Abstract
Introduction
‘Neurophobia’ is a well reported phenomenon in the literature where in medical students and junior doctors have an inherent nervousness or ‘fear’ of neurology and neurosurgery.
Research question
Why do less medical students choose neurology and neurosurgery as a career and identify if neurophobia is an ingrained belief or learned behaviour?
Materials and methods
We developed a questionnaire to assess medical student views and beliefs in connection with a career in neurosurgery. Specifically we examined the following domains: considering a career in neurology and neurosurgery, confidence with neuro anatomy and pathology, traits associated with neurosurgeons and neurologists and finally, their perceived barriers to a neuro career.
Results
264 medical students completed the survey. Students from fourteen different medical schools across the world responded, with the highest number of students being from Irish medical schools. Over half of participants (58%) felt that neurology is an intimidating module and/or career choice while a huge 80% felt neurosurgery was an intimidating choice.
We believe our research appears to be the first to open the survey to students across the world, with no limitations placed on region.
Discussion and conclusion
Neurophobia is not limited to any one geographical region, age group or gender. It appears to be mainly be driven by an intimidation of the complex nature of neuroanatomy and neuropathology. This negative perspective can be further enhanced when students go on to have a negative experience on clinical attachments.
Keywords: Neurophobia, Neurosurgery, Neurology, Education, Medical students, Teaching
Highlights
-
•
‘Neurophobia’ is when medical students have a fear of neurology and neurosurgery.
-
•
We developed a questionnaire to assess student views and beliefs.
-
•
264 medical students completed the survey.
-
•
Work life balance and competitive training path were perceived barriers.
-
•
Students advocated for increased teaching through placements or lectures.
1. Background
‘Neurophobia’ is a well-reported phenomenon in the literature, wherein medical students and junior doctors exhibit an inherent nervousness or ‘fear’ of neurology and neurosurgery (Abulaban et al., 2015). Neurophobia can be attributed to several factors, primarily the complexity of neurological and neurosurgical patients, as well as the intricate—and to a large extent, unknown—functional anatomy and physiology of the nervous system. Mastering this complex anatomy and physiology requires significant effort and time, and it is undoubtedly a source of anxiety for both medical students and doctors alike(Hill et al., 2010). Additionally, neurosurgeons are sometimes perceived as having challenging personalities, ranging from odd behavior to full-blown narcissistic traits (Greenblatt, 1991). Social media, including films, has played a major role in projecting these images (Garzali, 2022).
An estimated 22.6 million people require neurological care globally, with an estimated 13.8 million needing surgical intervention (Dewan et al., 2019). There is no question that the demand for neurologists and neurosurgeons will continue to grow. In the developed world, a ratio of 1 neurosurgeon per 80,000 patients is generally considered acceptable. In some parts of the world, however, this ratio can be as extreme as 1 neurosurgeon per 10 million patients (El Khamlichi, 2005). This care deficit is most acute in lower- and middle-income countries, which face significant challenges in recruiting and retaining doctors, particularly within surgical subspecialties, given the extensive and costly training required to practice these disciplines.
Our study aimed to survey a wide variety of medical students from different countries, socio-economic backgrounds, cultural beliefs, and medical schools to uncover the underlying reasons why medical students and junior doctors refrain from choosing neurological specialties as career options. Additionally, we sought to understand what conditions might encourage students to consider neurology and neurosurgery as career paths.
2. Methods
We assembled a group of medical students from five medical schools in the Republic of Ireland and developed a questionnaire to assess their views and beliefs regarding a career in neurosurgery. Specifically, we examined their perspectives in the following domains: considering a career in neurology, understanding and confidence with neuroanatomy and pathology, perception of neurosurgeons and neurologists, and perceived barriers to pursuing a career in a neurological specialty. Our aim was to elucidate their views, expectations, and concerns, as well as their spontaneous first thoughts when presented with the mental image of a neurologist or neurosurgeon, to identify what might help reduce anxiety in the context of diagnosing, treating, and managing neurological patients. We felt qualitative analysis represented an important means of understanding medical student perspectives on this topic.
The survey used to assess students' perceptions of neurophobia was developed using an online survey platform, following a rigorous process to ensure content validity. Initially, a comprehensive literature review on neurophobia and related educational challenges was conducted to identify key themes. Based on this, a preliminary questionnaire was formulated. To further refine the instrument, the survey was reviewed by a panel of experts, including experienced neurosurgeons and medical educators. Their feedback was incorporated to improve the questionnaire's accuracy and align it with the current understanding of neurophobia in medical education. This multi-step process ensured that the survey was both grounded in existing research and subject to review by domain specialists, enhancing its content validity.
Medical student volunteers were asked to share the survey with interested peers, doing so via various social media platforms. The survey consisted of an online form, with a mix of structured multiple-choice questions and free-text boxes. Responses were collected anonymously, and no identifying data were used or retained.
3. Results
A total of 264 medical students completed the survey. Of these, 161 (60.9%) identified as female, 102 (38.6%) as male, and one respondent (0.38%) identified as non-binary. The age of the respondents ranged from 18 to 33 years. Students from fourteen different medical schools worldwide participated, though the majority attended Irish medical schools. The year of study was distributed across all levels, from those who had just completed their first year to those who had recently graduated but had not yet begun working.
Notably, the vast majority of participants (82.2%) had entered medicine through a direct entry route, straight on from secondary education. In contrast, 13.26% had obtained a previous degree, and 4.54% had entered as mature students or via an alternative pathway. Table 1 displays the demographics of the survey respondents.
Table 1.
Table showing demographics of survey participants.
| Gender | |
| Female | 60.98% (n = 161) |
| Male | 38.64 % (n = 102) |
| Non-binary | 0.38% (n = 1) |
| Age | |
| 18–24 | 89.01% (n = 235) |
| 25–34 | 10.62% (n = 28) |
| Medical School Country | |
| Ireland | 74.24% (n = 196) |
| Bahrain | 20.46% (n = 54) |
| Egypt | 0.38% (n = 1) |
| Germany | 0.38% (n = 1) |
| Georgia | 0.38%(n = 1) |
| Oman | 1.89%(n = 5) |
| United Kingdom | 1.89% (n = 5) |
| USA | 0.38% (n = 1) |
| Year of Study | |
| Year 1 | 24.61% (n = 65) |
| Year 2 | 10.23% (n = 27) |
| Year 3 | 19.7% (n = 52) |
| Year 4 | 23.11% (n = 61) |
| Year 5 | 13.26% (n = 35) |
| Year 6 | 2.27% (n = 6) |
| Graduated this year | 6.82% (n = 18) |
| Route of Entry | |
| Direct School Entry | 82.2% (n = 217) |
| Graduate Entry Pathway | 12.36% (n = 35) |
| Mature Student/Alternative Pathway | 4.54% (n = 12) |
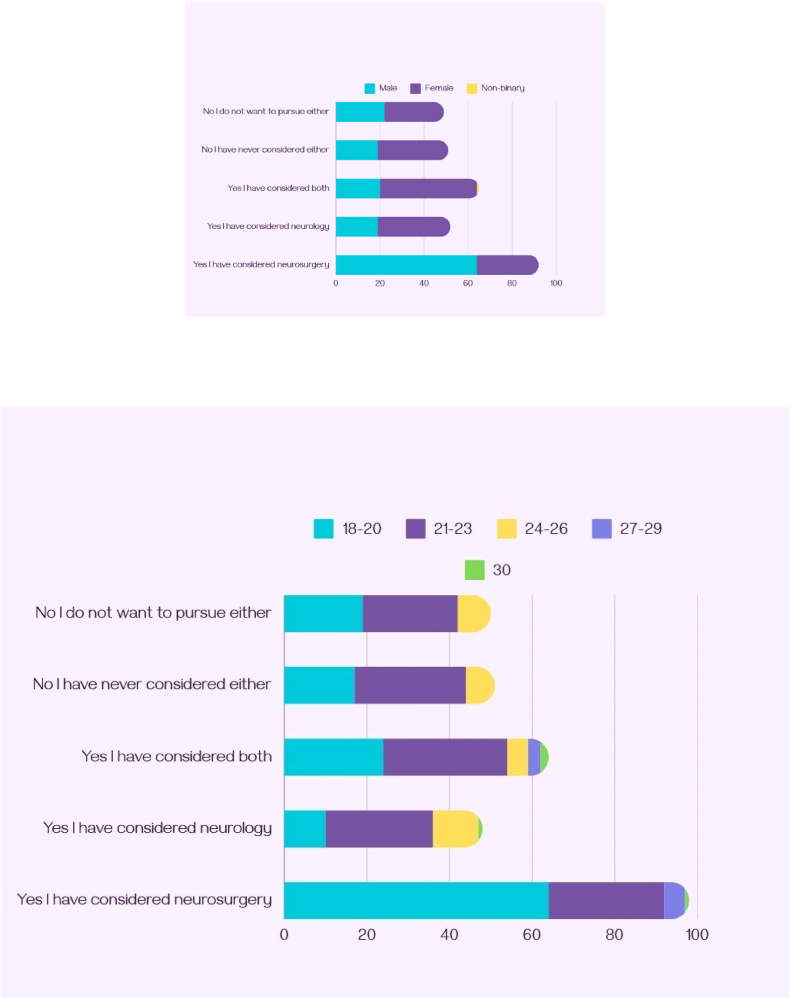
Over half of the participants (58%) felt that neurology is an intimidating module and/or career choice, while an overwhelming 80% viewed neurosurgery as intimidating. Fig. 1 breaks down these responses by age and gender. When asked if they had ever considered neurology or neurosurgery as a career choice, 62% of participants had, at some point, considered a career in neurology, neurosurgery, or both, while 38% said they had never considered it or were uninterested.
Fig. 1.
Graphs showing response to considering neurology and neurosurgery as a career, broken down by gender and age.
The next section asked participants how comfortable they felt conducting neurological physical exams, including a cranial nerve exam and a sensory and motor exam.
A total of 65% of participants felt comfortable or ‘somewhat comfortable’ in their ability to perform an upper or lower limb neurological assessment, while over a quarter (26%) felt either ‘somewhat’ or ‘completely’ unprepared. Only 11.7% described themselves as confident in performing the same exam. For the cranial nerve exam, just 44% of participants felt confident or comfortable, while 21% considered themselves “somewhat prepared,” and 35% felt somewhat or totally unprepared. As expected, comfort levels were higher among more senior medical students, though no group—including recent graduates—felt completely comfortable performing any exam. A further breakdown of student comfort with performing neurological exams is presented in Fig. 2.
Fig. 2.
Graphs demonstrating reported comfort levels with neurological exams by age and gender.
When asked if they felt confident identifying the location of a lesion or the underlying pathology following a clinical exam, only 10% (n = 27) of participants felt they could. Meanwhile, 48% (n = 126) felt they might be able to, and 42% (n = 112) believed they could not.
Our ordinal regression analysis examined how age and gender influence medical students’ comfort levels with performing neurological exams. Age was found to have a positive and highly significant effect (estimate = 0.35, p < 0.001), indicating that older students are more likely to feel comfortable or confident performing these exams. This is likely due to students advancing in their medical education and gaining more experience with exams, rather than being directly related to age. No significant differences were found between female and male participants (p = 0.9192), suggesting that comfort levels are similar across gender groups.
Participants were then given a free-text box and asked what words they associated with ‘neurologist.’ Responses were categorized into pathology or anatomy-based terms, perceived personality traits, references to training, impressions of neurology as a career, and other. Word associations were then analyzed according to gender, age, and academic year. A total of 64% of females provided responses related to neurological pathology, compared to 36% of males. The most common anatomical and pathological terms mentioned were ‘stroke,’ ‘brain,’ ‘nerves,’ and ‘palsies.’ In terms of personality traits, ‘smart’ was suggested by 43% of respondents, while ‘intelligent’ was suggested by 26%. Other common descriptors for neurologists included ‘hard-working’ (13%) and ‘detail-oriented’ (25%).
The next question was also a free-text box, this time asking participants for words they associate with ‘neurosurgeon.’ As before, these responses were grouped into categories: anatomical or pathological terms, personality traits, impressions of the career, and other. In comparison with neurologists, there was a stronger tendency for responders to comment on personality traits in relation to neurosurgeons, with remarks being a mixture of positive and negative.
Positive attributes accounted for 40.1% of responses (n = 108), with females making 59.3% (n = 64) of these comments and males the remaining 40.7% (n = 44). Neurosurgeons were repeatedly described as highly intelligent and skilled, reflecting the complex nature of their work. Words like “smart,” “genius,” “brilliant,” “bright,” and “talented” emphasized the perceived cognitive abilities required of neurosurgical specialists. Other frequently referenced terms included “precision” and “meticulous” (42%), emphasizing the technical skill associated with the profession.
Negative personality traits accounted for 8.3% of responses (n = 22). In terms of gender distribution, 68.2% of respondents who referenced negative attributes were female. There was also a divide based on year of study, with senior students or graduates being more likely to mention negative personality traits. First-, second-, and third-year students accounted for 36.4% (n = 8) of these responses, while those in fourth or fifth year or who had graduated accounted for 63.6% (n = 14).
Fig. 3 displays two word clouds, representing the most frequently mentioned words for neurologists and neurosurgeons. The overarching theme from both word clouds is that neurologists and neurosurgeons are perceived as intelligent and somewhat intimidating to students.
Fig. 3.
Word clouds showing words associated with ‘neurologist’ (3a) and ‘neurosurgeon’ (3b).
Participants were then asked about perceived barriers to pursuing a career in neurology or neurosurgery. For neurology, the most commonly referenced barrier (34%) was the difficulty and complexity of the specialty. The second most common barrier (20%) was a perceived lack of clinical exposure to neurology. Other reasons included a competitive training path (14%), poor teaching or curriculum issues (12%), lack of interest in the subject (8%), and negative stereotypes or perceptions of the specialty (7%).
Regarding neurosurgery, the primary barrier identified was the long hours and lack of work-life balance (20%), followed closely by the long, competitive training path (19.6%). Other barriers included a lack of clinical exposure (14%) and high-risk nature of the work (7.5%). A small minority of participants (3%) mentioned the gender imbalance as a deterrent.
Finally, participants were asked what medical schools could do to improve student attitudes toward neurology and neurosurgery. An overwhelming majority (87%) suggested offering more experience in these fields through clinical attachments and observerships. A total of 55% of participants felt that increasing surgical and medical exposure, particularly through real-life patient interactions in neurological or neurosurgical placements, would make these specialties more accessible. This was another free-text response, with many students advocating for a mandatory neurological or neurosurgical placement. Additionally, three students suggested that these placements should include an attached exam, similar to placements in obstetrics or pediatrics.
4. Discussion
Multiple studies have identified the complex nature of neuroanatomy and neurological pathology as the primary reasons many students and junior doctors develop neurophobia (Han et al., 2023; Jukna et al., 2023; McCarron, 2012; Tadeu et al., 2014). This appears to be a widespread problem, as our research did not identify any specific geographical location where students and new graduates felt more comfortable with neurology than in other regions. Of note, we believe our research is the first to open the survey to students globally, without limiting which students could respond. However, one limitation of this study is the overrepresentation of Irish students (74.24%) in the respondent pool. While the survey was open to medical students worldwide, most responses came from Irish participants, potentially introducing geographical and cultural biases. This imbalance could limit the generalizability of the findings, as medical education structures, clinical exposure, and experiences with neurology may differ across countries and institutions. Consequently, the perspectives captured in the survey predominantly reflect the experiences of Irish students, and potentially overlook diverse international viewpoints on neurophobia. Future studies should aim for a more balanced representation to enhance the global relevance of the findings.
A second limitation of this research is that it primarily focused on assessing students' attitudes toward neurology and neurosurgery, without comparing these perceptions to their views on other modules. In future research, we will incorporate a comparative framework, providing a more comprehensive view of students’ educational experiences and their impact on specialty choice.
There did not appear to be any significant gender differences in how males and females reported difficulties with neurological topics. However, male students were more likely to describe themselves as ‘confident’ with cranial nerve exams, while female students more often described themselves as feeling ‘comfortable.’ Previous reports suggest that male medical students tend to express more confidence in their abilities than female students, despite no significant discrepancy in academic performance (Blanch et al., 2008), which may tie into the ‘imposter syndrome’ frequently reported by female medical students and trainees (Clance and Imes, 1978).
As expected, younger students felt less confident with their ability to perform clinical exams and diagnose neurological conditions. However, the majority of respondents, including more senior students, still reported feeling unprepared.
The free-text responses asking students for words associated with ‘neurologist’ or ‘neurosurgeon’ highlighted internal biases and stereotypes that many students hold toward these specialties, particularly among those with less clinical exposure. There were fewer negative traits associated with neurosurgery compared to positive ones, however, negative traits were more commonly reported by senior medical students, suggesting that these opinions may be influenced by clinical experiences. Negative experiences with clinicians can significantly impact medical students, potentially leading them to dismiss an entire specialty based on interactions with one or two individuals. Previous research has shown that when medical teams fail to acknowledge a student's presence, it can undermine the student's confidence and cause them to distance themselves not only from a specialty, but also the placement itself (Valestrand et al., 2024), creating a negative feedback loop whereby students miss out on valuable teaching experiences.
Positive traits—such as ‘intelligent’ and ‘high functioning’—can also serve as barriers to engagement with certain specialties, as students who lack confidence may feel less capable of working in these areas. A 2021 study found that more than one-fifth of medical students struggle with low self-esteem (Shrestha et al., 2021).
When asked how neurophobia could be reduced among medical students, the vast majority advocated for increased teaching—whether through placements, or formal didactic lectures and tutorials. This indicates that interest for neurology exists across all stages of medical training, but that current teaching approaches may serve to limit enthusiasm that may otherwise have developed. Horan et al. previously demonstrated the positive impact that neurology and neurosurgery workshops can have on medical students (Horan et al., 2020). A mandatory module focusing on neurology and neurosurgery, potentially with an attached clinical component, should be considered as a means of improving student perceptions of these specialties.
5. Conclusion
This research further highlights ‘neurophobia’ as a persistent issue within medical education. A fear or apprehension toward neurology and neurosurgery is prevalent among medical students of all years and genders, and our findings suggest these fears are not merely fleeting concerns but significant barriers to learning, hindering students engagement with crucial neurological topics. Although neurophobia may be somewhat overstated, it is certainly a reality for many medical students.
Despite the hesitation expressed by the participants of this study toward neurological topics, students surveyed also showed a clear desire for more exposure, providing a compelling argument for the provision of more comprehensive learning opportunities in these areas, as a potential means of combatting neurophobia. This enthusiasm highlights several crucial insights: for one, while fear may deter engagement, the intrinsic motivation to learn can serve as a powerful catalyst for change. Secondly, students recognize that practical exposure is one of the simplest ways to demystify complex concepts and foster a deeper understanding, as evidenced by call for hands-on experience through clinical attachments. This underscores the necessity for medical curricula to incorporate more experiential learning opportunities, mentorship programs, and clinical rotations focused on neurology and neurosurgery.
Ultimately, the journey toward overcoming neurophobia must begin with acknowledgment and understanding of the themes highlighted by the current study. By providing the necessary resources and support, and addressing student fears head-on, medical schools can cultivate a generation of confident, knowledgeable healthcare professionals ready to tackle the complexities of the nervous system. Through collaboration between educators and students, neurophobia can be transformed from a barrier into a bridge, connecting aspiring physicians to potential careers in the fields of neurology and neurosurgery.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling editor: Dr W Peul
References
- Abulaban A., Obeid T.H., Alghatani H.A., Kojan S.M., Al-Khataami A.M., Abulaban A.A., Bokhari M.F., Merdad A.A., Radi S.A. Neurophobia amongst medical students. Neurosciences. 2015;20(1):37–40. [PMC free article] [PubMed] [Google Scholar]
- Blanch D.C., Hall J.A., Roter D.L., Frankel R.M. Medical student gender and issues of confidence. 2008;72(3):374–381. doi: 10.1016/j.pec.2008.05.021. [DOI] [PubMed] [Google Scholar]
- Clance P.R., Imes S.A. The imposter phenomenon in high achieving women: dynamics and therapeutic intervention. Psychother. Theory Res. Pract. 1978;15(3):241–247. [Google Scholar]
- Dewan M., Rattani A., Fieggen G., et al. Global Neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive summary of the blobal neurosurgery initiative at the program in in global surgery and social change. J. Neurosurg. 2019;130:1055–1064. doi: 10.3171/2017.11.JNS171500. [DOI] [PubMed] [Google Scholar]
- El Khamlichi A. Neurosurgery in africa. Clin. Neurosurg. 2005;52:214–217. [PubMed] [Google Scholar]
- Garzali I.U. The two sides of the scalpel: the polarizing image of surgery in early cinema. PLoS One. 2022;17(12) doi: 10.1371/journal.pone.0279422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenblatt S.H. The image of the ‘brain surgeon’ in American culture: the influence of Harvey Cushing. J. Neurosurg. 1991;75(5):808–811. doi: 10.3171/jns.1991.75.5.0808. [DOI] [PubMed] [Google Scholar]
- Han F., Zhang Y., Wang P., Dong W., Li-Xin Z., Ni J. Neurophobia among medical students and resident trainees in a tertiary comprehensive hospital in China. BMC Med. Educ. 2023;23:824. doi: 10.1186/s12909-023-04812-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill C.S., Dias L., Kitchen N. Perceptions of neurosurgery: a survey of medical srudents and foundation doctors. Br. J. Neurosurg. 2010;25(2):261–267. doi: 10.3109/02688697.2010.534197. [DOI] [PubMed] [Google Scholar]
- Horan J., Murphy S., O'Brien D. Neurosurgical education in Ireland: a conference and medical student experiences. Surgeon. 2020;18(3):159–164. doi: 10.1016/j.surge.2019.09.003. [DOI] [PubMed] [Google Scholar]
- Jukna S., Puteikis K., Mameniškienė Perception of neurology among undergraduate medical students- what can be done to counter neurophobia during clinical studies. BMC Med. Educ. 2023;23:447. doi: 10.1186/s12909-023-04405-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarron N. A Systematic review of neurophobia and perceived causes among medical students and junior doctors. Journal of Neurology, Neurosurgery and Psychiatry. 2012;83(e1) [Google Scholar]
- Shrestha B., Yadav S., Dhakal S., Ghimire P., Shrestha Y., Ragathure E.S. Status of self-esteem in medical students at a college in Kathmandu: a descriptive cross-sectional study. F1000 Research. 2021;10:1031. doi: 10.12688/f1000research.72824.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tadeu A., Fantanenau K., Eady K., Clarkin C., Demeulemeester C., Maclean H., Doja A. Neurophobia Inception: a Study of trainees' perception of neurology education. Canad J Neurol Sci. 2014;41:421–429. doi: 10.1017/s0317167100018436. [DOI] [PubMed] [Google Scholar]
- Valestrand E.A., Whelan B., Eilassen K.E.R., Schei E. Alienation in the teaching hospital: how physician non-greeting behaviour impacts medical students' learning and professional identity formation. Perspectives on Medical Education. 2024;13(1):239–249. doi: 10.5334/pme.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]