 5.36) compared to those without complications (22.84 ± 2.68), and logistic regression analysis confirmed BMI as an independent risk factor for postoperative complications. Obese patients tend to have thickened soft tissues, relatively poor blood supply, and a higher likelihood of wound complications, such as infection and delayed healing [27]. Moreover, obesity increases surgical complexity, prolongs operation times, and elevates intraoperative blood loss, all contributing to poorer short-term recovery. Previous study [28] has also shown that a high BMI negatively affects recovery time following calcaneal open reduction and internal fixation.
Distal tibiofibular injury significantly affects ankle joint stability and functional recovery. Injuries to the distal tibiofibular syndesmosis delay rehabilitation due to joint instability. Neumann et al. [29] reported that patients with distal tibia and fibula fractures, particularly those treated with intramedullary nails, were at a higher risk of postoperative complications, including delayed union and nonunion. Reducing intraoperative blood loss is crucial in decreasing postoperative inflammation, promoting wound healing, and enhancing early functional recovery. Excessive intraoperative blood loss can lead to the accumulation of inflammatory mediators and cytokines at the injury site, exacerbating the local inflammatory response, increasing swelling and pain, and delaying wound healing [30]. Additionally, excessive blood loss may result in hematoma formation, increasing the risk of postoperative infection and hindering recovery [31]. The lateral malleolus-posterior malleolus-medial malleolus sequence appears superior to the posterior malleolus-lateral malleolus-medial malleolus sequence in the short term, as it allows better visualization and management of fractures, shortens surgery duration, reduces blood loss, minimizes surgical trauma, and accelerates recovery.
Despite the short-term benefits observed with the lateral malleolus-posterior malleolus-medial malleolus sequence, further large-sample, multicenter prospective studies are necessary to confirm the reliability and generalizability of these findings and to explore other possible factors influencing postoperative recovery. Addressing these limitations will provide stronger evidence for determining optimal surgical approach to treating trimalleolar fractures.
Conclusion
For patients with trimalleolar fractures, the lateral malleolus-posterior malleolus-medial malleolus fixation sequence results in better ankle joint functional recovery at 3 months postoperatively compared to the posterior malleolus-lateral malleolus-medial malleolus sequence. However, there is no significant difference at 12 months postoperatively. Operation time and intraoperative blood loss have a significant impact on short-term recovery outcomes.
Disclosure of conflict of interest
None.
References
- 1.Lintz F, Bernasconi A, Buedts K, Welck M, Ellis S, de Cesar Netto C. Ankle joint bone density distribution correlates with overall 3-dimensional foot and ankle alignment. J Bone Joint Surg Am. 2023;105:1801–1811. doi: 10.2106/JBJS.23.00180. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L, Sun X, Jiang L, Zhou X, Shi H, Yang Y, Cai M, Wang G. The morphology of osseous structure in subtalar joint with chronic ankle instability. Foot Ankle Surg. 2024;30:74–78. doi: 10.1016/j.fas.2023.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Ferkel RD, Kwong C, Farac R, Pinto M, Fahimi N, Rahhal S, Marumoto J. Arthroscopic posterior ankle ligament anatomy. Foot Ankle Orthop. 2021;6:24730114211000624. doi: 10.1177/24730114211000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diop B, Mendy O, Tene Nde AF, Dione AB, Diop M, Diouf PA, Sow M, Sarr N, Faye I, Ndoye AY, Konate I. Anterior dislocation of the shoulder associated with a diaphyseal fracture of the ipsilateral humerus: a case report. Ann Med Surg (Lond) 2023;86:477–480. doi: 10.1097/MS9.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun N, Liu Y, Yan H, Zhang Z, Li Y, Zeng C. Recent progress in the classification and operation of sacral fractures. Emerg Med Int. 2023;2023:2795722. doi: 10.1155/2023/2795722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X, Xu X. Joint preservation for posttraumatic ankle arthritis after tibial plafond fracture. Foot Ankle Clin. 2022;27:73–90. doi: 10.1016/j.fcl.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Stead TS, Pomerantz LH, Ganti L, Leon L, Elbadri S. Acute management of trimalleolar fracture. Cureus. 2021;13:e12536. doi: 10.7759/cureus.12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pflüger P, Harder F, Müller K, Biberthaler P, Crönlein M. Evaluation of ankle fracture classification systems in 193 trimalleolar ankle fractures. Eur J Trauma Emerg Surg. 2022;48:4181–4188. doi: 10.1007/s00068-022-01959-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agrawal IT, Thakre VM, Deshpande MM, Bahirde C. Comprehensive physiotherapy protocol in post-operative case of trimalleolar fracture: a case report. Cureus. 2023;15:e50705. doi: 10.7759/cureus.50705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen DL, Liu P, Zheng LX, Zhu ZH, Zhang ZF. Fracture gap of the lateral malleolus via posterolateral approach: improved visualization of the posterior malleolus fracture. Injury. 2022;53:3849–3852. doi: 10.1016/j.injury.2022.08.051. [DOI] [PubMed] [Google Scholar]
- 11.Nasrallah K, Einal B, Shtarker H. Trimalleolar fracture: the endless posterior malleolus fracture debate, to repair or not to repair? Orthop Rev (Pavia) 2021;13:8784. doi: 10.4081/or.2021.8784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wawrose RA, Grossman LS, Tagliaferro M, Siska PA, Moloney GB, Tarkin IS. Temporizing external fixation vs splinting following ankle fracture dislocation. Foot Ankle Int. 2020;41:177–182. doi: 10.1177/1071100719879431. [DOI] [PubMed] [Google Scholar]
- 13.Buyukkuscu MO, Basilgan S, Mollaomeroglu A, Misir A, Basar H. Splinting vs temporary external fixation in the initial treatment of ankle fracture-dislocations. Foot Ankle Surg. 2022;28:235–239. doi: 10.1016/j.fas.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Kang C, Hwang DS, Lee JK, Won Y, Song JH, Lee GS. Screw fixation of the posterior malleolus fragment in ankle fracture. Foot Ankle Int. 2019;40:1288–1294. doi: 10.1177/1071100719865895. [DOI] [PubMed] [Google Scholar]
- 15.Fan Y, Bai D, Cheng C, Tian G. The effectiveness and safety of blood flow restriction training for the post-operation treatment of distal radius fracture. Ann Med. 2023;55:2240329. doi: 10.1080/07853890.2023.2240329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hwang WY, Kim K, Cho HY, Yang EJ, Suh DH, No JH, Lee JR, Hwang JW, Do SH, Kim YB. The voiding VAS score is a simple and useful method for predicting POUR after laparoscopy for benign gynaecologic diseases: a pilot study. J Obstet Gynaecol. 2022;42:2469–2473. doi: 10.1080/01443615.2022.2071149. [DOI] [PubMed] [Google Scholar]
- 17.Lin Z, Gao LY, Ruan KM, Guo DB, Chen YH, Liu QP. Clinical observation on the treatment of ankle fracture with buttress plate and traditional internal fixation and its effect on GQOLI-74 score and Baird-Jackson score. Pak J Med Sci. 2023;39:529–533. doi: 10.12669/pjms.39.2.6876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshimoto K, Noguchi M, Maruki H, Tominaga A, Okazaki K. Hindfoot alignment and ankle stability following arthroscopic lateral ankle ligament repair. Foot Ankle Int. 2023;44:872–878. doi: 10.1177/10711007231181123. [DOI] [PubMed] [Google Scholar]
- 19.Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10:558–560. doi: 10.1016/s0749-8063(05)80014-3. [DOI] [PubMed] [Google Scholar]
- 20.Bartoníček J, Fojtík P, Bunganičová E, Tuček M. Maisonneuve ankle fracture. Rozhl Chir. 2023;102:48–59. doi: 10.33699/PIS.2023.102.2.48-59. [DOI] [PubMed] [Google Scholar]
- 21.Pan Z, Cui X, Zhu Y, Qi H, Chen H, Tang P. Application of posterolateral approach for treatment of bimalleolar and trimalleolar fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2016;30:1488–1492. doi: 10.7507/1002-1892.20160308. [DOI] [PubMed] [Google Scholar]
- 22.Verhage SM, Hoogendoorn JM, Krijnen P, Schipper IB. When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg. 2018;138:1213–1222. doi: 10.1007/s00402-018-2949-2. [DOI] [PubMed] [Google Scholar]
- 23.Lambert LA, Falconer L, Mason L. Ankle stability in ankle fracture. J Clin Orthop Trauma. 2020;11:375–379. doi: 10.1016/j.jcot.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tian F, Xia R, Liu L, Fang S, Xu W. Clinical efficacy of posteromedial approaches for Haraguchi Type II fracture. Altern Ther Health Med. 2024;30:162–166. [PubMed] [Google Scholar]
- 25.Lanzetti RM, Lupariello D, Venditto T, Guzzini M, Ponzo A, De Carli A, Ferretti A. The role of diabetes mellitus and BMI in the surgical treatment of ankle fractures. Diabetes Metab Res Rev. 2018;34 doi: 10.1002/dmrr.2954. [DOI] [PubMed] [Google Scholar]
- 26.Xiao B, Lu M, Chen X, Qiu D, He Y, Li X. Study on the risk factors of postoperative wound complications in patients with ankle fracture. Int Wound J. 2024;21:e14845. doi: 10.1111/iwj.14845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu Y, Xu BY, Low SG, Low LL. Association of social support with rehabilitation outcome among older adults with hip fracture surgery: a prospective cohort study at post-acute care facility in Asia. J Am Med Dir Assoc. 2023;24:1490–1496. doi: 10.1016/j.jamda.2023.03.034. [DOI] [PubMed] [Google Scholar]
- 28.Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int. 1998;19:856–861. doi: 10.1177/107110079801901211. [DOI] [PubMed] [Google Scholar]
- 29.Neumann MV, Strohm PC, Reising K, Zwingmann J, Hammer TO, Suedkamp NP. Complications after surgical management of distal lower leg fractures. Scand J Trauma Resusc Emerg Med. 2016;24:146. doi: 10.1186/s13049-016-0333-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li HF, Yu T, Zhu XF, Wang H, Zhang YQ. Locking compression plate + T-type steel plate for postoperative weight bearing and functional recovery in complex tibial plateau fractures. World J Clin Cases. 2022;10:502–510. doi: 10.12998/wjcc.v10.i2.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kjørholt KE, Kristensen NR, Prieto-Alhambra D, Johnsen SP, Pedersen AB. Increased risk of mortality after postoperative infection in hip fracture patients. Bone. 2019;127:563–570. doi: 10.1016/j.bone.2019.07.023. [DOI] [PubMed] [Google Scholar]