Abstract
How do referral networks and medical conditions determine where patients get care? We study this question in the US Hospice Industry, where for-profit hospice programs enroll more long-term care patients and more patients with Alzheimer’s disease and related dementia. We find that for-profit hospice enrollees have 23% longer lifetime lengths-of-stay in hospice care than not for-profit hospice enrollees with the same medical conditions, institutional referral source, county of residence, and enrollment year. This and other differences in their end-of-life health care utilization suggest that hospice market segmentation is the result of a patient-specific selection mechanism that is partially independent of institutional barriers to hospice care.
Keywords: market segmentation, hospice, referral networks, Alzheimer's disease and related dementia
Are referral networks and patients' medical conditions enough to explain differences between for-profit and not for-profit hospices?
Introduction
Hospice is a large and growing segment of the US health care system that has been increasingly moving toward a for-profit business model. In 2022, nearly half of Medicare decedents received hospice care from one of the 5899 Medicare-certified hospice programs (up from 4639 in 2010).1 Growth in the number of hospice programs has been almost entirely driven by growth in the number of for-profit hospice programs, which increased from 3234 in 2010 to 4414 in 2022.1 Among these for-profit hospice programs are a large group of publicly traded national chains and private equity firms.2,3
Differences in hospice programs' business models are plausibly linked to differences in their enrollees' utilization of hospice care. For instance, for-profit hospice enrollees are more likely to have longer lifetime lengths-of-stay in hospice care (LLOS), less likely to have very short stays in hospice care, and are more likely to experience a live discharge.4-6 Since Medicare pays a flat rate for each patient-day and hospice programs' resource costs are highest during a patient's first few days in hospice care and last few days of life, hospice programs that enroll patients with longer average LLOS can earn higher average revenue (up to a regulated cap) and higher average profit.7-10 (Since 2016, Medicare has paid hospice programs ∼27% more per patient-day during a patient's first 60 days in hospice care. See CMS-1629-F: “FY 2016 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements.”)
However, the mechanisms underlying these differences are not yet well understood. Existing research shows that for-profit hospice enrollees are more likely to have stayed at a long-term care (LTC) facility shortly before their hospice enrollment, a large share of hospice enrollees from LTC facilities have Alzheimer's disease and related dementia (ADRD), and individuals with ADRD have longer LLOS.11-14 Together, these studies suggest that for-profit hospice programs achieve a higher average LLOS by selectively enrolling patients with ADRD from LTC facilities. But does that explain all of the differences between for-profit and not for-profit hospices enrollees?
Our objective is to empirically measure the extent to which patient characteristics and referral networks explain differential hospice utilization patterns between for-profit and not for-profit hospice programs. We find that after controlling for the interaction between hospice enrollees' referral sources and medical conditions, significant differences between for-profit and not for-profit hospice enrollees remain, including a 23% longer LLOS on average and an 1.1% point smaller likelihood of dying during a hospital stay.
Study data and methods
Analytical sample
Our primary data are the 100% sample of Medicare hospice claims spanning 2000–2019. We extract patient identification numbers, claim start and end dates, and hospice program identification numbers associated with each claim. We use these data to construct a patient-level dataset of Medicare beneficiaries who began hospice care between 2001 and 2018 (N = 15 832 781). (Specifically, although we use claims spanning 2000–2019, we restrict our sample to those Medicare beneficiaries who were first observed to enrolling hospice care between 2001 and 2018. We use the 2000 and 2019 claims to reduce left- and right-censoring in our measures of hospice enrollees' lifetime hospice utilization.)
We identify referrals from hospitals and nursing homes (NHs) using records of hospital and skilled nursing facility (SNF) stays in the Medicare Provider Analysis and Review files (MedPAR) and other NH stays in the minimum dataset (MDS). In particular, we define a referral from an institution if we observe that a hospice enrollee had a hospital or NH stay in MedPAR or the MDS in the week prior to their hospice enrollment date (N = 7 631 569). This excludes patients who are observed to have had such stays at multiple distinct hospitals or NHs (N = 1 591 679) or who were associated with multiple hospice programs on their first observed day in hospice care (N = 531). (For instance, we exclude Medicare beneficiaries who are observed to have had stays at two distinct hospitals, two distinct NHs, or both a hospital and a NH, in the week prior to their hospice enrollment. This restriction ensures our sample is “clean” in the sense that we can link hospice enrollments to one specific institutional referral source in the week prior to their hospice enrollment.) We define all remaining patients without a recent institutional stay as having a referral from “the community” (N = 6 609 002).
We link the patient and provider records in the hospice claims, MedPAR, and MDS to secondary data. First, we identify hospice programs' business model (for-profit or not for-profit), state of business, and opening year using the provider-of-service files. Second, we identify hospice enrollees' age, race, Medicare advantage (MA) enrollment, sex, death date (if any), and county of residence using the Medicare beneficiary summary file. Third, we identify hospice enrollees' medical conditions using the diagnosis codes on their first hospice claims. For hospice enrollees who had a hospital or SNF stay in MedPAR in the week prior to their hospice enrollment, we also identify their medical conditions using the diagnosis codes on their hospital or SNF claims.
We construct the primary outcome variables as follows. We define each hospice enrollee's LLOS as their total number of days in hospice care between 2001 and 2019. We likewise define each patient's lifetime number of hospice programs, lifetime number of live discharges, and length-of-stay during their first hospice spell (LOS). (A patient's first hospice spell is the first period of days that they are observed to be continuously enrolled with one hospice program. It ends when a patient dies, experiences a 1+ day break from hospice care, or is observed to be treated at a new hospice.) We say that a hospice enrollee died in hospice care, during a hospital stay, or during a NH stay if they had a record of a hospice enrollment, hospital stay, or NH stay on their date of death. We say that a hospice enrollee is a decedent if their date of death is between 2001 and 2019. We define each decedent's remaining days of life (RDOL) as the number of days between their hospice enrollment date and their date of death.15-17 We measure the fraction of each decedent's RDOL in a hospital or NH using the records of their hospital, SNF, or NH stays in MedPAR and the MDS. We measure the rurality of each patient's county using data published by the US Census Bureau, and we compute a Hirfindahl–Hirschman Index (HHI) between hospices operating in each patient's county. We report additional details about sample construction and data cleaning in the online Supplementary material.
Methods
First, we measured unadjusted and regression-adjusted differences between for-profit and not for-profit hospice enrollees' outcomes. In particular, we used a sequence of regressions saturated with patient-level fixed effects to account for variation attributable to their pre-hospice characteristics. For each outcome, we first used no fixed effects; then we added enrollment year, county of residence, sex, race, MA enrollment, and hospice opening year fixed effects; then, we added institutional referral source fixed effects; and then, we added medical condition fixed effects. The county fixed effects enable us to control for geographic characteristics, including local market characteristics (such as competition) and rurality. The referral source fixed effects are at the entity level; there is one fixed effect for each individual referring hospital and NH in our sample. All fixed effects are fully interacted with one another and with a continuous measure of patient age. The coefficient of interest is an indicator variable equal to 1 for for-profit hospice enrollees and 0 otherwise.
Second, we measured referral networks by calculating the fraction of each program's annual enrollees who were referred from hospitals, NHs, or the community, and the number of hospitals and NHs where they got any referrals. We measured unadjusted and regression-adjusted differences between for-profit and not for-profit hospice programs' referral networks. In the regression specifications, we included fully interacted state of business, year, and age fixed effects. (We control for states rather than counties in the hospice-level models because some hospices operate outside the county where their main business address is located.) The coefficient of interest is an indicator variable equal to 1 for for-profit hospice programs and 0 otherwise.
In both analyses, for outcomes that are indicator variables or measured in percentages, we used ordinary least squares (OLS) estimators and interpreted the coefficient of interest as the percentage point change in the outcome associated with for-profit hospice relative to not for-profit hospice. For outcomes that are other non-negative continuous variables, we used Poisson pseudo-maximum likelihood estimators (PPML) and interpreted the coefficient of interest as the percent change in the outcome associated with for-profit hospice relative to not for-profit hospice.18 In the referral network analysis, we adjusted standard errors for one-way clustering in hospice programs. In the enrollee-level analysis, we adjusted standard errors for two-way clustering in hospice programs and referral sources, and we excluded all hospice enrollees who were not observed to have an institutional referral source (N = 6 609 002). For each outcome, we fixed the estimation sample to be the same across specifications to enable making comparisons across specifications. See the online Supplementary material for additional details about the regression analysis.19 (For each outcome, the estimation sample excludes observations with missing values, singletons, and observations separated by a fixed effect in the specification with the richest set of fixed effects.)
We conducted several sensitivity analyses. First, we assessed whether our results were sensitive using quarter fixed effects instead of year fixed effects. If for-profit and not for-profit hospice programs systematically enroll patients at different times of the year, then some of the differences between their enrollees' hospice utilization may be attributable to seasonality. Second, we assessed whether our results were sensitive to measuring hospice enrollees' medical conditions using the diagnosis codes on their hospice claims. If for-profit and not for-profit hospice programs systematically report diagnosis codes differently for otherwise identical patients, then controlling for diagnosis codes may introduce measurement error in the regression analysis. In other contexts, research suggests that patients' diagnosis codes may be upcoded by providers to raise risk-adjusted payment rates.20 Concerns about upcoding in hospice are lessened because hospice programs' payment rates do not vary with their patient mix. Nevertheless, we conducted this sensitivity analysis by restricting the estimation sample to patients who had a referral from a hospital or SNF and measuring their medical conditions using the diagnosis codes reported in their MedPAR claims instead. Third, we assessed whether our results were sensitive to the sample period by restricting the estimation sample to patients who enrolled in hospice during 2011–2018. Fourth, we assessed whether our results were sensitive to excluding hospice opening year fixed effects. (We obtained IRB approval for this study through the University of Pennsylvania, protocol #831952.)
Limitations
This research has several limitations. First, we do not directly observe referrals to hospice programs in our claims data. The “referral sources” and “referral networks” we discuss are proxies generated by observing hospital and NH stays shortly before hospice enrollment. When a Medicare beneficiary first enrolls in hospice care, a non-hospice physician—such as their hospital or NH attending physician—must certify that their life expectancy is 6 months or less (42 CFR 418.22). Therefore, we think that such connections between hospice enrollment and a recent prior hospital or NH stay are plausible. And while we identify institutional referral sources where hospice enrollees stayed immediately before their hospice enrollment, it is possible that other providers were primarily responsible for coordinating their transition to hospice care. Second, we do not measure non-hospital and non-NH referral networks. Table S1 suggests that hospice enrollees who are referred from the community have higher LLOS than do patients who enroll after a hospital or NH stay. Third, there are no measures of hospice capacity in claims data to understand any potential differences in for-profit and not for-profit hospices' abilities to meet patient needs.
Study results
Referral networks
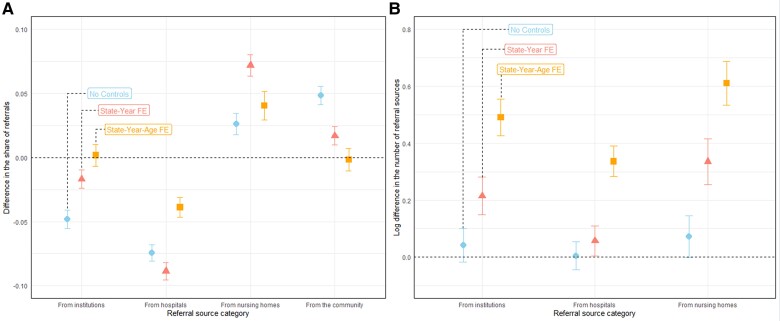
Figure 1 plots regression-adjusted differences between for-profit and not for-profit hospice programs' referral networks. It shows that for-profit hospice programs enrolled a larger share of patients from NHs and a smaller share of patients from hospitals. It also shows that they enrolled patients from a larger number of hospitals and NHs. These findings support the idea that for-profit hospice programs' institutional referral networks are larger and favor LTC facilities.
Figure 1.
Distribution of referral sources to for-profit vs not for-profit hospice programs (2000-2019). This figure plots estimates from our regression analysis. Panel (A) shows that the share of referrals from hospitals is lower at for-profit hospice programs than at not for-profit hospice programs; but the share of referrals from NHs is higher. Panel (B) shows that for-profit hospice programs have more institutional referral sources (including more hospitals and more NHs) than not for-profit hospice programs. Bars represent 95% CI that account for hospice-level cluster-robust standard errors (SEs). Source: authors' analysis of Medicare data.
Hospice enrollment
Table 1 describes the sample of ∼14 million hospice enrollees. Forty percent of them were for-profit hospice enrollees. They were 57% female, 88% White, and 82 years old at hospice enrollment, on average. Fifty-four percent of them were referred to hospice care from an institutional referral source, which was a NH for 37% of such patients (ie, for 20% of the sample). Thirty-six percent of hospice enrollees had a cancer diagnosis on their first hospice claim, 19% had an ADRD diagnosis, and 12% had a chronic obstructive pulmonary disease (COPD) diagnosis. On average, their LLOS was 95 days, and they experienced 0.23 live discharges. Among decedents, their RDOL was 138 days, they spent 7% of their RDOL in a hospital, and they spent 18% of their RDOL in a NH. (LLOS and RDOL are highly right-skewed. Among decedents, the median LLOS and RDOL are 20 days.)
Table 1.
Characteristics of sample by for-profit hospice enrollment status (2000-2019).
| Profit status | |||||
|---|---|---|---|---|---|
| All | For | Not | Δ | P-value | |
| (1) | (2) | (3) | (4) | (5) | |
| Demographic, biographic, and geographic characteristics | |||||
| Female (%) | 0.57 | 0.58 | 0.56 | 0.02 | 0.00 |
| White (%) | 0.88 | 0.85 | 0.90 | −0.05 | 0.00 |
| Black (%) | 0.08 | 0.10 | 0.07 | 0.03 | 0.00 |
| Asian (%) | 0.01 | 0.01 | 0.01 | 0.00 | 0.04 |
| Hispanic (%) | 0.02 | 0.03 | 0.01 | 0.01 | 0.00 |
| Nat. Am. (%) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| MA enrollee (%) | 0.26 | 0.28 | 0.25 | 0.03 | 0.00 |
| Age at enrollment | 81.59 | 81.94 | 81.36 | 0.58 | 0.00 |
| Decedent (%) | 0.98 | 0.97 | 0.99 | −0.02 | 0.00 |
| RDOL (#) | 138 | 175 | 113 | 62 | 0.00 |
| Age at death | 82.01 | 82.50 | 81.68 | 0.82 | 0.00 |
| County HHI | 2875 | 2069 | 3421 | −1351 | 0.00 |
| County rural (%) | 0.21 | 0.21 | 0.22 | −0.01 | 0.21 |
| Medical conditions | |||||
| ADRD (%) | 0.19 | 0.22 | 0.17 | 0.06 | 0.00 |
| Acute myocardial infarction (%) | 0.01 | 0.01 | 0.01 | −0.00 | 0.00 |
| Cancer (%) | 0.36 | 0.29 | 0.40 | −0.11 | 0.00 |
| Cerebrovascular disease (%) | 0.00 | 0.00 | 0.00 | −0.00 | 0.00 |
| Chronic kidney disease (%) | 0.03 | 0.02 | 0.03 | −0.00 | 0.00 |
| COPD (%) | 0.12 | 0.11 | 0.12 | −0.00 | 0.42 |
| Coronary artery disease (%) | 0.08 | 0.07 | 0.08 | −0.01 | 0.10 |
| Diabetes (%) | 0.06 | 0.06 | 0.07 | −0.01 | 0.01 |
| End-stage renal disease (%) | 0.02 | 0.02 | 0.02 | −0.00 | 0.30 |
| Flu (%) | 0.00 | 0.00 | 0.00 | −0.00 | 0.00 |
| Heart failure (%) | 0.14 | 0.14 | 0.14 | −0.00 | 0.82 |
| Pneumonia (%) | 0.02 | 0.02 | 0.03 | −0.01 | 0.00 |
| Septicemia (%) | 0.02 | 0.01 | 0.02 | −0.01 | 0.01 |
| Institutional referral characteristics | |||||
| Institutional referral (%) | 0.54 | 0.53 | 0.54 | −0.02 | 0.00 |
| NH referral (%) | 0.37 | 0.46 | 0.31 | 0.15 | 0.00 |
| Hospital referral (%) | 0.63 | 0.54 | 0.69 | 0.85 | 0.00 |
| Hospice program characteristics | |||||
| For profit (%) | 0.40 | 1.00 | 0.00 | 1.00 | 0.00 |
| Hospice start year | 1994 | 1999 | 1990 | 10 | 0.00 |
| Lifetime hospice utilization | |||||
| Enrollment year | 2011 | 2011 | 2010 | 1 | 0.00 |
| LLOS (#) | 95 | 121 | 77 | 44 | 0.00 |
| First spell LOS (#) | 78 | 96 | 66 | 31 | 0.00 |
| Hospices (#) | 1.06 | 1.10 | 1.04 | 0.06 | 0.00 |
| Live discharges (#) | 0.23 | 0.30 | 0.18 | 0.11 | 0.00 |
| Died in 6 mos. (%) | 0.81 | 0.76 | 0.85 | −0.09 | 0.00 |
| Decedents' healthcare utilization at end-of-life | |||||
| RDOL in hospital (%) | 0.07 | 0.06 | 0.08 | −0.02 | 0.05 |
| RDOL in NH (%) | 0.18 | 0.22 | 0.15 | 0.07 | 0.02 |
| Died in hospice (%) | 0.93 | 0.92 | 0.94 | −0.02 | 0.00 |
| Died in hospital (%) | 0.04 | 0.04 | 0.03 | 0.00 | 0.39 |
| Died in NH (%) | 0.19 | 0.23 | 0.16 | 0.07 | 0.01 |
| Died elsewhere (%) | 0.78 | 0.74 | 0.81 | −0.07 | 0.00 |
| N (millions) | 14.2 | 5.7 | 8.5 | — | — |
Abbreviations: ADRD, Alzheimer's disease and related dementia; LLOS, longer lifetime lengths-of-stay; LOS, length-of-stay; NH, nursing home; RDOL, remaining days of life.
This table describes the sample of hospice enrollees. Column (4) reports the average differences between for-profit and not for-profit enrollees. We conducted a two-sided test of the null Δ = 0 accounting for two-way clustering in hospice programs and referral sources. Column (5) reports the P-value of the t-statistic rounded to two digits. Source: authors' analysis of Medicare data.
Relative to not for-profit hospice enrollees, for-profit hospice enrollees had 44-day greater LLOS (121 vs 77) and they experienced 0.11 more live discharges (0.30 vs 0.18). Among decedents, their RDOL was 62 days greater (175 vs 113), they spent 2% points less of their RDOL in a hospital (6% vs 8%), and they spent 7% points more of their RDOL at a NH (22% vs 15%). They were ∼6% points more likely to have an ADRD diagnosis (22% vs 17%) and 11% points less likely to have a cancer diagnosis (29% vs 40%).
Table 2 reports how differences between for-profit and not for-profit hospice enrollees' LLOS change as we sequentially control for various pre-hospice characteristics. In column (1), it shows that for-profit hospice enrollees spend 0.466 log points (59%) more days in hospice care, on average. (Throughout the paper, we convert log point changes to percent changes using Percent = exp(Log) − 1.) In column (2), it shows that they spend 0.326 log point (39%) more days in hospice care, on average, after controlling for the year of their enrollment, their county of residence, their demographic information, their MA enrollment status, and the hospice program's age. In column (3), it shows that they spend 0.163 log point (18%) more days in hospice care, on average, after further controlling for their referral source. Finally, in column (4), it shows that they spend 0.210 log point (23%) more days in hospice care, on average, after further controlling for their medical conditions.
Table 2.
Regression-adjusted differences in LLOS between for-profit and not for-profit hospice enrollees (2000-2019).
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| LLOS | LLOS | LLOS | LLOS | |
| (#) | (#) | (#) | (#) | |
| Is for profit (1/0) | 0.466*** | 0.326*** | 0.163*** | 0.210*** |
| (0.026) | (0.043) | (0.058) | (0.057) | |
| Estimator | PPML | PPML | PPML | PPML |
| Coef. interpretation | Log Δ | Log Δ | Log Δ | Log Δ |
| Decedents only | N | N | N | N |
| Base FE | N | Y | N | N |
| Base × Referrer FE | N | N | Y | N |
| Base × Referrer × Med. FE | N | N | N | Y |
| Mean of Y | 62.702 | 62.702 | 62.702 | 62.702 |
| #[Hospice clusters] | 5005 | 5005 | 5005 | 5005 |
| #[Referrer clusters] | 21 141 | 21 141 | 21 141 | 21 141 |
| #[Effective observations] | 2 878 139 | 2 878 139 | 2 878 139 | 2 878 139 |
Abbreviation: LLOS, longer lifetime lengths-of-stay.
This table reports estimates from our regression analysis. It shows that for-profit hospice enrollees have longer LLOS than not for-profit hospice enrollees, even after accounting for a progressively richer set of pre-hospice characteristics. Referrer and hospice-level cluster-robust SEs in parentheses. *P < 0.10; **P < 0.05; ***P < 0.01. Base FE refers to enrollment year, county of residence, sex, race, MA enrollment, and hospice opening year fixed effects. Base × Referrer FE refers to adding institutional referral source fixed effect interactions. Base × Referrer × Med. FE refers to adding medical condition fixed effect interactions. Mean of Y reports the sample average value of the outcome. The effective number of observations is the number of observations remaining after dropping observations with missing values, singletons, and observations separated by a fixed effect.19 Source: authors' analysis of Medicare data.
Table S2 illustrates why these estimates change as we progressively add more fixed effect interactions. It shows that individuals who enroll in hospice care from NHs have longer LLOS on average (column [1]) and are more likely to enroll in for-profit hospice care (column [4]). Hence, the association between for-profit hospice enrollment and LLOS decreases from 0.326 to 0.163 log points in Table 2 after controlling for hospice enrollees’ referral sources. Table S2 also shows that after controlling for hospice enrollees’ referral sources, the associations between their medical conditions and their for-profit hospice enrollment decrease in magnitude (column [6]). Hence, the association between for-profit hospice enrollment and LLOS changes comparatively little in Table 2 after controlling for hospice enrollees’ medical conditions.
Table 3 reports other regression-adjusted differences between for-profit and not for-profit hospice enrollees' outcomes. For brevity, it only reports results from the specifications with the richest set of fixed effects. It shows that for-profit hospice enrollees experience 0.189 log point (21%) longer LOS in hospice care during their first hospice spell, 0.052 log point (5.3%) more live discharges, enroll with 0.009 log point (1%) more unique hospice programs, and are 1.9% points less likely to die within 6 months of their hospice enrollment than not for-profit hospice enrollees. Among decedents, for-profit hospice enrollees have 0.235 log point (26%) higher RDOL than not for-profit hospice enrollees. The share of their RDOL spent in a hospital is 1.2% points lower and they are 1.1% points less likely to die in a hospital. Likewise, the share of their RDOL spent in a NH is 0.4% points higher and they are 0.5% points more likely to die in a NH. They are 0.6% points more likely to die in hospice care.
Table 3.
Regression-adjusted differences in other outcomes between for-profit and not for-profit hospice enrollees (2000–2019).
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| LOS in | Live | Died in | ||||
| LLOS | first spell | discharges | Programs | 6 mos.? | RDOL | |
| (#) | (#) | (#) | (#) | (1/0) | (#) | |
| Is for profit (1/0) | 0.210*** | 0.189*** | 0.052 | 0.009* | −0.019*** | 0.235*** |
| (0.057) | (0.053) | (0.085) | (0.005) | (0.007) | (0.067) | |
| Estimator | PPML | PPML | PPML | PPML | OLS | PPML |
| Coef. interpretation | Log Δ | Log Δ | Log Δ | Log Δ | %point Δ | Log Δ |
| Decedents only | N | N | N | N | N | Y |
| Base FE | N | N | N | N | N | N |
| Base × Referrer FE | N | N | N | N | N | N |
| Base × Referrer × Med. FE | Y | Y | Y | Y | Y | Y |
| Mean of Y | 62.702 | 53.888 | 0.324 | 1.030 | 0.883 | 94.475 |
| #[Hospice clusters] | 5005 | 5005 | 4701 | 5005 | 5005 | 4951 |
| #[Referrer clusters] | 21 141 | 21 141 | 17 824 | 21 141 | 21 137 | 21 083 |
| #[Effective observations] | 2 878 139 | 2 878 139 | 1 255 318 | 2 878 139 | 2 875 870 | 2 848 918 |
| (7) | (6) | (7) | (8) | (9) | (10) | |
| Died in | RDOL in | RDOL in | Place of death | |||
| Hospice? | Hospitals | NHs | Hospital? | NH? | Elsewhere? | |
| (1/0) | (%) | (%) | (1/0) | (1/0) | (1/0) | |
| Is for profit (1/0) | 0.000 | −0.012 | 0.004 | −0.011** | 0.005 | 0.006 |
| (0.004) | (0.007) | (0.003) | (0.005) | (0.004) | (0.006) | |
| Estimator | OLS | OLS | OLS | OLS | OLS | OLS |
| Coef. interpretation | %point Δ | %point Δ | %point Δ | %point Δ | %point Δ | %point Δ |
| Decedents only | Y | Y | Y | Y | Y | Y |
| Base FE | N | N | N | N | N | N |
| Base × Referrer FE | N | N | N | N | N | N |
| Base × Referrer × Med. FE | Y | Y | Y | Y | Y | Y |
| Mean of Y | 0.948 | 0.146 | 0.229 | 0.052 | 0.227 | 0.722 |
| #[Hospice clusters] | 4951 | 4950 | 4949 | 4951 | 4951 | 4951 |
| #[Referrer clusters] | 21 087 | 21 083 | 21 052 | 21 087 | 21 087 | 21 087 |
| #[Effective observations] | 2 853 677 | 2 851 043 | 2 838 699 | 2 853 677 | 2 853 677 | 2 853 677 |
Abbreviations: NH, nursing home; OLS, ordinary least squares; RDOL, remaining days of life.
This table reports estimates from our regression analysis. It shows that for-profit hospice enrollees' patterns of hospice utilization differ from those of not for-profit hospice enrollees, even after accounting for a rich set of pre-hospice characteristics. Referrer and hospice-level cluster-robust SEs in parentheses. *P < 0.10; **P < 0.05; ***P < 0.01. Base FE refers to enrollment year, county of residence, sex, race, MA enrollment, and hospice opening year fixed effects. Base × Referrer FE refers to adding institutional referral source fixed effect interactions. Base × Referrer × Med. FE refers to adding medical condition fixed effect interactions. Mean of Y reports the sample average value of the outcome. The effective number of observations is the number of observations remaining after dropping observations with missing values, singletons, and observations separated by a fixed effect. Source: authors' analysis of Medicare data.
Sensitivity analysis
First, we assessed whether our results are sensitive to using quarter instead of year fixed effects. Table S3 presents our results. They are qualitatively similar to our main results, suggesting a small role for seasonality.
Second, we assessed whether our results are sensitive to using diagnosis codes reported on hospital or SNF claims in MedPAR instead of those on hospice claims. Table S4 presents our results. However, comparing Table S4 to our main results is complicated by the fact that the sample underlying Table S4 excludes hospice enrollees without a recent prior hospital or SNF stay. Therefore, differences between Table S4 and our main results may be driven by differences in the estimation samples (rather than differences in the diagnosis codes). We re-estimated our main regressions using only the sample of hospice enrollees with a recent prior hospital or SNF stay in MedPAR. Table S5 presents the results. They are qualitatively similar to the results in Table S4.
Third, we assessed whether our results are sensitive to the sample period by restricting the estimation sample to patients who enrolled in hospice during 2011-2018. Table S6 presents the results. They are qualitatively similar to our main results, suggesting that adjusted differences between for-profit and not for-profit hospice enrollees' patterns of hospice utilization were similar between 2001-2010 and 2011-2018.
Fourth, we assessed whether our results are sensitive to excluding hospice opening year fixed effects. Table S7 presents the results. These results indicate more substantial differences between for-profit and not for-profit hospice enrollees' patterns of hospice utilization. However, since not for-profit hospice programs are older on average than for-profit hospice programs, part of these differences are attributable to age rather than profit status. Our main estimates therefore control for hospice opening year fixed effects.
Discussion
We find that for-profit hospice enrollees have different patterns of hospice utilization than not for-profit hospice enrollees—even after accounting for the interaction between their institutional referral sources and medical conditions. In theory, these differences may be attributable to the causal effects of for profit vs not for-profit hospice care on patient outcomes—eg, quality of care—or patient selection. However, Gruber et al.9 find little evidence that for-profit hospice programs differentially affect 5-year mortality rates among ADRD patients relative to not for-profit hospice programs. Since the purpose of hospice care is to replace curative care with palliative care at the end of life, we hypothesize that these differences are largely attributable to selection on characteristics unobservable in claims data that predict LLOS—and, therefore, profitability. This has implications in several domains.
First, our findings suggest that market segmentation in the US hospice industry operates through a complex selection process. Part of this process separates patients based on their pre-hospice care providers and medical conditions. For instance, we affirm existing evidence that for-profit hospice enrollees are more likely to have had recent NH stays and are less likely to have a cancer diagnosis than an ADRD diagnosis. But we also find evidence that this process separates patients with the same referral sources and medical conditions between for-profit and not for-profit hospice programs; and it does so in ways that predict significant differences in their subsequent hospice utilization.
It is critical to learn more about the determinants of the patient–hospice match. Market segmentation can facilitate price or quality discrimination and market concentration by shrinking consumers' choice sets to only those firms that serve their market segment.21,22 But, it can also raise treatment quality in health care markets where providers' production functions have increasing returns to specialization.23 Profit motives have been linked to market segmentation in health insurance markets, hospitals, and NHs.24-27 In the US hospice industry, Dalton and Bradford14 find that the coexistence of for-profit and not for-profit hospice programs extends access to hospice care to a wider range of potential enrollees. But further research is needed to measure the extent and effects of market segmentation in hospice.
Second, our findings suggest that patient-specific barriers to hospice care are an important determinant of the timing of hospice enrollment. Studies have shown that hospice care is associated with lower costs, higher quality of care, and fewer unmet needs and hospitalizations at the end of life.9,17,28 They also suggest that barriers to timely enrollment in hospice care—such as non-hospice providers' “difficulty with prognosis” or patients' “lack of knowledge about hospice” and “denial of their terminal diagnosis”—may lower quality-of-life and raise health care costs.29
We find that for-profit hospice enrollees have longer LLOS and RDOL than not for-profit hospice enrollees with recent stays at the same hospitals and NHs. This supports the idea that barriers to hospice care differ across patients treated by the same pre-hospice provider, and that for-profit hospice programs overcome these barriers sooner or identify patients for whom they are relatively small. While our findings support the idea that reducing barriers to timely enrollment in hospice care at the pre-hospice provider-level may be effective, they also suggest that other barriers to hospice care may be comparably important.
Conclusion
We examined differences between for-profit and not for-profit hospice enrollees. Consistent with prior research, we find that for-profit hospice enrollees have 59% longer LLOS on average than not for-profit hospice enrollees. We also find that for-profit hospice programs enroll a larger share of patients from LTC facilities and a smaller share of patients from hospitals. However, we find that after controlling for hospice enrollees' institutional referral sources and medical conditions, significant differences between for-profit and not for-profit hospice enrollees remain, including a 23% longer LLOS on average and a 1.1% point smaller likelihood of dying during a hospital stay. A granular assessment of the mechanisms underlying these differences—such as the role of discharge planning and hospice care consultations—may be a fruitful area for future research.
Supplementary Material
Contributor Information
David A Rosenkranz, Department of Economics, Fordham University, 441 E Fordham Road, Dealy Hall, Bronx, NY 10458, United States.
Lindsay White, Department of Medical Ethics and Health Policy, University of Pennsylvania, 423 Guardian Drive, Blockley Hall, Philadelphia, PA 19104, United States.
Chuxuan Sun, Department of General Internal Medicine, University of Pennsylvania, 423 Guardian Drive, Blockley Hall, Philadelphia, PA 19104, United States.
Katherine E M Miller, Department of Health Policy and Management, Johns Hopkins University, 1812 Ashland Ave., Baltimore, MD 21205, United States.
Norma B Coe, Department of Medical Ethics and Health Policy, University of Pennsylvania, 423 Guardian Drive, Blockley Hall, Philadelphia, PA 19104, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Funding
This research was supported by the National Institute on Aging (grant no. R01AG062595).
Notes
- 1. Medicare Payment Advisory Commission . Report to Congress. Washington, DC; 2024. [Google Scholar]
- 2. Braun RT, Stevenson DG, Unruh MA. Acquisitions of hospice agencies by private equity firms and publicly traded corporations. JAMA Intern Med. 2021;181(8):1113–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stevenson DG, Dalton JB, Grabowski DC, Huskamp HA. Nearly half of all Medicare hospice enrollees received care from agencies owned by regional or national chains. Health Aff (Millwood). 2015;34(1):30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stevenson DG, Grabowski DC, Keating NL, Huskamp HA. Effect of ownership on hospice service use: 2005–2011. J Am Geriatr Soc. 2016;64(5):1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aldridge MD, Schlesinger M, Barry CL, et al. National hospice survey results: for-profit status, community engagement, and service. JAMA Intern Med. 2014;174(4):500–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wachterman MW, Marcantonio ER, Davis RB, McCarthy EP. Association of hospice agency profit status with patient diagnosis, location of care, and length of stay. JAMA. 2011;305(5):472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bogasky S, Sheingold S, Stearns SC. Medicare's hospice benefit: analysis of utilization and resource use. Medicare Medicaid Res Rev. 2014;4(2):E1–E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coe NB, Rosenkranz DA. Provider payment incentives: evidence from the U.S. hospice industry. 2024; NBER Working Paper 31691.
- 9. Gruber J, Howard DH, Leder-Luis J, Caputi TL. Dying or lying? For-profit hospices and end of life care. 2023; NBER Working Paper 31035.
- 10. Lindrooth RC, Weisbrod BA. Do religious nonprofit and for-profit organizations respond differently to financial incentives? The hospice industry. J Health Econ. 2007;26(2):342–357. [DOI] [PubMed] [Google Scholar]
- 11. Gandhi SO. Differences between non-profit and for-profit hospices: patient selection and quality. Int J Health Care Finance Econ. 2012;12(2):107–127. [DOI] [PubMed] [Google Scholar]
- 12. Furuno JP, Noble BN, McPherson ML, et al. Variation in hospice patient and admission characteristics by referral location. Med Care. 2020;58(12):1069–1074. [DOI] [PubMed] [Google Scholar]
- 13. Gaugler JE, Yu F, Davila HW, Shippee T. Alzheimer's disease and nursing homes. Health Aff. 2014;33(4):650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dalton CM, Bradford WD. Better together: coexistence of for-profit and nonprofit firms with an application to the U.S. hospice industry. J Health Econ. 2019;63:1–18. [DOI] [PubMed] [Google Scholar]
- 15. Luth E, Russell D, Cici J, et al. Survival in hospice patients with dementia: the effect of home hospice and nurse visits. J Am Geriatr Soc. 2021;69(6):1529–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris P, Stalam T, Ache K, et al. Can hospices predict which patients will die within six months? J Palliat Med. 2014;17(8):894–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff. 2013;32(3):552–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wooldridge JM. Distribution-free estimation of some nonlinear panel data models. J Econom. 1999;90(1):77–97. [Google Scholar]
- 19. Correia S. Linear Models With High-Dimensional Fixed Effects: An Efficient and Feasible Estimator. 2017. http://scorreia.com/research/hdfe.pdf[See also: Correia S, Guimaraes P, Zylkin T. ‘ppmlhdfe: fast Poisson estimation with high-dimensional fixed effects.’ arXiv: 1903.01690. preprint: not peer reviewed]Accessed October 2022.
- 20. Geruso M, Layton T. Upcoding: evidence from Medicare on squishy risk adjustment. J Public Econ. 2020;128(3):984–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Atal JP, Cuesta JI, Gonzalez F, Otero C. The economics of the public option: evidence from local pharmaceutical markets. Am Econ Rev. 2024;114(3):615–644. [Google Scholar]
- 22. Dickstein MJ, Ho K, Mark N. Market segmentation and competition in health insurance. J Polit Econ. 2023;132(1):96–148. [Google Scholar]
- 23. Gaynor M, Seider H, Vogt WB. The volume-outcome effect, scale economies, and learning-by-doing. AEA Pap Proc. 2005;95(2):243–247. [Google Scholar]
- 24. Lavetti K, Simon K. Strategic formulary design in Medicare part D plans. Am Econ J Econ Policy. 2018;10(3):154–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Park S, Basu A, Coe NB, Khalil F. Service-level selection: strategic risk selection in Medicare Advantage in response to risk adjustment. 2017; NBER Working Paper 24038.
- 26. Alexander D. How do doctors respond to incentives? Unintended consequences of paying doctors to reduce costs. J Polit Econ. 2020;128(11):4046–4096. Federal Reserve Bank of Chicago WP 2017-09. [Google Scholar]
- 27. Gandhi A. Picking your patients: selective admissions in the nursing home industry. 2023. 10.2139/ssrn.3613950 [DOI]
- 28. Teno JM, Gozalo PL, Lee IC, et al. Does hospice improve quality of care for persons dying from dementia? J Am Geriatr Soc. 2011;59(8):1531–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jenkins TM, Chapman KL, Ritchie CS, et al. Barriers to hospice care in Alabama: provider-based perceptions. Am J Hosp Palliat Care. 2011;28(3):153–160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.