Abstract
Objective: To evaluate the response and safety of combining acupuncture based on the Dunhuang “Moxibustion Classic” with carbamazepine in the treatment of neuropathic tinnitus. Methods: A retrospective analysis was conducted on 105 patients with neuropathic tinnitus treated at The First People’s Hospital of Lanzhou City from January 2019 to February 2023. Of these, 49 patients received acupuncture based on the Dunhuang “Moxibustion Classic” (research group), while 56 patients received conventional acupuncture (control group). Both groups were treated with carbamazepine in combination. The Tinnitus Handicap Inventory (THI), Tinnitus Evaluation Questionnaire (TEQ), Visual Analogue Scale for Aural Fullness (VAS), Hamilton Anxiety Rating Scale (HAMA), and Hamilton Depression Rating Scale (HAMD) scores were compared between the two groups. Treatment response and Pittsburgh Sleep Quality Index (PSQI) scores were also analyzed. Logistic regression analysis was performed to identify risk factors affecting patients’ sleep quality. Results: The overall response rate in the control group was significantly lower than that in the research group (P = 0.037). After treatment, THI, PSQI, TEQ, VAS, HAMA, and HAMD scores were higher in the control group than in the research group (P<0.05). The incidence of adverse reactions was significantly higher in the control group than in the research group (P = 0.025). Multivariate logistic regression analysis identified treatment options (P = 0.002, OR = 8.612, 95% CI = 2.466-39.565), disease duration (P = 0.687, OR = 0.779, 95% CI = 0.219-2.544), pre-treatment THI (P = 0.002, OR = 7.061, 95% CI = 2.17-26.368), pre-treatment TEQ (P<0.001, OR = 14.654, 95% CI = 4.196-65.376), and pre-treatment HAMA (P = 0.019, OR = 3.805, 95% CI = 1.271-12.209) as independent risk factors for impaired sleep quality. Conclusion: The combination of Dunhuang “Moxibustion Classic” acupuncture with carbamazepine is an effective and safe treatment for neuropathic tinnitus, leading to greater improvements in symptoms, sleep quality, anxiety, and depression compared to conventional acupuncture.
Keywords: Acupuncture, carbamazepine, neuropathic tinnitus, efficacy, safety
Introduction
Neuropathic tinnitus is characterized by the subjective perception of sound in the ears without any external stimuli. This sound can be monotone or mixed, vary in pitch, and occur intermittently or continuously [1,2]. Tinnitus may manifest as an independent condition or as a symptom of various underlying diseases [3]. Persistent or recurrent tinnitus significantly affects patients’ quality of life, disrupting daily activities, sleep, and cognitive functions [4]. Clinically, tinnitus is a prevalent condition, affecting up to 30% of the population, with a subset of patients experiencing severe emotional and psychological distress, leading to impaired functioning in personal and professional domains [5]. In extreme cases, neuropathic tinnitus can lead to suicidal tendencies due to its profound impact on mental and physical health.
Currently, there is no definitive treatment for neuropathic tinnitus; therefore, this condition remains challenging to manage effectively. Western medicine primarily relies on treatments including neurotrophic agents, circulation-improving drugs, hyperbaric oxygen therapy, habituation therapy, local anesthesia, and masking therapy. While these approaches can offer symptomatic relief, they are often limited in their long-term efficacy [6]. Many patients experience only temporary benefits, with symptoms frequently recurring after treatment. Additionally, these treatments can be costly and may involve complex regimens that are difficult for patients to maintain. The invasive nature of some interventions, coupled with the potential for adverse side effects, further reduces their acceptability among patients [7]. The unpredictable outcomes and the lack of a universally effective solutions contribute to the overall dissatisfaction with current treatment options. This situation underscores the urgent need for more effective, sustainable, and patient-friendly therapeutic approaches that can provide long-lasting relief and better quality of life for those suffering from neuropathic tinnitus.
The “Moxibustion Classic”, discovered in 1900 in the Dunhuang Mogao Caves in Gansu Province, China, is one of the earliest extant monographs on moxibustion [8]. This ancient text covers a wide range of diseases, and research has shown that the moxibustion techniques described in the “Moxibustion Classic” are notably effective and deserve further exploration [9]. The techniques emphasize multiple moxibustion sessions with significant doses, focusing on treating difficult and severe illnesses. Methods such as heavy moxibustion are believed to warm the meridians, disperse cold, harmonize qi and blood, and provide pain relief, which could be beneficial in treating neuropathic tinnitus [10]. Given that the etiology of neuropathic tinnitus involves blood circulation disorders in the ear and neurological abnormalities, the moxibustion methods from the “Moxibustion Classic” that stimulate specific acupoints might improve local and systemic blood circulation, potentially alleviating tinnitus symptoms.
This study explored the response and safety of combining the Dunhuang “Moxibustion Classic” acupuncture with carbamazepine for treating neuropathic tinnitus. Given the significant distress caused by neuropathic tinnitus and the limited efficacy of current treatments, there is a clear need for new therapeutic approaches. This innovative study retrospectively compared the combined “Moxibustion Classic” acupuncture and carbamazepine treatment with conventional acupuncture plus carbamazepine, aiming to provide a more holistic and effective treatment options for neuropathic tinnitus in clinical practice.
Materials and methods
General information
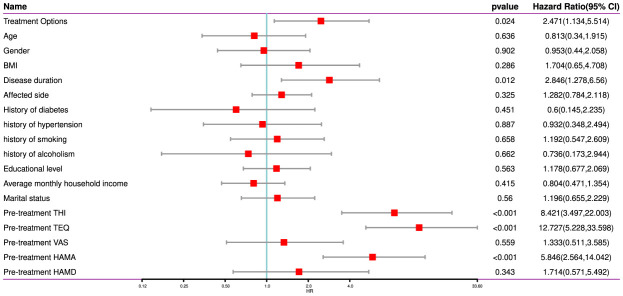
A retrospective analysis was conducted on patients with neuropathic tinnitus treated at The First People’s Hospital of Lanzhou City from January 2019 to February 2023. The study was approved by The First People’s Hospital of Lanzhou City medical ethics committee. A flow chart was constructed to provide an overview of the research process (Figure 1).
Figure 1.
Study flow and sample selection diagram.
Inclusion criteria: (1) Patients primarily presenting with tinnitus, meeting the diagnostic criteria for neuropathic tinnitus in both Chinese and Western medicine [11]. (2) Initial tinnitus diagnosis, with no related traditional Chinese medicine treatment in the past month. (3) No use of other related drugs or interventions for tinnitus during the study period. (4) Complete clinical data.
Exclusion criteria: (1) Pregnant and lactating women. (2) Tinnitus caused by trauma, tumors, systemic diseases, vascular tinnitus, muscle tinnitus, or complete deafness with tinnitus. (3) Conductive tinnitus of various causes. (4) Tinnitus patients with total hearing loss. (5) Severe cardiovascular, liver, kidney, or hematopoietic system complications, and other acute and chronic diseases causing tinnitus.
Treatment plans
Research group: This group was treated using the Dunhuang “Moxibustion Classic” acupuncture method, selecting acupoints based on the principles of yin-yang, five elements, and eight trigrams. Main acupoints included Hairline, Four Heavenly Courts, Dazhui, Hand Marrow Hole, Foot Five Boats, Foot Numbness, Zhongfeng, and Juegu. Differentiation acupoints included Hegu, Tianzhu, and Quchi for wind evil invasion; Taichong, Qiuxu, and Xiakai for liver and gallbladder fire; Fenglong for phlegm fire obstruction; Hegu and Xuehai for qi stagnation and blood stasis; Taixi and Zhaohai for kidney essence deficiency; Shenshu and Guanyuan for kidney yuan deficiency; Zusanli and Sanyinjiao for spleen qi deficiency; Shenmen and Sanyinjiao for heart and spleen blood deficiency. In severe cases, additional acupoints such as Four Heavenly Courts, Fengchi, Wangu, and Tianzhu were used. Needles were retained for 10 minutes using twisting and tonifying methods, with even supplementation and drainage for the main acupoints. Adjunct acupoints were treated with tonifying for deficiency and draining for excess evidence. Each session lasted 30 minutes, with 10 sessions per course, over 3 courses.
Control group: This group was treated with conventional acupuncture methods for neuropathic tinnitus. Main acupoints included Ermen, Tinggong, Tinghui, Yifeng, and Waiguan. Differentiation acupoints included Yingxiang, Hegu, Quchi, and Fengchi for wind evil invasion; Taichong, Qiuxu, Yanglingquan, and Xiakai for liver and gallbladder fire; Laogong and Fenglong for phlegm fire obstruction; Hegu and Xuehai for qi stagnation and blood stasis; Taixi and Rangu for kidney essence deficiency; Shenshu and Guanyuan for kidney yuan deficiency; Zusanli and Sanyinjiao for spleen qi deficiency; Shenmen and Sanyinjiao for heart and spleen blood deficiency. Needles were retained for 30 minutes daily using twisting and tonifying methods, with 10 sessions per course over 3 courses.
Medication: Both groups received carbamazepine tablets (Jiangsu Pengyao Pharmaceutical Co., Ltd.; specification: 0.1 g × 100 s; National Medicine Standard H32021018), administered with warm water, 3 times/day at 0.1 g/time, for 4 weeks.
Grouping of cases
According to the inclusion and exclusion criteria, 105 cases were included in the study, with 49 patients in the research group and 56 patients in the control group.
Clinical data collection
Clinical data and scoring information were obtained from outpatient follow-up records and electronic medical records. Clinical data included age, sex, body mass index (BMI), disease duration, affected side, history of diabetes, hypertension, smoking, drinking, education level, average monthly household income, marital status, clinical efficacy, and adverse reactions. Scoring information included the Tinnitus Handicap Inventory (THI), Pittsburgh Sleep Quality Index (PSQI), Tinnitus Evaluation Questionnaire (TEQ), Visual Analogue Scale for Aural Fullness (VAS), Hamilton Anxiety Rating Scale (HAMA), and Hamilton Depression Rating Scale (HAMD). All the scales were administered before treatment and after one month of treatment.
Functional scores
(1) THI [12] assesses the impact of tinnitus on daily life, including emotional, social, and work-related interference. Scores range from 0 to 100, with higher scores indicating a greater impact on life, suggesting the need for more medical or psychological support.
(2) PSQI [13] evaluates sleep quality and patterns over the past month, including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Scores range from 0 to 21, with higher scores indicating poorer sleep quality, suggesting potential sleep disorders.
(3) TEQ [14] measures tinnitus symptoms comprehensively, including frequency, duration, intensity, and impact on quality of life, providing a reference for clinical treatment. Scores range from 0 to 80, with higher scores indicating more severe symptoms and impact, necessitating deeper treatment and intervention.
(4) VAS [15] assesses the subjective degree of aural fullness, with patients marking the intensity on a line, providing a simple and intuitive symptom assessment. Scores range from 0 to 10, with higher scores indicating more severe fullness, suggesting further diagnosis and treatment.
(5) HAMA [16] measures the severity of anxiety symptoms, including various aspects of psychic and somatic anxiety, helping clinicians diagnose and monitor anxiety. Scores range from 0 to 56, with higher scores indicating more severe anxiety, potentially requiring more psychological or pharmacological intervention.
(6) HAMD [17] assesses the severity of depressive symptoms, including emotional, cognitive, and somatic aspects, widely used in the diagnosis, assessment, and monitoring of depression. Scores range from 0 to 52, with higher scores indicating more severe depression, suggesting the need for more active treatment and management.
Efficacy evaluation
Clinical efficacy was evaluated based on the Tinnitus Severity Grading and Efficacy Evaluation Standards [18]: (1) Cured: Hearing function recovers to normal, and tinnitus completely disappears with no recurrence. (2) Significantly effective: Slight tinnitus only heard in quiet environments, with no significant hearing impairment. (3) Effective: Tinnitus reduces from moderate or severe to mild. (4) Ineffective: No significant change in tinnitus symptoms, or hearing continues to decline. Total response rate = (number of cured + significantly effective + effective cases)/total cases × 100%.
Outcome measures
Primary outcomes
(1) The changes in various functional scores were evaluated before and one month after treatment. (2) The incidence of adverse reactions during treatment were compared between the two groups. (3) The patients were classified based on their post-treatment PSQI scores, those with PSQI score >5 points in a sleep quality impairment group and those with a score ≤5 points in a non-impairment group. Then, logistic regression analysis was conducted to identify risk factors affecting patients’ sleep quality.
Secondary outcomes
(1) Clinical information of patients was collected and compared between the two groups. (2) The clinical efficacy was compared between the two groups one a month after treatment.
Statistical analysis
Data were statistically analyzed using SPSS 20.0 software. Count data were expressed as rates (%) and analyzed using chi-square tests. The distribution of measurement data was assessed using the Kolmogorov-Smirnov test. Normally distributed data were expressed as mean ± standard deviation (Mean ± SD) and analyzed using independent sample t-tests for between-group comparisons and paired t-tests for within-group comparisons. Non-normally distributed data were expressed as quartiles P50 (P25, P75). Logistic regression analysis was employed to identify risk factors affecting patients’ sleep quality, using the enter method. A P-value of <0.05 was considered statistically significant.
Results
Baseline data
Comparison of baseline data between the research group and the control group revealed no statistical differences in age, sex, BMI, disease duration, affected side, history of diabetes, hypertension, smoking, drinking, education level, average monthly household income, or marital status (Table 1).
Table 1.
Comparison of baseline data
| Factors | Control group (n = 56) | Research group (n = 49) | χ2 Value | P Value |
|---|---|---|---|---|
| Age | ||||
| ≥45 years | 41 (73.21%) | 35 (71.43%) | 0.042 | 0.838 |
| <45 years | 15 (26.79%) | 14 (28.57%) | ||
| Gender | ||||
| Male | 32 (57.14%) | 25 (51.02%) | 0.395 | 0.530 |
| Female | 24 (42.86%) | 24 (48.98%) | ||
| BMI | ||||
| ≥25 kg/m2 | 10 (17.86%) | 11 (22.45%) | 0.344 | 0.557 |
| <25 kg/m2 | 46 (82.14%) | 38 (77.55%) | ||
| Disease duration | ||||
| ≥1 year | 25 (44.64%) | 18 (36.73%) | 0.676 | 0.411 |
| <1 year | 31 (55.36%) | 31 (63.27%) | ||
| Affected side | ||||
| Left | 19 (33.93%) | 15 (30.61%) | 0.162 | 0.922 |
| Right | 21 (37.5%) | 20 (40.82%) | ||
| Both | 16 (28.57%) | 14 (28.57%) | ||
| History of diabetes | ||||
| Yes | 4 (7.14%) | 6 (12.24%) | 0.789 | 0.374 |
| No | 52 (92.86%) | 43 (87.76%) | ||
| History of hypertension | ||||
| Yes | 12 (21.43%) | 8 (16.33%) | 0.441 | 0.507 |
| No | 44 (78.57%) | 41 (83.67%) | ||
| History of smoking | ||||
| Yes | 32 (57.14%) | 30 (61.22%) | 0.18 | 0.671 |
| No | 24 (42.86%) | 19 (38.78%) | ||
| History of drinking | ||||
| Yes | 4 (7.14%) | 5 (10.2%) | 0.312 | 0.576 |
| No | 52 (92.86%) | 44 (89.8%) | ||
| Education level | ||||
| ≤ Primary school | 6 (10.71%) | 7 (14.29%) | 0.590 | 0.745 |
| Junior high school | 23 (41.07%) | 17 (34.69%) | ||
| ≥ High school | 27 (48.21%) | 25 (51.02%) | ||
| Monthly income | ||||
| ≤3000 (RMB) | 32 (57.14%) | 25 (51.02%) | 1.901 | 0.386 |
| 3001-4499 (RMB) | 18 (32.14%) | 14 (28.57%) | ||
| ≥4500 (RMB) | 6 (10.71%) | 10 (20.41%) | ||
| Marital status | ||||
| Married | 45 (80.36%) | 42 (85.71%) | 2.062 | 0.357 |
| Divorced | 3 (5.36%) | 4 (8.16%) | ||
| Other | 8 (14.29%) | 3 (6.12%) |
Note: BMI = Body Mass Index.
Clinical efficacy evaluation
The overall response rate in the control group was significantly lower than that in the research group (P = 0.037), showing a statistical difference (Table 2).
Table 2.
Clinical efficacy evaluation
| Group | Cured | Significantly effective | Effective | Ineffective | Total response rate |
|---|---|---|---|---|---|
| Control group (n = 56) | 24 (42.86%) | 10 (17.86%) | 9 (16.07%) | 13 (23.21%) | 43 (76.79%) |
| Research group (n = 49) | 25 (51.02%) | 13 (26.53%) | 7 (14.29%) | 4 (8.16%) | 45 (91.84%) |
| χ2 Value | 4.363 | ||||
| P Value | 0.037 |
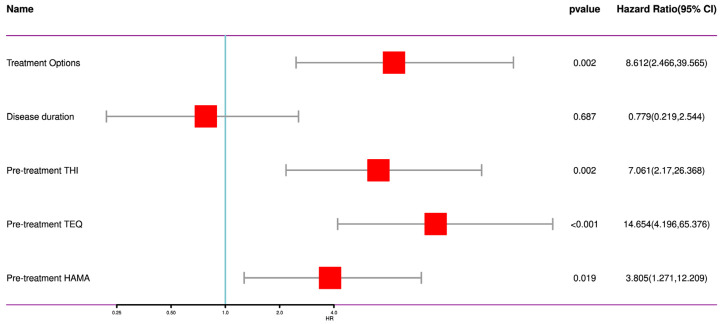
Changes in THI and PSQI scores before and after treatment
Comparison of THI and PSQI scores between the two groups before treatment reveal-ed no statistical differences (P>0.05). Within each group, post-treatment scores significantly decreased compared to pre-treatment scores (P<0.001). After treatment, THI and PSQI scores in the control group were higher than those in the research group, showing statistical differences (P<0.05, Figure 2).
Figure 2.
Changes in THI and PSQI scores before and after treatment. A. THI Scores; B. PSQI Scores. THI = Tinnitus Handicap Inventory, PSQI = Pittsburgh Sleep Quality Index; nsP>0.05, and ***P<0.001.
Changes in TEQ and VAS scores before and after treatment
Comparison of TEQ and VAS scores between the two groups before treatment also showed no significant differences (P>0.05). Both groups experienced significant decreases in TEQ and VAS scores post-treatment compared to pre-treatment (P<0.001). After treatment, TEQ and VAS scores in the control group were higher than those in the research group, with statistically significant differences (P<0.05, Figure 3).
Figure 3.
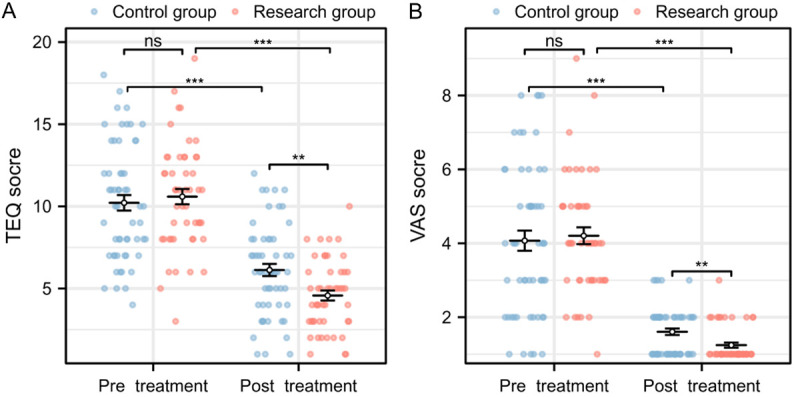
Changes in TEQ and VAS scores before and after treatment. A. TEQ Scores; B. VAS Scores. TEQ = Tinnitus Evaluation Questionnaire, VAS = Visual Analogue Scale for Aural Fullness; nsP>0.05, and ***P<0.001.
Changes in HAMA and HAMD scores before and after treatment
Comparison of HAMA and HAMD scores between the two groups before treatment revealed no statistical differences (P>0.05). Post-treatment, both groups showed significant decreases in HAMA and HAMD scores compared to pre-treatment (P<0.001). However, after treatment, HAMA and HAMD scores in the control group were higher than those in the research group, with significant differences (P<0.05, Figure 4).
Figure 4.
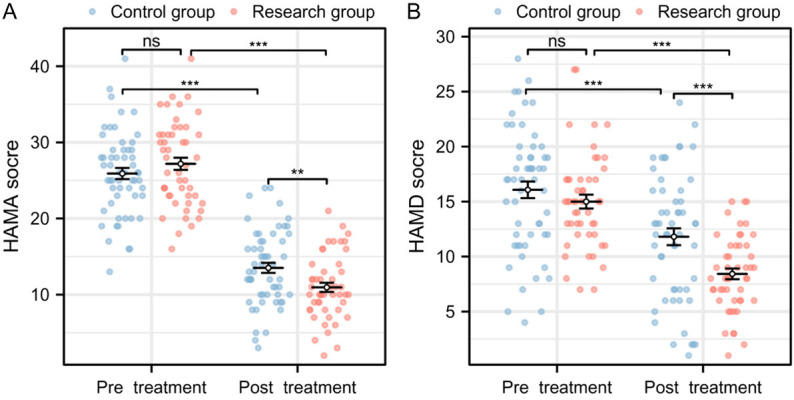
Changes in HAMA and HAMD scores before and after treatment. A. HAMA Scores; B. HAMD Scores. HAMA = Hamilton Anxiety Rating Scale, HAMD - Hamilton Depression Rating Scale; nsP>0.05, and ***P<0.001.
Comparison of the incidence of adverse reactions in patients during treatment
The incidence of adverse reactions in the control group during treatment was significantly higher than that in the research group, showing statistical differences (P = 0.025, Table 3).
Table 3.
Adverse reactions statistics
| Group | Rash | Drowsiness | Bone marrow suppression | Gastrointestinal reaction | Total incidence |
|---|---|---|---|---|---|
| Control group (n = 56) | 3 (5.36%) | 3 (5.36%) | 2 (3.57%) | 4 (7.14%) | 12 (21.43%) |
| Research group (n = 49) | 1 (2.04%) | 1 (2.04%) | 0 (0.00%) | 1 (2.04%) | 3 (6.12%) |
| χ2 Value | 5.000 | ||||
| P Value | 0.025 |
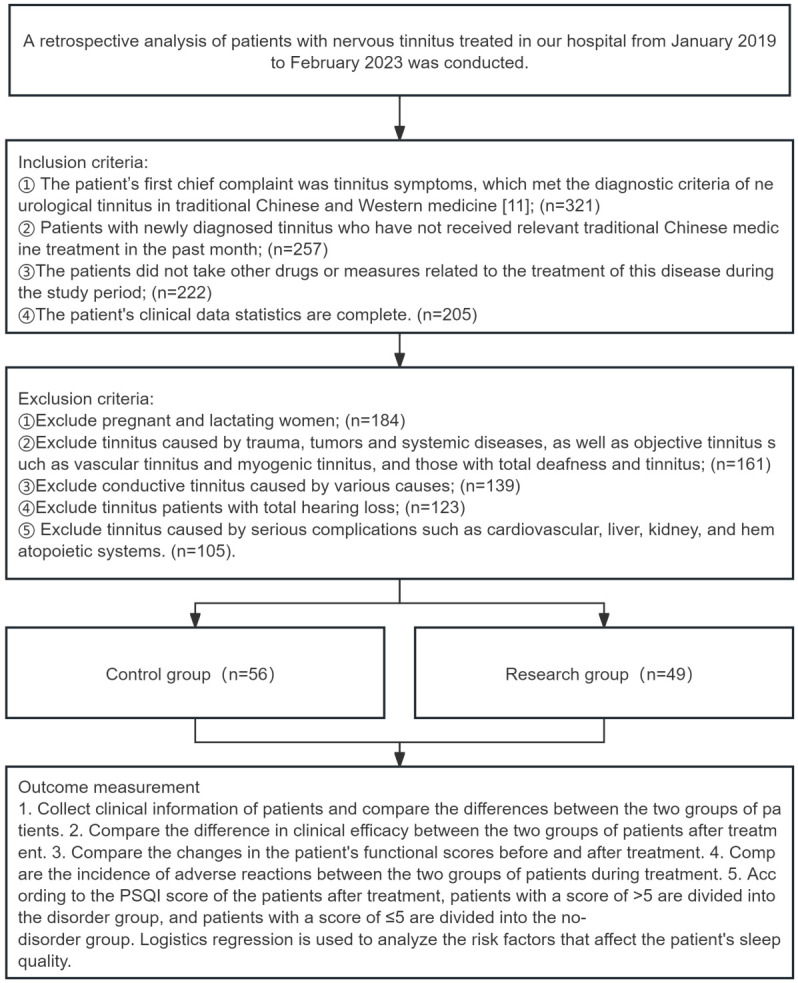
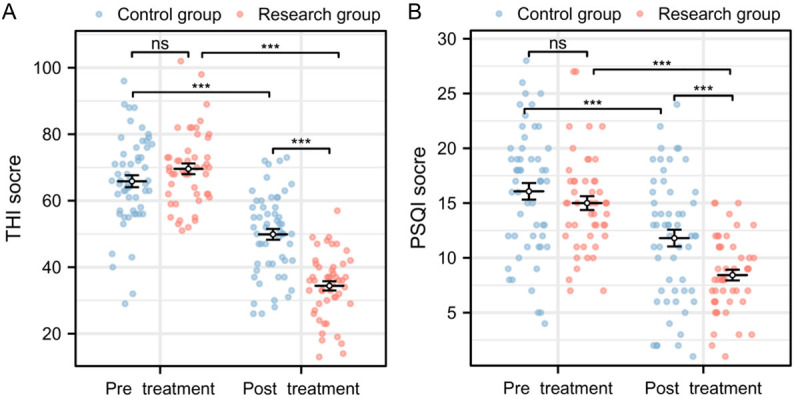
Analysis of risk factors affecting sleep quality
According to post-treatment PSQI scores, patients were divided into a sleep quality impairment group (n = 51) and a non-impairment group (n = 54). Data were classified and assigned based on the optimal cut-off values of the scores (Table 4). Univariate and multivariate logistics regression analyses identified treatment options (P = 0.002, OR = 8.612, 95% CI = 2.466-39.565), disease duration (P = 0.687, OR = 0.779, 95% CI = 0.219-2.544), pre-treatment THI (P = 0.002, OR = 7.061, 95% CI = 2.17-26.368), pre-treatment TEQ (P<0.001, OR = 14.654, 95% CI = 4.196-65.376), and pre-treatment HAMA (P = 0.019, OR = 3.805, 95% CI = 1.271-12.209) as independent risk factors for sleep quality impairment (Figures 5, 6).
Table 4.
Assignment table
| Factors | Assignment content |
|---|---|
| Treatment Options | Control group = 0, Research group = 1 |
| Age | ≥45 years = 0, <45 years = 1 |
| Gender | Male = 0, Female = 1 |
| BMI | ≥25 kg/m2 = 0, <25 kg/m2 = 1 |
| Disease duration | ≥1 year = 0, <1 year = 1 |
| Affected side | Left = 0, Right = 1, Both = 2 |
| History of diabetes | Present = 0, Absent = 1 |
| History of hypertension | Present = 0, Absent = 1 |
| History of smoking | Present = 0, Absent = 1 |
| History of alcoholism | Present = 0, Absent = 1 |
| Educational level | ≤ Primary = 0, Middle = 1, ≥ High = 2 |
| Average monthly household income | ≤3000 yuan = 0, 3001-4499 yuan = 1, ≥4500 yuan = 2 |
| Marital status | Married = 0, Divorced = 1, Other = 2 |
| Pre-treatment THI | ≥70.5 = 0, <70.5 = 1 |
| Pre-treatment TEQ | ≥10.5 = 0, <10.5 = 1 |
| Pre-treatment VAS | ≥2.5 = 0, <2.5 = 1 |
| Pre-treatment HAMA | ≥25.5 = 0, <25.5 = 1 |
| Pre-treatment HAMD | ≥21.5 = 0, <21.5 = 1 |
| Sleep Quality | Impaired = 0, Not impaired = 1 |
Note: BMI = Body Mass Index, THI = Tinnitus Handicap Inventory, TEQ = Tinnitus Evaluation Questionnaire, VAS = Visual Analogue Scale for Aural Fullness, HAMA = Hamilton Anxiety Rating Scale, HAMD = Hamilton Depression Rating Scale.
Figure 5.
Univariate analysis of factors affecting sleep quality. Note: BMI = Body Mass Index, THI = Tinnitus Handicap Inventory, TEQ = Tinnitus Evaluation Questionnaire, VAS = Visual Analogue Scale for Aural Fullness, HAMA = Hamilton Anxiety Rating Scale, HAMD = Hamilton Depression Rating Scale.
Figure 6.
Multivariate analysis of factors affecting sleep quality. Note: THI = Tinnitus Handicap Inventory, TEQ = Tinnitus Evaluation Questionnaire, HAMA = Hamilton Anxiety Rating Scale.
Discussion
Neuropathic tinnitus is a growing and challenging condition in otology, increasingly affecting younger individuals [19]. Mild symptoms can cause anxiety and depression, while severe condition may lead to suicidal tendencies, significantly disrupting daily life [20]. Western medical treatments, such as medication and sound therapy, often provide only temporary relief and fail to address the underlying causes. In contrast, traditional Chinese acupuncture has demonstrated significant advantages in treating this condition [21].
In this study, the research group demonstrated significantly better clinical outcomes compared to the control group. The total response rate in the research group was 91.84%, notably higher than the 76.79% observed in the control group. Post-treatment, the research group showed significant improvements in THI, PSQI, TEQ, VAS, HAMA, and HAMD scores, surpassing those in the control group. These results suggest that the Dunhuang “Moxibustion Classic” acupuncture method offers substantial advantages in alleviating tinnitus symptoms, enhancing sleep quality, reducing aural fullness, and mitigating anxiety and depression. Furthermore, the research group experienced a significantly lower incidence of adverse reactions, highlighting the safety of this acupuncture treatment.
The observed benefits are largely attributed to the precise selection of acupoints in the “Moxibustion Classic” acupuncture method. Acupoints such as Hairline, Four Heavenly Courts, and Dazhui are strategically chosen for their ability to regulate meridians, clear the head and eyes, promote yang, and relieve exterior syndromes [22-24]. The Shenmen acupoint, often used to address insomnia, irritability, and anxiety, plays a crucial role in calming the mind and improving sleep quality [25]. Similarly, the Taixi acupoint is instrumental in regulating nervous system functions, alleviating anxiety and depression related to kidney essence deficiency, and enhancing patients’ psychological and physiological resilience [26]. The combination of yin-yang balance, five-element theory, and tailored acupoint selection allows for the harmonization of qi and blood, warming of the meridians, and improvement of overall circulation. This holistic approach not only addresses the physical symptoms of tinnitus but also significantly improves the psychological and neurological well-being of patients, ultimately leading to better overall quality of life.
Chen et al. [27] found that combining scraping therapy with Western medicine significantly improved tinnitus severity, volume, and hearing function in patients with kidney essence deficiency-type neuropathic tinnitus, showing greater efficacy than Western medicine alone. Similarly, Lee et al. [28], in a clinical review of 106 studies on acupuncture for tinnitus, highlighted the importance of acupoint selection in determining treatment outcomes. Wu et al. [29] also supported the effectiveness of acupuncture through a meta-analysis, showing that it effectively reduces tinnitus severity and enhances quality of life in primary tinnitus patients. Furthermore, Zhou et al. [30] reported notable clinical improvements in neuropathic tinnitus patients treated with electroacupuncture near the ear, demonstrating a reduction in tinnitus severity. Our study aligns with these findings, reinforcing the critical role of acupuncture in managing neuropathic tinnitus. The “Moxibustion Classic” acupuncture method not only stands out for its unique theoretical approach to acupoint selection but also demonstrates significant clinical efficacy, further corroborating previous research on the benefits of acupuncture in tinnitus treatment.
Moreover, sleep quality is a crucial factor influencing both the quality of life and treatment outcomes in patients with neuropathic tinnitus [31]. Research suggests a strong correlation between tinnitus and sleep disorders, where poor sleep quality can exacerbate tinnitus symptoms, leading to increased anxiety and depression [32]. This creates a vicious cycle, severely impacting patients’ physical health and daily functioning. In our study, logistic regression analysis identified treatment options, disease duration, pre-treatment THI, pre-treatment TEQ, and pre-treatment HAMA as significant risk factors affecting sleep quality. Specifically, patients treated with the Dunhuang “Moxibustion Classic” acupuncture method exhibited significantly better sleep quality than those in the control group. This suggests that acupuncture not only alleviates tinnitus symptoms but also significantly improves sleep quality. Patients with longer disease durations are more susceptible to sleep disorders, likely due to chronic stress from prolonged tinnitus symptoms [33]. Additionally, higher pre-treatment THI and TEQ scores, indicative of more severe tinnitus, were associated with a greater likelihood of sleep disturbances during treatment [34]. Patients with elevated anxiety levels (high pre-treatment HAMA scores) also experienced poorer sleep quality, further exacerbating their tinnitus symptoms and emotional distress [35].
By improving tinnitus symptoms and alleviating anxiety and depression, acupuncture not only enhances patients’ overall quality of life but also significantly improves their sleep quality. Improved sleep quality, in turn, helps to alleviate tinnitus symptoms, creating a positive feedback loop. Therefore, addressing and improving sleep quality in the treatment of neuropathic tinnitus is of significant clinical importance. The study results support the broader clinical use of acupuncture to enhance treatment outcomes and improve the quality of life for patients. For clinicians, understanding and assessing patients’ sleep conditions and taking appropriate measures can comprehensively improve the prognosis of patients with neuropathic tinnitus.
Despite providing valuable preliminary evidence for the effectiveness of the Dunhuang “Moxibustion Classic” acupuncture method in treating neuropathic tinnitus, this study has some limitations. First, the sample size was relatively small, with only 105 cases, which may limit the generalizability and statistical power of the results. Second, the single-center study design might restrict the applicability of the findings, as it is constrained to specific regions and medical practices. Third, the follow-up period was short, focusing mainly on short-term effects after treatment, and lacking long-term follow-up data to evaluate the sustained efficacy and recurrence rates of acupuncture therapy. Finally, the lack of standardization in acupuncture techniques might introduce individual variations during specific procedures, affecting the reproducibility of results. Future studies should aim to increase sample size, conduct multicenter and long-term follow-up research, and enhance the standardization of acupuncture techniques to further validate and promote the use of acupuncture therapy in the treatment of neuropathic tinnitus.
In summary, combining the Dunhuang “Moxibustion Classic” acupuncture with carbamazepine demonstrates good clinical efficacy in treating neuropathic tinnitus. The “Moxibustion Classic” acupuncture method is significantly more effective than conventional acupuncture in symptom recovery for neuropathic tinnitus and is worth promoting in clinical practice.
Disclosure of conflict of interest
None.
References
- 1.Dalrymple SN, Lewis SH, Philman S. Tinnitus: diagnosis and management. Am Fam Physician. 2021;103:663–671. [PubMed] [Google Scholar]
- 2.Chemali Z, Nehmé R, Fricchione G. Sensory neurologic disorders: tinnitus. Handb Clin Neurol. 2019;165:365–381. doi: 10.1016/B978-0-444-64012-3.00022-8. [DOI] [PubMed] [Google Scholar]
- 3.Mazurek B, Szczepek AJ, Hebert S. Stress and tinnitus. HNO. 2015;63:258–265. doi: 10.1007/s00106-014-2973-7. [DOI] [PubMed] [Google Scholar]
- 4.Mares T, Albrecht J, Buday J, Podgorna G, Le TH, Magyarova E, Poshor K, Halik J, Buna J, Capek V, Kostylkova L, Klasova J, Fabian V, Anders M. Long-term effect of transcranial direct current stimulation in the treatment of chronic tinnitus: a randomized, placebo-controlled trial. Front Psychiatry. 2022;13:969800. doi: 10.3389/fpsyt.2022.969800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazurek B, Szczepek AJ, Brüggemann P. Tinnitus - clinical symptoms and therapy. Laryngorhinootologie. 2017;96:47–59. doi: 10.1055/s-0042-119419. [DOI] [PubMed] [Google Scholar]
- 6.Chen X, Ren L, Xue X, Yu N, Liu P, Shen W, Zhou H, Wang B, Zhou J, Yang S, Jiang Q. The comorbidity of depression and anxiety symptoms in tinnitus sufferers: a network analysis. Brain Sci. 2023;13:583. doi: 10.3390/brainsci13040583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altissimi G, Colizza A, Cianfrone G, de Vincentiis M, Greco A, Taurone S, Musacchio A, Ciofalo A, Turchetta R, Angeletti D, Ralli M. Drugs inducing hearing loss, tinnitus, dizziness and vertigo: an updated guide. Eur Rev Med Pharmacol Sci. 2020;24:7946–7952. doi: 10.26355/eurrev_202008_22477. [DOI] [PubMed] [Google Scholar]
- 8.Doi MY, Tano SS, Schultz AR, Borges R, Marchiori LL. Effectiveness of acupuncture therapy as treatment for tinnitus: a randomized controlled trial. Braz J Otorhinolaryngol. 2016;82:458–465. doi: 10.1016/j.bjorl.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu S, Wu J, Sun Y, Lyu J. Advances in acupuncture treatment for tinnitus. Am J Otolaryngol. 2024;45:104215. doi: 10.1016/j.amjoto.2024.104215. [DOI] [PubMed] [Google Scholar]
- 10.Ji L, Zhang H, Wang L, Yin Z, Cen J, Guo Y. Network meta-analysis of acupuncture for tinnitus. Medicine (Baltimore) 2023;102:e35019. doi: 10.1097/MD.0000000000035019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Expert Panel on Neurological Imaging. Jain V, Policeni B, Juliano AF, Adunka O, Agarwal M, Dubey P, Friedman ER, Gule-Monroe MK, Hagiwara M, Hunt CH, Lo BM, Oh ES, Rath TJ, Roberts JK, Schultz D, Taheri MR, Zander D, Burns J. ACR appropriateness criteria® tinnitus: 2023 update. J Am Coll Radiol. 2023;20:S574–S591. doi: 10.1016/j.jacr.2023.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Neupane AK, Ghimire A, Bhattarai B, Prabhu P. Development and standardization of tinnitus handicap inventory in Nepali. Int Tinnitus J. 2019;23:47–51. doi: 10.5935/0946-5448.20190009. [DOI] [PubMed] [Google Scholar]
- 13.Zitser J, Allen IE, Falgàs N, Le MM, Neylan TC, Kramer JH, Walsh CM. Pittsburgh sleep quality index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLoS One. 2022;17:e0270095. doi: 10.1371/journal.pone.0270095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Z, Zheng Y, Fei Y, Wu D, Yang X. Validation of the mandarin tinnitus evaluation questionnaire: a clinician-administered tool for tinnitus management. Medicine (Baltimore) 2021;100:e26490. doi: 10.1097/MD.0000000000026490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moshtaghi O, Ghavami Y, Mahboubi H, Sahyouni R, Haidar Y, Ziai K, Lin HW, Djalilian HR. Migraine-related aural fullness: a potential clinical entity. Otolaryngol Head Neck Surg. 2018;158:100–102. doi: 10.1177/0194599817739255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson E. Hamilton rating scale for anxiety (HAM-A) Occup Med (Lond) 2015;65:601. doi: 10.1093/occmed/kqv054. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg LI. The Ham-D is not Hamilton’s depression scale. Psychopharmacol Bull. 2022;52:117–153. [PMC free article] [PubMed] [Google Scholar]
- 18.Fan L, Gao Y, Zhou J, Hu H, Gao H. The efficacy and safety of acupuncture for tinnitus-associated insomnia: a protocol for a systematic review and meta-analysis. J Pain Res. 2022;15:2957–2965. doi: 10.2147/JPR.S383968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yin T, Ni J, Zhu W. Deep needling and shallow needling at three acupoints around ear for subjective tinnitus: a randomized controlled trial. Zhongguo Zhen Jiu. 2015;35:1015–1019. [PubMed] [Google Scholar]
- 20.Li KS, Liu YH. Impact of migraine and vestibular migraine on audiometric profiles and quality of life in patients with tinnitus. Otol Neurotol. 2024;45:e443–e449. doi: 10.1097/MAO.0000000000004196. [DOI] [PubMed] [Google Scholar]
- 21.Han M, Yang X, Lv J. Efficacy of tinnitus retraining therapy in the treatment of tinnitus: a meta-analysis and systematic review. Am J Otolaryngol. 2021;42:103151. doi: 10.1016/j.amjoto.2021.103151. [DOI] [PubMed] [Google Scholar]
- 22.Lee HK, Moon SK, Jin C, Cho SY, Park SU, Jung WS, Park JM, Ko CN, Cho KH, Kwon S. Effects of GV14 acupuncture on cerebral blood flow velocity in the basilar and middle cerebral arteries and CO(2) reactivity during hypercapnia in normal individuals. Evid Based Complement Alternat Med. 2021;2021:9319413. doi: 10.1155/2021/9319413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aoyama N, Fujii O, Yamamoto T. Efficacy of parietal acupoint therapy: scalp acupuncture for neck/shoulder stiffness with related mood disturbance. Med Acupunct. 2017;29:383–389. doi: 10.1089/acu.2017.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Su K, Hao W, Lv Z, Wu M, Li J, Hu Y, Zhang Z, Gao J, Feng X. Electroacupuncture of Baihui and Shenting ameliorates cognitive deficits via Pten/Akt pathway in a rat cerebral ischemia injury model. Front Neurol. 2022;13:855362. doi: 10.3389/fneur.2022.855362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yuan J, Chen Y, Yu P, Luo F, Gao Y, Chen J, Wang P, Wang Y, Zhao Y, Lei Y. Effect of magnetic stimulation of Shenmen point on cognitive function of chronic insomnia: a randomized controlled clinical trial. Medicine (Baltimore) 2020;99:e23807. doi: 10.1097/MD.0000000000023807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen S, Xu M, Li H, Liang J, Yin L, Liu X, Jia X, Zhu F, Wang D, Shi X, Zhao L. Acupuncture at the Taixi (KI3) acupoint activates cerebral neurons in elderly patients with mild cognitive impairment. Neural Regen Res. 2014;9:1163–1168. doi: 10.4103/1673-5374.135319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen JF, Chen LY, Zheng X, Yang Y, Chen YT, Zheng MR. Scraping needling technique combined with western medication for neurogenic tinnitus of kidney essence deficiency: a randomized controlled trial. Zhongguo Zhen Jiu. 2022;42:991–994. doi: 10.13703/j.0255-2930.20211102-k0002. [DOI] [PubMed] [Google Scholar]
- 28.Lee KH, Kim MH, Kim J, Nam HJ. Acupuncture for tinnitus: a scoping review of clinical studies. Complement Med Res. 2024;31:292–301. doi: 10.1159/000538236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Q, Wang J, Han D, Hu H, Gao H. Efficacy and safety of acupuncture and moxibustion for primary tinnitus: a systematic review and meta-analysis. Am J Otolaryngol. 2023;44:103821. doi: 10.1016/j.amjoto.2023.103821. [DOI] [PubMed] [Google Scholar]
- 30.Zhou X, Ruan J, Li Z, Xing B. Short-term and long-term efficacy analysis of acupoint catgut embedding at cervical Jiaji (EX-B 2) points combined with electroacupuncture at acupoints near ears for nervous tinnitus. Zhongguo Zhen Jiu. 2015;35:32–35. [PubMed] [Google Scholar]
- 31.Ding Z, Zhang C, Wang F, Wu X, Chen T, Wang L, Jiang Y, Han D, Shen W. The association between tinnitus sensation-level loudness and sleep quality in patients with subjective consecutive tinnitus: a mediation analysis. Am J Audiol. 2024;33:433–441. doi: 10.1044/2024_AJA-23-00063. [DOI] [PubMed] [Google Scholar]
- 32.Gallo KEB, Corrêa CC, Gonçalves CGO, Correia Baran JB, Marques JM, Zeigelboim BS, José MR. Effect of tinnitus on sleep quality and insomnia. Int Arch Otorhinolaryngol. 2023;27:e197–e202. doi: 10.1055/s-0041-1735455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutter J, Cuvelier A, Lukaszewicz R, Maris J, Arnulf I, Similowski T, Patout M. Poor sleep quality and nocturnal home noninvasive ventilation: prevalence, risk factors and impact. Pulmonology. 2023;29:546–549. doi: 10.1016/j.pulmoe.2023.04.002. [DOI] [PubMed] [Google Scholar]
- 34.Jia XD, Li YK, Xie CC, Ding XL, Ding SG, Liu HJ. Effects of transcranial direct current stimulation combined with tinnitus retraining therapy on sleep disorders in patients with chronic tinnitus. Eur Rev Med Pharmacol Sci. 2024;28:1768–1776. doi: 10.26355/eurrev_202403_35590. [DOI] [PubMed] [Google Scholar]
- 35.Serrano-Checa R, Hita-Contreras F, Jiménez-García JD, Achalandabaso-Ochoa A, Aibar-Almazán A, Martínez-Amat A. Sleep quality, anxiety, and depression are associated with fall risk factors in older women. Int J Environ Res Public Health. 2020;17:4043. doi: 10.3390/ijerph17114043. [DOI] [PMC free article] [PubMed] [Google Scholar]