Abstract
Objectives
This study aims to evaluate the quantity, types, and trends of surgical procedures used to treat obstructive sleep apnea (OSA) within a diverse national population, utilizing a comprehensive proprietary healthcare database.
Methods
This descriptive observational study analyzed longitudinal data from the Optum Clinformatics® Data Mart databases, covering the period from January 2004 to December 2020. The study included patients aged 18 to 89 years, both male and female, with a confirmed diagnosis of OSA. These patients were either treated with continuous positive airway pressure (CPAP) or underwent surgical interventions.
Results
Throughout the study period, 1,250,273 individuals were diagnosed with OSA. The average age at diagnosis was 62 years (SD = 16), with a male predominance of 62.3%, and 75% of the patients were identified as Caucasian. The most frequently performed surgical procedure for OSA was Uvulopalatopharyngoplasty (UPPP). However, the implantable hypoglossal nerve stimulator was more commonly utilized among older patients.
Conclusions
This study provides essential insights into the prevalence and characteristics of surgical procedures used in OSA treatment across a diverse national population. The findings underscore the significance of understanding surgical intervention patterns and trends to enhance patient care and outcomes.
Keywords: Obstructive sleep apnea, Airway obstruction, Airway management
Introduction
Obstructive sleep apnea (OSA) is characterized by the repetitive obstruction of the upper airway during sleep, often due to the relaxation of upper airway muscles or a structural imbalance between the airway and surrounding skeletal components [1].
Estimates indicate that OSA affects roughly 25–30% of adults in the United States, reflecting its prevalence across the population [2, 3]. Among obese individuals, the incidence is even more pronounced, surpassing 50% [4–12]. OSA is associated with an elevated risk of cardiovascular morbidity and mortality. The primary treatment for OSA remains continuous positive airway pressure (CPAP), although its effectiveness and patient adherence vary; many individuals cease using CPAP within the first year [13, 14]. Surgical interventions are available as an alternative to CPAP, either as a long-term solution or as a means to enhance CPAP efficacy [15–17]. Surgical options range from ENT procedures, such as uvulopalatopharyngoplasty, expansion sphincter pharyngoplasty, barbed pharyngoplasty, genioglossus advancement, hyoid myotomy, to radiofrequency tongue base reduction. In more severe cases, oral and maxillofacial surgeries, including maxillomandibular advancement, have shown excellent outcomes [15, 16].
Despite the growing variety of surgical approaches for OSA, there remains a limited understanding of the patterns of surgical care and patient demographics in this field [18, 19]. Moreover, social determinants significantly affect a patient's medical journey, with some minority groups experiencing lower-quality care and facing higher rates of morbidity and mortality [20–22]. Racial, ethnic, and socioeconomic disparities can impact access to OSA treatments. It is therefore vital to deepen our understanding of current surgical practices and identify the obstacles contributing to these disparities [23–26].
This study aims to analyze a comprehensive healthcare database to evaluate the quantity, types, and distribution patterns of therapeutic procedures for OSA across different social groups on a national scale, considering parameters such as BMI, OSA severity, and surgical treatment modalities.
Methods
Study design
This study is a descriptive observational analysis that involved adults diagnosed with OSA who underwent surgical treatment. Data for this analysis was sourced from the Optum Clinformatics® Data Mart Database (Optum), covering the period from January 2004 to December 2020. This database includes de-identified information from a vast claims data warehouse.
Inclusion criteria were as follows: 1) Patients aged 18 years and above up to 89 years; 2) Individuals diagnosed with OSA, identified using specific ICD-9 and ICD-10 codes. 3) Patients with records of CPAP prescriptions were included to ensure selection of individuals with confirmed OSA. Surgical therapies were identified based on Current Procedural Terminology (CPT) codes corresponding to different procedures. Patients without gender definition were excluded.
Since this study utilized only de-identified data and commercially available information, it did not require institutional review at Stanford University School of Medicine, where the statistical analysis was conducted. The database is not publicly accessible; thus, IRB exemption was applicable under 45 CFR § 46.104(d)(4)(ii).
Study population
The study aimed to assess the quantity, types, and distribution patterns of therapeutic procedures for OSA across various social groups on a national level, considering factors such as BMI, OSA severity, and surgical treatment modalities.
The surgical interventions evaluated in the study included palatal procedures, tonsillectomy, tongue base procedures, genioglossus advancement, lingual tonsillectomy, skeletal surgeries (such as maxillomandibular advancement), and hypoglossal nerve stimulation.
Gender and ethnicity data were extracted from the Optum database, which utilizes self-identifying information based on classifications from the United States Census Bureau.
Results
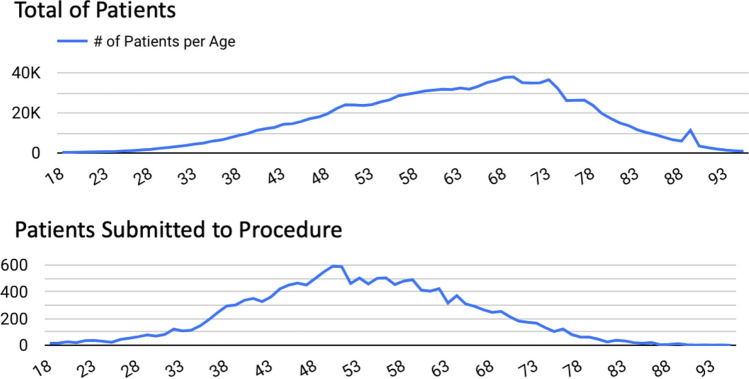
The analysis included a sample of 58,531,304 individuals, among which 1,250,273 were diagnosed with OSA between 2004 and 2020. The annual number of OSA diagnoses increased from 2.7% of total diagnoses in 2004 to 9.4% in 2017 (Table 1). The average age at diagnosis was 62 years, with a higher prevalence in males (61.3%) compared to females (38.7%) (Fig. 1). The racial and ethnic distribution among OSA patients was as follows: 75.6% Caucasian, 10.8% Black, 9.2% Hispanic, 2.3% Asian, and 2.1% unknown or undisclosed. Regarding education, the majority of patients (56.2%) had some post-high school education (Fig. 2).
Table 1.
Left: from 2004 to 2020 yearly OSA diagnoses
| Year | # Pat | % |
|---|---|---|
| 2004 | 35,474 | 2.8% |
| 2005 | 52,032 | 4.2% |
| 2006 | 52,881 | 4.2% |
| 2007 | 60,758 | 4.9% |
| 2008 | 63,126 | 5.0% |
| 2009 | 69,028 | 5.5% |
| 2010 | 67,103 | 5.4% |
| 2011 | 66,916 | 5.4% |
| 2012 | 69,027 | 5.5% |
| 2013 | 66,799 | 5.3% |
| 2014 | 70,075 | 5.6% |
| 2015 | 78,318 | 6.3% |
| 2016 | 102,127 | 8.2% |
| 2017 | 118,03 | 9.4% |
| 2018 | 104,041 | 8.3% |
| 2019 | 97,754 | 7.8% |
| 2020 | 76,784 | 6.1% |
Fig. 1.
(a) Age distribution of adult OSA diagnosed patients (b) Age distribution of patients submitted to therapeutic procedures for the condition
Fig. 2.
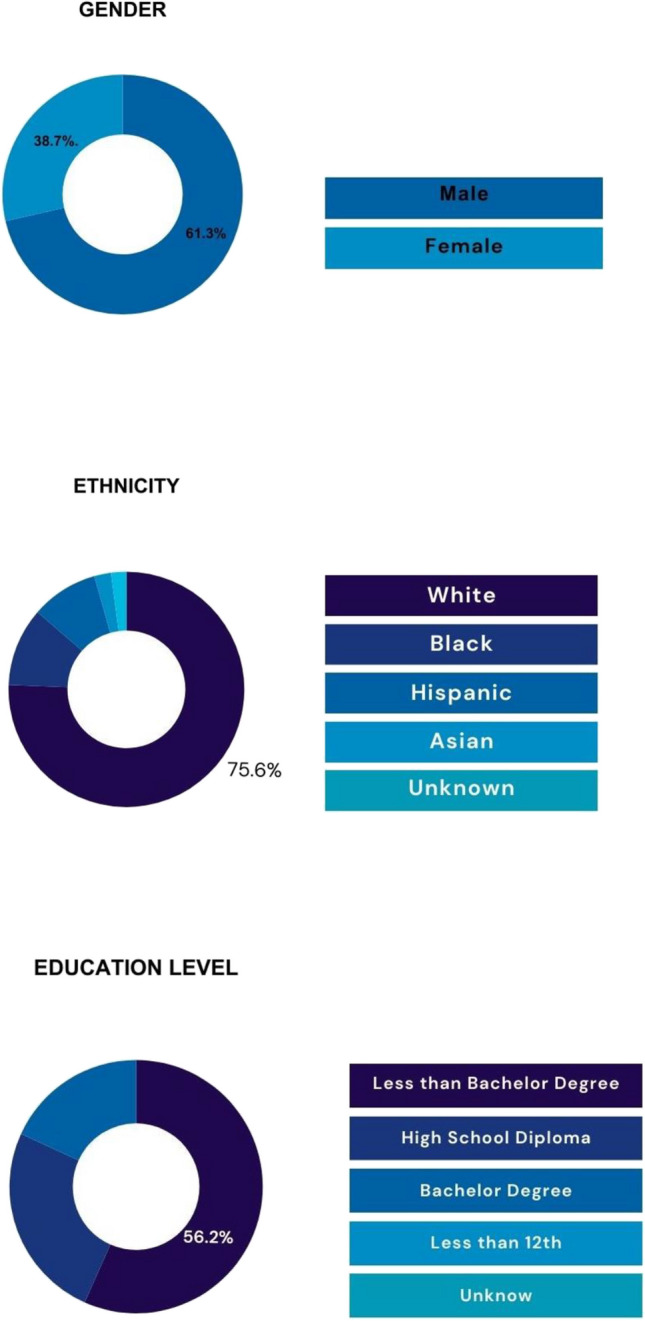
Demonstrate the distribution of gender, ethnicity and education level among the diagnosed patients with OSA between 2004-2020 in the EUA
Throughout the period from 2004 to 2020, the number of individuals diagnosed with obstructive sleep apnea (OSA) increased, whereas the proportion of those opting for surgical interventions declined. In 2006, approximately 2.9% of those diagnosed with OSA underwent surgical procedures. However, this percentage steadily decreased over the years, reaching a low of 0.6% in 2019 (Table 2). The year 2020 was notably impacted by the COVID-19 pandemic, with both OSA diagnoses and surgical interventions dropping to 0.2%.
Table 2.
Total surgeries by surgery type and in surgical OSA patients between 2004-2020 in EUA of OSA patients diagnosis between 200-2017 and patients number opting for surgical procedures
| Year | Total Pat. # | Cum. Pat. # | OSA Pat.# | Cum. OSA Pat. # | Surgery # | Cum. Surg. # | % OSA Pat | % Surgery Pat | Total % OSA Diag | Total % Surg |
|---|---|---|---|---|---|---|---|---|---|---|
| 2004 | 3,498,710 | 3,498,710 | 35,474, | 35,474 | 623.0 | 623.0 | 1.0% | 1.8% | 1.0% | 1.76% |
| 2005 | 4,916,692 | 8,415,402 | 52,032 | 87,506 | 1,326.0 | 1,949.0 | 1.1% | 2.5% | 1.0% | 2.15% |
| 2006 | 3,989,423 | 12,404,825 | 52,881 | 140,387 | 1,559.0 | 3,508.0 | 1.3% | 2.9% | 1.1% | 2.42% |
| 2007 | 3,972,471 | 16,377,296 | 60,758 | 201,145 | 1,521.0 | 5,028.0 | 1.5% | 2.5% | 1.2% | 2.44% |
| 2008 | 3,706,459 | 20,083,755 | 63,126 | 264,271 | 1,424.0 | 6,453.0 | 1.7% | 2.3% | 1.3% | 2.4% |
| 2009 | 3,203,623 | 23,287,378 | 69,028 | 333,299 | 1,416.0 | 7,869.0 | 2.2% | 2.1% | 1.5% | 2.34% |
| 2010 | 2,804,376 | 26,091,754 | 67,103 | 400,402 | 1,288.0 | 9,157.0 | 2.4% | 1.9% | 1,60% | 2.28% |
| 2011 | 2,707,420 | 28,799,174 | 66,916 | 467,318 | 1,037.0 | 10,194.0 | 2.5% | 1.5% | 1.7% | 2.19% |
| 2012 | 2,718,182 | 31,517,356 | 69,027 | 536,345 | 955.0 | 11,149.0 | 2.5% | 1.4% | 1.8% | 2.1% |
| 2013 | 2,707,942 | 34,225,298 | 66,799 | 603,144 | 831.0 | 11,980.0 | 2.5% | 1.2% | 1.9% | 2.02% |
| 2014 | 2,887,533 | 37,112,831 | 70,075 | 673,219 | 636.0 | 12,616.0 | 2.4% | 0.9% | 1.9% | 1.92% |
| 2015 | 3,267,258 | 40,380,089 | 78,318 | 751,537 | 619.0 | 13,235.0 | 2.4% | 0.8% | 2.0% | 1.82% |
| 2016 | 3,944,512 | 44,324,601 | 102,127 | 853,664 | 591.0 | 13,826.0 | 2.6% | 0.6% | 2.0% | 1.73% |
| 2017 | 4,244,576 | 48,569,177 | 118,03 | 971,694 | 637.0 | 14,463.0 | 2.8% | 0.5% | 2.1% | 1.64% |
| 2018 | 3,574,927 | 52,144,104 | 104,041 | 1,075,735 | 629.0 | 15,092.0 | 2.9% | 0.6% | 2.1% | 1.57% |
| 2019 | 3,244,917 | 55,389,021 | 97,754 | 1,173,489 | 631.0 | 15,723.0 | 3.0% | 0.6% | 2.2% | 1.51% |
| 2020 | 3,142,283 | 58,531,304 | 76,784 | 1,250,273 | 445.0 | 16,168.0 | 2.4% | 0.6% | 2.2% | 1.46% |
| Grand… | 58,531,304 | 58,531,304 | 1,250,273 | 1,250,273 | 16,168.0 | 16,168.0 | 2.1% | 1.3% | 2.1% | 1.29% |
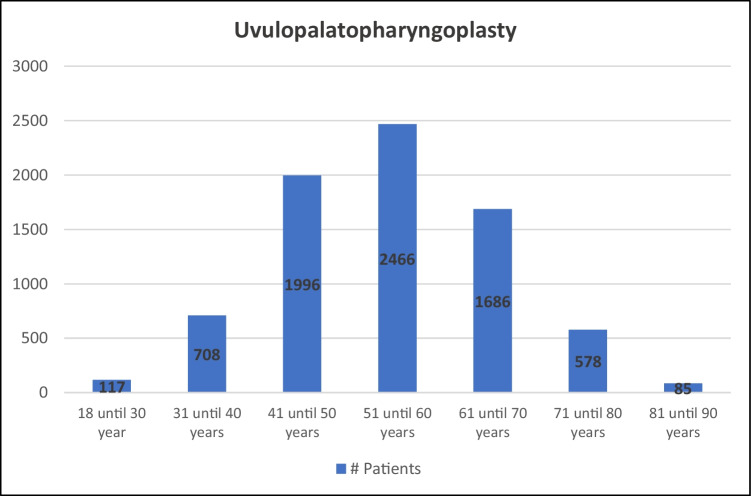
Among the surgical procedures performed, uvulopalatopharyngoplasty (UPPP) was the most common, with a total of 7,636 patients undergoing the procedure (Fig. 3). The average age for UPPP was 50.5 years. The frequency of UPPP peaked in 2006 with 883 cases, but subsequently declined to 100 cases by 2020. This procedure was performed more frequently on males than females (77.5% versus 22.5%, respectively), and the majority of patients identified as white (73.6%), followed by Hispanic (10.8%) and Black individuals (9.8%).
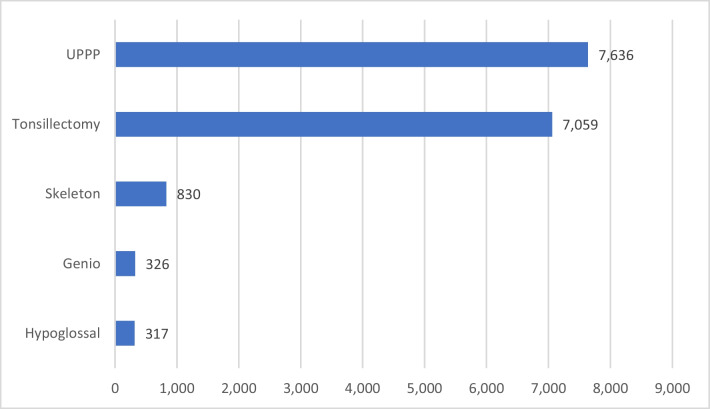
Fig. 3.
Age, overall number, gender, and ethnicity of patients submitted specifically to UPPP
Facial skeletal procedures for OSA, including isolated maxillary or mandibular advancements, as well as the more common combined maxillomandibular advancement (MMA), accounted for a smaller proportion of cases, with a total of 830 procedures or 5.1% of the reported cases (Fig. 4). The gender distribution for these procedures was relatively balanced (48.5% male and 42.6% female), and the number of annual procedures remained steady at around 50 until it dropped to 32 in 2020. Genioglossus advancement saw the most significant decline, with 50 cases reported in 2004 and single-digit cases from 2012 to 2020. The average age for facial skeletal surgeries was 55.2 years.
Fig. 4.
Percentage of each surgical procedure
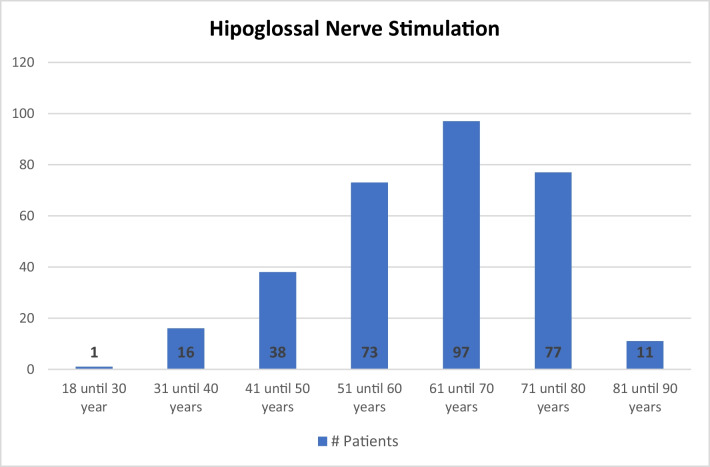
Another treatment option for OSA, the implantable hypoglossal nerve stimulator, was performed in 1.9% of patients, with its numbers increasing since 2016 (Fig. 5). Compared to other surgical interventions, this procedure was more prevalent among older patients, with a mean age of 62.0 years (Table 3). The male-to-female ratio for this procedure was approximately 2 to 1 (67.1% male and 32.9% female). Unlike other surgical procedures, the rate of patients opting for hypoglossal nerve stimulation has increased over time. However, there were pronounced racial disparities in this treatment modality, with 81.2% of patients identifying as white, 8% as Hispanic, and 6.1% as Black.
Fig. 5.
Age, overall number, gender, and ethnicity of patients submitted specifically to HNS
Table 3.
Medium age of patients in each type surgery
| Procedure | Average age |
|---|---|
| Tonsillectomy | 50.5 |
| UPPP | 54.7 |
| Skeleton | 55.2 |
| Genio | 55.8 |
| Hypoglossal | 62 |
Discussion
This investigation analyzed a large healthcare database in the United States to assess the volume, types, and distribution patterns of therapeutic procedures provided for Obstructive Sleep Apnea (OSA) across different social groups. The study considered variables such as Body Mass Index (BMI), OSA severity, and various surgical treatment modalities.
The real-world data presented in this study indicate that single-level palatal surgeries, such as uvulopalatopharyngoplasty (UPPP) and tonsillectomy, have been the most common surgical approaches for treating obstructive sleep apnea (OSA) in the United States [27–29]. These procedures accounted for the majority of sleep surgeries, with UPPP representing 47.2% and tonsillectomy representing 43.1% of the total from 2004 to 2020. However, the frequency of these surgeries has progressively decreased over time. In 2006, there were 1,453 procedures recorded, whereas in 2019, only 456 procedures were reported in the evaluated database. It is important to note that this study relies on the Optum database, which includes over 70 million patients, though other studies have also shown a reduction in surgical procedures for OSA over the years [28, 29].
This comprehensive review of surgical trends for treating Obstructive Sleep Apnea (OSA) across various demographics underscores the need for adaptive healthcare policies that respond to the evolving landscape of patient needs and treatment efficacies. Such insights could drive targeted improvements in clinical training and resource allocation.
The reasons behind the decline in palatal soft tissue surgeries for OSA during the study period remain unclear. The database used in this study does not assess referrals to sleep surgeons, and surgical approaches have evolved to address different phenotypes of OSA. It is possible that with improved patient selection, surgical procedures are now reserved for individuals with favorable anatomy, rather than being considered a necessary step before alternative procedures [30].
The decline in traditional palatal surgeries for OSA, as evidenced by our findings, may reflect an increased adoption of less invasive, more effective alternatives, such as hypoglossal nerve stimulation. This shift could represent a paradigm change in patient management, emphasizing precision medicine tailored to individual anatomical and physiological profiles.
The study findings revealed a male predominance across every subgroup within the cohort, including statistically significant sex disparities among patients who underwent surgical procedures. Although OSA prevalence and severity are generally lower in pre-menopausal women compared to men [31], recent data suggest that women may experience more severe outcomes from the disease, and these outcomes may be even worse than those observed in men with comparable degrees of OSA severity [32–34]. The hypoglossal nerve stimulation (HNS) procedure had the highest proportion of female patients (32.9%), while UPPP had the lowest (22.5%). The specific effects and outcomes of non-continuous positive airway pressure (CPAP) therapies across genders have not been extensively studied. However, recent findings suggest that females may have a higher likelihood of successful HNS therapy [35].
The study results demonstrate that hypoglossal nerve stimulation has been increasingly used as a treatment for OSA, despite an overall decrease in other surgical approaches. However, there remains a significant disparity in its application, with a higher proportion of Caucasian patients (81.2%) receiving this procedure, further highlighting the racial segregation in surgical approaches to OSA.
This national-level database study highlights the existence of sex and ethnic disparities in the treatment of OSA, indicating that sex and ethnic minorities may receive lower-quality healthcare and are less likely to receive routine medical care for OSA. These results raise concerns about healthcare equality and the possibility of selection bias.
The persistent disparities in surgical treatment for OSA highlight a significant area for policy intervention and research. Future studies should explore the barriers to equitable care and investigate the impact of socioeconomic and demographic factors on treatment efficacy. By understanding these dynamics, healthcare systems can develop more inclusive strategies that ensure all patients receive optimal care, regardless of their background.
The limitations of this study should be acknowledged. The Optum database primarily includes patients with private insurance, which may introduce a selection bias toward younger patients with active medical insurance and better access to healthcare. The analysis is also limited to the quality of data input by clinicians, and there is a possibility that the available codes may not accurately reflect patients’ true diagnoses from the prior year. As a database study, certain variables could not be evaluated, such as CPAP adherence and comorbidities. Additionally, other therapies, such as oral appliances and surgical procedures not included in the utilized code list, were not accounted for.
Improving the healthcare delivery system could directly enhance data outcomes by increasing the accuracy and completeness of the database used in the study. For instance, integrating comprehensive electronic health records with real-time data capture could ensure that more detailed patient information is recorded, leading to a richer dataset. This, in turn, could facilitate more nuanced analyses of surgical outcomes and patient demographics in relation to Obstructive Sleep Apnea (OSA) treatments. Additionally, standardizing data entry processes across different healthcare providers could reduce discrepancies and improve the reliability of the study findings, enabling a more effective assessment of treatment modalities and their impacts across diverse populations.
Conclusion
This descriptive observational study offers valuable demographic insights that provide a broad overview of OSA treatment in the USA. Nonetheless, further retrospective and prospective studies are necessary to explore healthcare disparities in OSA treatment, taking into account factors such as BMI, OSA severity, and non-surgical treatment options, to effectively address these inequalities.
Acknowledgements
This work was supported by the American Heart Association AHA #19CDA34660245 award granted to T.F.C.
Abbreviations
- CPAP
Continuous positive airway pressure
- CPT
Current procedural terminology
- HNS
Hypoglossal nerve stimulation
- ICD
International classification of diseases
- MMA
Maxilla-mandibular advancement
- OSA
Obstructive sleep apnea
- SD
Standard deviation
- UPPP
Uvulopalatopharyngoplasty
Funding
No funding was received for this research.
Data availability
All data supporting the findings of this study are available within the paper and its Identifier: DOI 10.17605/OSF.IO/H235F
Declarations
All authors have seen and approved the manuscript.
Ethical approval
For this type of study formal consent is not required.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gastaut H, Tassinari CA, Duron B (1965) Polygraphic study of diurnal and nocturnal (hypnic and respiratory) episodal manifestations of Pickwick syndrome. Rev Neurol (Paris) 112(6):568–579 [PubMed] [Google Scholar]
- 2.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heinzer R, Vat S, Marques-Vidal P et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4):310–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235 [DOI] [PubMed] [Google Scholar]
- 5.Vgontzas AN, Papanicolaou DA, Bixler EO et al (2000) Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab 85(3):1151–1158 [DOI] [PubMed] [Google Scholar]
- 6.Tufik S, Santos-Silva R, Taddei JA, Bittencourt LRA (2010) Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med 11(5):441–446 [DOI] [PubMed] [Google Scholar]
- 7.Punjabi NM, Bandeen-Roche K, Marx JJ, Neubauer DN, Smith PL, Schwartz AR (2002) The association between daytime sleepiness and sleep-disordered breathing in NREM and REM sleep. Sleep 25(3):307–314 [PubMed] [Google Scholar]
- 8.Gami AS, Howard DE, Olson EJ, Somers VK (2005) Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 352(12):1206–1214 [DOI] [PubMed] [Google Scholar]
- 9.Punjabi NM, Caffo BS, Goodwin JL et al (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6(8):e1000132 (Patel A, ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young T, Finn L, Peppard PE et al (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31(8):1071–1078 [PMC free article] [PubMed] [Google Scholar]
- 11.Marshall NS, Wong KKH, Liu PY, Cullen SRJ, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(8):1079–1085 [PMC free article] [PubMed] [Google Scholar]
- 12.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353(19):2034–2041 [DOI] [PubMed] [Google Scholar]
- 13.Iftikhar IH, Bittencourt L, Youngstedt SD et al (2017) Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 30:7–14 [DOI] [PubMed] [Google Scholar]
- 14.Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R (2018) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 22(3):555–568 [DOI] [PubMed] [Google Scholar]
- 15.Neruntarat C, Wanichakorntrakul P, Khuancharee K, Saengthong P, Tangngekkee M (2022) Upper airway stimulation vs other upper airway surgical procedures for OSA: a meta-analysis. Sleep Breath 26(1):407–418 [DOI] [PubMed] [Google Scholar]
- 16.Ayers CM, Lohia S, Nguyen SA, Gillespie MB (2016) The effect of upper airway surgery on continuous positive airway pressure levels and adherence: a systematic review and meta-analysis. ORL 78(3):119–125 [DOI] [PubMed] [Google Scholar]
- 17.Camacho M, Riaz M, Capasso R et al (2015) The effect of nasal surgery on continuous positive airway pressure device use and therapeutic treatment pressures: a systematic review and meta-analysis. Sleep 38(2):279–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kent D, Stanley J, Aurora RN et al (2021) Referral of adults with obstructive sleep apnea for surgical consultation: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 17(12):2507–2531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aurora RN, Casey KR, Kristo D et al (2010) Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep 33(10):1408–1413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mackey K, Ayers CK, Kondo KK et al (2021) Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med 174(3):362–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH (2017) Vital signs: racial disparities in age-specific mortality among Blacks or African Americans — United States, 1999–2015. MMWR Morb Mortal Wkly Rep 66(17):444–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts M, Reither EN, Lim S (2020) Contributors to the black-white life expectancy gap in Washington D.C. Sci Rep 10(1):13416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grandner MA (2020) Sleep, health, and society. Sleep Med Clin 15(2):319–340 [DOI] [PubMed] [Google Scholar]
- 24.Cohen SM, Howard JJM, Jin MC, Qian J, Capasso R (2022) Racial disparities in surgical treatment of obstructive sleep apnea. OTO Open 6(1):2473974X2210888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams DR, Lawrence JA, Davis BA, Vu C (2019) Understanding how discrimination can affect health. Health Serv Res 54(S2):1374–1388. 10.1111/1475-6773.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nong P, Williamson A, Anthony D, Platt J, Kardia S (2022) Discrimination, trust, and withholding information from providers: Implications for missing data and inequity. SSM - Population Health 18:101092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Won CHJ, Li KK, Guilleminault C (2008) Surgical treatment of obstructive sleep apnea: upper airway and maxillomandibular surgery. Proc Am Thorac Soc 5(2):193–199 [DOI] [PubMed] [Google Scholar]
- 28.Abdelwahab M, Marques S, Previdelli I, Capasso R (2022) Perioperative antibiotic use in sleep surgery: clinical relevance. Otolaryngol Head Neck Surg 166(5):993–1002 [DOI] [PubMed] [Google Scholar]
- 29.Abdelwahab M, Marques S, Howard J et al (2022) Incidence and risk factors of chronic opioid use after sleep apnea surgery. J Clin Sleep Med 18(7):1805–1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Camacho M, Li D, Kawai M et al (2016) Tonsillectomy for adult obstructive sleep apnea: a systematic review and meta-analysis: adult Tonsillectomy for OSA. Laryngoscope 126(9):2176–2186 [DOI] [PubMed] [Google Scholar]
- 31.Bixler EO, Vgontzas AN, Lin HM et al (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163(3):608–613 [DOI] [PubMed] [Google Scholar]
- 32.Kumar S, Anton A, D’Ambrosio CM (2021) Sex differences in obstructive sleep apnea. Clin Chest Med 42(3):417–425 [DOI] [PubMed] [Google Scholar]
- 33.Lozo T, Komnenov D, Badr MS, Mateika JH (2017) Sex differences in sleep disordered breathing in adults. Respir Physiol Neurobiol 245:65–75 [DOI] [PubMed] [Google Scholar]
- 34.Geer JH, Hilbert J (2021) Gender issues in obstructive sleep apnea. Yale J Biol Med 94(3):487–496 [PMC free article] [PubMed] [Google Scholar]
- 35.Kent DT, Carden KA, Wang L, Lindsell CJ, Ishman SL (2019) Evaluation of hypoglossal nerve stimulation treatment in obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg 145(11):1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting the findings of this study are available within the paper and its Identifier: DOI 10.17605/OSF.IO/H235F