Abstract
Purpose: To characterize the clinical features and outcomes of open-globe injuries with associated retinal detachment (RD). Methods: A retrospective review was performed. Results: Thirty-six patients with open-globe injuries and subsequent rhegmatogenous RD were analyzed between January 2016 and September 2021. The median time to diagnosis and to the initial vitrectomy repair was 2.5 days and 20 days, respectively. Six months postoperatively, the median Snellen best-corrected visual acuity (BCVA) improved from light perception to hand motions. The logMAR BCVAs were significantly higher (worse) for patients who had more than 20 days between their injury and the initial vitrectomy repair (P = .01) and if their retinal detachment after open-globe injury score was higher than 5 (P = .03). The number of days between the open-globe injury and the initial vitrectomy repair was directly correlated with the final logMAR BCVA (P = .03). On multivariate analysis, a duration of more than 20 days between the open-globe injury and the initial vitrectomy repair was statistically significant for predicting the 6-month logMAR BCVA (P = .02). Conclusions: The final visual outcome for cases of RD associated with open-globe injury may be improved by minimizing the time between the injury and the initial vitrectomy repair.
Keywords: ocular trauma, open-globe injury, retinal detachment, vitrectomy
Introduction
Of the approximately 200 000 open-globe injuries that occur annually in the United States, the rate of cases of rhegmatogenous retinal detachment (RRD) presenting at or within 24 hours ranges from 2.5% to 39.9%. 1 In addition to the presence of RD, an initial best-corrected visual acuity (BCVA) of hand motions (HM) or worse, a relative afferent pupillary defect, and posterior extension of the injury are reported to predict poor visual outcomes after an open-globe injury.1 –5 Few studies, however, have evaluated the outcomes of subsequent RD after repair of this type of injury. Determining the incidence of subsequent RD is complicated by the lack of follow-up in some studies as well as the difficulty in assessing the posterior segment of an eye with a previous open-globe injury.1 –6
Trauma-related factors that are more highly associated with RD after open-globe injury include the presence of vitreous hemorrhage, a higher Ocular Trauma Classification Group zone of injury, a longer wound length (>10 mm), vitreous loss, blunt trauma, and a retained intraocular foreign body (IOFB).4,6 The visual prognosis after RD is variable, with preoperative attachment of the macula having a more favorable outcome1,7 –9; the prognosis after RDs resulting from penetrating injuries is also worse than that for blunt injuries.6,10 Traumatic proliferative vitreoretinopathy (PVR) and tractional RD are additional risk factors for a poor functional outcome after injury. 11 Likewise, the extent of the RD (number of quadrants) is inversely related to the visual outcome and directly related to the likelihood of subsequent enucleation. 12
More than one half of RDs occurring after an open-globe injury are diagnosed 1 week or more after the initial trauma. Risk factors and clinical outcomes of concomitant RDs diagnosed shortly after open-globe injury have not been well studied. The objectives of this study were to understand the clinical features and outcomes of RDs diagnosed after open-globe injury. Understanding the preoperative and intraoperative risk factors of early-onset or concomitant RDs may assist the clinician in planning follow-up and counseling for patients.
Methods
An institutional review board–approved single-center retrospective chart review was performed of all patients who presented with open-globe injuries and developed early-onset RDs, defined as occurring within 14 days of the initial injury. All patients were evaluated at the University of Illinois at Chicago from January 2016 to September 2021. A vitreoretinal faculty member diagnosed all cases of RD. Patients presenting with an RD 14 days after the initial injury or patients without an RD were excluded. Patients with less than 6 months of follow-up (19 patients) after RD repair were also excluded from the study.
Collected data included demographics, medical history, information pertaining to the mechanism and location of the ocular injury, ocular injury parameters, surgical intervention, time between the diagnosis and repair of the globe injury and the occurrence of RD, and the postoperative visual and anatomic outcomes. The ocular trauma score and the retinal detachment after open-globe injury score were calculated, and the results were correlated with the patient outcomes. The VA was obtained using standard clinic Snellen charts and then converted to logMAR notation for statistical purposes.
Univariate and multivariate analyses were performed to determine the association between baseline factors and the VA and anatomic outcomes. Statistical comparisons were performed with Student t tests, the Fisher exact test, and χ2 tests in addition to logistic and linear regression analysis for univariate models and multivariate models. Statistical significance was set at P < .05 and a 95% CI not including 1.0. All statistical analyses were performed using R software (version 4.1.1, R Foundation for Statistical Computing).
Results
There were 214 open-globe injuries between January 2016 and September 2021. After excluding patients lost to follow-up, those with incomplete records, those who underwent enucleation, and those who did not meet the inclusion criteria for RD diagnosis and repair, 36 patients were eligible for inclusion in the study (Figure 1). Twenty-five patients (69.4%) were men, and the median age was 48.5 years (range, 13-82). Table 1 shows the preoperative patient characteristics and BCVA outcomes.
Figure 1.
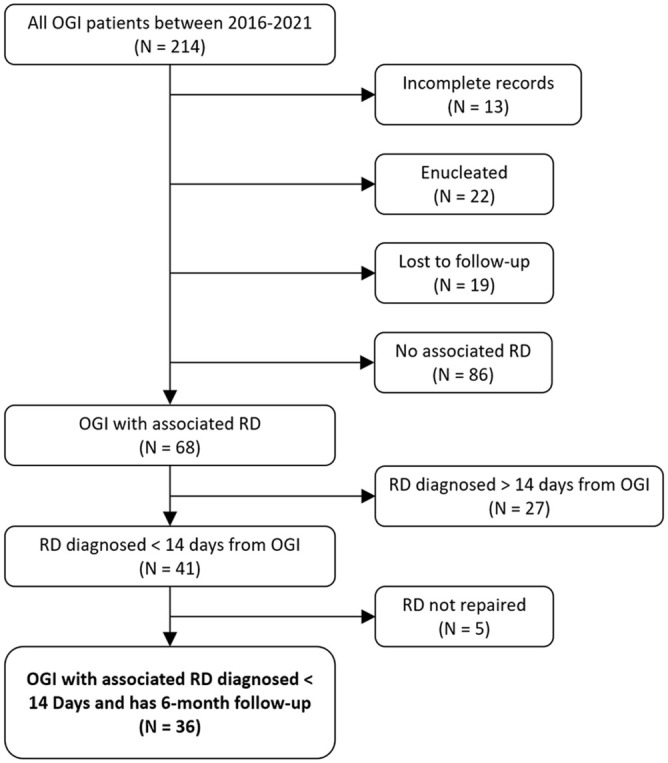
Flow diagram of inclusion criteria.
Abbreviations: OGI, open-globe injury; RD, retinal detachment.
Table 1.
Preoperative Characteristics and BCVA Outcomes.
| Parameter | Number (%) | Mean BCVA | |||||
|---|---|---|---|---|---|---|---|
| Presenting | At 6 Months | ||||||
| LogMAR | Snellen | P Value | LogMAR | Snellen | P Value | ||
| RD-OGI score | <.01 a | .03 a | |||||
| <5 | 18 (50.0) | 2.11 | 20/4000 | 1.69 | 20/800 | ||
| ≥5 | 18 (50.0) | 2.69 | 20/10 000 | 2.19 | 20/4000 | ||
| Ocular trauma classification | .87 | .87 | |||||
| Zone 1 | 10 (27.8) | 2.32 | 20/4000 | 1.97 | 20/2000 | ||
| Zone 2 | 5 (13.9) | 2.34 | 20/4000 | 2.1 | 20/4000 | ||
| Zone 3 | 21 (58.3) | 2.46 | 20/10 000 | 1.89 | 20/2000 | ||
| No view of AC or traumatic hyphema | .02 a | .10 | |||||
| Yes | 23 (63.9) | 2.63 | 20/10 000 | 2.08 | 20/4600 | ||
| No | 13 (36.1) | 1.99 | 20/2000 | 1.69 | 20/800 | ||
| Injury type | <.01 a | .35 | |||||
| Blunt | 22 (61.1) | 2.70 | 20/10 000 | 2.10 | 20/4000 | ||
| Penetrating | 10 (27.8) | 1.96 | 20/2000 | 1.65 | 20/800 | ||
| Perforating | 4 (11.1) | 1.90 | 20/2000 | 1.82 | 20/2000 | ||
| Gunshot wound | .08 | .25 | |||||
| Yes | 3 (8.3) | 1.30 | 20/400 | 1.43 | 20/500 | ||
| No | 33 (91.7) | 2.50 | 20/10 000 | 1.99 | 20/2000 | ||
| External globe deformity | .03 a | .09 | |||||
| Yes | 25 (69.4) | 2.61 | 20/10 000 | 2.08 | 20/4000 | ||
| No | 11 (30.6) | 1.94 | 20/2000 | 1.62 | 20/800 | ||
| IOFB | .01 a | .05 a | |||||
| Yes | 10 (27.8) | 1.72 | 20/800 | 1.50 | 20/630 | ||
| No | 26 (72.2) | 2.67 | 20/10 000 | 2.11 | 20/4000 | ||
Abbreviations: AC, anterior chamber; BCVA, best-corrected visual acuity; IOFB, intraocular foreign body; RD-OGI, retinal detachment after open-globe injury.
Statistically significant at the 5% level.
The most common mechanism of open-globe injury was blunt trauma (61.1%), and all injuries were repaired within 24 hours of presentation. Four patients had simultaneous open-globe repair and pars plana vitrectomy (PPV) for RD. Of the 36 RDs, 39% were macula-on, 66.7% were anterior to the equator, 11.1% were equatorial, and 22.2% were posterior to the equator. The median interval from the open-globe injury to the RD diagnosis was 2.5 days (range, 0-13); 52.8% presented before 5 days. RDs were noted to occur sooner after open-globe injury if there was an associated IOFB or perforating injury (both P < .01). The median time from open-globe injury to initial vitrectomy repair was 20 days.
The median logMAR VA at presentation was 2.7 (20/10 000) (range, 1.0 [20/200]-3.0 [20/20 000]). The median time from the injury to presentation was 8 hours. Four patients presented more than 24 hours after their initial injury, although their median presenting and final VA were equivalent to that of the other patients. There was no significant independent correlation between the time to presentation and the final VA (R 2 = 0.008; P = .60). The median ocular trauma score at presentation was 1 (raw score, 36; range, 12-66). The median retinal detachment after open-globe injury score was 4.75 (range, 0-7.5). At presentation, the BCVA was significantly worse for patients with macula-off detachments (P = .01), an obscured view of the anterior chamber or traumatic hyphema (P = .02), blunt injuries (P < .01), external globe deformity (P = .03), or choroidal detachment (P = .02). The initial BCVA was more favorable in patients who developed RDs soon (within 5 days) after the open-globe injury (P = .03) and those with an IOFB (P = .01). Table 2 shows the characteristics of the RDs and the BCVA outcomes.
Table 2.
RD Characteristics and BCVA Trajectories.
| Parameter | Number (%) | Mean BCVA | |||||
|---|---|---|---|---|---|---|---|
| Presenting | At 6 Months | ||||||
| LogMAR | Snellen | P Value | LogMAR | Snellen | P Value | ||
| Macula | .01 a | .07 | |||||
| On | 14 (38.9) | 1.97 | 20/2000 | 1.66 | 20/800 | ||
| Off | 22 (61.1) | 2.68 | 20/10 000 | 2.12 | 20/4000 | ||
| RD diagnosed within 5 days of OGI | .03 a | .42 | |||||
| Yes | 19 (52.8) | 2.11 | 2.64 (20/10 000) | 1.97 | 20/2000 | ||
| No | 17 (47.2) | 2.34 | 20/4000 | 1.92 | 20/2000 | ||
| Vitrectomy >20 days after OGI | .01 a | .01 a | |||||
| Yes | 18 (50) | 2.67 | 20/10 000 | 2.24 | 20/4000 | ||
| No | 18 (50) | 2.13 | 20/4000 | 1.64 | 20/800 | ||
| PVR | .13 | .20 | |||||
| Yes | 20 (55.6) | 2.54 | 20/10 000 | 2.05 | 20/2000 | ||
| No | 16 (44.4) | 2.23 | 20/4000 | 1.81 | 20/2000 | ||
| Vitreous heme | .27 | .32 | |||||
| Yes | 31 (86.1) | 2.45 | 20/10 000 | 1.98 | 20/2000 | ||
| No | 5 (13.9) | 2.10 | 20/4000 | 1.72 | 20/800 | ||
| Equatorial RD | .09 | .11 | |||||
| Yes | 4 (11.1) | 1.45 | 20/500 | 1.20 | 20/320 | ||
| No | 32 (88.9) | 2.52 | 20/10 000 | 2.03 | 20/2000 | ||
| RD anterior to equator | .10 | .05 a | |||||
| Yes | 24 (66.7) | 2.53 | 20/10 000) | 2.14 | 20/4000 | ||
| No | 12 (33.3) | 2.15 | 20/4000 | 1.55 | 20/800 | ||
| Macular hole | .13 | .31 | |||||
| Yes | 5 (13.9) | 2.60 | 20/10 000 | 2.10 | 20/4000 | ||
| No | 31 (86.1) | 2.37 | 20/4000 | 1.92 | 20/2000 | ||
| Subretinal heme | .29 | .39 | |||||
| Yes | 14 (38.9) | 2.48 | 20/10 000 | 1.99 | 20/2000 | ||
| No | 22 (61.1) | 2.35 | 20/4000 | 1.91 | 20/2000 | ||
| Suprachoroidal heme | .33 | .38 | |||||
| Yes | 3 (8.3) | 2.00 | 20/2000 | 1.67 | 20/800 | ||
| No | 33 (91.7) | 2.44 | 20/4000 | 1.97 | 20/2000 | ||
| Choroidal detachment | .02 a | .07 | |||||
| Yes | 14 (38.9) | 2.66 | 20/10 000 | 2.18 | 20/4000 | ||
| No | 22 (61.1) | 2.24 | 20/4000 | 1.79 | 20/2000 | ||
Abbreviations: BCVA, best-corrected visual acuity; OGI, open-globe injury; PVR, proliferative vitreoretinopathy; RD, retinal detachment.
Statistically significant at the 5% level.
Retinal tamponade included silicone oil (SO) in 25 patients, perfluoropropane gas in 6 patients, sulfur hexafluoride gas in 2 patients, and air in 1 patient. For the remaining 2 patients, no tamponade agent was used because it was deemed that the detachment could not be repaired intraoperatively.
After 6 months, the median logMAR BCVA was 2.3 (Snellen equivalent, 20/4000), which corresponded to a median improvement in clinic-obtained Snellen acuity from light perception (LP) to HM. The VA ranged preoperatively from 20/25 to no LP (NLP) and postoperatively from 20/20 to NLP. During this period, 23 patients (63.9%) had an improvement in vision. For the 4 cases that had simultaneous open-globe repair and PPV, the median presenting logMAR VA was 1.3 (Snellen equivalent, 20/400) and the median final logMAR VA was 1.8 (Snellen equivalent, counting fingers). The logMAR BCVA was significantly worse in cases in which the duration between the injury and the initial vitrectomy repair was more than 20 days (P = .01) and the retinal detachment after open-globe injury score was 5 or higher (P = .03). Of note, 2 patients were found to have macular scars and thus had no visual improvement postoperatively. Five patients had RDs that could not be repaired. Twenty patients had PVR. Fourteen patients had gas or SO without a postoperative refraction, and 27 patients had lenticular opacities or uncorrected aphakia.
Univariate linear regression analysis showed that the presenting BCVA (P = .01) and ocular trauma score (P = .04) were significant predictors of 6-month BCVA (ie, a higher ocular trauma score being predictive of better BCVA). During this period, 13 patients (36.1%) required a second RD repair. Patients who required a second RD repair were more likely to have initially presented with a lower ocular trauma score (28 vs 37; P < .01).
Univariate analysis found the number of days between the open-globe injury and the initial vitrectomy (P = .03) was a significant predictor of the 6-month BCVA, as was a duration between the open-globe injury and the initial vitrectomy of 20 or more days (P = .02) (Figure 2). Table 3 shows the demographic and ocular findings of patients who had PPV less than 20 days after their open-globe injury and those who had PPV more than 20 days after. A multivariate model using a stepwise approach for predicting the 6-month BCVA was developed and included the following variables: a duration of 20 or more days between the open-globe injury and the initial vitrectomy repair (P = .02), equatorial RD (P = .08), macula-off RD (P = .07), and days between the open-globe injury and RD (P = .15) (Table 4).
Figure 2.
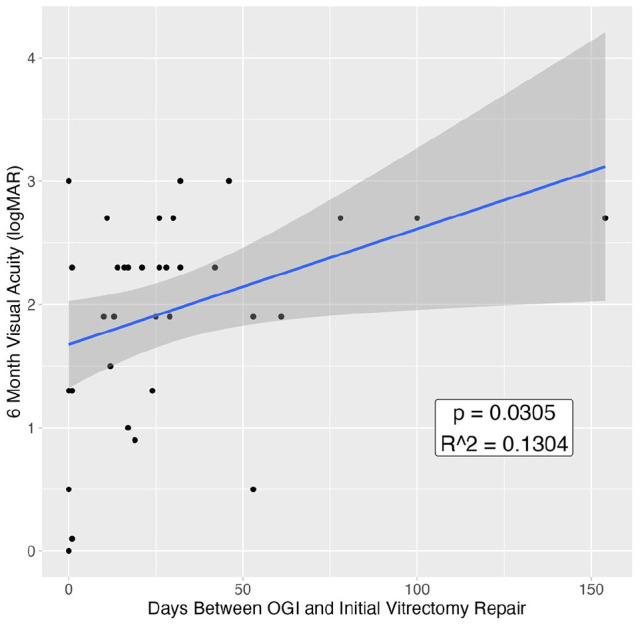
Relationship between time from OGI to initial vitrectomy repair and 6-month visual acuity.
A statistically significant relationship was observed between these 2 variables, with patients who had more time between the OGI and the initial vitrectomy having worse (higher logMAR) visual acuity at 6 months.
Abbreviation: OGI, open-globe injury.
Table 3.
Patient Characteristics Stratified by Timing of PPV After OGI.
| Variable | Vitrectomy <20 Days From OGI | Vitrectomy ≥20 Days From OGI | P Value |
|---|---|---|---|
| Mean logMAR VA | |||
| Baseline | 2.13 | 2.67 | .03 a |
| Final | 1.64 | 2.24 | .02 a |
| Mean age (y) | 45.5 | 49 | .58 |
| Lens status, n (%) | .21 | ||
| No view | 6 (33.3) | 12 (66.7) | |
| Clear | 4 (22.2) | 2 (11.1) | |
| Cataract | 4 (22.2) | 1 (5.5) | |
| Rupture/violated lens capsule | 3 (16.7) | 2 (11.1) | |
| Not available | 1 (5.6) | 1 (5.6) | |
| Ocular trauma classification, n (%) | .80 | ||
| Zone 1 | 6 (33.3) | 4 (22.2) | |
| Zone 2 | 2 (11.1) | 3 (16.7) | |
| Zone 3 | 10 (55.6) | 11 (61.1) | |
| IOFB, n (%) | <.01 a | ||
| Yes | 10 (44.4) | 0 | |
| No | 8 (55.6) | 18 (100) | |
| OTS, n (%) | .34 | ||
| 1 | 14 (77.8) | 17 (94.4) | |
| 2 | 3 (16.7) | 1 (5.56) | |
| 3 | 1 (5.5) | 0 (0) | |
| 4 | 0 | 0 (0) | |
| 5 | 0 | 0 (0) | |
| Mean RD-OGI score | 4.67 | 5.5 | .14 |
| PVR, n (%) | .74 | ||
| Yes | 9 (50) | 11 (61.1) | |
| No | 9 (50) | 7 (38.9) | |
| RD quadrants, n (%) | .03 a | ||
| 1 | 7 (38.9) | 0 | |
| 2 | 2 (11.1) | 3 (16.7) | |
| 3 | 0 | 1 (5.5) | |
| 4 | 9 (50) | 14 (77.8) | |
| Vitreous hemorrhage, n (%) | 1 | ||
| Yes | 16 (88.9) | 15 (83.3) | |
| No | 2 (11.1) | 3 (16.7) | |
| Mean days since OGI of RD | 2.78 | 6.22 | .01 a |
Abbreviations: IOFB, intraocular foreign body; OGI, open-globe injury; OTS, Ocular Trauma Score; PPV, pars plana vitrectomy; PVR, proliferative vitreoretinopathy; RD, retinal detachment; RD-OGI, retinal detachment after open globe injury; VA, visual acuity.
Statistically significant at the 5% level.
Table 4.
Multivariate Analysis Results.
| Variable | Estimate | SE | P Value |
|---|---|---|---|
| Vitrectomy >20 days after OGI | 0.6376 | 0.2616 | .02 a |
| Equatorial RD | −0.7009 | 0.3852 | .08 |
| Macula-on RD | −0.4945 | 0.2584 | .07 |
| Days between OGI and RD | −0.0479 | 0.0327 | .15 |
Abbreviations: OGI, open-globe injury; RD, retinal detachment.
Statistically significant at the 5% level.
Conclusions
Multiple previous studies have examined the incidence and risk factors for RD after open-globe injury, although to our knowledge none has specifically evaluated the unique features and outcomes in eyes that develop RDs within 2 weeks of injury. We chose a threshold of 14 days between the injury and the RD diagnosis for inclusion in our case series, in alignment with a study analyzing posttraumatic RD with the same definition. 13 The BCVA at 6 months was considered equivalent to the patient’s final BCVA, an accepted duration for maximum recovery of VA after blunt ocular trauma. 14
Sixty-one percent of RDs were macula-off, suggesting that the visual prognosis may be better with a careful and early referral to a retina specialist. On presentation, more than one half of patients with open-globe injuries and concomitant RDs had no view of the anterior chamber or a traumatic hyphema, which can make the initial assessment difficult and the long-term visual prognosis poor. Furthermore, as shown in previous studies,5,15,16 a large portion of patients presented with vitreous hemorrhage (87%), where conservative management in nontraumatic cases has been shown to lead to a higher incidence of retinal breaks, RDs, and PVR. The presence of a choroidal detachment was associated with a poorer initial BCVA and final BCVA, although postoperatively the improvement in BCVA was similar to that in cases with and cases without choroidal detachment. A significant portion of cases (63%) presented after a blunt mechanism of injury, suggesting that the mechanism of injury may contribute to the development of an RD. In addition, the majority (77%) of injuries presented with some deformity external to the globe (ie, lid laceration); thus, in the presence of such injuries, there should be a high level of concern for additional posterior segment pathology. Nearly one half of the cases developed PVR, the high possibility of which should be disclosed and discussed with the patient.
Surprisingly, patients with an IOFB had a better presenting BCVA and final BCVA than patients who did not have an IOFB. Patients with an IOFB were also significantly more likely than patients without an IOFB to develop an RD sooner (defined as less than 5 days between the open-globe injury and RD, the median time in our dataset) after open-globe injury. The shorter time to diagnosis and repair may contribute to a better final BCVA. As established by Liu et al, 17 the prognosis of IOFBs is variable and depends on several factors, including the presenting BCVA. On review of our cases with IOFBs in the series, 3 of 7 had a presenting logMAR BCVA of 0.5 or lower (Snellen equivalent, 20/60 or higher), significantly better than the average presenting BCVA of all cases in our study. These patients in particular should be counseled about the importance of follow-up with a retina specialist.
The ocular trauma score is a widely accepted tool used in ocular trauma to provide clinicians with valuable visual prognostic information. 18 The retinal detachment after open-globe injury score, established by Stryjewski et al, 6 calculates the cumulative probability of developing an RD by evaluating the presenting BCVA, zone of injury, and presence of a vitreous hemorrhage. One of the objectives of our study was to assess the predictive value of these scores in the setting of open-globe injury and subsequent RRD. In our study population, retinal detachment after open-globe injury scores higher than 5 were predictive of a worse initial BCVA and final BCVA. Our findings also indicate that a low ocular trauma score on presentation may be predictive of requiring a second RD repair. These scores may thus still provide valuable prognostic information in the setting of concomitant RDs, contrary to what has been established in other studies.13,19
Our findings suggest that the number of days between the open-globe injury and the initial vitrectomy was a critical factor in predicting the final visual outcome at 6 months. A time to the initial repair of more than 20 days, which was the median interval in our study, was associated with a worse final BCVA. This remained true on multivariate analysis even when controlling for the presenting BCVA. Of the 14 cases in which the repair was performed more than 20 days after the diagnosis of RD, 9 (64%) were the result of a delayed retina referral or scheduling-related issues and were confirmed to have had modifiable reasons for delay (ie, appointment rescheduling by the patient or other scheduling issues, or transportation reasons that led to delayed repair, as opposed to a delay that was medically indicated/recommended). The other cases involved a poor corneal view, required care coordination for dual penetrating keratoplasty, had hemorrhagic choroidal detachments, or had NLP. Notably, an RD diagnosis within 5 days of the open-globe injury was not a statistically significant predictor of the final BCVA. This suggests that clinicians should maintain a high index of suspicion for the development of an RD with a longer duration and that a strong emphasis on prompt RD repair can result in improved final VA and outcomes. Of the 4 cases that had simultaneous open-globe repair and PPV for RD, there was a small decline in the median logMAR VA at 6 months, suggesting that simultaneous repair may have unique consequences for the long-term visual potential of the eye. Further research is needed to compare the risks and benefits of simultaneous repair.
Multivariate regression analysis of the baseline factors showed that a duration of more than 20 days between the open-globe injury and the initial vitrectomy was significant for predicting the final BCVA, thus supporting the tenet of prompt repair of this type of RD. It is generally accepted that earlier intervention minimizes the risk for PVR, 20 in particular in younger individuals with open-globe injuries. In our series, the presence of PVR was present in more than one half of the patients and was associated with a less favorable initial VA and final VA. Given the many reasons for poor visual outcomes among all our patients, however, these figures did not reach statistical significance.
Our study has several limitations, most notably related to its retrospective design and sample size. Furthermore, we included only patients who had at least 6 months of follow-up. Beyond 6 months, more than one half of our study population (19 patients) was lost to follow-up. A future, larger scale study may consider assessing the longer term visual outcomes in similar cases of ocular trauma.
Footnotes
Authors’ Note: Presented at the annual meeting of the Association for Research and Vision in Ophthalmology, April 26, 2023, New Orleans, LA, USA.
Ethical Approval: This study was conducted in accordance with the Declaration of Helsinki. The collection and evaluation of all protected patient health information were performed in a US Health Insurance Portability and Accountability Act–compliant manner. Ethical approval for this study was obtained from the Institutional Review Board, University of Illinois at Chicago (2021-1481).
Statement of Informed Consent: Informed consent was not obtained because no patient identifiers were included.
Dr. Massengill has patent royalties with Iveric Bio unrelated to the present work. Dr. Lim is a consultant to Allergan, Aura, Cognition, Eyenuk, Iveric Bio, JAMA Ophthalmology Editorial Board, Luxa, Novartis Pharma AG, Opthea, Quark, Regeneron, Roche/Genentech, Inc, Santen, Unity, and Viridian; receives other grant support from Adverum, Aldeyra, Chengdu Kanghong, Graybug, Janssen, NGM Bio, Ocugen, RegenexBio, Roche/Genentech, Inc, Spring Vision, and Stealth; receives patent royalties from CRC Press/Taylor and Francis; and is a recipient honoraria of Alimera, Genentech/Roche. None of the other authors declared potential conflicts of interest with respect to the research, authorship, and/or publication of the article.
Funding: This study was supported by an Institutional Grant from Research to Prevent Blindness and an NIH Core Grant for vision research awarded to the University of Illinois at Chicago (EY01792).
ORCID iDs: Neil Sheth  https://orcid.org/0000-0003-2345-2918
https://orcid.org/0000-0003-2345-2918
Arthur Y. Chang  https://orcid.org/0000-0002-4090-4675
https://orcid.org/0000-0002-4090-4675
John M. Bryan  https://orcid.org/0000-0003-2085-5113
https://orcid.org/0000-0003-2085-5113
References
- 1. Chee YE, Patel MM, Vavvas DG. Retinal detachment after open-globe injury. Int Ophthalmol Clin. 2013;53(4):79-92. [DOI] [PubMed] [Google Scholar]
- 2. Andreoli MT, Andreoli CM. Surgical rehabilitation of the open globe injury patient. Am J Ophthalmol. 2012;153(5):856-860. doi: 10.1016/j.ajo.2011.10.013 [DOI] [PubMed] [Google Scholar]
- 3. Al-Mezaine HS, Osman EA, Kangave D, Abu El-Asrar AM. Prognostic factors after repair of open globe injuries. J Trauma. 2010;69:943-947. [DOI] [PubMed] [Google Scholar]
- 4. Entezari M, Rabei HM, Badalabadi MM, Mohebbi M. Visual outcome and ocular survival in open-globe injuries. Injury. 2006;37:633-637. [DOI] [PubMed] [Google Scholar]
- 5. Lin H, Lema GM, Yoganathan P. Prognostic indicators of visual acuity after open globe injury and retinal detachment repair. Retina. 2016;36(4):750-757. [DOI] [PubMed] [Google Scholar]
- 6. Stryjewski TP, Andreoli CM, Eliott D. Retinal detachment after open globe injury. Ophthalmology. 2014;121(1):327-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sarrazin L, Averbukh E, Halpert M, Hemo I, Rumelt S. Traumatic pediatric retinal detachment: a comparison between open and closed globe injuries. Am J Ophthalmol. 2004;137:1042-1049. [DOI] [PubMed] [Google Scholar]
- 8. Rouberol F, Denis P, Romanet JP, Chiquet C. Comparative study of 50 early- or late-onset retinal detachments after open or closed globe injury. Retina. 2011;31:1143-1149. [DOI] [PubMed] [Google Scholar]
- 9. Nashed A, Saikia P, Herrmann WA, Gabel VP, Helbig H, Hillenkamp J. The outcome of early surgical repair with vitrectomy and silicone oil in open-globe injuries with retinal detachment. Am J Ophthalmol. 2011;151:522-528. [DOI] [PubMed] [Google Scholar]
- 10. Meredith TA, Gordon PA. Pars plana vitrectomy for severe penetrating injury with posterior segment involvement. Am J Ophthalmol. 1987;103:549-554. [DOI] [PubMed] [Google Scholar]
- 11. Jin Y, Chen H, Xu X, Hu Y, Wang C, Ma Z. Traumatic proliferative vitreoretinopathy: clinical and histopathological observations. Retina. 2017;37(7):1236-1245. [DOI] [PubMed] [Google Scholar]
- 12. Matthews GP, Das A, Brown S. Visual outcome and ocular survival in patients with retinal detachments secondary to open- or closed-globe injuries. Ophthalmic Surg Lasers. 1998;29:48-54. [PubMed] [Google Scholar]
- 13. Dulz S, Dimopoulos V, Katz T, et al. Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury. Int J Ophthalmol. 2021;14(10):1589-1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eagling EM. Ocular damage after blunt trauma to the eye. Its relationship to the nature of the injury. Br J Ophthalmol. 1974;58(2):126-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sarrafizadeh R, Hassan TS, Ruby AJ, et al. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundus-obscuring vitreous hemorrhage. Ophthalmology. 2001;108(12):2273-2278. [DOI] [PubMed] [Google Scholar]
- 16. Tan HS, Mura M, Bijl HM. Early vitrectomy for vitreous hemorrhage associated with retinal tears. Am J Ophthalmol. 2010;150(4):529-533. [DOI] [PubMed] [Google Scholar]
- 17. Liu Y, Wang S, Li Y, Gong Q, Su G, Zhao J. Intraocular foreign bodies: clinical characteristics and prognostic factors influencing visual outcome and globe survival in 373 eyes. J Ophthalmol. 2019;2019:5208092. doi: 10.1155/2019/5208092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163-165. [DOI] [PubMed] [Google Scholar]
- 19. Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models—the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond). 2010;24(1):84-89. [DOI] [PubMed] [Google Scholar]
- 20. Idrees S, Sridhar J, Kuriyan AE. Proliferative vitreoretinopathy: a review. Int Ophthalmol Clin. 2019;59(1):221-240. [DOI] [PMC free article] [PubMed] [Google Scholar]


