Abstract
Objective: To assess the effect of psychocardiology-based nursing intervention on cardiac function and self-efficacy in elderly patients with angina pectoris. Methods: A total of 127 elderly patients with angina pectoris admitted to the First Affiliated Hospital of Xi’an Jiaotong University from December 2022 to December 2023 were divided into two groups: the control group (n=63) received routine nursing care, while the observation group (n=64) received psychocardiology-based nursing intervention in addition to routine care. The psychological status, self-efficacy, cardiac function, and severity of angina were compared between the two groups before and after intervention. Results: After intervention, Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) scores significantly decreased in both groups compared to pre-intervention levels (both P<0.05), with the observation group showing a more pronounced reduction (both P<0.05). The left ventricular ejection fraction (LVEF) increased significantly in both groups post-intervention (P<0.05), while left ventricular end-diastolic diameter (LVEDD) and left ventricular wall thickness (LVWT) showed no significant changes (both P>0.05). Self-efficacy scores significantly improved in both groups post-intervention (P<0.05), with a greater increase observed in the observation group (P<0.05). Additionally, all dimensions of the Seattle Angina Questionnaire (SAQ) showed significant improvement in both groups post-intervention (P<0.05), with higher scores in the observation group compared to the control group (P<0.05). Conclusion: Psychocardiology-based nursing intervention effectively improves psychological well-being, self-efficacy, quality of life, and cardiac function in elderly patients with angina pectoris.
Keywords: Psychocardiology-based nursing mode, nursing intervention, angina pectoris, cardiac function, self-efficacy
Introduction
Cardiovascular diseases are prevalent conditions that pose significant risks to human life and health. Research indicates that patients with cardiovascular diseases often experience psychological disorders such as anxiety and depression, which can adversely affect clinical outcomes and contribute to disease progression [1,2]. Coronary heart disease (CHD), caused by coronary atherosclerosis, results in myocardial ischemia and hypoxia, particularly affecting middle-aged and elderly individuals [3]. Angina pectoris, a clinical syndrome characterized by acute and brief episodes of myocardial ischemia and hypoxia, is caused by insufficient blood supply to the coronary arteries [4]. Patients with CHD and angina pectoris frequently suffer from psychological disorders, including depression, anxiety, and fear. Conventional treatment and care for these conditions primarily focus on alleviating clinical symptoms, often neglecting the importance of psychological intervention. This oversight can lead to the worsening of the patient’s condition. Therefore, effective care must address both the physical and psychological aspects of the disease, aiming to alleviate negative emotions and improve the patient’s quality of life [5].
Psychocardiology, also known as psychological or behavioral cardiology, focuses on addressing the emotional, social, and behavioral issues associated with heart disease. It emphasizes the psychological well-being of patients alongside the diagnosis and treatment of cardiovascular conditions. While current research primarily concentrates on the physical aspects of CHD or psychological care in isolation, there is a need for a more comprehensive exploration of the interplay between CHD and psychological factors. This study investigates the effects of psychocardiology-based nursing intervention on cardiac function and self-efficacy in elderly patients with angina pectoris.
Materials and methods
Research subjects
In this retrospective study, 127 elderly patients with angina pectoris, admitted to the First Affiliated Hospital of Xi’an Jiaotong University from December 2022 to December 2023, were divided into a control group (n=63) and an observation group (n=64) based on their admission time. The study was approved by the ethics committee of the First Affiliated Hospital of Xi’an Jiaotong University.
Inclusion criteria
(1) Patients diagnosed with angina pectoris and CHD according to WHO clinical diagnostic criteria, confirmed by electrocardiogram, dynamic electrocardiogram, coronary angiography, and echocardiography [6]; (2) Patients aged between 60-80 years old; (3) Patients with grade I-II cardiac function; (4) Patients with an education level above elementary school; and (5) Patients capable of effective communication.
Exclusion criteria
(1) Patients with cognitive impairment or hearing loss; (2) Patients with myocardial infarction, severe arrhythmia, or heart failure; (3) Patients with mental disorders; (4) CHD patients with severe liver or kidney dysfunction, cerebrovascular disease, or malignant tumors.
Methods
Patients in the control group received routine nursing care: (1) Patients were instructed to stay in bed and remain quiet, with close monitoring; (2) Adverse reactions to anti-angina drugs (e.g., nitroglycerin) were observed, including vasodilation symptoms such as headache, facial flushing, and dizziness. Patients sensitive to the medication were monitored for orthostatic hypotension; (3) The room temperature was controlled to avoid increasing the cardiac workload or triggering angina; (4) Patients were advised to follow a low-fat, low-cholesterol, high-vitamin diet, with small, frequent meals, and to avoid smoking and alcohol; (5) Heart rate, pain location, nature, and duration, as well as responses to medication, were closely monitored. Night rounds were intensified, and any changes in the frequency or nature of angina were documented; (6) Patients were guided to engage in moderate exercise once pain was stable; (7) Health education was reinforced during hospitalization.
The observation group received psychocardiology-based nursing intervention in addition to routine care. This included relaxation therapy combined with exercise therapy. Mindfulness was used as the relaxation therapy, and cardiac rehabilitation exercises were implemented as the exercise therapy. The specific interventions were as follows.
Cardiac rehabilitation exercise therapy: It was conducted daily at 4 p.m. in the open corridor space of the inpatient ward. Nurses guided patients through cardiac rehabilitation exercises, ensuring no discomfort such as chest tightness or shortness of breath. Exercises were avoided within 2 hours of eating. Patients followed nurses or instructional videos for 20-30 minutes, accompanied by background music and professional guidance.
Meditation therapy: This therapy was conducted at 8:30 p.m. daily during hospitalization (not within 2 hours after a meal). Nurses instructed patients in meditation therapy in a calm environment, ensuring emotional stability. Patients were seated upright, in a flat sitting position, or cross-legged, with hands held above the head. Breathing techniques were emphasized, with deep chest-abdomen breathing, inhaling through the nose and exhaling through the mouth. The tip of the tongue should lightly touch the roof of the mouth when inhaling, and should rest flat when exhaling. during exhalation. Breathing was paced at 8-10 breaths per minute. Each session lasted 10-15 minutes, with low-decibel meditation music and professional instruction.
Psychological intervention and nursing: Nurses in the Department of Geriatrics were trained in psychological nursing, enabling them to identify and address patients’ psychological issues effectively. This training helped cultivate professional competence in psychological nursing. Nurses established strong nurse-patient relationships, monitored mood changes, identified negative emotions, and provided individualized psychological interventions based on each patient’s specific condition.
Observation of indexes
Anxiety: The patients’ anxiety levels were assessed using the Hamilton Anxiety Scale (HAMA) before and after the intervention, with a maximum score of 100 points [7]. A higher HAMA score indicates more severe anxiety. The anxiety levels were classified as follows: a score less than 50 indicates no anxiety, 50-59 indicates mild anxiety, 60-69 indicates moderate anxiety, and a score of 70 or above indicates severe anxiety.
Depression: Patients’ depression levels were measured using the Hamilton Depression Scale (HAMD) before and after the intervention, also with a total score of 100 points [8]. The depression levels were classified similarly to the HAMA: a score less than 50 indicates no depression, 50-59 indicates mild depression, 60-69 indicates moderate depression, and a score of 70 or above indicates severe depression.
Cardiac function: Cardiac function was evaluated by measuring the left ventricular ejection fraction (LVEF), left ventricular end-diastolic diameter (LVEDD), and left ventricular wall thickness (LVWT) before and after the intervention. These measurements were obtained using a GE Vivid E9 ultrasonic diagnostic instrument with an M5s probe. ECG leads were placed on the chest, and cardiac ultrasound images were optimized by adjusting gain, focus, fan width, and depth to achieve the best image quality. The echocardiographic views included left ventricular long-axis, aortic short-axis, apical (four-chamber, two-chamber, and three-chamber), and left ventricular short-axis views (at the mitral valve, papillary muscle, and apex levels). For each slice, 3-5 cardiac cycles were recorded.
Self-efficacy: Patients’ self-efficacy was assessed using a self-efficacy scale before and after the intervention [9]. The scale comprises five dimensions: emotion management, symptom management, disease cognition, medication compliance, and medication management, with each dimension scoring up to 20 points. A higher score indicates a stronger self-efficacy in managing these aspects.
Degree of angina pectoris: The degree of angina pectoris was evaluated using the Seattle Angina Questionnaire (SAQ) [10]. This questionnaire includes five dimensions: physical activity limitation, stability of angina, frequency of angina, treatment satisfaction, and disease awareness. The standard score is calculated as follows: Standard score = (actual score - the lowest score)/(the highest score - the lowest score) × 100. A higher score indicates a better quality of life and functional status.
Statistical analysis
Data were analyzed using SPSS 22.0. Two independent sample t-tests were used for comparisons between groups, paired t-tests were used for within-group comparisons, and chi-square tests were used for comparing categorical data. A p-value <0.05 was considered statistically significant.
Results
Comparison of clinical materials
The comparison of general data between the two groups, including gender, age, disease duration, and educational level, showed no significant differences (all P>0.05, Table 1).
Table 1.
Comparison of clinical data between two groups
| Group | Number of cases | Gender | Age (years old, x̅±s) | Course of disease (years, x̅±s) | Education degree | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Male | Female | Junior high school and below | High school and above | ||||
| Observation group | 64 | 35 | 29 | 69.36±9.75 | 5.74±1.36 | 42 | 22 |
| Control group | 63 | 31 | 32 | 68.94±8.94 | 5.93±1.52 | 39 | 23 |
| t/X2 | - | 0.382 | 0.253 | 0.743 | 0.102 | ||
| P | - | 0.537 | 0.801 | 0.459 | 0.750 | ||
Comparison of anxiety and depression before and after intervention
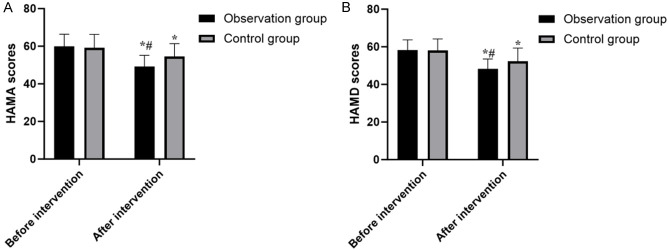
After the intervention, the HAMA and HAMD scores in both groups decreased significantly compared to pre-intervention levels (both P<0.05), with the scores in the observation group being significantly lower than those of the control group (both P<0.05, Tables 2, 3 and Figure 1).
Table 2.
Comparison of HAMA scores between two groups before and after intervention (points, x̅±sd)
| Group | Number of cases | Before intervention | After intervention | t | P |
|---|---|---|---|---|---|
| Observation group | 64 | 59.83±6.49 | 49.21±5.94 | 9.657 | <0.001 |
| Control group | 63 | 59.10±7.21 | 54.52±6.82 | 3.691 | <0.001 |
| t | - | 0.600 | 4.681 | - | - |
| P | - | 0.550 | <0.001 | - | - |
HAMA: Hamilton Anxiety Scale.
Table 3.
Comparison of HAMD scores between two groups before and after intervention (points, x̅±sd)
| Group | Number of cases | Before intervention | After intervention | t | P |
|---|---|---|---|---|---|
| Observation group | 64 | 58.32±5.39 | 48.27±5.26 | 10.676 | <0.001 |
| Control group | 63 | 58.05±6.12 | 52.31±7.02 | 4.892 | <0.001 |
| t | - | 0.265 | 3.674 | - | - |
| P | - | 0.792 | <0.001 | - | - |
HAMD: Hamilton Depression Scale.
Figure 1.
Comparison of HAMA and HAMD scores between the two groups before and after intervention. Note: A: Hamilton Anxiety Scale (HAMA); B: Hamilton Depression Scale (HAMD). Compared to before intervention, paired t-test, *P<0.05; compared to control group, U, #P<0.05.
Comparison of cardiac function
The LVEF in both groups increased significantly after the intervention compared to before (P<0.05), with the observation group showing a notably higher LVEF than the control group (P<0.05). However, there were no significant differences in LVEDD and LVWT before and after the intervention in either group (both P>0.05, Table 4).
Table 4.
Comparison of cardiac function between two groups before and after intervention (x̅±sd)
| Group | Period | LVEF | LVEDD | LVWT |
|---|---|---|---|---|
| Observation group (n=64) | Before intervention | 42.93±3.74 | 60.27±6.83 | 70.82±7.38 |
| After intervention | 48.65±3.96* | 58.95±6.20 | 69.32±5.63 | |
| t | 8.040 | 1.145 | 1.293 | |
| P | <0.001 | 0.255 | 0.199 | |
| Control group (n=63) | Before intervention | 42.65±3.62 | 61.02±5.33 | 71.21±8.03 |
| After intervention | 45.27±2.75 | 59.28±7.22 | 69.84±6.84 | |
| t | 4.597 | 1.539 | 1.031 | |
| P | <0.001 | 0.126 | 0.305 |
Note: Compared to the control group in the same period, U;
P<0.05.
LVEF: left ventricular ejection fraction; LVEDD: left ventricular end-diastolic diameter; LVWT: left ventricular wall thickness.
Comparison of self-efficacy
As shown in Table 5, self-efficacy scores in both groups significantly increased after the intervention compared to pre-intervention levels (P<0.05), with the observation group achieving higher self-efficacy scores than the control group (P<0.05).
Table 5.
Comparison of self-efficacy scores between two groups before and after intervention (points, x̅±sd)
| Group | Period | Emotion Management | Symptom Management | Disease Cognition | Medication Compliance | Medication Management |
|---|---|---|---|---|---|---|
| Observation group (n=64) | Before intervention | 12.97±1.03 | 13.84±1.75 | 13.28±1.65 | 11.95±2.17 | 13.64±1.27 |
| After intervention | 18.19±2.16* | 19.27±2.03* | 20.19±2.37* | 17.69±1.79* | 18.96±2.24* | |
| t | 17.451 | 16.208 | 19.143 | 16.324 | 16.528 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Control group (n=63) | Before intervention | 13.11±1.26 | 13.97±1.81 | 13.79±1.75 | 11.62±1.72 | 13.77±1.64 |
| After intervention | 15.39±1.68 | 16.28±1.95 | 17.49±1.97 | 14.85±1.88 | 15.90±2.18 | |
| t | 8.618 | 6.891 | 11.145 | 10.061 | 6.197 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Note: Compared to the control group in the same period, U;
P<0.05.
Comparison of angina pectoris
As shown in Table 6, all dimensions of the SAQ in both groups improved significantly after the intervention compared to pre-intervention levels (P<0.05), with the observation group scoring higher than the control group (P<0.05).
Table 6.
Comparison of SAQ scores between two groups of patients before and after intervention (points, x̅±s)
| Group | Period | Physical activity limitation | Stable state | Frequency | Satisfaction degree | Awareness of disease | Total score |
|---|---|---|---|---|---|---|---|
| Observation group (n=64) | Before intervention | 32.64±3.04 | 4.10±0.52 | 7.96±0.75 | 13.26±2.08 | 7.28±1.66 | 65.41±6.94 |
| After intervention | 41.98±3.29* | 5.27±0.83* | 9.37±1.21* | 17.21±3.27* | 11.20±1.53* | 83.27±9.30* | |
| t | 16.680 | 9.556 | 7.924 | 8.090 | 13.891 | 12.313 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Control group (n=63) | Before intervention | 32.87±2.92 | 4.08±0.44 | 7.84±0.85 | 13.18±1.96 | 7.19±1.58 | 65.93±7.02 |
| After intervention | 37.95±3.17 | 4.70±0.69 | 8.20±0.97 | 15.01±2.75 | 9.89±1.26 | 76.58±7.82 | |
| t | 9.429 | 6.013 | 2.216 | 4.301 | 10.605 | 8.044 | |
| P | <0.001 | <0.001 | 0.029 | <0.001 | <0.001 | <0.001 |
Note: Compared to the control group in the same period, U;
P<0.05.
SAQ: Seattle Angina scale.
Discussion
Numerous studies have demonstrated that accurate diagnosis, effective treatment methods, and early nursing intervention can significantly enhance the therapeutic outcome and clinical prognosis of patients with CHD and angina pectoris [11,12]. Elderly patients often experience long-term psychological stress and tension due to factors such as declining physical health, limited social interaction, reduced communication with others, recurrent illness, prolonged disease duration, and frequent hospital admissions. These factors can exacerbate negative emotions, impair arterial dilation, increase heart rate and blood pressure, and consequently worsen myocardial ischemia and hypoxia [13]. Therefore, psychological disorders such as anxiety and depression have emerged as critical risk factors for cardiovascular diseases, warranting attention from clinical practitioners [14]. The psychocardiology medical model, derived from the biopsychosocial model, provides a framework for understanding patients’ psychological states by integrating psychological monitoring with clinical diagnosis and treatment [15]. To further enhance the therapeutic efficacy and quality of life in elderly patients with CHD and angina pectoris, this study explores the impact of nursing interventions based on the biopsychosocial model on cardiac function and self-efficacy in this patient population.
The results of this study demonstrated that the HAMA and HAMD scores in both patient groups significantly decreased after treatment compared to baseline. Furthermore, the observation group exhibited significantly lower scores than the control group post-intervention. This aligns with the findings of other studies [16,17], indicating that the dual-heart medical model effectively alleviated anxiety and mood disturbances in patients. This further supports the notion that effective psychological intervention can enhance the mental health of elderly patients with CHD and angina pectoris.
Self-efficacy, shaped by information from various sources, is a critical factor in behavioral decision-making and a key determinant of healthy behavior in patients with CHD [18]. Patients with high self-efficacy tend to attribute their illness to external factors, view it as a personal challenge, and believe that they can manage their daily lives and improve their health through their efforts [19]. In contrast, patients with low self-efficacy are more likely to doubt their abilities, focus on potential failures, and experience negative psychological states such as tension, anxiety, and depression when faced with setbacks [20]. The study found that the self-efficacy scores in both groups improved significantly after intervention, with the observation group showing greater improvements than the control group. This suggests that nursing interventions based on the dual-heart medical model can enhance patients’ self-efficacy, which in turn improves their psychological state, aids in disease recovery, and promotes treatment adherence. The model likely improves patients’ psychological states by reducing symptoms of angina pectoris and enhancing their ability to manage the disease, creating a positive feedback loop for disease management.
The SAQ is a comprehensive tool for assessing psychological status, bodily function, and quality of life in post-intervention patients. It is a practical and effective method for evaluating body function, quality of life, treatment efficacy, and prognosis in patients with CHD in China [21]. The study indicated that all SAQ dimensions improved significantly post-intervention, with the observation group showing higher scores than the control group. This suggests that the psychocardiology-based nursing intervention effectively addresses the negative psychological conditions in patients with angina pectoris, consistent with previous reports [22,23]. Additionally, the LVEF values in both groups were significantly higher post-intervention, with the observation group outperforming the control group. This indicates that the dual-heart medical model not only enhances cardiac function but may also improve psychological status and self-efficacy, thereby contributing to better clinical outcome [24,25].
However, this study included only 127 patients with CHD and angina pectoris, which limits its scope. The sample size was small, and long-term follow-up was not conducted after discharge. Future studies should aim to expand the sample size, broaden the study areas, and analyze long-term impacts to develop effective care models for improving patient quality of life.
In conclusion, the psychocardiology-based nursing intervention improved the psychological states, self-efficacy, quality of life, and cardiac function of elderly patients with angina pectoris.
Disclosure of conflict of interest
None.
References
- 1.Lutski M, Weinstein G, Tanne D, Goldbourt U. Angina pectoris severity and late-life frailty among men with cardiovascular disease. Aging Male. 2020;23:1022–1029. doi: 10.1080/13685538.2019.1657082. [DOI] [PubMed] [Google Scholar]
- 2.Dibben GO, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur Heart J. 2023;44:452–469. doi: 10.1093/eurheartj/ehac747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samuels BA, Shah SM, Widmer RJ, Kobayashi Y, Miner SES, Taqueti VR, Jeremias A, Albadri A, Blair JA, Kearney KE, Wei J, Park K, Barseghian El-Farra A, Holoshitz N, Janaszek KB, Kesarwani M, Lerman A, Prasad M, Quesada O, Reynolds HR, Savage MP, Smilowitz NR, Sutton NR, Sweeny JM, Toleva O, Henry TD, Moses JW, Fearon WF, Tremmel JA Microvascular Network (MVN) Comprehensive management of ANOCA, part 1-definition, patient population, and diagnosis: JACC State-of-the-Art Review. J Am Coll Cardiol. 2023;82:1245–1263. doi: 10.1016/j.jacc.2023.06.043. [DOI] [PubMed] [Google Scholar]
- 4.Tsai CC, Chuang SY, Hsieh IC, Ho LH, Chu PH, Jeng C. The association between psychological distress and angina pectoris: a population-based study. PLoS One. 2019;14:e0224451. doi: 10.1371/journal.pone.0224451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maagaard M, Nielsen EE, Sethi NJ, Ning L, Yang SH, Gluud C, Jakobsen JC. Effects of adding ivabradine to usual care in patients with angina pectoris: a systematic review of randomised clinical trials with meta-analysis and trial sequential analysis. Open Heart. 2020;7:e001288. doi: 10.1136/openhrt-2020-001288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrari R, Ford I, Fox K, Marzilli M, Tendera M, Widimský P, Challeton JP, Danchin N. A randomized, double-blind, placebo-controlled trial to assess the efficAcy and safety of Trimetazidine in patients with angina pectoris having been treated by percutaneous coronary intervention (ATPCI study): rationale, design, and baseline characteristics. Am Heart J. 2019;210:98–107. doi: 10.1016/j.ahj.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Yang J, Shan D, Wang X, Sun X, Shao M, Wang K, Pan Y, Wang Z, Schoepf UJ, Savage RH, Zhang M, Dong M, Xu L, Zhou Y, Ma X, Hu X, Xia L, Zeng H, Liu Z, Chen Y. On-site computed tomography-derived fractional flow reserve to guide management of patients with stable coronary artery disease: the TARGET randomized trial. Circulation. 2023;147:1369–1381. doi: 10.1161/CIRCULATIONAHA.123.063996. [DOI] [PubMed] [Google Scholar]
- 8.Schindler TH, Fearon WF, Pelletier-Galarneau M, Ambrosio G, Sechtem U, Ruddy TD, Patel KK, Bhatt DL, Bateman TM, Gewirtz H, Shirani J, Knuuti J, Gropler RJ, Chareonthaitawee P, Slart RHJA, Windecker S, Kaufmann PA, Abraham MR, Taqueti VR, Ford TJ, Camici PG, Schelbert HR, Dilsizian V. Myocardial perfusion PET for the detection and reporting of coronary microvascular dysfunction: a JACC: cardiovascular imaging expert panel statement. JACC Cardiovasc Imaging. 2023;16:536–548. doi: 10.1016/j.jcmg.2022.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Shen Y, Yan T, Peng Q, Zhang B, Zhao K, Yang Z. Kinesiophobia in patients with angina pectoris of coronary artery disease: a cross-sectional survey. Heart Lung. 2023;57:7–11. doi: 10.1016/j.hrtlng.2022.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Yang M, Sun M, Du T, Long H, Chen J, Liang F, Lao L. The efficacy of acupuncture for stable angina pectoris: a systematic review and meta-analysis. Eur J Prev Cardiol. 2021;28:1415–1425. doi: 10.1177/2047487319876761. [DOI] [PubMed] [Google Scholar]
- 11.Hokimoto S, Kaikita K, Yasuda S, Tsujita K, Ishihara M, Matoba T, Matsuzawa Y, Mitsutake Y, Mitani Y, Murohara T, Noda T, Node K, Noguchi T, Suzuki H, Takahashi J, Tanabe Y, Tanaka A, Tanaka N, Teragawa H, Yasu T, Yoshimura M, Asaumi Y, Godo S, Ikenaga H, Imanaka T, Ishibashi K, Ishii M, Ishihara T, Matsuura Y, Miura H, Nakano Y, Ogawa T, Shiroto T, Soejima H, Takagi R, Tanaka A, Tanaka A, Taruya A, Tsuda E, Wakabayashi K, Yokoi K, Minamino T, Nakagawa Y, Sueda S, Shimokawa H, Ogawa H Japanese Circulation Society and Japanese Association of Cardiovascular Intervention and Therapeutics and Japanese College of Cardiology Joint Working Group. JCS/CVIT/JCC 2023 Guideline focused update on diagnosis and treatment of vasospastic angina (coronary spastic angina) and coronary microvascular dysfunction. Circ J. 2023;87:879–936. doi: 10.1253/circj.CJ-22-0779. [DOI] [PubMed] [Google Scholar]
- 12.Tamis-Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, Lerman A, Cushman M, Kumbhani DJ, Arslanian-Engoren C, Bolger AF, Beltrame JF American Heart Association Interventional Cardiovascular Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; and Council on Quality of Care and Outcomes Research. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139:e891–e908. doi: 10.1161/CIR.0000000000000670. [DOI] [PubMed] [Google Scholar]
- 13.Vestergaard JM, Dalbøge A, Bonde JPE, Garde AH, Hansen J, Hansen ÅM, Larsen AD, Härmä M, Costello S, Böttcher M, Kolstad HA. Night shift work characteristics and risk of incident coronary heart disease among health care workers: national cohort study. Int J Epidemiol. 2023;52:1853–1861. doi: 10.1093/ije/dyad126. [DOI] [PubMed] [Google Scholar]
- 14.Ponticelli F, Giannini F. Coronary sinus reducer for the treatment of chronic refractory angina pectoris. Future Cardiol. 2022;18:523–537. doi: 10.2217/fca-2021-0064. [DOI] [PubMed] [Google Scholar]
- 15.Mehilli J, Presbitero P. Coronary artery disease and acute coronary syndrome in women. Heart. 2020;106:487–492. doi: 10.1136/heartjnl-2019-315555. [DOI] [PubMed] [Google Scholar]
- 16.Tian Y, Deng P, Li B, Wang J, Li J, Huang Y, Zheng Y. Treatment models of cardiac rehabilitation in patients with coronary heart disease and related factors affecting patient compliance. Rev Cardiovasc Med. 2019;20:27–33. doi: 10.31083/j.rcm.2019.01.53. [DOI] [PubMed] [Google Scholar]
- 17.Weir-McCall JR, Williams MC, Shah ASV, Roditi G, Rudd JHF, Newby DE, Nicol ED. National trends in coronary artery disease imaging: associations with health care outcomes and costs. JACC Cardiovasc Imaging. 2023;16:659–671. doi: 10.1016/j.jcmg.2022.10.022. [DOI] [PubMed] [Google Scholar]
- 18.Andreini D, Modolo R, Katagiri Y, Mushtaq S, Sonck J, Collet C, De Martini S, Roberto M, Tanaka K, Miyazaki Y, Czapla J, Schoors D, Plass A, Maisano F, Kaufmann P, Orry X, Metzdorf PA, Folliguet T, Färber G, Diamantis I, Schönweiß M, Bonalumi G, Guglielmo M, Ferrari C, Olivares P, Cavallotti L, Leal I, Lindeboom W, Onuma Y, Serruys PW, Bartorelli AL SYNTAX III REVOLUTION Investigators. Impact of fractional flow reserve derived from coronary computed tomography angiography on heart team treatment decision-making in patients with multivessel coronary artery disease: insights from the SYNTAX III REVOLUTION trial. Circ Cardiovasc Interv. 2019;12:e007607. doi: 10.1161/CIRCINTERVENTIONS.118.007607. [DOI] [PubMed] [Google Scholar]
- 19.Oeing CU, Matheson MB, Ostovaneh MR, Rochitte CE, Chen MY, Pieske B, Kofoed KF, Schuijf JD, Niinuma H, Dewey M, di Carli MF, Cox C, Lima JAC, Arbab-Zadeh A. Coronary artery disease grading by cardiac CT for predicting outcome in patients with stable angina. J Cardiovasc Comput Tomogr. 2023;17:310–317. doi: 10.1016/j.jcct.2023.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Peltzer S, Müller H, Köstler U, Blaschke K, Schulz-Nieswandt F, Jessen F, Albus C CoRe-Net study group. Quality of health care with regard to detection and treatment of mental disorders in patients with coronary heart disease (MenDis-CHD): study protocol. BMC Psychol. 2019;7:21. doi: 10.1186/s40359-019-0295-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moran KE, Ommerborn MJ, Blackshear CT, Sims M, Clark CR. Financial stress and risk of coronary heart disease in the Jackson heart study. Am J Prev Med. 2019;56:224–231. doi: 10.1016/j.amepre.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 22.Li L, Tan P, Li G, Yang S, Guo M, Zhang C. The application of dual-heart nursing mode in patients with coronary heart disease and angina pectoris and its impact on anxiety, depression, and quality of life. Medicine (Baltimore) 2023;102:e36530. doi: 10.1097/MD.0000000000036530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robbins MR, Strauch KA. Treatment of a mandibular abscess in a patient with coronary artery disease and intermittent angina. Dent Clin North Am. 2023;67:407–410. doi: 10.1016/j.cden.2023.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Cartlidge T, Kovacevic M, Navarese EP, Werner G, Kunadian V. Role of percutaneous coronary intervention in the modern-day management of chronic coronary syndrome. Heart. 2023;109:1429–1435. doi: 10.1136/heartjnl-2022-321870. [DOI] [PubMed] [Google Scholar]
- 25.Ahmad A, Corban MT, Moriarty JP, Kanaji Y, Rosedahl JK, Gulati R, Rihal CS, Prasad A, Sara JD, Toya T, Ter Horst I, Lerman LO, Borah B, Lerman A. Coronary reactivity assessment is associated with lower health care-associated costs in patients presenting with angina and nonobstructive coronary artery disease. Circ Cardiovasc Interv. 2023;16:e012387. doi: 10.1161/CIRCINTERVENTIONS.122.012387. [DOI] [PubMed] [Google Scholar]