Abstract
Background: Sulfur cream is reported to relieve itching and treat skin diseases caused by bacterial, fungal, and scabies infections. However, there is limited data on the efficacy of sulfur cream blowing and parching combined with compound ketoconazole ointment (ketoconazole, clobetasol propionate, and neomycin sulfate) in curing palmoplantar keratotic eczema. This prospective study proposed to investigate the clinical efficacy of sulfur cream on people who suffer with palmoplantar keratotic eczema. Methods: In total, 116 patients with palmoplantar keratotic eczema (those who met the diagnostic criteria of Expert Consensus on Standardized Diagnostic Terminology of Dermatitis and Eczematous Diseases) were chosen and divided into a control group (C, n = 58) and a study group (S, n = 58) depending on the treatment method. Patients in group C were cured with compound ketoconazole cream, while those in group S were given sulfur cream blowing and parching (10-15 min, once in the morning and once in the evening, with 4 weeks as a course of treatment) combined with compound ketoconazole cream treatment. Scores of erythema, keratinization, scales, chapping, pruritus, quality of life, and psychological status of patients were evaluated before and 4 weeks treatment. Results: The overall response rate (93% vs. 79%) and scores of quality of life, physiological burden, and social interaction of patients of group S were higher than those of group C (P < 0.05), and the incidence of adverse reactions and scores of self-rating anxiety scale, self-rating depressive scale, erythema, keratinization, scales, and skin lesions were lower in group S than those in the group C (P < 0.05) 4 weeks after treatment. In addition, pruritus scores at 1, 2, and 4 weeks after treatments were fewer in patients of group S than those in group C (P < 0.05). Conclusions: Sulfur cream blowing and parching for 4 weeks of treatment combined with compound ketoconazole cream is more effective than compound ketoconazole cream alone for 4 weeks in treating palmoplantar keratotic eczema.
Keywords: Blowing, compound ketoconazole cream, erythema, keratinization, parching, pruritus, palmoplantar keratotic eczema, quality of life, sulfur
Introduction
Palmoplantar keratotic eczema is a complicated clinical disease seen in dermatology [1]. Generally, as a common intractable localized inflammatory dermatosis, palmoplantar keratotic eczema is characterized by its chronicity, recurrence, pruritus, and hypertrophy, and patients usually suffer from red, hard and thick patches, which are of mung bean size on their palms or feet [2]. Palmoplantar keratotic eczema is mainly caused by inflammatory irritation or exposure to allergens. Inflammatory responses triggered by irritants or allergens form a vicious cycle with destruction of the barrier of the skin, which is a key link associated with its recurrence [3]. Recurrent eczema can lead to keratoplasia, a form of keratosis, and even induce chapped skin based on keratosis [4]. Palmoplantar keratotic eczema can be classified as congenital or acquired. The former is mainly associated with genetic factors, with many patients developing it in infancy or youth, and can be diagnosed based on the patient’s family history. The latter is associated with contact factors and mechanical injury [5].
Symptomatic treatment is the principal method for the treatment of palmoplantar keratotic eczema in modern medicine. In the past, oral antihistamines combined with tretinoin cream were commonly applied [6]. Considering that the palmoplantar corneum is thicker than other parts, and the prolonged scratching and grasping stimulation further thickens the stratum corneum, are drugs are not able to reach the lesions [7]. Besides, traditional therapies have some disadvantages, such as a high recurrence rate, varying degrees of drug resistance, and adverse reactions caused by long-term medication use. These shortcomings usually influence the quality of life of patients [8]. Compound ketoconazole cream, which can be used for various skin diseases, primarily contains ketoconazole, clobetasol propionate, and neomycin sulfate [9]. As the first orally active azole antifungal agent, ketoconazole has an inactivating effect on fungi like dermatophytes and yeasts [10]. Clobetasol propionate, a potent corticosteroid, has anti-inflammatory and anti-itch effects and is widely applied in various skin conditions [11]. Neomycin sulfate is an aminoglycoside antibiotic with good antibacterial effects [12]. Sulfur cream is mainly composed of sulfur and petroleum jelly and plays a role in degreasing, dissolving stratum corneum, relieving itching, and treating skin diseases caused by bacterial, fungal, and scabies infections [13].
Presently, there are few clinical studies on sulfur cream blowing and parching combined with compound ketoconazole ointment in curing palmoplantar keratotic eczema. Thus, our study proposed to investigate the clinical efficacy of sulfur cream blowing and parching combined with compound ketoconazole cream on patients with palmoplantar keratotic eczema.
Materials and methods
Ethics approval and consent to participate
All patients and their families were informed and signed an informed consent form. This work was approved by the ethics committee of the Guangdong Provincial Hospital of Chinese Medicine (ID: BF2021-144-01, dated June 15, 2015). The study follows the laws of China and the v2008 Declarations of Helinski.
Study subjects
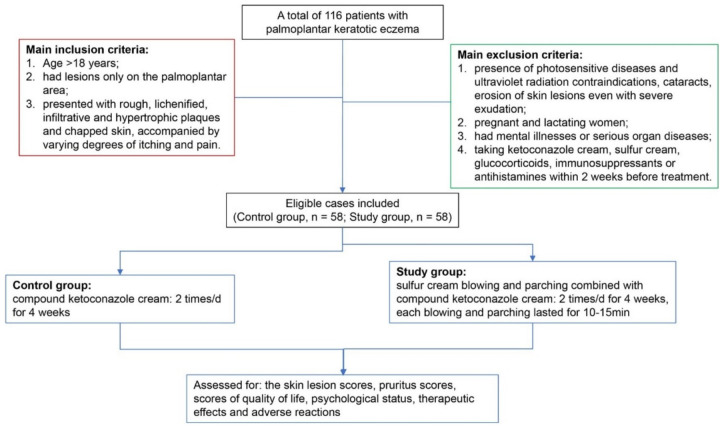
In prospective study 116 patients with palmoplantar keratotic eczema admitted to the Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China from October 2015 to October 2019 were divided into a control group (C, n = 58) and a study group (S, n = 58) depending on the adopted treatment methods. The selected patients met the diagnostic criteria of the Expert Consensus on Standardized Diagnostic Terminology of Dermatitis and Eczematous Diseases [14]. The case selection flow chart is shown in Figure 1.
Figure 1.
Flow chart of case selection for the current study.
Inclusion conditions
Accepted conditions were (1) over 18 years old; (2) had lesions only on the palmoplantar area; (3) presented with rough, lichenified, infiltrative, and hypertrophic plaques and chapped skin, accompanied by varying degrees of itching and pain.
Exclusion criteria
Excluded conditions were (1) the presence of photosensitive diseases and ultraviolet radiation contraindications, cataracts, and erosion of skin lesions even with severe exudation; (2) pregnant and lactating women; (3) patients with mental illnesses; (4) serious organ diseases such as heart, lung, liver, and kidney; (5) taking ketoconazole cream, sulfur cream, glucocorticoids, immunosuppressants or antihistamines within 2 weeks before treatment.
Interventions
The general information of included patients was recorded. In the control group (C group), the affected areas were treated with compound ketoconazole cream (Kaifeng Pharmaceutical (Group) Co., Ltd., USFDA approval number: H20074115, strength: 10 g/box) 2 times/day for 4 weeks as a course of treatment. In the study group (S group), the affected part was treated with sulfur cream blowing and parching (Xinxiang Qining Pharmaceutical Co., Ltd., SFDA approval number: H19983172, strengths: 15 g/box) combined with compound ketoconazole cream. Specifically, we used compound ketoconazole cream first, followed by sulfur cream treatment, and then the affected part of the patient was blown by the hot wind of a hair dryer or directly shined with the electromagnetic wave therapy instrument. Each blowing and parching lasted for 10-15 min, once in the morning and once in the evening, with 4 weeks as a course of treatment.
Both groups of patients avoided spicy and overly sour food, drinking alcohol, scratching, and hot washing during the treatments period. Any adverse reactions during medication were monitored, and the medicine was discontinued if the skin itching was aggravated or there was a burning sensation.
Observed indicators
Skin lesion scoring
Changes in skin erythema, keratinization, scales, and chapping were determined and scored based on a four-point scale before and after treatment in both groups. Erythema scoring rules are as follows: 0 means no erythema; 1 means mild erythema; 2 means moderate erythema; 3 means severe erythema. Keratinization scoring rules are as follows: 0 means no keratinization; 1 means mild keratinization; 2 means moderate keratinization; 3 means severe keratinization. Scales scoring rules are as follows: 0 means no scales; 1 means mild scales; 2 means moderate scales; 3 means severe scales. Chapping scoring rules are as follows: 0 means no chapping; 1 means mild chapping; 2 means moderate chapping; 3 means severe chapping. A higher total score represented a more severe skin lesions [15].
Pruritus scoring
The changes in the degree of pruritus before treatments and 1, 2, and 4 weeks after treatments were monitored in both groups and the corresponding scores were determined and recorded according to a four-point scale. Specifically, 0 indicated no pruritus; 1 indicated mild pruritus and no irritation; 2 indicated moderate pruritus but tolerable, and; 3 indicated severe pruritus and unbearable [16].
Quality of life score
The World Health Organization Quality-of-Life Brief Scale (WHOQOL-BREF) was administered to patients to value the quality of life in both groups [17]. The scale consisted of three aspects (daily life, physiological burden, and social interaction), and the score ranged from 0 to 100. An upper total score represented a better quality of life.
Psychological state
The Chinese version of the self-rating anxiety scale (SAS) and self-rating depressive scale (SDS) were carried out to value the psychological status of patients. A higher score indicated poorer psychological status [18].
Efficacy evaluation
The efficacy of treatments was evaluated in line with the following criteria. Cured: all lesions had subsided, and the symptoms had disappeared, with an efficacy index ≥ 95%; Excellently effective: most of the lesions had subsided, and the symptoms were significantly relieved, with 95% > efficacy index ≥ 70%; Effective: the lesions had partially subsided, and the symptoms were improved, with 70% > efficacy index ≥ 50%; Ineffective: alleviation of the lesion was not significant, the symptoms were not relieved and even deteriorated, with efficacy index < 50%. Efficacy index was estimated based on Eq. (1):
The score was determined by the sum of the lesion score and pruritus score.
Adverse reactions
The adverse reactions after drug administration, including skin atrophy, capillary dilation, and skin pigmentation were recorded in both groups.
Statistical analysis
InStat 3.01, statistical software, San Diego, CA, USA was chosen to break down the statistical information. The measurement information is statistically described as mean ± standard deviation (SD) or frequencies (percentages), or median (Q3-Q1) for categorical, normal continuous, and non-normal continuous variables, respectively. Because this was a pilot study we have not calculated the sample size with effect size and power calculations. An unpaired t-test with or without Welch correction was used for comparison of continues variables between two groups, and univariate analysis was performed for comparison between multiple groups comparison of continues variables. For non-normal continuous variables Mann-Whitney test or Wilcoxon matched-pairs signed-ranks test or Kruskal-Wallis’ test (nonparametric ANOVA) was performed between or within groups. Dunnett or Dunn’s multiple comparison test was used for post hoc analyses. The statistical information is denoted as n (%), and the Chi-square (χ 2 )-test was chosen for statistical analysis of categorical variables. Kolmogorov and Smirnov method was used to evaluate normality of variables. Interquartile range for non-normal continuous variables was calculated using Calculator Soup®. P < 0.05 was considered as the criterion for remarkable discrepancies.
Results
Baseline information
All enrolled patients were Han Chinese in ethnicity. In total, 116 individuals suffering from palmoplantar keratotic eczema were involved in the study, comprising 58 patients per group. Group C was composed of 33 males and 25 females, with a mean age of 30.26±8.37 years (range: 20 to 61 years) and a mean disease course of 51.34±24.82 months (range: 6 months to 8 years). Group S consisted of 32 males and 26 females, with a mean age of 31.66±10.51 years (range: 21 to 60 years) and a mean disease course of 54.24±30.97 months (range: 7 months to 9 years). The differences in general data for these two groups were not statistically remarkable (P > 0.05, parametric/non-parametric tests), revealing that patients of the two groups were comparable (Table 1).
Table 1.
Basic clinical information of the study patients
| Variables | Total (n = 116) | Group C (n = 58) | Group S (n = 58) | Comparisons between groups | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| P-value | Test value | df | 95% CI | ||||
| Gender | |||||||
| Male | 65 (56) | 33 (57) | 32 (55) | 0.8516 (X2-test with Yate’s corrections) | 0.035 | 1 | 0.7165 to 1.497 (using the approximation of Katz.) |
| Female | 51 (44) | 25 (43) | 26 (45) | ||||
| Age (years) | 30.96±9.49 | 30.26±8.37 | 31.66±10.51 | 0.4303 (Unpaired t test with Welch correction) | 0.7916 | 108 | -2.100 to 4.894 |
| Disease course (months) | 52.79±27.98 | 51.34±24.82 | 54.24±30.97 | 0.5795 (Unpaired t test with Welch correction) | 0.5558 | 108 | -7.433 to 13.226 |
| Erythema | 3 (3-2) | 3 (3-2) | 3 (3-2) | 0.8068 (Mann-Whitney test) | 1,638 | N/A | N/A |
| Keratinization | 2 (3-2) | 2 (3-2) | 2.5 (3-2) | 0.6268 (Mann-Whitney test) | 1,595 | N/A | N/A |
| Scales | 2 (3-2) | 2 (3-2) | 2 (3-2) | 0.5333 (Mann-Whitney test) | 1,541 | N/A | N/A |
| Chapping | 2 (2-1) | 2 (2-1) | 2 (2-1) | 0.5449 (Mann-Whitney test) | 1,573 | N/A | N/A |
| Total scores | 8.95±1.32 | 8.83±1.43 | 9.07±1.98 | 0.3261 (unpaired test; df: 114) | 0.9863 | N/A | N/A |
Erythema: 0: no erythema; 1: mild erythema; 2: moderate erythema; 3: severe erythema. Keratinization: 0: keratinization; 1: mild keratinization; 2: moderate keratinization; 3: severe keratinization. Scales: 0: no scales; 1: mild scales; 2: moderate scales; 3: severe scales. Chapping: 0: no chapping; 1: mild chapping; 2: moderate chapping; 3: severe chapping. A higher total score represented a more severe skin lesion. Variables are presented as frequencies (percentages) or mean ± standard deviation or median (Q3-Q1). Test value (X2-value for X2-test; Welch’s approximate for unpaired t-test with Welch correction; Mann-Whitney U-statistic for Mann-Whitney test). df: degree of freedom; CI: confidence interval; N/A: not applicable. P < 0.05 was considered as the criterion of remarkable discrepancies.
Skin lesion and pruritus scores
The skin lesion scores (Table 2) and pruritus scores (Table 3) of the two groups of patients with palmoplantar keratotic eczema were compared before and after treatment. The outcomes showed no statistical discrepancy between the two groups in line with erythema, keratinization, scales, chapping, and total lesion scores before treatment (P > 0.05, Mann-Whitney test), while after treatment, the above scores (erythema, keratinization, scales, chapping, and total lesion scores) of patients of the S group were much lower than those of the patients of the group C (P < 0.01, Kruskal-Wallis’ test/Dunn’s test). Sulfur cream blowing and parching treatment combined with compound ketoconazole cream improved skin lesion and pruritus scores after treatments.
Table 2.
Comparison of skin lesion scores for the two groups before and after treatment
| Variables | Control (C) group | Study (S) group | Comparisons between C and S groups at after treatment | |||
|---|---|---|---|---|---|---|
| Numbers of patients | 58 | 58 | Test-value | P-value | ||
| Erythema | Before treatment | 3 (3-2) | 3 (3-2) | 61.07 | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | |
| After treatment | 2 (3-2) | 2 (2-1) | ||||
| Comparisons between before and after treatment | Test-value | N/A | 68.163 | N/A | ||
| P-value | 0.084 (Wilcoxon matched-pairs test) | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | N/A | |||
| Keratinization | Before treatment | 2 (3-2) | 2.5 (3-2) | 1,451 | 0.1972 (Mann-Whitney test) | |
| After treatment | 2 (2-2) | 2 (2-1) | ||||
| Comparisons between before and after treatment | Test-value | 11.968 | 19.06 | N/A | ||
| P-value | < 0.05* (Kruskal-Wallis’ test/Dunn’s test) | < 0.01* (Kruskal-Wallis’ test/Dunn’s test) | ||||
| Scales | Before treatment | 2 (3-2) | 2 (3-2) | 25.652 | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | |
| After treatment | 2 (2-2) | 1 (2-1) | ||||
| Comparisons between before and after treatment | Test-value | N/A | 32.232 | N/A | ||
| P-value | 0.2004 (Wilcoxon matched-pairs test) | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | ||||
| Chapping | Before treatment | 2 (2-1) | 2 (2-1) | 39.221 | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | |
| After treatment | 2 (2-1) | 1 (1-1) | ||||
| Comparisons between before and after treatment | Test-value | 5.903 | 39.221 | N/A | ||
| P-value | 0.0523 (Kruskal-Wallis’ test) | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | ||||
| Total scores | Before treatment | 9 (10-8) | 9 (10-8) | 94.318 | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | |
| After treatment | 8 (9-7) | 6 (7-5) | ||||
| Comparisons between before and after treatment | Test-value | 24.25 | 94.318 | N/A | ||
| P-value | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | ||||
Erythema: 0: no erythema; 1: mild erythema; 2: moderate erythema; 3: severe erythema. Keratinization: 0: keratinization; 1: mild keratinization; 2: moderate keratinization; 3: severe keratinization. Scales: 0: no scales; 1: mild scales; 2: moderate scales; 3: severe scales. Chapping: 0: no chapping; 1: mild chapping; 2: moderate chapping; 3: severe chapping. A higher total score represented a more severe skin lesion. The data are described as median (Q3-Q1). Test value (Kruskal-Wallis’-statistic for Kruskal-Wallis’ test; Mann-Whitney-statistic for Mann-Whitney test). P < 0.05 was considered as the criterion of remarkable discrepancies.
P < 0.05.
Table 3.
Comparison of pruritus scores for the two groups before and after treatment
| Variables | Group C (n = 58) | Group S (n = 58) | Test-value | P | |
|---|---|---|---|---|---|
| Before treatment | 2 (3-2) | 2 (3-2) | 1,598 | 0.6412 (Mann-Whitney test) | |
| 1 week after treatment | 2 (3-2) | 2 (3-2) | 1,643 | 0.827 (Mann-Whitney test) | |
| Comparison with respect to before treatment | P | 0.3672 (Wilcoxon matched-pairs signed-ranks test) | > 0.05 (Kruskal-Wallis’ test/Dunn’s test) | N/A | N/A |
| Test-value | 1,520 | 53 | N/A | N/A | |
| 2 weeks after treatment | 2 (2-2) | 2 (2-2) | 1,612 | 0.693 (Mann-Whitney test) | |
| Comparison with respect to before treatment | P | 0.1601 (Wilcoxon matched-pairs signed-ranks test) | > 0.05 (Kruskal-Wallis’ test/Dunn’s test) | N/A | N/A |
| Test-value | 1.430 | 53 | N/A | N/A | |
| 4 weeks after treatment | 2 (2-2) | 1 (2-1) | 28.025 | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | |
| Comparison with respect to before treatment | P | < 0.05* (Kruskal-Wallis’ test/Dunn’s test) | < 0.001* (Kruskal-Wallis’ test/Dunn’s test) | N/A | N/A |
| Test-value | 8.7 | 53 | N/A | N/A | |
0: Pruritus; 1: mild pruritus and no irritation; 2: moderate pruritus but tolerable, and; 3: severe pruritus and unbearable. The data are described as median (Q3-Q). Test value (Kruskal-Wallis’-statistic for Kruskal-Wallis’ test; Mann-Whitney-statistic for Mann-Whitney test). P < 0.05 was considered as the criterion of remarkable discrepancies.
P < 0.05.
N/A: not applicable.
Moreover, no statistically remarkable discrepancy in pruritus scores was observed for patients of these two groups before treatment (P > 0.05, Mann-Whitney test). The pruritus scores in patients of group S were remarkably inferior to those in patients of group C at 1, 2, and 4 weeks after treatments (P < 0.05, Kruskal-Wallis’ test/Dunn’s test), and the score difference was shown to increase with treatment time (P < 0.05, Kruskal-Wallis’ test/Dunn’s test).
Quality of life and psychological status
The quality of life and psychological status of individuals in these two groups were assessed before and after treatment. The results showed no statistical differences in the daily life, physiological burden, and social interaction scores for these two groups before treatment (P > 0.05, Mann-Whitney test), while scores of patients of group S were remarkably higher than those of patients of group C after treatment (P < 0.01, Kruskal-Wallis’ test/Dunn’s test; Table 4). In addition, no statistical difference between the two groups in SAS and SDS was observed before treatment, and both SAS and SDS in patients of group C were significantly inferior to those in patients of group S after treatment (P < 0.01, Kruskal-Wallis’ test/Dunn’s test; Table 5). Sulfur cream blowing and parching treatment combined with compound ketoconazole cream improved the quality of life and psychological status of patients after treatment.
Table 4.
Comparison of quality of life for two groups before and after treatment
| Variables | Group C (n = 58) | Group S (n = 58) | t-value | P | df | 95% CI | |
|---|---|---|---|---|---|---|---|
| Daily Life | Before treatment | 61.83±5.15 | 61.83±5.15 | 0.318 | 0.7511 (Unpaired t test) | 114 | -2.119 to 1.533 |
| After treatment | 61.64±4.8 | 74.02±4.11 | 131.21 | < 0.01* (One-way ANOVA/Dunnett test) | 173 | N/A | |
| Physiological burden | Before treatment | 61.83±5.15 | 68.05±5.66 | 28.454 | < 0.01* (One-way ANOVA/Dunnett test) | 173 | N/A |
| After treatment | 61.6±4.83 | 74.05±4.1 | 93.535 | < 0.01* (One-way ANOVA/Dunnett test) | 173 | N/A | |
| Social Interaction | Before treatment | 61.83±5.15 | 61.59±4.83 | 28.6 | < 0.01* (One-way ANOVA/Dunnett test) | 173 | N/A |
| After treatment | 68.05±5.66 | 74.05±4.09 | 94 | < 0.01* (One-way ANOVA/Dunnett test) | 173 | N/A | |
The score ranged from 0 to 100. An upper total score represented a better quality of life. The data are described as mean ± standard deviation (SD). df: Degree of freedom; N/A: not applicable; CI: confidence interval; ANOVA: Analysis of variance. Test value (t-value for unpaired t-test or F-value for one-way ANOVA/Danette test). P < 0.05 was considered as the criterion of remarkable discrepancies.
P < 0.05.
Table 5.
Comparison of psychological status for these two groups before and after treatment
| Variables | Group C (n = 58) | Group S (n = 58) | Test value | P | Degree of freedom | 95% CI | |
|---|---|---|---|---|---|---|---|
| SAS | Before treatment | 57.48±4.95 | 57.24±5.05 | 0.2606 | 0.7949 (unpaired t-test) | 114 | -2.077 to 1.594 |
| After treatment | 49 (50-47) | 42 (45-40) | 108 | < 0.0001* (Kruskal-Wallis’ test/Dunn’s test) | N/A | N/A | |
| SDS | Before treatment | 57.47±4.94 | 57.25±5.01 | 0.27 | 0.7949 (unpaired t-test) | 114 | -2.08 to 1.6 |
| After treatment | 50 (50-47) | 43.5 (45-40) | 139 | < 0.0001* (Kruskal-Wallis’ test/Dunn’s test) | N/A | N/A | |
A higher score indicated poorer psychological status. The data are described as mean ± standard deviation (SD) or median (Q3-Q1). Test value (t-value for unpaired t-test; Kruskal-Wallis’-statistic for Kruskal-Wallis’ test). P < 0.05 was considered as the criterion of remarkable discrepancies.
P < 0.05.
SAS: Self-rating anxiety scale; SDS: Self-rating depressive scale; CI: Confidence interval; N/A: Not applicable.
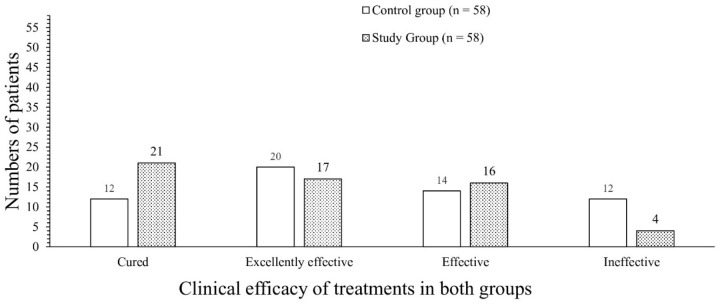
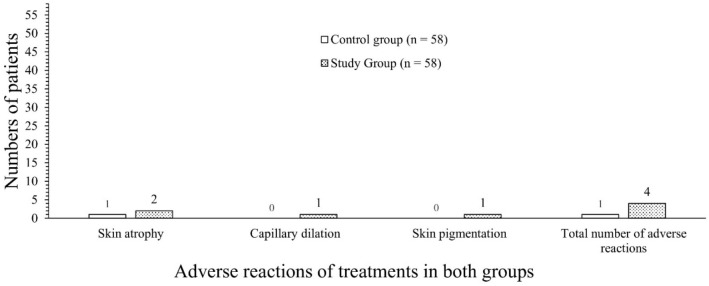
Clinical efficacy and adverse reactions
The clinical efficacy and the occurrence of adverse reactions between the two groups were also compared. As shown in Table 6 and Figure 2, 36% of patients in the group S were cured, while only 21% of patients in the group C were cured. The treatment overall response rate of group S was remarkably higher compared with that of group C (P < 0.05, X2-test). The adverse reactions mainly were skin atrophy, capillary dilation, and skin pigmentation, and these adverse reactions were significantly fewer in patients of group S than in patients of group C (P < 0.05, X2-test, Figure 3). Sulfur cream blowing and parching treatment combined with compound ketoconazole cream has better clinical efficacy and fewer adverse reactions. The results of the assumption tests are presented in Table 7.
Table 6.
Comparison of clinical efficacy and adverse reactions for these two groups
| Variables | Group C (n = 58) | Group S (n = 58) | χ2 statistics | P |
|---|---|---|---|---|
| Clinical efficacy | ||||
| Cured | 12 (21) | 21 (36) | 2.71 | 0.0997 |
| Excellently effective | 20 (34) | 17 (29) | 0.1587 | 0.6903 |
| Effective | 14 (24) | 16 (28) | 0.045 | 0.8321 |
| Ineffective | 12 (21) | 4 (7) | 3.553 | 0.0595 |
| Overall response rate | 46 (79) | 54 (93) | 5.362 | 0.02* |
| Adverse reactions | ||||
| Skin atrophy | 1 (2) | 2 (3) | 0.3422 | 0.5586 |
| Capillary dilation | 0 (0) | 1 (2) | 1.009 | 0.3152 |
| Skin pigmentation | 0 (0) | 1 (2) | 1.009 | 0.3152 |
| Total number of adverse reactions | 1 (2) | 4 (7) | 1.881 | 0.17 |
The data are expressed as frequencies (%). X2-value was used for statistical analysis. P < 0.05 was considered as the criterion of remarkable discrepancies.
P < 0.05.
Figure 2.
Bar chart of comparison of clinical efficacy between two groups. Variables are presented as frequencies. Cured: all lesions had subsided, and the symptoms had disappeared, with an efficacy index ≥ 95%; Excellently effective: most of the lesions had subsided, and the symptoms were significantly relieved, with 95% > efficacy index ≥ 70%; Effective: the lesions had partially subsided, and the symptoms were improved, with 70% > efficacy index ≥ 50%; Ineffective: alleviation of the lesion was not significant, the symptoms were not relieved and even deteriorated, with efficacy index < 50%.
Figure 3.
Bar chart of comparison of adverse reactions between two groups. Variables are presented as frequencies.
Table 7.
Results of assumption test
| Parameters | Test | Sub test |
|---|---|---|
| Categorical variable | Fisher exact test or X2-test (individual sample > 5 and total sample size ≥ 40). | |
| Age (between groups; years) | F = 1.580. The P value is 0.0436 for Barette’s test, i.e. alternate test for unequal SDs. | Unpaired t test with Welch correction |
| Disease course (between groups; months) | F = 1.557. The P value is 0.0487 for Barette’s test, i.e. alternate test for unequal SDs. | Unpaired t test with Welch correction |
| Skin lesion scores (within and between groups) | All column passed in normality tests > 0.05 then unpaired t-test or parametric test, if any one column failed in normality tests < 0.05, i.e. non-parametric tests. | |
| Pruritus scores and psychological status (between groups) | Any one column failed in normality tests < 0.05, i.e. non-parametric tests. | |
| Quality of life (between groups) | All column passed in normality tests > 0.05 then unpaired t-test or parametric test. | |
Discussion
Scores of erythema, keratinization, scales, chapping, pruritus, quality of life, and psychological status of patients enrolled in the study were worse before treatment. Due to its complex etiologies, long disease duration, and easy recurrent attacks after drug withdrawal, keratotic eczema is not only an intractable disease for clinical dermatology but also seriously impacts the study, work, daily life and psychological health of the patients [19]. As the effects of traditional methods have not been satisfying, identifying more effective treatments is necessary.
This study revealed higher response rates and lower incidence of adverse reactions in patients with palmoplantar keratotic eczema treated by sulfur cream blowing and parching combined with compound ketoconazole cream than in those treated with compound ketoconazole cream alone. It was reported that ketoconazole cream has a rapid onset of action, high safety, and plays a strong role in vasoconstriction, inflammation elimination, and fungus resistance [20]. Furthermore, sulfur cream blowing and parching are empirical therapies in our hospital. The sulfur powder in sulfur cream can be converted into hydrogen sulfide and pentane sulfonic acid after contact with the skin, which can effectively promote the differentiation of epidermal cells, the dissolution of stratum corneum, and the inhibition of bacteria [21]. Besides, sulfur cream can relieve pruritus and lubricate the skin well and has good therapeutic effects on dermatologic disorders of keratinization and skin disorders associated with tissues and organs [22]. As for blowing and parching, this method can promote blood circulation, reduce capillary permeability, enhance vascular endothelial repair, all of which are conducive to inflammatory skin recovery, reduce exudation and itching, and promote epidermis recovery. Altogether, we found that sulfur cream blowing and parching combined with compound ketoconazole cream exhibited good efficacy and high clinical value in the treatment of palmoplantar keratotic eczema.
Additionally, this study demonstrated the scores of erythema, keratinization, scales, chapping, and pruritus of patients with palmoplantar keratotic eczema treated with sulfur cream blowing and parching combined with compound ketoconazole cream were remarkably inferior to those of patients treated with compound ketoconazole cream alone. Nearly 20 years of relevant research revealed that the positive ratio and density of staphylococcus aureus and Malassezia were higher in skin lesion sites than in adjacent normal skin and that Malassezia was relatively more sensitive to compound ketoconazole cream [23]. Compound ketoconazole cream prevents the differentiation, growth, degeneration, and terminal differentiation of keratinocytes, inhibits the production of keratin, and restores the growth and differentiation of the skin at the epidermal lesions [24]. However, some scholars have also discovered that excessive use of hormonal drugs was not conducive to later treatments. Specifically, excessive hormonal medication can thicken the palmoplantar cuticle and cause drug resistance in a local areas rather than achieve therapeutic effects [25]. Sulfur cream has the effects of dissolving stratum corneum, inhibiting bacteria, reducing cortical secretion, and relieving itching [21]. Apart from alleviating the harmful effects of hormones in compound ketoconazole cream, sulfur cream blowing and parching combined with compound ketoconazole cream exerts functions in nondestructive sterilization and skin lesion repair.
Moreover, in this paper, patients with palmoplantar keratotic eczema treated with sulfur cream blowing and parching combined with compound ketoconazole cream exhibited an increase in the scores of daily life, psychological burden, and social interaction and a decrease in anxiety and depression. All scores were superior to those of patients taking compound ketoconazole cream alone. In addition, patients showed poor absorption and were prone to malignant complications after receiving external hormonal agents [25]. Long-term chronic diseases have a certain influence on the psychological state of patients, and some serious adverse events such as depression may even occur [26]. Thus, effective treatment could modulate psychological pressure and further the psychological state of the sufferer to a certain extent.
The study investigates the use of sulfur cream blowing and parching combined with compound ketoconazole cream for the treatment of palmoplantar keratotic eczema, which is a novel approach. Previous studies do not present any substantial new insights or advancements in the field and the current work has explored the individual use of these treatments. Nevertheless, due to the small sample size, there may be some bias and limitations in the data statistics, and the conclusions of this paper require further analysis for validation. In addition, there are lack of the validation of the evaluation methods used.
Conclusions
Compared with compound ketoconazole cream alone, sulfur cream blowing and parching combined with compound ketoconazole cream was significantly more effective in treating palmoplantar keratotic eczema, with the patients demonstrating better response rates, skin lesion scores, quality of life, and psychological status. Therefore, sulfur cream blowing and parching combined with compound ketoconazole should be further investigated and validated for potential use in clinical practice.
Acknowledgements
The authors are thankful to the medical and non-medical staff of the Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China.
Disclosure of conflict of interest
None.
Abbreviations
- SAS
Self-rating anxiety
- SAD
Self-rating depression
- SD
Standard deviation
- X2-test
Chi-square test
- ANOVA
Analysis of variance
References
- 1.Vasanthkumar YH, Chandrasekhar MH, Murugesh SB. Clinical aspects of palmoplantar dermatoses in patients attending tertiary health care centre. Int J Res Dermato. 2020;6:383–387. [Google Scholar]
- 2.Çetinarslan T, Türel Ermertcan A, Temiz P. Dermoscopic clues of palmoplantar hyperkeratotic eczema and palmoplantar psoriasis: a prospective, comparative study of 90 patients. J Dermatol. 2020;47:1157–1165. doi: 10.1111/1346-8138.15487. [DOI] [PubMed] [Google Scholar]
- 3.Thyssen JP, Menné T. Acute and recurrent vesicular hand dermatitis. In: Rustemeyer T, Elsner P, John SM, Maibach HI, editors. Kanerva’s Occupational Dermatology. Berlin, Heidelberg: Springer; 2012. [Google Scholar]
- 4.Pena J, Zameza PA, Pixley JN, Remitz A, Feldman SR. A comparison of topical corticosteroids and topical calcineurin inhibitors for the treatment of atopic dermatitis. J Allergy Clin Immunol Pract. 2023;11:1347–1359. doi: 10.1016/j.jaip.2023.03.022. [DOI] [PubMed] [Google Scholar]
- 5.Thomas BR, O’Toole EA. Diagnosis and management of inherited palmoplantar keratodermas. Acta Derm Venereol. 2020;100:adv00094. doi: 10.2340/00015555-3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frazier W, Bhardwaj N. Atopic dermatitis: diagnosis and treatment. Am Fam Physician. 2020;101:590–598. [PubMed] [Google Scholar]
- 7.Politiek K, Loman L, Pas HH, Diercks GFH, Lemmink HH, Jan SZ, van den Akker PC, Bolling MC, Schuttelaar MLA. Hyperkeratotic hand eczema: eczema or not? Contact Dermatitis. 2020;83:196–205. doi: 10.1111/cod.13572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thyssen JP, Schuttelaar MLA, Alfonso JH, Andersen KE, Angelova-Fischer I, Arents BWM, Bauer A, Brans R, Cannavo A, Christoffers WA, Crépy MN, Elsner P, Fartasch M, Filon FL, Giménez-Arnau AM, Gonçalo M, Guzmán-Perera MG, Hamann CR, Hoetzenecker W, Johansen JD, John SM, Kunkeler ACM, Hadzavdic SL, Molin S, Nixon R, Oosterhaven JAF, Rustemeyer T, Serra-Baldrich E, Shah M, Simon D, Skudlik C, Spiewak R, Valiukevičienė S, Voorberg AN, Weisshaar E, Agner T. Guidelines for diagnosis, prevention, and treatment of hand eczema. Contact Dermatitis. 2022;86:357–378. doi: 10.1111/cod.14035. [DOI] [PubMed] [Google Scholar]
- 9.Rana P, Ghadlinge M, Roy V. Topical antifungal-corticosteroid fixed-drug combinations: need for urgent action. Indian J Pharmacol. 2021;53:82–84. doi: 10.4103/ijp.ijp_930_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashara KC, Paun JS, Soniwala MM, Chavda JR. Microemulgel of voriconazole: an unfathomable protection to counter fungal contagiousness. Folia Med (Plovdiv) 2017;59:461–471. doi: 10.1515/folmed-2017-0051. [DOI] [PubMed] [Google Scholar]
- 11.Raney SG, Ghosh P, Ramezanli T, Lehman PA, Franz TJ. Cutaneous pharmacokinetic approaches to compare bioavailability and/or bioequivalence for topical drug products. Dermatol Clin. 2022;40:319–332. doi: 10.1016/j.det.2022.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Bandyopadhyay D. Topical antibacterials in dermatology. Indian J Dermatol. 2021;66:117–125. doi: 10.4103/ijd.IJD_99_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao YK, Lu JF, Liu JH, Wu HH, Song LL, Wan CL, Luo DQ. Recalcitrant nodular scabies showing excellent response to tofacitinib: five case reports. Ther Adv Chronic Dis. 2023;14:20406223231195632. doi: 10.1177/20406223231195632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Immunology Group, Chinese Society of Dermatology; Guideline Formulation and Standardization Committee, and China Dermatologists Association. Expert consensus on standardized diagnostic terminology of dermatitis and eczematous diseases. Chinese Journal of Dermatology. 2021;54:937–942. [Google Scholar]
- 15.Abdlaty E, Doerwald-Munoz L, Madooei A, Sahli S, Yeh SA, Zerubia J, Wong RK, Hayward JE, Farrell TJ, Fang Q. Hyperspectral imaging and classification for grading skin erythema. Front Phys. 2018;6:1–10. [Google Scholar]
- 16.Xu M, Xu X, Wang X, Shi W, Zhang J, Xue J. Localization and the evaluation of reliability and validity of four-item scale about pruitus. Chinese Journal of Practical Nursing. 2015;31:1150–1153. [Google Scholar]
- 17.Le QM, Sun PW, Liu YZ. Curative effect of Jiedu Zhiyang lotion combined with white vaseline ointment in the treatment of keratotic eczema. Chinese Journal of Integrative Dermatology and Venereology. 2022;38:314–317. [Google Scholar]
- 18.Zhang Y, Liu R, Li G, Mao S, Yuan Y. The reliability and validity of a Chinese-version short health anxiety inventory: an investigation of university students. Neuropsychiatr Dis Treat. 2015;11:1739–1747. doi: 10.2147/NDT.S83501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang D, Tang Z, Qiu X, Liu X, Guo Z, Yang B, Guo Q, Xiong H. Hand eczema among healthcare workers in Guangzhou city: a cross-sectional study. Ann Transl Med. 2020;8:1664. doi: 10.21037/atm-20-7652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abd El-Baky RM, Sandle T, John J, Abuo-Rahma GEA, Hetta HF. A novel mechanism of action of ketoconazole: inhibition of the NorA efflux pump system and biofilm formation in multidrug-resistant Staphylococcus aureus. Infect Drug Resist. 2019;12:1703–1718. doi: 10.2147/IDR.S201124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asilian A, Mohammadian P, Hosseini SM, Heidaripour F, Yekta A, Nateghi MR. Comparison of the effect of topical triamcinolone 0.1% cream with sulfur 2.0% cream in the treatment of patients with hand eczema: a randomized controlled trial. J Cosmet Dermatol. 2024;23:1753–1757. doi: 10.1111/jocd.16208. [DOI] [PubMed] [Google Scholar]
- 22.Arslan H, Gündüz Ö. Bullous scabies, the light shed on etiopathogenesis and treatment: report of five paediatric cases. Postepy Dermatol Alergol. 2023;40:432–436. doi: 10.5114/ada.2023.128976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song F. Bacteriological study on skin lesions of eczema and atopic dermatitis. Investigación Clínica. 2020;61:989–997. [Google Scholar]
- 24.Yang W, Yang X, Shi F, Liao Z, Liang Y, Yu L, Wang R, Li Q, Bi K. Qualitative and quantitative assessment of related substances in the compound ketoconazole and clobetasol propionate cream by HPLC-TOF-MS and HPLC. J Pharm Anal. 2019;9:156–162. doi: 10.1016/j.jpha.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pérez P. The mineralocorticoid receptor in skin disease. Br J Pharmacol. 2022;179:3178–3189. doi: 10.1111/bph.15736. [DOI] [PubMed] [Google Scholar]
- 26.Ma Y, Xiang Q, Yan C, Liao H, Wang J. Relationship between chronic diseases and depression: the mediating effect of pain. BMC Psychiatry. 2021;21:436. doi: 10.1186/s12888-021-03428-3. [DOI] [PMC free article] [PubMed] [Google Scholar]