Abstract
Ovarian hemorrhage during antithrombotic therapy is sometimes difficult to manage. A 38-year-old woman, diagnosed with Marfan syndrome and implanted with a left ventricular assist device (LVAD) and taking aspirin and warfarin potassium, had a history of right adnexal oophorectomy via open surgery for a right ovarian hemorrhage at the age of 35 years. Thereafer, she had been treated with dienogest to suppress ovulation as much as possible. The patient was admitted to a local hospital with lower abdominal pain, and computed tomography showed a 10 cm left adnexal mass with suspected ovarian hemorrhage. Two days after the initiation of careful conservative treatment, with the cessation of antithrombotic therapy and monitoring of hemostasis, the patient was referred to a tertiary hospital. As the left ovarian hemorrhage continued 3 days after the transfer, emergency laparoscopic left salpingo-oophorectomy was performed due to the difficulty in conserving the left normal ovary. Although coagulopathy caused continuous oozing of blood from the pelvis after the removal of the left ovarian mass, hemostasis was successfully achieved laparoscopically. No postoperative bleeding was noted, and anticoagulant therapy was resumed on postoperative day 1 to prevent life-threatening thrombotic events associated with the LVAD. Postoperative pathological examination of the left ovary revealed an endometriotic cyst. To manage surgical menopause, complementary therapy using Japanese traditional herbal medicine was administered, as hormone replacement therapy was not recommended, to avoid the risk of fatal LVAD-associated thrombosis. Less invasive laparoscopic surgery for ovarian hemorrhage during anticoagulant therapy can be considered for reducing bleeding during and after surgery.
Keywords: Laparoscopic surgery, Ovarian hemorrhage, Implantable left ventricular assist device, Antithrombotic therapy, Dienogest, Case report
Highlights
-
•
Patients implanted with left ventricular assist device require antithrombotic drugs.
-
•
Women receiving anticoagulation occasionally occur major gynecologic bleeding.
-
•
Even under treatment with dienogest, hemorrhage from endometriotic cyst occurs.
-
•
Laparoscopic surgery for patients during antithrombotic therapy can be considered.
1. Introduction
Ovarian hemorrhage is common in women of reproductive age, with causes including functional cysts (follicular or corpus luteal cysts), ovulation-related events, and ovarian tumor (benign, borderline, and malignant) [1,2]. Although most physiological ovarian hemorrhages can be managed with conservative treatment, surgical treatment is sometimes required to control bleeding, especially in patients receiving antithrombotic therapy. In women on anticoagulation, corpus luteum hemorrhage can be fatal in 3–11 % of cases [3].
A left ventricular assist device (LVAD) is an electromechanical support for left cardiac pump function in severe heart failure [4]. Patients implanted with an LVAD require intensified antithrombotic therapy due to the high risk of blood clots forming in the device, which can lead to fatal events. Even during hemorrhagic events in patients with LVAD, continuing antithrombotic therapy, to some extent, is ideal, which makes surgical treatment, especially open surgery, difficult to manage [5]. Herein, we report a case of ovarian hemorrhage treated with laparoscopic surgery in a patient with LVAD implantation and coagulopathy on antithrombotic therapy.
2. Case Presentation
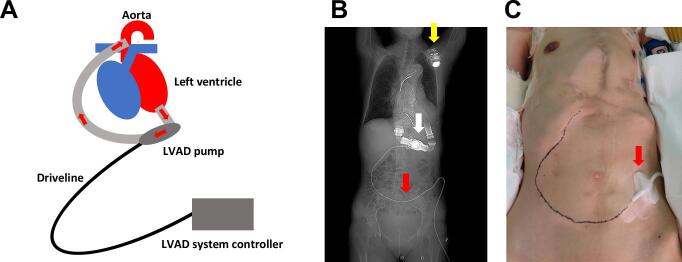
A 38-year-old woman was diagnosed with Marfan syndrome, dilated cardiomyopathy, and valvular heart disease at the age of 25 years. Thereafter, the patient underwent implantation of a cardioverter-defibrillator and five cardiovascular surgeries. At the age of 34 years, an LVAD (HeartMate II™, Thoratec Corporation, Pleasanton, CA, USA) was implanted due to worsening heart failure (Fig. 1A-C), and aspirin (100 mg per day) and warfarin potassium were started as intensified antithrombotic treatment. The dosage of warfarin potassium was adjusted to maintain a prothrombin time-international normalized ratio (PT-INR) between 2.0 and 3.0.
Fig. 1.
A. A schematic representation of the left ventricular assist device (LVAD). The LVAD pump draws blood from the left ventricle and delivers it to the ascending aorta. The battery-operated pump is connected to a driveline that runs subcutaneously, is inserted through the abdomen, and is connected to the LVAD system controller. B. A radiograph shows the implanted LVAD (white arrow), the driveline (red arrow), and cardioverter defibrillator (yellow arrow). C. The driveline (red arrow) of the LVAD is inserted through the left lower abdomen and runs subcutaneously to the LVAD. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
At the age of 35 years, the patient underwent right salpingo-oophorectomy via open surgery for right ovarian hemorrhage in the luteal phase [5]. At that time, her hemoglobin (Hb) level decreased to 4.6 g/dL, and her hemodynamic state was unstable; therefore, emergency open surgery (Pfannenstiel incision to spare the driveline component of the LVAD) was performed. The intraoperative blood loss and duration of surgery were 2970 mL and 1 h 20 min, respectively, and red blood cell transfusion was required. Persistent bleeding and hematoma formation around the skin incision necessitated compression treatment for 2 additional postoperative days. Following this, the patient was treated with dienogest (2 mg/day) to suppress ovulation.
The patient was admitted to a local hospital with lower abdominal pain, and computed tomography (CT) images showed a 10 cm left adnexal mass with suspected ovarian hemorrhage. The patient's Hb level, platelet count, PT-INR, and C-reactive protein (CRP) level were 10.4 g/dL, 124,000 cells/μL, 5.23, and 7.46 mg/dL, respectively. As PT-INR was elevated from the target range, conservative treatment was initiated, including cessation of aspirin and warfarin and administration of fresh frozen plasma, and hemostasis was closely monitored. Cardiovascular surgeons recommended maintaining PT-INR above 1.5 due to the risk of life-threatening LVAD-associated thrombosis. Two days post-admission, Hb level, PT-INR, and CRP level were 8.7 g/dL, 3.34, and 10.92 mg/dL, respectively.
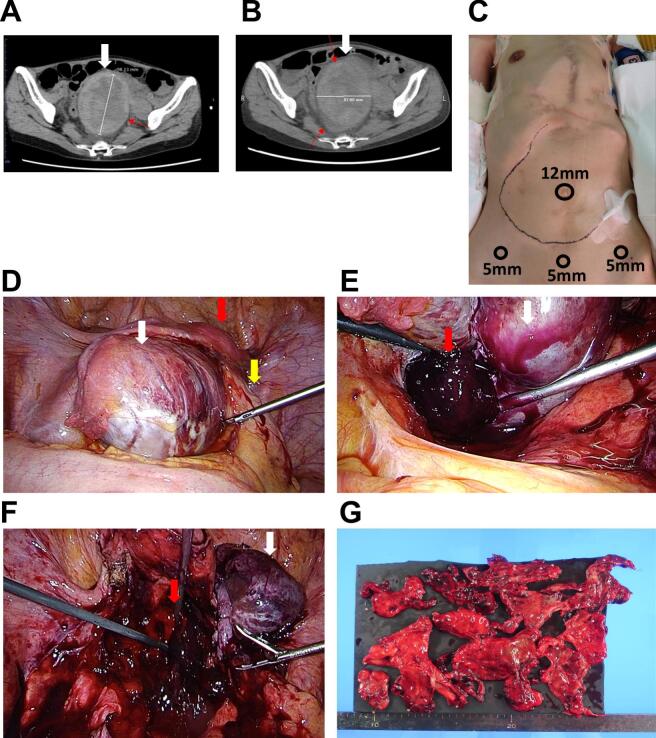
As her anemia gradually worsened and the left ovarian hematoma enlarged (Fig. 2A), the patient was referred to a tertiary hospital. Three days post-admission, despite transfusion of 1120 mL of red blood cells, Hb level, PT-INR, and CRP level were 10.4 g/dL, 1.95, and 18.10 mg/dL, respectively, indicating continued left ovarian hemorrhage and severe inflammation due to possible ovarian abscess. Follow-up CT revealed further enlargement of the left ovarian hemorrhage (Fig. 2B). The doctors determined that conservative treatment without antithrombotic therapy could not be continued, and emergency surgery was performed. Considering the difficulty in observing the deep pelvis and managing postoperative wound bleeding during coagulopathy in the previous open surgery for right ovarian hemorrhage [5], laparoscopic surgery with four-port incisions was performed to spare the driveline component of the LVAD (Fig. 2C).
Fig. 2.
A. A computed tomography (CT) image showing a 10 cm left ovarian hemorrhage (white arrow) at the time of admission to a tertiary hospital. B. A CT image showing an enlarged left ovarian hematoma (white arrow) 3 days after admission to a tertiary hospital. C. Four laparoscopic port incision sites (one 12 mm trocar on the umbilicus and three 5 mm trocars on the lower abdomen), avoiding the driveline component of the left ventricular assist device (LVAD). D. Laparoscopic view of newborn's head-sized left ovary (white arrow) in the pelvis and extensive adhesions involving the left and right pelvic peritoneum, uterus (red arrow), sigmoid colon, and rectum (yellow arrow). E. A large volume of blood clots (red arrow) from the ruptured left ovarian hematoma (red arrow). F. Oozing blood (red arrow) from the pelvis after the removal of left ovarian mass (white arrow). G. Macroscopic view of resected left adnexa mass. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Intraoperatively, a left ovarian mass the size of a newborn's head was found in the pelvis, with extensive adhesions involving the left and right pelvic peritoneum, uterus, sigmoid colon, and rectum (Fig. 2D). While the fragile left ovarian mass was carefully removed from the surrounding organs, the hematoma ruptured, releasing a large volume of blood clots without any abscess (Fig. 2E).
Due to the difficulty in controlling the left ovarian hemorrhage and preserving the normal ovary, a left salpingo-oophorectomy was performed. Despite intraperitoneal carbon dioxide pressure of 10–15 mmHg during laparoscopic surgery, coagulopathy led to continuous oozing of blood from the pelvis after the removal of the left ovarian mass (Fig. 2F). Human prothrombin complex (1000 units of Kcentra®, CSL Behring, King of Prussia, PA, USA) was intravenously administered to reverse the warfarin-induced coagulation disorder. Hemostasis was achieved through repeated surgical coagulation using bipolar forceps and oxidized regenerated cellulose (SURGICEL™ NU-KNIT™ Absorbable Hemostat; Ethicon Inc., Bridgewater, NJ, USA). Intraoperative blood loss was 590 mL, and the duration of surgery was 3 h 23 min. No red blood cell transfusion was required during or after the surgery.
The patient did not experience any postoperative complication, such as bleeding, and antithrombotic therapy using aspirin and warfarin potassium was resumed on postoperative day 1. The Hb level, PT-INR, and CRP level were 9.8 g/dL, 2.19, and 12.54 mg/dL, respectively, and the patient was transferred to a local hospital on postoperative day 9. Postoperative pathological examination of the left ovary revealed an endometriotic cyst without malignancy (Fig. 2G). Considering the risk of fatal LVAD-associated thrombosis, hormone replacement therapy for surgical menopause was not recommended. Instead, complementary and alternative treatments using Japanese traditional herbal medicines were initiated to relieve menopausal symptoms.
3. Discussion
This article reports a case of left ovarian hemorrhage treated with laparoscopic surgery in a patient with an implantable LVAD on antithrombotic therapy.
The mortality rate for most advanced heart failure with medical therapy alone remains high, ranging from 30 % to 80 % within the first year [4]. LVAD contributes to an improved prognosis, and the mean survival following LVAD implantation is approximately 5 years [4]. Complications associated with LVAD and antithrombotic therapy include bleeding, infection, pump thrombosis, and stroke [4]. In this case, left ovarian hemorrhage spontaneously occurred with severe coagulopathy (PT-INR, 5.23), even though the patient was routinely being administered the prescribed amount of warfarin potassium daily. This event indicates the fluctuation and challenges in managing intensified antithrombotic therapy with warfarin potassium [6,7]. In women receiving antithrombotic therapy, the likelihood of a severe gynecological event, particularly involving the uterus and ovary, is high. Long-term anticoagulation is associated with an increased risk of hemorrhage, with an annual risk of major bleeding ranging from 1.1 % to 7.5 % [3]. In women on anticoagulation, corpus luteum hemorrhage can be fatal in 3–11 % of cases and may recur in approximately 25–31 % of patients [3]. The risk of hemorrhage escalates with PT-INR of 3.0 or more and becomes much more substantial when PT-INR exceeds 4.5 [3]. Considering these risks, as the patient had already undergone right salpingo-oophorectomy due to right ovarian hemorrhage caused by a suspected ruptured functional cyst in the luteal phase [5], dienogest, which is also used for endometriosis treatment, was administered to suppress ovulation and the menstrual cycle. Dienogest (≥2 mg daily) has been shown to moderately suppress estradiol production and reliably inhibit ovulation, which reverses rapidly after treatment cessation [8]. However, in the present case, the pathological examination of the resected left ovary revealed an endometriotic cyst without malignancy despite the assumption that ovulation was suppressed. The hemorrhage from the endometriotic cyst in the left ovary was not preventable due to severe coagulopathy.
Laparoscopic and robot-assisted laparoscopic surgeries have gained widespread popularity across surgical departments. A systematic review of 185 articles reported that, compared with open surgery, laparoscopic surgery offers several advantages, including minimized trauma to the abdominal wall, less blood loss, faster recovery, shorter hospital stay, quicker return to normal activities, a lower rate of wound infections, and lower perioperative morbidity in appendectomy, cholecystectomy, esophageal surgery, gastric surgery, colorectal surgery, liver surgery, and pancreatic surgery [9]. In gynecology, minimally invasive surgery has demonstrated similar benefits to laparotomy, including reduced blood loss [10]. For patients receiving antithrombotic treatment, laparoscopic surgery in the digestive system has also shown satisfactory results in preventing bleeding and thromboembolic events [11]. In this case, despite the differences in circumstances between both surgeries, open surgery for the right ovarian hemorrhage at the age of 35 years resulted in massive blood loss (2970 mL), a requirement for transfusion, and postoperative bleeding and hematoma [4]. Conversely, the laparoscopic approach for the left ovarian hemorrhage at the age of 38 years resulted in significantly less blood loss (590 mL), no requirement for transfusion, and no postoperative complications. Although achieving hemostasis under antithrombotic therapy is difficult, laparoscopic surgery can be considered a viable option for patients with coagulopathy when the patient's condition, hemodynamic status, tolerance for pneumoperitoneum, and the Trendelenburg position for lung and heart are favorable.
4. Conclusion
Less invasive laparoscopic surgery for managing ovarian hemorrhage during anticoagulant therapy could be considered to reduce bleeding during and after surgery as well as other complications.
pneumoperitoneum, and the Trendelenburg position for lung and heart are favorable.
5. Conclusion
Less invasive laparoscopic surgery for managing ovarian hemorrhage during anticoagulant therapy could be considered to reduce bleeding during and after surgery as well as other complications.
Acknowledgments
Contributors
Yasuto Kinose contributed to patient care, conception of the case report, acquisition and interpretation of data, drafting of the manuscript, literature review, and critical revision of the article for important intellectual content.
Aasa Shimizu, Mamoru Kakuda, Satoshi Nakagawa, Tsuyoshi Takiuchi, Tadashi Iwamiya, Michiko Kodama critically contributed to the revision of this article for important intellectual content.
Eiji Kobayashi contributed to patient care, and acquired and interpreted the data.
Yutaka Ueda, Kenjiro Sawada, and Tadashi Kimura critically contributed to the revision of this article for important intellectual content.
All authors approved the final submitted manuscript.
Funding
The authors received no funding from any external source to support the publication of this case report.
Patient consent
Written informed consent for publication was obtained from the patient.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Acknowledgments
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Bottomley C., Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract. Res. Clin. Obstet. Gynaecol. 2009;23(5):711–724. doi: 10.1016/j.bpobgyn.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Medvediev M.V., Malvasi A., Gustapane S., Tinelli A. Hemorrhagic corpus luteum: clinical management update. Turk. J. Obstet. Gynecol. 2020;17(4):300–309. doi: 10.4274/tjod.galenos.2020.40359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A., Gupta S., Manaktala U., Gupta M.M., Solanki V. Conservative management of corpus luteum haemorrhage in patients on anticoagulation: a report of three cases and review of literature. Arch. Gynecol. Obstet. 2015;291(2):427–431. doi: 10.1007/s00404-014-3394-2. [DOI] [PubMed] [Google Scholar]
- 4.Miller L.W., Rogers J.G. Evolution of left ventricular assist device therapy for advanced heart failure: a review. JAMA Cardiol. 2018;3(7):650–658. doi: 10.1001/jamacardio.2018.0522. [DOI] [PubMed] [Google Scholar]
- 5.Aya N., Michiko K., Eiji K., Kae H., Yuji T., Tadashi K. Benefits of laparoscopic surgery for bleeding events in patients with implantable left ventricular assist devices during antithrombotic therapy. Gynecol. Minim. Invasive Ther. 2022;11(2):110–113. doi: 10.4103/GMIT.GMIT_35_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cropp J.S., Bussey H.I. A review of enzyme induction of warfarin metabolism with recommendations for patient management. Pharmacotherapy. 1997;17(5):917–928. doi: 10.1002/j.1875-9114.1997.tb03782.x. [DOI] [PubMed] [Google Scholar]
- 7.Wells P.S., Holbrook A.M., Crowther N.R., Hirsh J. Interactions of warfarin with drugs and food. Ann. Intern. Med. 1994;121(9):676–683. doi: 10.7326/0003-4819-121-9-199411010-00009. [DOI] [PubMed] [Google Scholar]
- 8.Klipping C., Duijkers I., Remmers A., Faustmann T., Zurth C., Klein S., et al. Ovulation-inhibiting effects of dienogest in a randomized, dose-controlled pharmacodynamic trial of healthy women. J. Clin. Pharmacol. 2012;52(11):1704–1713. doi: 10.1177/0091270011423664. [DOI] [PubMed] [Google Scholar]
- 9.Buia A., Stockhausen F., Hanisch E. Laparoscopic surgery: a qualified systematic review. World J. Methodol. 2015;5(4):238–254. doi: 10.5662/wjm.v5.i4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levy L., Tsaltas J. Recent advances in benign gynecological laparoscopic surgery. Fac. Rev. 2021;10 doi: 10.12703/r/10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujikawa T., Ando K. Safety of laparoscopic surgery in digestive diseases with special reference to antithrombotic therapy: a systematic review of the literature. World J. Clin. Cases. 2018;6(14):767–775. doi: 10.12998/wjcc.v6.i14.767. [DOI] [PMC free article] [PubMed] [Google Scholar]