Abstract
This case report discusses a compelling case involving acrania, exencephaly, and spinal myeloschisis in a 22-year-old pregnant woman from rural Nepal. The delayed diagnosis due to limited healthcare access underscores the importance of early prenatal care and screening. The case sheds light on the complexity of congenital anomalies and their implications. Acrania with exencephaly is a severe cranial neural tube defect that results from the failure of neural tube closure during embryogenesis. Exencephaly on the other hand is the absence of the cranial vault with exposed brain tissue. The study emphasizes the significance of maternal nutrition, folic acid supplementation, and genetic risk assessment in preventing such conditions. This report contributes to raising awareness and improving management strategies for intricate congenital abnormalities, ultimately enhancing maternal and fetal well-being
Keywords: Acrania, Exencephaly, Myeloschisis, Prenatal care, Folic acid supplementation
Introduction
Acrania with exencephaly is a severe cranial neural tube defect that results from the failure of neural tube closure during embryogenesis. The incidence rate of NTD is 1 in every 1000 live births [1]. Exencephaly is characterized by the absence of the cranial vault with exposed brain tissue, while anencephaly refers to the absence of the brain, skull, and scalp. These conditions are part of a spectrum of cranial defects, including acrania and encephalocele. The global burden of disease associated with neural tube defects varies, with Southeast Asia having the highest prevalence rate. These birth defects can vary in severity and pose significant risks of mortality and morbidity [2].
While acrania is not typically detectable on ultrasound until around 12 weeks of gestation when the fetal cranial vault begins to ossify, serial ultrasound scans have demonstrated a progression from exencephaly to anencephaly [3]. Exencephaly is associated with various system anomalies, such as the rachischisis of the whole or part of the spine due to defective induction by the notochord [4].
This article aims to present a rare case of acrania with exencephaly and spinal myeloschisis and discuss the clinical significance, management, and prevention of such congenital anomalies.
Case presentation
A 22-year-old woman from a rural area in Nepal visited the Gynecology outpatient department of a tertiary care center, presenting with a 6-month absence of menstrual periods, lower abdominal pain, and reduced fetal movement for the past week. She had not been taking any iron or calcium supplements. The pregnancy was confirmed through a urine pregnancy test at home, 2 months after the onset of amenorrhea. This was her first pregnancy, and due to concerns about reduced fetal movement, she was advised to seek medical attention. Subsequently, she was referred to our institution. She had not undergone any previous antenatal checkups, and there was no family history of hereditary diseases, congenital abnormalities, or pregnancy complications. She did not smoke, consume alcohol, and followed a vegetarian diet. She incorporates dairy products, fruits, and green leafy vegetables into her diet, but she refrains from consuming any meat products or eggs. There was no prior diagnosis of chronic illnesses such as hypertension, diabetes mellitus, or thyroid disorder.
Upon examination, the patient was alert and oriented to time, place, and person. Her pulse rate was 62 beats per minute, and her blood pressure was 110/80 mmHg. The measurement of her fundal height corresponded to 24 weeks of gestation with a cephalic presentation. She experienced abdominal pain along with moderate contractions, but fetal heart sounds could not be detected. A vaginal examination revealed a mildly dilated external-os measuring 3 cm, minimal show, and intact membranes. An ultrasound examination was performed, which revealed the absence of the cranial vault above the orbits. The brain tissue was covered by a membrane and was observed to be herniated posteriorly, floating in the amniotic fluid (Fig. 1). There was no cardiac activity, and the color and spectral Doppler study of the middle cerebral artery showed no blood flow.
Fig. 1.
Axial grayscale ultrasound image showing the herniated brain tissue (indicated by the green arrow) through the calvarial defect covered with membranes (indicated by the white arrow).
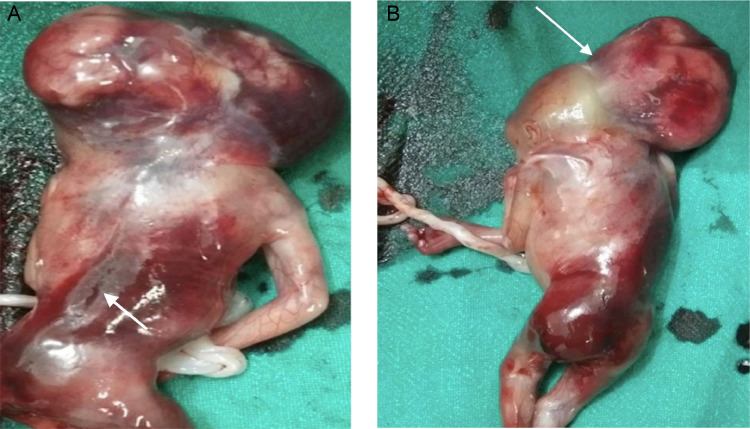
All laboratory investigations, including beta-human chorionic gonadotropin (β -HCG), yielded normal results. Following the induction of labor using vaginal misoprostol, a stillborn female fetus weighing approximately 850 grams was delivered. Placenta was normal weighing about 400gm. The APGAR scores at 1 and 5 minutes were zero. The abortus exhibited the absence of the cranial vault with herniation of brain tissue (covered by a membrane) posteriorly. Additionally, a large defect involving the skin and vertebrae at the level of the lumbar spine was observed (Figs. 2A and B), which was not identified during the ultrasound examination. The defect in the lumbar spine measured about 1.9 × 1.3 cm. The umbilical cord displayed 2 arteries and 1 vein. An autopsy examination of the fetus was not performed due to the patient's refusal to grant permission. Consequently, a diagnosis of acrania with exencephaly and spinal myeloschisis was made, which carried a poor prognosis for the fetus.
Fig. 2.
(A) Gross specimen of an aborted fetus showing the herniated brain tissue with the absence of the calvarium and a defect in the lumbar spine region (indicated by the white arrow). (B) Gross specimen of an aborted fetus showing the herniating brain parenchyma covered by membrane (indicated by the white arrow) as well as a defect in the lumbar spinal region.
After delivery, the patient received intravenous administration of Oxytocin 10 units, ceftriaxone 1 gram, and metronidazole 500 milligrams. The patient received a suggestion to consult with an obstetrician if she intended to conceive soon. Additionally, she was guided by preconception care, encompassing aspects such as physical recuperation, emotional welfare, contraception, nutritional intake, supplements, and health evaluations. She was discharged from the hospital a day after admission with directives for consistent follow-up appointments. At her subsequent visit a month later, she communicated her well-being and progress. She underwent counseling concerning the incorporation of folic acid through dietary supplementation and was swiftly initiated on a folate regimen.
Discussions
Neural tube defects are the most common congenital anomalies of the central nervous system, resulting from the incomplete closure of the neural tube during embryonic development [5]. Exencephaly is a rare malformation characterized by the absence of the skull or scalp, with the brain tissue protruding outside into the amniotic cavity. Over time, the herniated brain tissue degenerates, leading to anencephaly [3]. Exencephaly is often associated with other structural abnormalities and carries a poor prognosis, primarily affecting females [6]. In this specific study, a female patient presented with exencephaly, accompanied by spinal myeloschisis in the lumbar region. Ultrasound is a valuable tool for detecting congenital defects and fetal deformities, allowing for early identification of conditions such as acrania [7]. Acrania is a rare congenital anomaly that is characterized by a partial or complete absence of the cranium. It starts with the closure of the anterior neuropore after 4th week of gestation, leading to no development of the calvarial bones of the skull, related underlying musculature, and dura mater [8].
Genetic risk factors for the development of neural tube defects include maternal folic acid deficiency and gene alterations related to folic acid metabolism. Environmental factors such as age, periconceptional infection, recreational drug use, caffeine, smoking, and alcohol influence the genesis of NTDs. Poor maternal nutrition, micronutrients like vitamin B6, B12, and minerals like zinc are important for proper development of the neural tube [9]. Due to her low education and limited access to healthcare, she sought medical attention late. Additionally, she had not taken folic acid either before or after conception.
The raised level of alpha-fetoprotein (AFP) in the amniotic fluid or serum is a nonspecific reliable indicator of open neural tube defects before 26 weeks [10]. Although she did not undergo it, combining the measurement of AFP levels with an ultrasound anomaly scan assists in the early identification process.
The rare association of acrania with exencephaly and myeloschisis in our study highlights its utmost importance. Given its noncurable nature and poor prognosis, early management plays a crucial role in dealing with the condition. Folate supplementation, along with early diagnosis through ultrasound and AFP testing becomes of pivotal value in preventing and managing the condition effectively.
Conclusion
This case report presents a rare occurrence of acrania with exencephaly and myeloschisis in a young pregnant woman from rural Nepal. The clinical and imaging findings highlight the seriousness and intricacy of these congenital abnormalities, emphasizing the significance of early detection through ultrasound and prenatal care. The case also underscores the importance of thorough counseling, folic acid supplementation, and evaluation of genetic risk factors to prevent neural tube defects. Further research and greater awareness are essential in improving the management and prognosis of these uncommon congenital conditions.
Ethical approval
The study is exempt from ethical approval in our institution.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Patient consent
Written informed consent was obtained from the patient's biological mother for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: None available.
References
- 1.Copp AJ, Stanier P, Greene NDE. Neural tube defects: recent advances, unsolved questions, and controversies. Lancet Neurol. 2013;12(8):799–810. doi: 10.1016/S1474-4422(13)70110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blencowe H, Kancherla V, Moorthie S, Darlison MW, Modell B. Estimates of global and regional prevalence of neural tube defects for 2015: a systematic analysis. Ann N Y Acad Sci. 2018;1414(1):31–46. doi: 10.1111/nyas.13548. [DOI] [PubMed] [Google Scholar]
- 3.Beinder E, Grüner C, Erhardt I, Mauch E, Begon S. The exencephaly-anencephaly sequence. Ultrasound diagnosis in early pregnancy. Ultraschall Med Stuttg Ger 1980. 1995;16(4):192–195. doi: 10.1055/s-2007-1003937. [DOI] [PubMed] [Google Scholar]
- 4.Langman's medical embryology. - NLM Catalog - NCBI [accessed 17.06.23]. Available from: https://www.ncbi.nlm.nih.gov/nlmcatalog/101562744
- 5.Hadžagić-Ćatibušić F, Maksić H, Užičanin S, Heljić S, Zubčević S, Merhemić Z, et al. Congenital malformations of the central nervous system: clinical approach. Bosn J Basic Med Sci. 2008;8(4):356–360. doi: 10.17305/bjbms.2008.2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prashanth R, Shenoy S, Ks R, Vs R, Ss H. Anencephaly with cervical rachischisis (craniorachischisis) and congenital bronchogenic cyst : an autopsy case report of a rare association. 2014 [accessed 18.06.23]. Available from: https://www.semanticscholar.org/paper/Anencephaly-with-Cervical-Rachischisis-and-Cyst-/3A-a-Prashanth-Shenoy/d5cb9819761624a9c211b6ed6cf933fb6f612a77
- 7.Karim JN, Roberts NW, Salomon LJ, Papageorghiou AT. Systematic review of first-trimester ultrasound screening for detection of fetal structural anomalies and factors that affect screening performance. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2017;50(4):429–441. doi: 10.1002/uog.17246. [DOI] [PubMed] [Google Scholar]
- 8.Peer D, Moroder W, Delucca A. Prenatal diagnosis of the pentalogy of Cantrell combined with exencephaly and amniotic band syndrome. Ultraschall Med Stuttg Ger 1980. 1993;14(2):94–95. doi: 10.1055/s-2007-1005224. [DOI] [PubMed] [Google Scholar]
- 9.Kotrannavar SS, Kotrannavar VS. Anencephalic fetus with craniospinal rachischisis - Case report. IP Indian J Anat Surg Head Neck Brain. 2020;5(4):124–126. [Google Scholar]
- 10.Weiss RR, Macri JN, Elligers K, Princler GL, McIntire R, Waldman TA. Amniotic fluid alpha-fetoprotein as a marker in prenatal diagnosis of neural tube defects. Obstet Gynecol. 1976;47(2):148–151. [PubMed] [Google Scholar]