Abstract
Background
Prior studies have shown that cardiovascular disease (CVD) can be effectively managed through telehealth. However, there are little national data on the use of telehealth in people with CVD or CVD risk factors. We aimed to determine the prevalence of telehealth visits and visit modality (video versus audio‐only) in people with CVD and CVD risk factors. We also assessed their rationale and satisfaction with telehealth visits.
Methods and Results
A nationally representative sample of 6252 participants from the 2022 Health Information National Trends Survey 6 was used. We defined the CVD risk categories as having no self‐reported CVD (coronary heart disease or heart failure) or CVD risk factors (hypertension, diabetes, obesity, or current smoking), CVD risk factors alone, and CVD. Multivariable logistic regression, adjusting for major sociodemographic factors, assessed the relationship between CVD risk and telehealth uptake. The weighted prevalence of using telehealth was 50% (95% CI, 44%–56%) for individuals with CVD and 40% (95% CI, 37%–43%) for those with CVD risk factors alone. Individuals with CVD had the highest odds of using any telehealth (audio‐only or video) (adjusted odds ratio [OR], 2.02 [95% CI, 1.39–2.93]) when compared with those without CVD or CVD risk factors. Notably, 21% (95% CI, 16.3%–25.6%) of patients with CVD used audio‐only visits (adjusted OR, 2.38 [95% CI, 1.55–3.64]) compared with patients without CVD or CVD risk factors.
Conclusions
In a nationally representative survey, there was high prevalence of any (video or audio‐only) telehealth visits in people with CVD, and audio‐only visits comprised a significant proportion of telehealth visits in this population.
Keywords: digital health, mHealth, policy, telehealth
Subject Categories: Digital Health, Health Services
Nonstandard Abbreviations and Acronyms
- HINTS
Health Information National Trends Survey
Clinical Perspective.
What Is New?
Patients with cardiovascular disease were more likely to use telehealth visits compared with those without cardiovascular disease, with ≈50% of patients with cardiovascular disease reporting using a telehealth visit (video or audio‐only) in the past year.
Approximately one‐fifth of participants with cardiovascular disease had audio‐only visits, suggesting that this is an important modality for patient access.
What Are the Clinical Implications?
Telehealth provisions put in place during the COVID‐19 public health emergency have only been extended through December 31, 2024, and only allow audio‐only visits temporarily, suggesting patients may lose access to care if these policies are not extended.
The COVID‐19 pandemic led to increased use of telehealth. Before 2020, telehealth visits made up <1% of visits across all specialties. 1 Since the pandemic, telehealth visits have stabilized at higher rates, with data from the 2021 National Health Interview Survey showing that 37% of adults in the United States had a telehealth visit in the preceding 12 months. 2 The Consolidated Appropriations Act of 2023 has extended telehealth flexibilities for Medicare patients until December 31, 2024, allowing for continued reimbursement of telehealth services, defined as real‐time communication between a patient and health care provider. 3 Currently, through the Consolidated Appropriations Act, many audio‐only telehealth services are provisional in nature, whereas behavioral and mental health audio‐only visits will be permanently part of the physician fee schedule and Medicare telehealth policy. 3
Cardiovascular disease (CVD) is highly prevalent, with >40% of the US population having CVD, and it is projected that both prevalence and cost of care for patients with CVD will increase in the coming decade. 4 CVD, such as heart failure and coronary artery disease, along with CVD risk factors, such as hyperlipidemia, hypertension, and diabetes, have been shown to be effectively managed via telehealth, which incorporates both remote clinician visits along with remote patient monitoring. 5 , 6 , 7 With the onset of the pandemic and the increasing role of telehealth for management of CVD and risk factor modification, the American Heart Association published a scientific statement reviewing the effectiveness of telehealth in CVD. 8 Given wide recognition that CVD disproportionately affects those who are older, from racial and ethnic minority groups, and of low socioeconomic status, care must be taken for telehealth to be delivered equitably to prevent exacerbation of the digital divide. 9
Significant efforts have been made to study the use of telehealth visits since the pandemic. Eberly et al identified several patient groups (older patients, Asian patients, and non–English‐speaking patients) with fewer telehealth visits in a large academic health center. 10 In addition, among those with telehealth visits, there are disparities in audio‐only versus video visits, with national data showing higher use of audio‐only visits in older, socioeconomically vulnerable, and minority groups. 11 Another study by Zachrison et al showed that video participation in telehealth visits was less likely in older adults, women, individuals of Black race, and those with increased social vulnerability. 12 Within the field of cardiology specifically, there have been disparities observed in the use of telehealth visits in academic practices, with further disparities seen in the use of video versus audio‐only visits, including among older patients, Black patients, and those with limited English proficiency. 13 In contrast, Yuan et al were able to describe impacts of telehealth use on cardiology practice patterns and follow‐up testing in the COVID‐19 era and showed that minorities and those with multiple cardiovascular comorbidities were more likely to have telehealth visits. 14 Single‐institution survey data of telehealth visit use for cardiology visits in Kentucky have given early insights into CVD patient satisfaction on communication and medical care provided during telehealth visits. 15
However, despite this prior work and the rapid expansion of telehealth visits in the general population, little is known about the uptake of telehealth visits among patients with CVD at the national level, and the modality of telehealth (audio versus video) used in this patient population. Given the potential of telehealth in improving the efficiency and effectiveness of CVD management, it is important to understand the barriers to the use of telehealth strategies in this population.
Using most recent data from the 2022 Health Information National Trends Survey (HINTS) 6, we sought to assess the prevalence and modality of telehealth visits in individuals diagnosed with CVD and those having CVD risk factors in a nationally representative survey of the US population. Additionally, we assessed participant rationale for telehealth visit selection, satisfaction with telehealth visits, and sociodemographic predictors of telehealth visits in this population and the association of these factors with visit modality.
METHODS
The data that support the findings of this study are available from the corresponding author on reasonable request.
Data Source
This study uses the HINTS data, which is the largest nationally representative survey of health technology use. HINTS 6 was collected from March 7 to November 8, 2022, and is the first cycle to include questions about telehealth. 16 The survey is sampled through a 2‐stage stratified design in which a sample of addresses are first chosen from a file of residential addresses, and 1 adult is chosen in each sampled household. The sampling strata consist of 4 strata based on high (>34% of the population are Hispanic ethnicity or Black race) versus low minority strata, which is further stratified by rural and urban geographic area. This ensures the sampling of minority and rural strata at higher rates to ensure a representative sample. Survey weights are demographically calibrated using 2021 American Community Survey estimates.
Analyses using the HINTS database met criteria for nonhuman subjects' research by an institutional review board, and this analysis did not require review. This cross‐sectional study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines.
Study Population
We included the 6252 adult participants from HINTS 6. Respondents were categorized as having CVD if they answered yes to the survey question “Has a doctor or other health professional ever told you that you had any of the following medical conditions: a heart condition such as heart attack, angina, or congestive heart failure?” 16 The presence of CVD risk factors was defined as having at least 1 CVD risk factor among survey questions asking respondents about the presence of hypertension, diabetes, or current cigarette smoking. Obesity was also included as a risk factor and was defined as a body mass index of at least 30 kg/m2.
Telehealth Measures
Telehealth use was assessed on the basis of the response to “In the past 12 months, did you receive care from a doctor or health professional using telehealth?” 16 A telehealth visit was defined as a “telephone or video appointment with a doctor or health professional.” Response options included “(select one): Yes, by video; Yes, by phone call (voice only with no video); Yes, some by video and some by phone call; and No telehealth visits in the past 12 months.” A survey response with any 1 of the first 3 options was considered positive for having a telehealth visit in the prior 12 months. We classified respondents as having video visits if they selected “yes, by video” or “yes, some by video and some by phone call,” whereas those who stated “yes, by phone call” as having audio‐only visits. Although telehealth as a term can include both clinical visits and other forms of nonclinical services, such as remote patient monitoring, based on the definition used by the survey, we use the term telehealth visit. 17
Other survey questions (Table S1) were used to assess the reasons why a telehealth visit was or was not used, the primary reason for recent telehealth visits, and participant experiences with their telehealth visits.
Statistical Analysis
Prevalence estimates and SEs were calculated using national survey weighting and linearized Taylor series variance estimation, according to HINTS analytics recommendations. 18 Demographic characteristics were described as the weighted proportion among the subpopulation without CVD or risk factors, those with CVD, and those with CVD risk factors only. The Pearson χ2 test was used to assess for differences between groups. We then determined telehealth use and modality (video versus audio‐only) for these groups and further described demographic characteristics based on modality.
We used multivariable regression to estimate the odds and 95% CI of any telehealth visit (versus no telehealth visit) in association with CVD risk category (no CVD or CVD risk factors alone, CVD risk factors, and CVD). We used binomial logistic models with 2 mutually exclusive indicator variables for telehealth modalities based on participant survey response: (1) audio‐only visit group or (2) video visit group (those with video visits only or a mix of video and audio visits). For each telehealth modality group, we assessed the odds of each modality versus no telehealth visit. Additional variables were introduced into the model in a stepwise manner: first, by adjusting for age and sex, then by incorporating race, educational level, income, and rurality, and then lastly including frequency of provider visits over the preceding 12 months. Frequency of provider visits was defined in the survey by the response to the survey question, “In the past 12 months, not counting times you went to an emergency room, how many times did you go to a doctor, nurse, or other health professional to get care for yourself?” To maintain predictive power, demographic variables were collapsed into binary variables. The Archer‐Lemeshow goodness‐of‐fit test was used to determine final model fit.
All analyses were conducted using Stata, version 15.1 (StataCorp, College Station, TX). All statistical tests were 2 sided, with the level of statistical significance set at α=0.05.
RESULTS
The HINTS survey from 2022 included 6252 participants, representing 258.4 million US adults. The mean±SD age among these survey respondents was 54.6±19.1 years. Women represented 51% of the population‐weighted estimate of respondents. A total of 3480 participants, representing 135.7 million US adults, had risk factors for CVD, self‐reporting the presence of diabetes, hypertension, current tobacco use, or a body mass index ≥30 kg/m2. A total of 607 participants had a self‐reported heart condition (CVD), representing 18.9 million US adults.
Table 1 shows the weighted prevalence of demographic characteristics in the population without CVD or CVD risk factors, those with CVD risk factors, and those with CVD. Compared with those without CVD or CVD risk factors, participants with CVD were more likely to be aged ≥65 years, men, of Black race, have a lower educational level and household income, and be from a rural region. Additionally, participants with CVD reported increased health care use, with higher numbers of outpatient visits in the preceding 12 months. Figure S1 provides additional data on the weighted prevalence of CVD and CVD risk factors across demographic groups.
Table 1.
Demographic Characteristics by Presence of History of or Risk Factors for CVD
| Characteristic | No CVD or CVD risk factors (n=1804) | CVD risk factors (n=3480) | CVD (n=607) | P value by χ2 |
|---|---|---|---|---|
| Age, y | ||||
| 18–34 | 39.1 (35.2–43.1) | 17.9 (14.4–22.0) | 5.7 (3.2–10.2) | <0.001 |
| 35–49 | 25.6 (22.6–28.9) | 26.1 (23.1–29.3) | 12.1 (7.8–18.1) | |
| 50–64 | 23.1 (20.4–26.1) | 30.3 (27.5–33.4) | 28.2 (22.8–34.3) | |
| ≥65 | 12.1 (10.5–14.0) | 25.6 (23.7–27.6) | 54.0 (47.2–60.8) | |
| Sex | ||||
| Women | 51.5 (47.7–55.2) | 51.8 (48.4–55.2) | 39.3 (34.4–44.4) | <0.05 |
| Men | 48.5 (44.8–52.3) | 48.2 (44.8–51.5) | 60.7 (55.6–65.5) | |
| Race and ethnicity | ||||
| Non‐Hispanic White | 63.7 (59.8–67.5) | 58.9 (54.9–62.9) | 67.4 (59.9–73.9) | <0.001 |
| Non‐Hispanic Black | 7.6 (5.9–9.3) | 13.2 (11.5–14.9) | 13.0 (9.4–17.9) | |
| Hispanic | 15.9 (13.1–19.4) | 18.2 (15.8–20.8) | 11.2 (7.8–15.9) | |
| Non‐Hispanic Asian | 8.7 (6.7–11.3) | 3.9 (2.4–6.2) | 4.5 (1.6–11.9) | |
| Non‐Hispanic other* | 4.0 (2.5–6.4) | 5.8 (3.9–8.4) | 3.9 (2.0–7.6) | |
| Educational level | ||||
| Less than high school | 3.1 (1.9–4.9) | 7.8 (6.2–9.8) | 14.5 (9.9–20.7) | <0.001 |
| High school graduate | 19.1 (16.0–22.7) | 23.2 (21.0–25.8) | 21.0 (16.4–26.6) | |
| Some college | 31.9 (27.7–36.3) | 43.4 (40.6–46.4) | 42.3 (35.8–49.0) | |
| Bachelor's degree or more | 45.9 (41.9–49.9) | 25.3 (23.3–27.5) | 22.1 (18.2–26.6) | |
| Annual household income, % | ||||
| <20 000 | 9.8 (7.4–13.0) | 15.3 (13.1–17.7) | 24.1 (19.2–29.7) | <0.001 |
| 20 000 to <35 000 | 7.4 (5.9–9.1) | 13.6 (11.7–15.7) | 10.7 (7.6–14.9) | |
| 35 000 to <50 000 | 9.7 (7.3–12.7) | 12.9 (11.1–14.9) | 15.5 (11.5–20.6) | |
| 50 000 to <75 000 | 18.9 (15.8–22.5) | 18.2 (15.7–20.9) | 17.0 (12.3–23.2) | |
| ≥75 000 | 52.1 (50.4–57.8) | 39.9 (36.8–43.2) | 32.7 (26.4–39.7) | |
| Location | ||||
| Urban | 89.3 (88.9–91.3) | 84.2 (81.8–86.3) | 80.2 (74.9–84.7) | <0.001 |
| Rural | 10.7 (8.6–13.1) | 15.8 (13.7–18.1) | 19.8 (15.3–25.1) | |
| Frequency of provider visits | ||||
| 0 | 16.4 (13.6–19.5) | 12.8 (10.8–15.1) | 7.0 (4.5–10.8) | <0.001 |
| 1–4 | 66.6 (62.9–70.2) | 63.7 (60.8–66.6) | 52.6 (46.3–58.7) | |
| 5–9 | 10.1 (8.1–12.5) | 14.3 (12.4–16.3) | 18.5 (14.9–22.7) | |
| ≥10 | 6.9 (5.2–9.2) | 9.1 (7.7–10.9) | 21.9 (17.3–27.4) | |
Data are given as percentage of US adult weighted population (95% CI). Demographic characteristics of the study population were compared between those patients with no CVD or CVD risk factors, CVD risk factors alone, and CVD. P values were calculated using the χ2 test. CVD indicates cardiovascular disease.
Other race includes Native American, Alaskan, Pacific Islander, and those who selected multiple races.
Use of Telehealth Visits
A total of 2517 participants, representing a weighted percentage of 39% (95% CI, 37–41%) or 97.9 million US adults, reported having either an audio or video telehealth visit in the 12 months before survey administration. In terms of telehealth modality, 27% of the total weighted sample of respondents (95% CI, 26%–29%) had a video visit and 12% had an audio‐only visit (95% CI, 11%–13%). Prevalence of any telehealth visit among participants with CVD (weighted percentage 50% [95% CI, 44%–56%]) was higher than that in participants with CVD risk factors only (40% [95% CI, 37–43%]) or without any CVD risk (36% [95% CI, 32%–39%]). Of participants with CVD, a weighted estimate of 29% (95% CI, 23%–36%), representing 5.4 million US adults, had video visits and 21% (95% CI, 16%–26%), representing 3.8 million US adults, had audio‐only visits (Table 2).
Table 2.
Use of Telehealth Visits in HINTS 6
| Telemedicine modality | Any telehealth visit | Video telehealth visit | Audio telehealth visit | ||||||
|---|---|---|---|---|---|---|---|---|---|
| population | Any telehealth visit users, N (%) | Weighted national estimate (95% CI) | Weighted % (95% CI) | Video telehealth visit users, N (%) | Weighted national estimate (95% CI) | Weighted % (95 CI) | Audio telehealth visit users, N (%) | Weighted national estimate (95% CI) | Weighted % (95 CI) |
| HINTS 6 participants | 2517/6046 (41.6) | 97.9 (91.3–104.5) million | 39.3 (37.4–41.3) | 1641/6046 (27.1) | 67.8 (62.7–72.9) million | 27.2 (25.6–28.9%) | 876/6046 (14.5) | 30.1 (27.0–33.2) million | 12.2 (11.0–13.3) |
| HINTS 6 participants without CVD or CVD risk factors | 688/1790 (38.4) | 31.5 (28.0–35.0) million | 35.7 (32.2–39.3) | 482/1790 (26.9) | 22.5 (19.6–25.5) million | 25.6 (22.4–29.0) | 206/1790 (11.5) | 8.9 (7.0–10.9) million | 10.1 (8.0–12.7) |
| HINTS 6 participants at risk for CVD | 1430/3409 (41.9) | 53.7 (48.9–58.6) million | 40.3 (37.4–43.2) | 935/3409 (27.4) | 37.8 (33.7–42.0) million | 28.4 (25.9–31.0) | 495/3409 (14.5) | 15.9 (14.0–17.8) million | 11.9 (10.5–13.5) |
| HINTS 6 participants with CVD | 300/598 (50.2) | 9.3 (7.6–10.9) million | 49.7 (43.6–55.9) | 167/598 (27.9) | 5.4 (4.3–6.6) million | 29.1 (23.4–35.5) | 133/598 (22.2) | 3.8 (3.2–4.5) million | 20.6 (16.3–25.6) |
Frequencies and proportions of participants with telehealth visits are reported for those in the entire HINTS 6 survey, without CVD or CVD risk factors, with CVD risk factors, and with CVD. The weighted national estimate and weighted national percentage of the population with 95% CIs are also reported using Taylor series variance estimation in accordance with HINTS 6 method guidelines. CVD indicates cardiovascular disease; and HINTS, Health Information National Trends Survey.
Demographic characteristics were compared in patients with CVD or CVD risk factors according to telehealth modalities (no telehealth visit, video, and audio‐only visit). In patients with CVD, there were no differences in video versus audio‐only telehealth visits by age, sex, race, educational level, income, or frequency of provider visits (Table S2). Compared with participants without a telehealth visit, those with audio‐only visits tended to live in urban areas. In contrast, for patients with CVD risk factors, a greater percentage of patients with audio‐only visits were aged ≥65 years, were White race, were at least high school graduates, and had income ≥$75 000 (Table S3).
In the entire cohort, having CVD was associated with higher odds of having a telehealth visit. In multivariable regression modeling that adjusted for demographic factors and frequency of provider visits, those with CVD risk factors had an odds ratio (OR) of 1.2 (95% CI, 0.98–1.55; P=0.076), whereas those with CVD were twice as likely (OR, 2.0 [95% CI, 1.39–2.93]; P<0.001) to report a telehealth visit compared with those with no CVD or CVD risk factors. In the regression, other covariates that were associated with telehealth visits included being a woman, being a college graduate, and having at least 5 visits with a health care professional in the preceding 12 months. In contrast, age >50 years and being from a rural area were associated with lower odds of telehealth visits (Figure 1). No significant interactions between each of the demographic variables with CVD status were observed. Archer‐Lemeshow goodness‐of‐fit test had a P value of 0.43, indicating appropriate fit of the data. No collinearity between independent variables was observed.
Figure 1. Multivariable analysis of telehealth visit (video or audio‐only) use in all respondents.
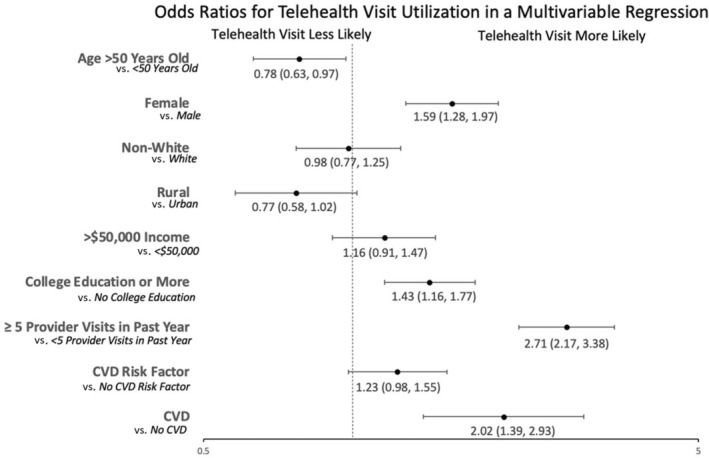
Odds ratios and corresponding 95% CIs for individual variables incorporated into a multivariable logistic regression of telehealth use in all participants are reported in a forest plot. The x axis of the plot is reported on a log scale. Variables with statistically significant odds ratios included cardiovascular disease (CVD), college education, female sex, and >5 visits in a year (denoting seeing a provider >5 times in a year).
CVD was also associated with higher odds of having an audio‐only telehealth visit. After adjusting for demographic factors and visit frequency, those with CVD were more than twice as likely (OR, 2.3 [95% CI, 1.6–3.6]; P<0.001) to report an audio‐only visit versus no telehealth visit (Figure 2). Having at least 5 visits with a health care professional in the preceding 12 months (OR, 1.9 [95% CI, 1.5–2.5]; P<0.001) and being a woman (OR, 1.5 [95% CI, 1.1–2.1]; P<0.001) were also associated with audio‐only visits. Being from a rural area was associated with lower odds of having an audio‐only visit (OR, 0.58 [95% CI, 0.4–0.8]). Archer‐Lemeshow goodness‐of‐fit test had a P value of 0.8, indicating appropriate fit of the data. No collinearity between independent variables was observed. CVD was also associated with use of video telehealth (OR, 1.8 [95% CI, 1.1–2.9]; P=0.02). For those with video visits, female sex, being a college graduate, income >$50 000, and >5 visits with a health care professional were associated with more video visits. Age >50 years was associated with lower odds of having a video visit (OR, 0.7 [95% CI, 0.5–0.9]; P=0.005).
Figure 2. Multivariable analysis of audio‐only and video telehealth visit use in all respondents.
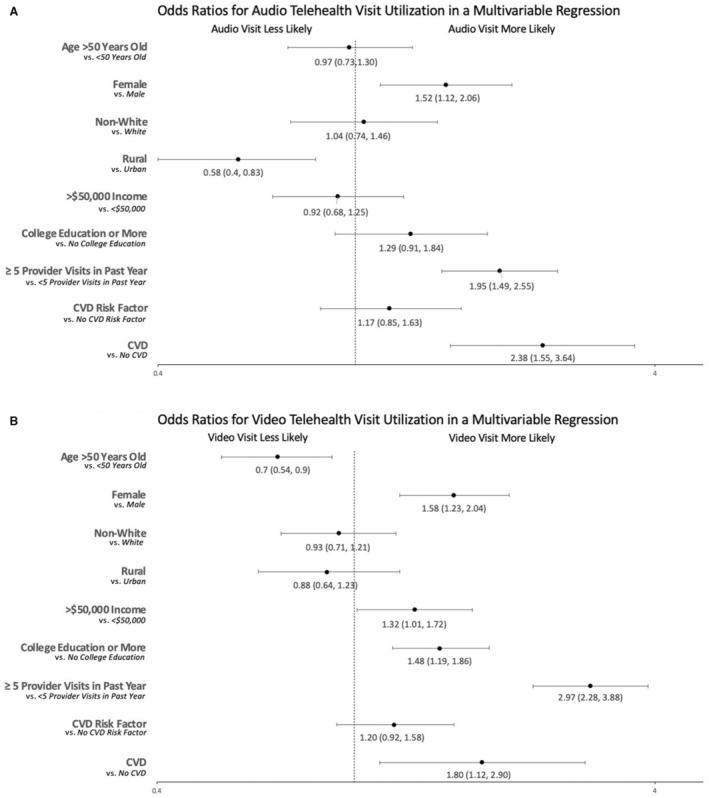
Odds ratios and corresponding 95% CIs for individual variables incorporated into a multivariable logistic regression of audio‐only (A) and video (B) telehealth visit use in all participants are reported in a forest plot compared with those without any telehealth visits. A telehealth visit was defined as a “telephone or video appointment with a doctor or health professional.” Survey response options included “(select one): Yes, by video; Yes, by phone call (voice only with no video); Yes, some by video and some by phone call; and No telehealth visits in the past 12 months.” We classified respondents as having video visits if they selected “yes, by video” or “yes, some by video and some by phone call,” whereas those who stated “yes, by phone call” as having audio‐only visits. The x axis of the plot is reported on a log scale. CVD indicates cardiovascular disease.
Among those with telehealth visits, participants were asked to identify why they had a telehealth visit. Across all groups, the most common reason was that the provider recommended a telehealth visit, with 71% (95% CI, 65%–76%) of individuals without CVD or CVD risk factors, 75% (95% CI, 72%–78%) with CVD risk factors, and 73% (95% CI, 64%–80%) with CVD reporting this as the reason why they chose telehealth as a visit modality. Convenience was also cited as a major reason for telehealth visits, with 68% (95% CI, 63%–73%) of individuals without CVD or CVD risk factors, 64% (95% CI, 60%–68%) with CVD risk factors, and 54% (95% CI, 46%–63%) with CVD providing this answer. Fewer than half of respondents across all subgroups agreed that they chose telehealth to determine if an in‐person visit was necessary, to avoid infection exposure, or to include family in the visit.
The primary reason for participants' most recent telehealth visit differed across subgroups (Table 3). For those without CVD or risk factors for CVD, the most common reason for participants' most recent telehealth visit was minor illness/acute care (37% [95% CI, 31%–43%]) regardless of telehealth visit modality. A higher percentage of those with audio‐only visits used their telehealth visit for an annual visit (24% [95% CI, 14.9%–36.4%]) compared with those with video visits (10% [95% CI, 7.8%–14.6%]). For those with CVD risk factors alone or CVD, having a chronic health condition was the most common reason for participants' most recent telehealth visit. A total of 27% (95% CI, 24%–31%) of those with CVD risk factors alone cited a chronic health condition as the rationale for their prior visit, whereas 36% (95% CI, 27%–46%) of those with CVD reported their telehealth visit was for chronic health condition management. Those with CVD or CVD risk factors were also numerically more likely to use telehealth for their annual visit, although 95% CIs overlapped. Those with CVD were less likely to use telehealth visits for mental health compared with the group without CVD or CVD risk factors. In patients with CVD or CVD risk factors, no differences were seen in reasons for telehealth visits by modality.
Table 3.
Primary Reason for Most Recent Telehealth Visit
| Visit type | No CVD or risk factors | CVD risk factors | CVD |
|---|---|---|---|
| Annual visit | 14.4 (10.8–19.0) | 19.1 (15.2–23.7) | 21.9 (16–29.1) |
| Minor illness/acute care | 36.8 (31.2–42.6) | 25.4 (21.5–29.7) | 20.7 (12.9–31.3) |
| Chronic health condition | 11.3 (7.7–16.2) | 27.3 (23.8–31.1) | 36.0 (27.1–46.1) |
| Medical emergency | 1.8 (0.7–4.1) | 1.4 (0.8–16.4) | 0.28 (0.08–0.8) |
| Mental health | 21.4 (16.4–27.4) | 13.4 (10.9–16.4) | 8.6 (4.9–14.9) |
| Other | 14.4 (10.8–18.9) | 13.4 (11.2–15.9) | 12.5 (6.9–21.3) |
Data are given as percentage US adult weighted population (95% CI). The proportion of survey respondents reporting the above reasons for telehealth visits are presented in percentage terms for those with no CVD or CVD risk factors, those with CVD risk factors, and those with CVD. All percentages are weighted estimates of the US adult population. CVD indicates cardiovascular disease.
Of those participants who did not have telehealth visits in the preceding 12 months, respondents with CVD or CVD risk factors were more likely to have been offered telehealth visits. A total of 69% (95% CI, 62%–75%) of those with CVD risk factors and 75% (95% CI, 61%–85%) of those with CVD reported they were offered telehealth visits but declined versus 17% (95% CI, 13%–21%) of those without CVD or CVD risk factors.
For those who were offered but chose not to participate in a telehealth visit, across all subgroups, ≥80% of participants agreed that this was because they preferred in‐person visits. A total of 28% (95% CI, 15%–46%) of those with CVD also agreed that they chose not to participate in telehealth visits because of a belief that the technology would be too difficult to use compared with 19% (95% CI, 13%–26%) of those with CVD risk factors and 20% (95% CI, 12%–31%) of those without CVD or CVD risk factors.
Satisfaction With Telehealth Visits
Among respondents with a telehealth visit in the past year, there were no differences in telehealth visit satisfaction by modality or CVD subgroup. Of those without CVD or CVD risk factors, 73% (95% CI, 67%–78%) with video visits versus 76% (95% CI, 62%–85%) with audio‐only visits reported that they either somewhat agreed or strongly agreed that their telehealth visit was as good as an in‐person visit. These proportions were similar across those with CVD risk factors or CVD, with 77% (95% CI, 72%–82%) of those with video visits and 74% (95% CI, 67%–80%) of those with audio‐only visits with CVD risk factors reporting satisfaction with telehealth quality. Similarly, among those with CVD, 74% (95% CI, 60%–85%) of those with video visits and 85% (95% CI, 75%–90%) of those with audio‐only visits were satisfied with the quality of their visit.
A total of 30% of respondents with CVD agreed that they had technical problems with their telehealth visit, such as difficulty using the technology or trouble seeing or hearing their health care professional. There were no statistically significant differences based on video versus audio‐only visits in reporting of difficulty with technology, with 32% (95% CI, 22%–42%) of those with video visits and 27% (95% CI, 17%–40%) of those with audio‐only visits reporting difficulty with technology. A total of 20% of participants with CVD risk factors, and 17% of those without CVD or CVD risk factors, reported technical difficulties; however, these differences were not statistically significant compared with those with CVD. In addition, no differences were seen in reporting of technical difficulties in these groups based on modality of telehealth visit.
DISCUSSION
In this nationally representative sample, we found that US respondents with CVD were more likely to have a telehealth visit than those without CVD or CVD risk factors, even after adjusting for frequency of provider visits and demographic factors. We found that approximately half of participants with CVD reported a telehealth visit in the preceding 12 months, compared with ≈39% of the entire study population. The rates of national telehealth visit use in this analysis are similar to the 2021 National Health Interview Survey study showing that 37% of US adults had a telehealth visit in the preceding 12 months, indicating that national telehealth use has remained stable. 2 However, our findings of high national telehealth visit use in those with CVD following the COVID‐19 pandemic are novel. A recently published study on telehealth visits in patients with CVD from June 2020 to June 2021 showed similar trends to this national population and found those who were younger, women, and from an urban area were more likely to use telehealth visits. 19 Although this analysis also showed that participants who are aged <50 years and women were more likely to use telehealth visits overall, these factors were not significant in predicting telehealth visits in those with CVD based on interaction term testing.
Notably, we found that approximately one‐fifth of participants with CVD report audio‐only visits, and participants with CVD had more than twice the odds of having an audio‐only visit. This finding of 21% of patients with CVD using audio‐only visits at a national level represents a significant amount of care being provided through an audio‐only medium. These findings are similar to a single‐institution study conducted at Stanford, which showed that 21% of visits at 2 outpatient cardiology practices were delivered by telephone, with audio‐only visits more prevalent in patients who were aged >80 years, of Black race, and non–English‐speaking individuals. 13 In contrast, our study did not show differences in sociodemographic variables based on telehealth visit modality in patients with CVD, although older adults with CVD risk factors were more likely to use audio‐only visits. In the entire cohort, our findings of higher educational level, higher income, and younger age being associated with video visits is similar to prior studies. Rural patients were less likely to have audio‐only use despite the fact that these areas typically have less broadband access, conceivably making audio visits particularly important. Prior studies have shown some association of urbanicity, especially with inner‐city individuals in the use of telehealth visits. 19 However, the significant association of rurality with lower use of audio‐only visits is concerning, especially given the known disparities in cardiovascular outcomes in rural versus urban populations. 20 , 21 Considering the known shortage of cardiologists in rural areas, the lower access to audio‐only visits in this population may point to decreased access to care. 22
Audio‐only reimbursement is only permanent for behavioral and mental health conditions past December 31, 2024, unless further legislation is passed to continue reimbursement for these visits for other health conditions. 3 Although video visits allow for a visual physical examination and 1 study showed telephone visits were associated with worse outcomes compared with video visits in remote heart failure care, there is need for further studies on the impact of audio‐only versus video telehealth visits given the significant and lasting proportion of uptake of audio‐only visits. 23 In addition, audio‐only visits have been associated with increased digital inclusivity, and the loss of access to these visits may cause challenges in delivering care to patients who have been using these types of visits since the public health emergency in 2020. 24
Approximately 73% of those with CVD reported using telehealth because their health professional recommended it, with 36% reporting their most recent telehealth visit was for chronic disease management. These findings did not differ across video or audio‐only telehealth visit modality. Additionally, even among those who did not use telehealth, those with CVD or CVD risk factors reported they were offered telehealth at a higher rate than those without, with ≈70% offered telehealth. This survey shows that the clinician recommendation is the most cited reason for using telehealth, and clinicians in the CVD space may be offering patients telehealth more often. A recent meta‐analysis of telehealth for the management of CVD showed that telehealth visits reduced cardiovascular‐related mortality and hospitalization in patients with heart failure when remote consultation was combined with remote patient monitoring. 25 In addition, the analysis found that telehealth visits could be used for cardiovascular risk modification, such as improvements in blood pressure, cholesterol, and body mass index. 25 Given the robust evidence, the American Heart Association's scientific statement on the use of telehealth for CVD management may reflect a stronger embrace of telehealth in cardiovascular medicine compared with other fields. 8
Our analysis found a high level of participant satisfaction with telehealth visits, with >70% of respondents across all groups agreeing that their telehealth visit was as good as an in‐person visit. Notably, satisfaction levels were high across both video and audio‐only participants, with no differences seen, similar to a prior single‐institution study that showed that patients perceived audio visits favorably. 26 Approximately one‐third of respondents with CVD reported experiencing some technical difficulties with their visit, which was not statistically significant but trended higher than was reported in prior studies in cardiology. 15 Additionally, in those without telehealth visits, difficulty using technology was cited by ≈30% of patients with CVD as a reason why telehealth was declined in favor of an in‐person visit. Although there are not standardized metrics for assessing telehealth quality, the high overall satisfaction with telehealth seen in this study is similar to prior studies. 15 , 26 , 27
As telehealth use increased during the pandemic, there was concern that telehealth may exacerbate the digital divide, with those who are older, from racial/ethnic minority groups, and with lower socioeconomic status having less access to care. Our analysis found that women and those with at least a college education were significantly more likely to report telehealth visits overall, and there were no differences in use in those with CVD by sociodemographic factors. This is in contrast to a prior analysis that found that patients who were older and of racial/ethnic minority groups were less likely to use telehealth visits, although another analysis showed that underrepresented minority groups were more likely to use remote cardiovascular care. 10 , 14 Given known associations between older age and underrepresented minority status with broadband and smartphone access, further work is needed to ensure that telehealth implementation among those with CVD does not exacerbate health inequities. 28 In addition, given some studies have associated telehealth use in cardiology with fewer prescriptions and tests, further work should delineate the health outcomes of increased telehealth uptake and audio‐only visits in the population with CVD. 14 , 29
Limitations
There are several important limitations of this study. Given that this analysis uses cross‐sectional survey data, it is unable to demonstrate causation. In addition, the HINTS 6 survey response rate is 28%, which is low but similar to other national surveys, and the survey is weighted to adjust for nonresponse. The survey requires participants to self‐report data over the prior 12 months, which can lead to recall bias. The survey also asks participants if they have had any history of heart disease but does not distinguish between the specific diagnosis the participant may have. There is also no linkage to laboratory data, such as cholesterol levels, and the survey did not ask about hyperlipidemia. However, HINTS is the largest national survey of health information technology use and the first to report national telehealth visit use following the COVID‐19 pandemic.
CONCLUSIONS
This analysis of a nationally representative survey demonstrates that patients with CVD are more likely to use telehealth visits than those without CVD or CVD risk factors, even after adjusting for frequency of provider visits and demographic factors. Furthermore, more than one‐fifth of participants with CVD received audio‐only visits, suggesting that this is an important modality for patient access. Given Medicare telehealth flexibilities have only been extended through the end of 2024, the findings of this study can inform policy efforts for sustainable telehealth visit use, especially for those using audio‐only visits. Addressing technical issues in the use of telehealth visits remains an area that requires further study with the increasing adoption of telehealth in patients with CVD. Future studies may additionally explore the impacts of audio‐only versus video telehealth visits on cardiovascular outcomes of interest.
Sources of Funding
None.
Disclosures
Under a license agreement between Corrie Health and Johns Hopkins University, the university owns equity in Corrie Health. The university, Dr Marvel, and Dr Martin are entitled to royalty distributions related to Corrie Health. Additionally, Drs Martin and Marvel are cofounders of and holds equity in Corrie Health. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict‐of‐interest policies. Dr Martin reports support from the American Heart Association (20SFRN35380046, 20SFRN35490003, 878924, 882415, and 946222), the Patient‐Centered Outcomes Research Institute (ME‐2019C1‐15 328 and IHS‐2021C3‐24 147), the National Institutes of Health (P01 HL108800 and R01AG071032), the David and June Trone Family Foundation, the Pollin Digital Innovation Fund, Sandra and Larry Small, CASCADE FH, Google, Amgen, and Merck. Dr Martin has also received research and material support from Apple and iHealth. Furthermore, Dr Martin is on the Advisory Board for Care Access and reports personal consulting fees from Amgen, AstraZeneca, BMS, Chroma, Kaneka, Merck, NewAmsterdam, Novartis, Novo Nordisk, Premier, Sanofi, and 89bio. Dr Spaulding reports support from the American Heart Association (20SFRN35380046 and 878924) and National Institutes of Health (U01HL096812). Dr Spaulding reports personal consulting fees from Corrie Health. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S3
Figure S1
Acknowledgments
Author contributions: Drs Bhatla and Ding had full access to all the data in the study and take responsibility for the integrity and accuracy of the data analysis. Concept and design: Drs Bhatla, Ding, and Martin; acquisition, analysis, and interpretation of the data: Drs Bhatla, Ding, and Martin; drafting of the manuscript: all authors; critical revision of the manuscript for important intellectual content: all authors; statistical analysis: Drs Bhatla and Ding.
This manuscript was sent to Kori S. Zachrison, MD, MSc, Guest Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.124.036475
For Sources of Funding and Disclosures, see page 10.
References
- 1. Samson L, Tarazi Turrini G, Sheingold S. Medicare Beneficiaries' Use of Telehealth Services in 2020—Trends by Beneficiary Characteristics and Location (Issue Brief No. HP‐2021‐27). Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2021. [Google Scholar]
- 2. Lucas JW, Villarroel MA. Telemedicine Use Among Adults: United States, 2021. NCHS Data Brief, no 445. National Center for Health Statistics; 2022. [PubMed] [Google Scholar]
- 3. Telehealth Policy Changes After the COVID‐19 Public Health Emergency. Department of Health and Human Services; 2023. Accessed January 24, 2024. https://telehealth.hhs.gov/providers/telehealth‐policy/policy‐changes‐after‐the‐covid‐19‐public‐health‐emergency [Google Scholar]
- 4. American Heart Association . Cardiovascular disease: a costly burden for America. Projections through 2035. Accessed January 3, 2023. https://www.heart.org/‐/media/Files/Get‐Involved/Advocacy/Burden‐Report‐Consumer‐Report.pdf.
- 5. Rosen D, McCall JD, Primack BA. Telehealth protocol to prevent readmission among high‐risk patients with congestive heart failure. Am J Med. 2017;130:1326–1330. doi: 10.1016/j.amjmed.2017.07.007 [DOI] [PubMed] [Google Scholar]
- 6. Inglis SC, Clark RA, Dierckx R, Prieto‐Merino D, Cleland JG. Structured telephone support or non‐invasive telemonitoring for patients with heart failure. Heart. 2017;103:255–257. doi: 10.1002/14651858.CD007228.pub3 [DOI] [PubMed] [Google Scholar]
- 7. Kenealy TW, Parsons MJ, Rouse AP, Doughty RN, Sheridan NF, Hindmarsh JK, Masson SC, Rea HH. Telecare for diabetes, CHF or COPD: effect on quality of life, hospital use and costs. A randomised controlled trial and qualitative evaluation. PLoS One. 2015;10:e0116188. doi: 10.1371/journal.pone.0116188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Takahashi EA, Schwamm LH, Adeoye OM, Alabi O, Jahangir E, Misra S, Still CH. An overview of telehealth in the management of cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2022;146:e558–e568. doi: 10.1161/CIR.0000000000001107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, Adusumalli S. Telemedicine outpatient cardiovascular care during the COVID‐19 pandemic: bridging or opening the digital divide? Circulation. 2020;142:510–512. doi: 10.1161/CIRCULATIONAHA.120.048185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, Snider C, Chokshi NP, Eneanya ND, Takvorian SU, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID‐19 pandemic. JAMA Netw Open. 2020;3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karimi M, Lee EC, Couture SJ, Gonzales A, Grigorescu V, Smith SR, De Lew N, Sommers BD. National Trends in Telehealth Use in 2021: Disparities in Utilization and Audio vs. Video Services. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2022. [Google Scholar]
- 12. Zachrison KS, Yan Z, Sequist T, Licurse A, Tan‐McGrory A, Erskine A, Schwamm LH. Patient characteristics associated with the successful transition to virtual care: lessons learned from the first million patients. J Telemed Telecare. 2023;29:621–631. doi: 10.1177/1357633X211015547 [DOI] [PubMed] [Google Scholar]
- 13. Osmanlliu E, Kalwani NM, Parameswaran V, Qureshi L, Dash R, Scheinker D, Rodriguez F. Sociodemographic disparities in the use of cardiovascular ambulatory care and telemedicine during the COVID‐19 pandemic. Am Heart J. 2023;263:169–176. doi: 10.1016/j.ahj.2023.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yuan N, Pevnick JM, Botting PG, Elad Y, Miller SJ, Cheng S, Ebinger JE. Patient use and clinical practice patterns of remote cardiology clinic visits in the era of COVID‐19. JAMA Netw Open. 2021;4:e214157. doi: 10.1001/jamanetworkopen.2021.4157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Singh A, Mountjoy N, McElroy D, Mittal S, Al Hemyari B, Coffey N, Miller K, Gaines K. Patient perspectives with telehealth visits in cardiology during COVID‐19: online patient survey study. JMIR Cardio. 2021;5:e25074. doi: 10.2196/25074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Institutes of Health . Health Information National Trends Survey. Accessed January 3, 2024. https://hints.cancer.gov/docs/Instruments/HINTS6‐AnnotatedEnglishInstrument.pdf.
- 17. World Health Organization . Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. World Health Organization; 2010. Accessed May 4, 2022. https://apps.who.int/iris/handle/10665/44497 [Google Scholar]
- 18. Westat . Health Information National Trends Survey 6 (HINTS 6) Methodology Report. Rockville, MD: Westat; 2023. Accessed December 27, 2024. https://hints.cancer.gov/docs/methodologyreports/HINTS_6_MethodologyReport.pdf [Google Scholar]
- 19. Lee JS, Lowe Beasley K, Schooley MW, Luo F. Trends and costs of US telehealth use among patients with cardiovascular disease before and during the COVID‐19 pandemic. J Am Heart Assoc. 2023;12:e028713. doi: 10.1161/JAHA.122.028713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khan MS, Kumar P, Sreenivasan J, Khan SU, Nasir K, Mehra MR, O'Donnell C, Warraich HJ. Rural‐urban differences in mortality from ischemic heart disease, heart failure, and stroke in the United States. Circ Cardiovasc Qual Outcomes. 2021;14:e007341. doi: 10.1161/CIRCOUTCOMES.120.007341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Loccoh EC, Joynt Maddox KE, Wang Y, Kazi DS, Yeh RW, Wadhera RK. Rural‐urban disparities in outcomes of myocardial infarction, heart failure, and stroke in the United States. J Am Coll Cardiol. 2022;79:267–279. doi: 10.1016/j.jacc.2021.10.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aneja S, Ross JS, Wang Y, Matsumoto M, Rodgers GP, Bernheim SM, Rathore SS, Krumholz HM. US cardiologist workforce from 1995 to 2007: modest growth, lasting geographic maldistribution especially in rural areas. Health Aff (Millwood). 2011;30:2301–2309. doi: 10.1377/hlthaff.2011.0255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yuan N, Botting PG, Elad Y, Miller SJ, Cheng S, Ebinger JE, Kittleson MM. Practice patterns and patient outcomes after widespread adoption of remote heart failure care. Circ Heart Fail. 2021;14:e008573. doi: 10.1161/CIRCHEARTFAILURE.121.008573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hughes HK, Hasselfeld BW, Greene JA. Health care access on the line—audio‐only visits and digitally inclusive care. N Engl J Med. 2022;387:1823–1826. doi: 10.1056/NEJMp2118292 [DOI] [PubMed] [Google Scholar]
- 25. Kuan PX, Chan WK, Fern Ying DK, Rahman MAA, Peariasamy KM, Lai NM, Mills NL, Anand A. Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta‐analysis. Lancet Digit Health. 2022;4:e676–e691. doi: 10.1016/S2589-7500(22)00124-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kruis R, Brown EA, Johnson J, Simpson KN, McElligott J, Harvey J. Patient perceptions of audio‐only versus video telehealth visits: a qualitative study among patients in an Academic Medical Center setting. Telemed Rep. 2024;5:89–98. doi: 10.1089/tmr.2023.0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ramaswamy A, Yu M, Drangsholt S, Ng E, Culligan PJ, Schlegel PN, Hu JC. Patient satisfaction with telemedicine during the COVID‐19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22:e20786. doi: 10.2196/20786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Masterson Creber R, Dodson JA, Bidwell J, Breathett K, Lyles C, Harmon Still C, Ooi SY, Yancy C, Kitsiou S; American Heart Association Cardiovascular Disease in Older Populations Committee of the Council on Clinical Cardiology and the Council on Cardiovascular and Stroke Nursing, Council on Quality of Care and Outcomes Research, Council on Peripheral Vascular Disease . Telehealth and health equity in older adults with heart failure: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2023;16:e000123. doi: 10.1161/HCQ.0000000000000123 [DOI] [PubMed] [Google Scholar]
- 29. Wosik J, Clowse MEB, Overton R, Adagarla B, Economou‐Zavlanos N, Cavalier J, Henao R, Piccini JP, Thomas L, Pencina MJ, et al. Impact of the COVID‐19 pandemic on patterns of outpatient cardiovascular care. Am Heart J. 2021;231:1–5. doi: 10.1016/j.ahj.2020.10.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3
Figure S1


