Abstract
Objective: To compare the perioperative analgesic effect and safety of ultrasound-guided external oblique intercostal (EOI) block versus oblique subcostal transversus abdominis plane (OSTAP) block in patients receiving laparoscopic radical gastrectomy. Methods: A prospective study was conducted on sixty patients who underwent laparoscopic radical gastrectomy for gastric cancer at the First Affiliated Hospital of Nanchang University from January 2022 to September 2022. Patients were divided into the EOI block group and the OSTAP block group according to the random number table, with 30 patients in each group. Outcome measures were Visual Analog Scale scores assessed at rest and during activity at different time points, the number of effective analgesic pump compressions at 24 h post-surgery, the number of rescue analgesia at 24 h post-surgery, fentanyl consumption at 24 h post-surgery, and the occurrence of postoperative block-related complications. Results: The postoperative pain scores, measured at rest and during coughing, decreased in both groups. The pain scores at 12 h post-surgery were lower than those at 1 h and 6 h post-surgery in both groups (all P<0.05), and the pain scores at 24 h and 48 h post-surgery were also lower than those at 1 h, 6 h, and 12 h post-surgery (all P<0.05). The EOI block group exhibited reduced pain scores at 12 h and 24 h post-surgery compared to the OSTAP block group (all P<0.01). Additionally, the EOI group demonstrated a decreased number of effective analgesic pump compressions and a lower incidence of patients requiring rescue analgesia at 24 h post-surgery (all P<0.05), along with reduced cumulative fentanyl consumption at 6-12 h and 12-24 h post-surgery (P<0.05). There was no significant difference in the incidence of postoperative block-related complications between the two groups (P>0.05). Conclusion: Ultrasound-guided EOI block offers superior postoperative analgesic effect compared to OSTAP block in patients undergoing laparoscopic radical gastrectomy, without increasing the risk of complications postoperatively (Clinical registration number: ChiCTR2300070668).
Keywords: External oblique intercostal block, oblique subcostal transversus abdominis plane block, laparoscopic radical gastrectomy, postoperation pain, complication
Introduction
Gastric cancer is one of the most common malignancies in China, ranking the third in incidence and the second in mortality among all cancers, with an annual incidence rate of up to 485 per 100,000 individuals [1-3]. Radical gastrectomy is an effective and safe treatment for gastric cancer [4]. Compared to traditional open radical gastrectomy, laparoscopic radical gastrectomy offers several advantages, including reduced trauma, expedited postoperative recovery, and shorter hospital stays [5]. This minimally invasive approach has been endorsed in clinical guidelines for gastric cancer treatment in Japan [6]. Despite the advantages of laparoscopic techniques, postoperative pain remains a significant clinical concern, with some patients experiencing severe incision pain even after laparoscopic procedures [7]. Unmanaged pain can activate the sympathetic nervous system, leading to complications such as postoperative gastric dilatation and paralytic ileus. Moreover, pain can hinder effective coughing, increasing the risk of pulmonary infection and hypoxemia [8]. Current postoperative analgesic methods mainly include intravenous injection of non-steroidal anti-inflammatory drugs (NSAIDs) and opioids, local anesthetic infiltration for peritoneal and skin incisions, and regional anesthesia techniques [9]. However, local anesthetic infiltration often provides inadequate pain relief, and while intravenous NSAIDs and opioids are commonly employed, high doses of opioids may lead to an increased risk of adverse events [10,11]. Given these challenges, there is a pressing need to explore regional anesthesia techniques in the context of radical gastrectomy to alleviate postoperative pain, minimize the reliance on analgesic drugs, and improve patient safety.
According to the characteristics of laparoscopic radical gastrectomy, postoperative pain mainly originates from the anterior branches (T6-T10) of the intercostal nerves, which innervate the upper abdominal wall. Targeting these anterior branches (T6-T10) through anesthetic blocks has become a promising clinical approach for reducing postoperative pain. The gold standard for anesthesia in major laparoscopic abdominal surgeries remains general anesthesia combined with epidural block; however, while epidural blocks offer certain advantages in the context of multimodal analgesia, they are associated with risks such as hypotension and other complications [9,12]. The advent of ultrasound-guided techniques has facilitated the application of various fascial plane blocks in clinical practice. However, the subcostal transversus abdominis plane (TAP) block remains the sole analgesic method for upper abdominal surgery [13]. The oblique subcostal transversus abdominis plane (OSTAP) block, first described by Hebard in 2009, represents a modification of the TAP block [14]. OSTAP block allows for more cephalad spread of anesthetic compared to classical TAP block and has demonstrated potential for reducing postoperative pain in patients undergoing upper abdominal surgeries. Clinical evidence supports that the OSTAP block can achieve anesthesia in the T6-L1 region through the lateral spread of local anesthetic injected along the oblique subcostal line, effectively providing analgesia for upper abdominal surgeries [15,16]. However, a recent study has reported that the OSTAP block provides sensory blockade for only 90% of the middle abdominal and 26% of the lateral abdominal skin areas between T7 and T12 [17]. Given that pain in radical gastrectomy primarily originates from the T6-T10 region, the OSTAP block may not adequately cover the T6 nerve area.
In response to the clinical need for effective postoperative analgesia following upper abdominal surgery, Hesham et al. introduced the external oblique intercostal (EOI) block. Their anatomical study, conducted on two cadavers, supported the feasibility of this approach, demonstrating that injected dye could effectively spread to the lateral and anterior cutaneous branches of the intercostal nerves (T6/7-T10/11) [18]. By blocking these branches, the EOI block can provide continuous analgesia for the upper abdominal wall, achieving effective postoperative pain control after upper abdominal surgery. This technique has also shown promising results in clinical practice; for instance, Leigh White reported favorable outcomes in two patients with morbid obesity-one undergoing open distal pancreatectomy and the other open cholecystectomy, followed by postoperative analgesia via bilateral EOI catheterization, resulting in favorable effect and high patient satisfaction [19]. Notably, the EOI block can be performed under ultrasound guidance, with easily identifiable landmarks (T6 or T7), allowing for the injection site to be positioned away from the surgical field, thus minimizing the risk of incision infection [19].
Despite these advancements, the clinical application of the EOI block is still largely based on case reports and anatomical studies, with limited randomized controlled trials available [18,19]. Therefore, this study aims to compare the clinical efficacy of ultrasound-guided EOI and OSTAP blocks in patients undergoing radical gastrectomy.
Materials and methods
General information
This prospective study involved sixty patients undergoing laparoscopic radical gastrectomy for gastric cancer at the First Affiliated Hospital of Nanchang University from January 2022 to September 2022. Patients were assigned to two groups using a random number table: the EOI block group, which comprised 30 patients undergoing laparoscopic radical gastrectomy with ultrasound-guided EOI block, and the OSTAP block group, consisting of 30 patients undergoing laparoscopic radical gastrectomy with ultrasound-guided OSTAP block. All patients were anesthetized, with no withdrawals recorded. The age range of participants was 18 to 75 years, with a male-to-female ratio of 41:19. This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University.
Sample size calculation: The outcome hypothesis was primarily based on the reduction in VAS scores following treatment in both groups. The VAS of the two groups was 3 points before treatment, 1 point in the EOI block group and 3 points in the OSTAP block group after treatment, and the overall standard deviation was 1.5, which was calculated using the sample size calculation formula n = 2 × (σ2 × (Z1-α/2 + Z1-β)2)/d2. Determine the parameter values: population standard deviation σ=1.5, assuming the significance level is bilateral a=0.05, then Z1-α/2=1.96. Assuming that the test efficiency is 80% (1-β), Z1-β=0.84. The difference between the two means d=3-1=2. Calculate by substituting the formula N = 2 × (1.52 × (1.96 + 0.84)2)/22≈25, each group needs about 25 samples, plus 10% shedding rate, and the total sample size is 60 [20].
Inclusion criteria
Patients were eligible for inclusion based on the following criteria: 1) a confirmed diagnosis of gastric cancer with a planned laparoscopic radical gastrectomy [21]; 2) age between 18 and 75 years; 3) weight between 40 and 75 kg, with a body mass index of 18-28 kg/m2; 4) classified as American Society of Anesthesiologists (ASA) physical status I-II.
Exclusion criteria
The exclusion criteria included: 1) known allergies to any medications used in this study; 2) severe coagulation disorders; 3) infection at the puncture site; 4) liver or renal dysfunction, or severe heart or lung diseases; 5) a history of chronic pain or long-term use of opioids or non-steroidal anti-inflammatory drugs; 6) inability to cooperate in scoring outcome measures.
Methods
Preoperative preparation: All patients were fasted for 8 h and refrained from drinking for 4 h before surgery, without the administration of prophylactic drugs. Upon arrival in the operating room, patients were monitored using a 5-lead electrocardiogram, a noninvasive blood pressure monitor, and a pulse oximeter. Peripheral venipuncture was subsequently conducted. All blocks were performed using a 12L-RS high-frequency linear probe (5-13 MHz) from the Wisonic Ultrasound System. A 21-gauge, 100 mm nerve block needle (USG-Type CCR, Japan) was used to administer a mixture of local anesthetic comprising 10 mL of 1% ropivacaine (NAYB, AstraZeneca, Sweden), 5 mL of 2% lidocaine, and 5 mL of normal saline (NS). During the procedure, complications, surgical pain, anatomical structures, and needle visualization were also assessed.
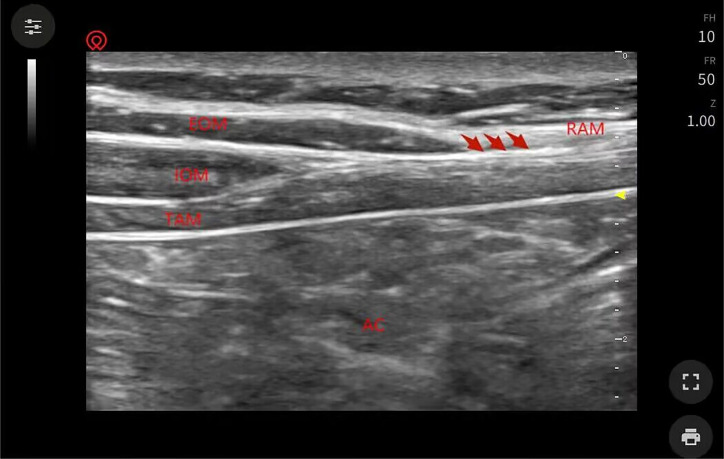
EOI block group: The EOI block was conducted under ultrasound guidance, following the method described by Hesham [18]. Patients were positioned supine, and the ultrasound probe was placed in the sagittal plane between the midclavicular line and the anterior axillary line at the level of the sixth rib, with the probe’s marker oriented toward the patient’s head. The sixth rib was identified by locating the tenth rib through horizontal plane visualization at the rib margins or by locating the seventh rib at the xiphoid level and moving the probe superiorly. The probe was then adjusted to create a paramedian sagittal oblique view, providing a short-axis view of the ribs, covering an area approximately 1 to 2 cm within the anterior axillary line. Structures visualized, from superficial to deep layers, included subcutaneous tissue, external oblique muscle, intercostal muscles (external, internal, and innermost intercostal), pleura, and lung. The entry point for the needle was determined at the superior aspect of the sixth rib, inside the anterior axillary line. The nerve block needle was inserted through the external oblique muscle, progressing from the superior medial to the inferior lateral direction (Figure 1), with the needle tip positioned at the tissue plane between the external oblique and intercostal muscles, between the sixth and seventh ribs. To facilitate muscle separation, about 3 mL of NS was injected. Following repeated aspiration, a mixture of 10 mL of 1% ropivacaine, 5 mL of 2% lidocaine, and 5 mL of NS were injected. The contralateral side was blocked using the same methods.
Figure 1.
Methods of ultrasound-guided EOI block. Note: EOI: external oblique intercostal.
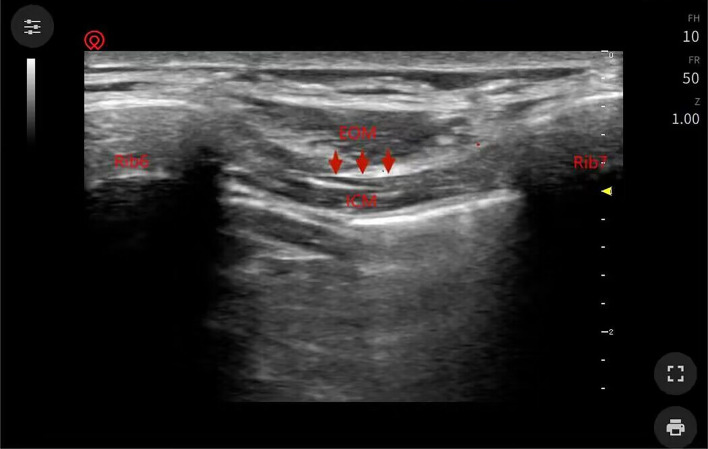
OSTAP block group: The OSTAP block was conducted according to the method described by Hebbard et al. [14]. Patients were positioned supine, and the ultrasound probe was oriented perpendicular to the abdominal wall, aligned parallel to the costal margin while being oblique to the sagittal plane. This orientation allowed visualization of structures from the rectus abdominis outward through the external abdominal oblique, internal abdominal oblique, and transverse abdominis (Figure 2). Using an in-plane technique, the nerve block needle was inserted along the costal margin, advancing from lateral to medial. Once the needle tip reached the transverse abdominis plane, situated between the transverse abdominis and rectus abdominis, about 3 mL of NS was injected to facilitate muscle separation. Following repeated aspiration, a mixture of 10 mL of 1% ropivacaine, 5 mL of 2% lidocaine, and 5 mL of NS were injected. The contralateral side was subjected to the same blocking methods (Figure 2).
Figure 2.
Methods of ultrasound-guided OSTAP block. Note: OSTAP: oblique subcostal transversus abdominis plane.
Following the operation, fentanyl was administered intravenously for pain relief. After the operation, fentanyl was injected intravenously for analgesia. The intravenous injection dose of fentanyl was 0.15 ug/kg/h using PCIA pump for 48 consecutive hours. If the patient’s pain was relieved to less than 3 points after pumping fentanyl, the pump speed was lowered; if the patient’s pain continued to exceed 3 points after pumping fentanyl, the pump speed was increased. If the analgesic effect of fentanyl was inadequate, an additional postoperative analgesic could be utilized. Specifically, if the VAS score remained above 4 after fentanyl treatment, Flurbiprofen Axetil injection was administered. A single dose of 50 mg intravenous injection, according to the degree of pain relief, was repeated to use the above dose, and the maximum dose did not exceed 200 mg.
Outcome measures
Clinical outcome measures
Primary outcome measures
The primary outcome was assessed using the Visual Analog Scale (VAS) to quantify subjective pain sensation. The VAS is a 10-cm scale, where 0 represents no pain and 10 indicates the worst pain imaginable. Patients were instructed to select a point on the scale that best reflected their pain level, yielding a corresponding VAS score [22]. Pain assessments were conducted at rest and during activity at 1, 6, 12, 24, and 48 hours after surgery. If patients were unable to engage in activity, they were advised to perform VAS assessment after a coughing maneuver.
Secondary outcome measures
Secondary outcomes included the number of effective analgesic pump compressions at 24 h post-surgery, defined as the number of anesthetic drug administration after compression.
Additionally, the number of patients requiring rescue analgesia at 24 h post-surgery was recorded; rescue analgesia consisted of 50 mg Flurbiprofen Axetil administered intravenously.
Fentanyl consumption was tracked during different postoperative intervals: 0-2 h, 2-6 h, 6-12 h, and 12-24 h.
Perioperative safety indicators
Postoperative block-related complications were monitored and compared between the two groups. Observed complications included bleeding, hematoma, local anesthetic toxicity, nerve injury and neuritis, allergic reaction, pruritus, and abdominal organ injury.
Statistical analysis
Data were analyzed using SPSS 17.0 software. Measurement data were expressed as mean ± standard deviation (x̅ ± SD). Independent samples t-tests were employed for comparisons between groups, while repeated measure analysis of variance, followed by post hoc LSD tests, was used for comparisons at different time points. Enumeration data were expressed as counts and percentages (n/%) and analyzed using Pearson’s chi-square test. A P value of less than 0.05 indicated a statistical significance.
Results
General and baseline data
There were no significant differences in age, gender, body mass index, tumor stage, tumor diameter, surgical approach, operation duration, ASA grade or presence of comorbidities between the two groups, showing comparability (P>0.05) (Table 1).
Table 1.
Comparison of general and baseline data
| Item | EOI block group (n=30) | OSTAP block group (n=30) | χ2/z/t | P |
|---|---|---|---|---|
| Age (years) | 58.3±12.9 | 60.9±8.2 | 0.910 | 0.367 |
| Gender | 0.693 | 0.450 | ||
| Male | 19 | 22 | ||
| Female | 11 | 8 | ||
| Body mass index (kg/m2) | 21.18±3.03 | 20.25±2.49 | 1.308 | 0.196 |
| Operation time (min) | 272.5±66.0 | 298.2±69.2 | 1.470 | 0.147 |
| Tumor stage (n) | 0.806 | 0.668 | ||
| Stage I | 10 | 9 | ||
| Stage II | 14 | 12 | ||
| Stage III | 6 | 9 | ||
| Tumor diameter (cm) | 4.8±0.9 | 4.9±1.1 | 0.385 | 0.701 |
| Surgical approach (n) | - | - | - | - |
| Total gastrectomy | 11 | 13 | 0.278 | 0.598 |
| Radical distal subtotal gastrectomy | 19 | 17 | ||
| ASA grade | - | - | - | - |
| Grade I | 3 | 4 | 0.162 | 0.688 |
| Grade II | 27 | 26 | ||
| Comorbidities | - | - | - | - |
| Hypertension | 9 | 12 | 0.659 | 0.417 |
| Diabetes | 10 | 7 | 0.739 | 0.390 |
| Other diseases | 4 | 5 | 0.131 | 0.718 |
Note: χ2 indicates chi-square test, z indicates rank sum test, and t indicates independent-samples t test. EOI: external oblique intercostal; OSTAP: oblique subcostal transversus abdominis plane; ASA: American Society of Anesthesiologists.
Comparison of VAS scores at rest at different time points
Postoperative pain scores at rest showed a downward trend in both groups. The pain scores at 12 h post-surgery were lower than those recorded at 1 h and 6 h post-surgery in both groups (all P<0.05). Similarly, pain scores at 24 h and 48 h post-surgery were reduced compared to those at 1 h, 6 h, and 12 h post-surgery (all P<0.05). The EOI block group exhibited significantly lower pain scores than the OSTAP block group at 12 h and 24 h post-surgery (all P<0.01) (Table 2).
Table 2.
Comparison of VAS scores at rest at different time points
| VAS pain scores at rest | EOI block group (n=30) | OSTAP block group (n=30) | χ2 | P |
|---|---|---|---|---|
| 1 h post-surgery | 2.77±0.90 | 2.93±0.78 | 0.765 | 0.447 |
| 6 h post-surgery | 2.33±1.09 | 2.67±0.80 | 1.346 | 0.183 |
| 12 h post-surgery | 1.53±0.68*,# | 2.23±0.77*,# | 3.718 | <0.001 |
| 24 h post-surgery | 1.23±0.43*,#,@ | 1.67±0.71*,#,@ | 2.856 | 0.006 |
| 48 h post-surgery | 1.17±0.83*,#,@ | 1.37±0.25*,#,@ | 1.264 | 0.211 |
| F | 24.011 | 26.802 | ||
| P | <0.001 | <0.001 |
Compared with 1 h post-surgery, P<0.05;
Compared with 6 h post-surgery, P<0.05;
Compared with 12 h post-surgery, P<0.05.
1 h post-surgery: postanesthesia care unit.
Comparison of VAS scores during activity at different time points
Postoperative pain scores during activity also showed a downward trend in both groups. Pain scores at 12 h post-surgery were lower than those at 1 h and 6 h post-surgery in both groups (all P<0.05). Furthermore, pain scores at 24 h and 48 h post-surgery were reduced compared to those at 1 h, 6 h, and 12 h post-surgery (all P<0.05). In the OSTAP block group, the pain score at 48 h post-surgery was lower than that at 24 h post-surgery (P<0.05). The EOI block group again demonstrated lower pain scores compared to the OSTAP block group at 12 h and 24 h post-surgery (all P<0.05) (Table 3).
Table 3.
Comparison of VAS scores during activity at different time points
| VAS pain scores during activity | EOI block group (n=30) | OSTAP block group (n=30) | χ2 | P |
|---|---|---|---|---|
| 1 h post-surgery | 5.33±1.09 | 5.23±0.90 | 0.387 | 0.700 |
| 6 h post-surgery | 4.76±1.31 | 4.97±1.00 | 1.554 | 0.126 |
| 12 h post-surgery | 3.37±0.89*,# | 4.20±0.92*,# | 3.556 | <0.001 |
| 24 h post-surgery | 2.93±1.20*,#,@ | 3.57±0.90*,#,@ | 2.313 | 0.024 |
| 48 h post-surgery | 2.43±1.17*,#,@ | 2.63±1.07*,#,@,& | 0.694 | 0.491 |
| F | 35.023 | 36.461 | ||
| P | <0.001 | <0.001 |
Compared with 1 h post-surgery, P<0.05;
Compared with 6 h post-surgery, P<0.05;
Compared with 12 h post-surgery, P<0.05;
Compared with 24 h post-surgery, P<0.05.
Comparison of perioperative analgesic effect indicators
The EOI block group had a reduced number of effective analgesic pump compressions at 24 h post-surgery, as well as a lower number of patients requiring rescue analgesia at the same time point (all P<0.05). Additionally, cumulative fentanyl consumption was significantly lower in the EOI block group during the intervals of 6-12 h and 12-24 h post-surgery compared to the OSTAP block group (P<0.05) (Tables 4 and 5).
Table 4.
Comparison of the number of analgesic pump compressions and patients requiring rescue analgesia
| Item | EOI block group (n=30) | OSTAP block group (n=30) | χ2/t | P |
|---|---|---|---|---|
| Number of effective analgesic pump compressions at 24 h post-surgery (times) | 6.82±2.02 | 10.72±2.79 | 6.202 | <0.001 |
| Number of patients with rescue analgesia at 24 h post-surgery [n (%)] | 2 (6.67) | 8 (26.67) | 4.320 | 0.038 |
Note: χ2 represents the chi-square test, and t represents the independent-samples t test. EOI: external oblique intercostal; OSTAP: oblique subcostal transversus abdominis plane.
Table 5.
Comparison of cumulative fentanyl consumption in different postoperative time periods
| Postoperative cumulative fentanyl consumption (μg) | EOI block group (n=30) | OSTAP block group (n=30) | t | P |
|---|---|---|---|---|
| 0-2 h | 37.46±4.03 | 37.88±4.07 | 0.402 | 0.689 |
| 2-6 h | 73.42±8.39 | 75.59±8.21 | 1.013 | 0.315 |
| 6-12 h | 189.45±32.45 | 258.74±47.46 | 6.601 | <0.001 |
| 12-24 h | 226.83±32.68 | 247.67±34.88 | 2.388 | 0.020 |
Note: t represents the independent-samples t test. EOI: external oblique intercostal; OSTAP: oblique subcostal transversus abdominis plane.
Comparison of incidence of nerve block-related complications
No significant differences were found in the incidence of postoperative complications between the two groups, such as bleeding, hematoma, nerve injury and local anesthetic toxicity, allergic reaction, pruritus, and abdominal organ injury (P>0.05) (Table 6).
Table 6.
Comparison of incidence of nerve block-related complications
| Nerve block-related complications | EOI block group (n=30) | OSTAP block group (n=30) | χ2 | P |
|---|---|---|---|---|
| Bleeding and hematoma | 0 (0.00%) | 0 (0.00%) | 0.000 | 1.000 |
| Nerve injury and neuritis | 0 (0.00%) | 0 (0.00%) | 0.000 | 1.000 |
| Local anesthetic toxicity | 1 (3.33%) | 0 (0.00%) | 1.017 | 0.313 |
| Allergic reaction | 0 (0.00%) | 1 (3.33%) | 1.017 | 0.313 |
| Pruritus | 0 (0.00%) | 1 (3.33%) | 1.017 | 0.313 |
| Abdominal organ injury | 0 (0.00%) | 0 (0.00%) | 0.000 | 1.000 |
| Total number of patients | 1 (3.33%) | 2 (6.67%) | 0.351 | 0.554 |
Note: χ2 represents the chi-square test. EOI: external oblique intercostal; OSTAP: oblique subcostal transversus abdominis plane.
Discussion
Radical gastrectomy is the most effective treatment for gastric cancer. With advancements in minimally invasive techniques, open radical gastrectomy is increasingly being supplanted by laparoscopic approaches. This shift is largely attributed to laparoscopic radical gastrectomy’s advantages, including reduced postoperative pain and expedited recovery compared to open surgery. However, patients often experience varying degrees of pain postoperatively due to factors such as prolonged operation time and the establishment of pneumoperitoneum [23]. Numerous studies have confirmed that implementing scientifically sound anesthesia methods tailored to specific surgical sites positively influences the stability of perioperative vital signs, mitigates postoperative pain, and improves prognosis [7,24].
Informed by previous theoretical frameworks and clinical findings, this study employed the EOI block as the anesthesia method for laparoscopic radical gastrectomy [18,19]. This choice aligns well with the surgical characteristics and postoperative analgesic requirements inherent to the procedure. Our findings showed that the EOI block resulted in significantly lower VAS pain scores at rest and during coughing at both 12 h and 24 h postoperatively compared to the commonly used OSTAP block. The OSTAP block, a modification of the TAP block, has been proved to provide effective anesthesia to the T6-L1 region by allowing local anesthetic to diffuse along the oblique subcostal line. This technique can yield significant postoperative analgesia in upper abdominal surgery [15,16]. However, pain after radical gastrectomy is not confined solely to the mid-abdominal operative area; it also extends to the lateral abdomen, where it plays a significant role in the overall pain experience. A recent clinical study has shown that the OSTAP block can cover only 90% of the middle abdominal and 26% of the lateral abdominal skin areas between T7 and T12 [17]. In contrast, the EOI block demonstrated a superior analgesic effect for the lateral abdominal wall. The analgesic mechanism of the EOI block is predicated on its ability to provide continuous coverage of the upper abdominal wall through the blockade of the lateral and anterior cutaneous branches (T6/7-T10/11) that spread to the intercostal nerve [18]. Previous studies have shown that the pain after upper abdominal surgery tends to be more severe than that after lower abdominal procedures [25]. Several mechanisms may underlie the analgesic effects observed with the EOI block: (1) It likely engages pain receptors and neurons within the local fascial plane, effectively achieving analgesia; (2) Analgesia may also result from systemic absorption of the anesthetic drugs; (3) Additionally, the diffusion of anesthetic drugs through fascial planes may play a role in pain relief. While the precise diffusion mechanisms of anesthetics between fascial planes remain unclear, it is understood that local anesthetics can permeate surrounding muscles and tissues via fascial pathways and ultimately enter systemic circulation [26,27]. In this study, significant analgesic benefits were observed following the EOI block in patients undergoing laparoscopic radical gastrectomy; however, further investigation is warranted to elucidate the specific mechanisms by which the EOI block exerts its analgesic effects.
In this study, we compared the analgesic outcomes following the use of the EOI block and the OSTAP block. The results showed a significant reduction in the number of effective analgesic pump compressions at 24 h post-surgery, as well as fewer patients requiring rescue analgesia at the same time point, in the EOI block group compared to the OSTAP block group. Additionally, cumulative fentanyl consumption was lower in the EOI block group during the 6-12 h and 12-24 h postoperative periods. Li et al. reported that pain intensity after upper abdominal surgery was greater than that after lower abdominal procedures, necessitating increased opioid analgesic usage in these patients [25]. Similarly, White et al. reported that the application of the EOI block significantly reduced opioid requirements in two patients with morbid obesity [19]. Furthermore, a significant reduction in opioid consumption was also noted in patients undergoing hepatectomy following EOI block. Existing studies have shown that EOI block may be the preferred anesthesia method for upper abdominal surgery to reduce opioid consumption [28]. This reduction in opioid needs may be related to the effective diffusion of anesthetics to the lateral and anterior cutaneous branches of the intercostal nerves (T6/7-T10/11) achieved through the EOI block, thereby ensuring continuous postoperative analgesia.
Our analysis of complications associated with both anesthesia methods revealed comparable incidence rates, suggesting that the EOI block does not introduce significant side effects during laparoscopic radical gastrectomy. This is consistent with previously reported results [19,28].
Limitations and future directions: This study is limited by its single-center design, and future multicenter studies are warranted to validate these findings. Additionally, while we observed significant analgesic effects with the EOI block, the specific mechanisms underlying this analgesia were not explored and warrant further investigation.
In conclusion, ultrasound-guided EOI block provides a superior postoperative analgesic effect compared to OSTAP block in the context of laparoscopic radical gastrectomy, with no side effects in clinical practice.
Acknowledgements
This work was supported by Science and Technology Plan Project of Jiangxi Provincial Health Commission (202410184): Comparison of the analgesic effects of ultrasound-guided external oblique intercostal muscle block and oblique rib lower abdominal transverse plane block for laparoscopic radical gastrectomy.
Disclosure of conflict of interest
None.
References
- 1.Feng RM, Zong YN, Cao SM, Xu RH. Current cancer situation in China: good or bad news from the 2018 global cancer statistics? Cancer Commun (Lond) 2019;39:22. doi: 10.1186/s40880-019-0368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 3.Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric cancer: epidemiology, risk factors, classification, genomic characteristics and treatment strategies. Int J Mol Sci. 2020;21:4012. doi: 10.3390/ijms21114012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gu L, Zhang K, Shen Z, Wang X, Zhu H, Pan J, Zhong X, Khadaroo PA, Chen P. Risk factors for duodenal stump leakage after laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2020;20:81–94. doi: 10.5230/jgc.2020.20.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li J, Li S, Xi H, Liu P, Liang W, Gao Y, Wang C, Wei B, Chen L, Tang Y, Qiao Z. Effect of preoperative nutrition therapy type and duration on short-time outcomes in gastric cancer patient with gastric outlet obstruction. Chin J Cancer Res. 2021;33:232–242. doi: 10.21147/j.issn.1000-9604.2021.02.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition) Gastric Cancer. 2021;24:1–21. doi: 10.1007/s10120-020-01042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu M, Qi Y, He H, Zhang S, Mei Y. Effect of quadratus lumborum block on postoperative cognitive function in elderly patients undergoing laparoscopic radical gastrectomy: a randomized controlled trial. BMC Geriatr. 2021;21:238. doi: 10.1186/s12877-021-02179-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Chen C, Hu Y, Zhu C, Luo X, Wang L, Wang X, Sun X, Chen X, Xie W, Lou H, Huang X, Li C, Xu J, Xue X, Shen X. Three-dimensional ex vivo culture for drug responses of patient-derived gastric cancer tissue. Front Oncol. 2020;10:614096. doi: 10.3389/fonc.2020.614096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desai N, El-Boghdadly K, Albrecht E. Epidural vs. transversus abdominis plane block for abdominal surgery - a systematic review, meta-analysis and trial sequential analysis. Anaesthesia. 2021;76:101–117. doi: 10.1111/anae.15068. [DOI] [PubMed] [Google Scholar]
- 10.Mulier JP. Is opioid-free general anesthesia for breast and gynecological surgery a viable option? Curr Opin Anaesthesiol. 2019;32:257–262. doi: 10.1097/ACO.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 11.Koepke EJ, Manning EL, Miller TE, Ganesh A, Williams DGA, Manning MW. The rising tide of opioid use and abuse: the role of the anesthesiologist. Perioper Med (Lond) 2018;7:16. doi: 10.1186/s13741-018-0097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qin C, Liu Y, Xiong J, Wang X, Dong Q, Su T, Liu J. The analgesic efficacy compared ultrasound-guided continuous transverse abdominis plane block with epidural analgesia following abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20:52. doi: 10.1186/s12871-020-00969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. 2018;43:341–346. doi: 10.1097/AAP.0000000000000750. [DOI] [PubMed] [Google Scholar]
- 14.Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35:436–441. doi: 10.1097/aap.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 15.Fernández Martín MT, López Álvarez S. BRILMA and PEC blocks: Simpler and more adequate options in radical breast surgery. Rev Esp Anestesiol Reanim (Engl Ed) 2018;65:478–479. doi: 10.1016/j.redar.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Sanllorente-Sebastián R, de Vicente-Lorenzo JM, Mediavilla-Herrera FJ, Gutiérrez-García S, Alario-Poza IS, Bustinza-Beaskoetxea Z. Case report: serratus intercostal plane block/BRILMA and sedation for mastectomy in a high risk patient. Rev Esp Anestesiol Reanim (Engl Ed) 2019;66:46–48. doi: 10.1016/j.redar.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Shi K, Xia Y, Zhang X, Papadimos TJ, Xu X, Wang Q. Sensory assessment and regression rate of bilateral oblique subcostal transversus abdominis plane block in volunteers. Reg Anesth Pain Med. 2018;43:174–179. doi: 10.1097/AAP.0000000000000715. [DOI] [PubMed] [Google Scholar]
- 18.Elsharkawy H, Kolli S, Soliman LM, Seif J, Drake RL, Mariano ER, El-Boghdadly K. The external oblique intercostal block: anatomic evaluation and case series. Pain Med. 2021;22:2436–2442. doi: 10.1093/pm/pnab296. [DOI] [PubMed] [Google Scholar]
- 19.White L, Ji A. External oblique intercostal plane block for upper abdominal surgery: use in obese patients. Br J Anaesth. 2022;128:e295–e297. doi: 10.1016/j.bja.2022.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Wang X, Ji X. Sample size estimation in clinical research: from randomized controlled trials to observational studies. Chest. 2020;158:S12–S20. doi: 10.1016/j.chest.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 21.National Health Commission of the People’s Republic of China. Diagnosis criteria for primary gastric cancer: WS316-2010. Beijing: Standards Press of China; 2010. [Google Scholar]
- 22.Dahlstrand U, Sandblom G, Nordin P, Wollert S, Gunnarsson U. Chronic pain after femoral hernia repair: a cross-sectional study. Ann Surg. 2011;254:1017–1021. doi: 10.1097/SLA.0b013e31822ba9b6. [DOI] [PubMed] [Google Scholar]
- 23.Jiao J, Liu S, Chen C, Maimaiti A, He Q, Hu S, Yu W. Comparative study of laparoscopic radical gastrectomy and open radical gastrectomy. J Minim Access Surg. 2020;16:41–46. doi: 10.4103/jmas.JMAS_155_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balocco AL, López AM, Kesteloot C, Horn JL, Brichant JF, Vandepitte C, Hadzic A, Gautier P. Quadratus lumborum block: an imaging study of three approaches. Reg Anesth Pain Med. 2021;46:35–40. doi: 10.1136/rapm-2020-101554. [DOI] [PubMed] [Google Scholar]
- 25.Li TT, Chang QY, Xiong LL, Chen YJ, Li QJ, Liu F, Wang TH. Patients with gastroenteric tumor after upper abdominal surgery were more likely to require rescue analgesia than lower abdominal surgery. BMC Anesthesiol. 2022;22:156. doi: 10.1186/s12871-022-01682-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haskins SC, Memtsoudis SG. Fascial plane blocks for cardiac surgery: new frontiers in analgesia and nomenclature. Anesth Analg. 2020;131:125–126. doi: 10.1213/ANE.0000000000004744. [DOI] [PubMed] [Google Scholar]
- 27.Chin KJ, Lirk P, Hollmann MW, Schwarz SKW. Mechanisms of action of fascial plane blocks: a narrative review. Reg Anesth Pain Med. 2021;46:618–628. doi: 10.1136/rapm-2020-102305. [DOI] [PubMed] [Google Scholar]
- 28.Dieu A, Huynen P, Lavand’homme P, Beloeil H, Freys SM, Pogatzki-Zahn EM, Joshi GP, Van de Velde M PROSPECT Working Group of the European Society of Regional Anaesthesia and Pain Therapy (ESRA) Pain management after open liver resection: procedure-specific postoperative pain management (PROSPECT) recommendations. Reg Anesth Pain Med. 2021;46:433–445. doi: 10.1136/rapm-2020-101933. [DOI] [PMC free article] [PubMed] [Google Scholar]