Abstract
Abstract
Purpose
Patients with cancer experience many Transitions in Care (TiC), occurring when a patient’s care transfers between healthcare providers or institutions/settings. Among other patient populations, TiC are associated with medical errors, patient dissatisfaction and elevated healthcare use and expenditure. However, our understanding of TiC among patients with cancer is lacking.
Objective
To map and characterise evidence about TiC among patients with cancer.
Participants
Adult patients with cancer at any stage in the cancer continuum.
Intervention
Evidence sources exploring TiC among patients with cancer were eligible.
Outcome
Evidence sources exploring TiC among patients with cancer using any outcome were eligible.
Setting
Any setting where a patient with cancer received care.
Design
This scoping review included any study describing TiC among patients with cancer with no restrictions on study design, publication type, publication date or language. Evidence sources, identified by searching six databases using search terms for the population and TiC, were included if they described TiC. Two independent reviewers screened titles/abstracts and full texts for eligibility and completed data abstraction. Quantitative data were summarised using descriptive statistics and qualitative data were synthesised using thematic analysis.
Results
This scoping review identified 801 evidence sources examining TiC among patients with cancer. Most evidence sources focused on the TiC between diagnosis and treatment and breast or colorectal cancer. Six themes emerged from the qualitative evidence sources: the transfer of information, emotional impacts of TiC, continuity of care, patient-related factors, healthcare provider-related factors and healthcare system-related factors. Interventions intended to improve TiC among patients with cancer were developed, implemented or reviewed in 163 evidence sources.
Conclusion
While there is a large body of research related to TiC among patients with cancer, there remains a gap in our understanding of several TiC and certain types of cancer, suggesting the need for additional evidence exploring these areas.
Keywords: ONCOLOGY, Organisation of health services, Quality in health care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A validated search strategy for cancer and a previously published search strategy for transitions in care guided the development of the search strategy used in this study, which was developed by a researcher with expertise in systematic and scoping reviews.
The eligibility criteria included all cancer types, which allowed us to compare and contrast findings between patient populations but may not be generalisable to all cancer populations.
The findings of our study will inform future research designing, implementing and evaluating interventions to improve TiC among patients with cancer.
Purpose
The incidence of cancer is increasing, with an expected increase to 29.4 million new diagnoses by 2040.1 2 Despite these trends, advances in early detection and life-saving cancer treatments have contributed to increased survival rates, resulting in patients having more interactions with the healthcare system.1 3 Patients with cancer face complex healthcare journeys and experience many Transitions in Care (TiC).4,6 TiC are points in care when the responsibility for a patient’s care transfers between healthcare providers, institutions or settings.7 8 Examples of TiC include the transition from the operating room to a hospital ward, or from home to an emergency department.9,11 The concept of TiC is similar to continuity of care in that, if TiC are effective care will be continuous and seamless. However, unlike the concept of continuity of care, TiC are distinct periods in care delivery that require a set of actions.12 13
TiC are times when the risk of error is high and therefore a vulnerable period for patients during healthcare delivery.59 14,21 Evidence suggests that ineffective TiC are linked to excessive costs, healthcare delays, duplicate testing, inaccurate transfer of information, elevated healthcare resource usage, preventable readmissions to hospital, additional primary care or emergency visits and dissatisfaction with care.59 14,21 Effective TiC require multidisciplinary collaborations to ensure complete and timely transfer of information, support from leadership, patient education and early identification of patients with elevated risk.22 23
TiC and the consequences of poor TiC have been investigated in several patient populations,514,20 including patients living with and beyond cancer; however, to our knowledge, the evidence on TiC for patients with cancer has not been comprehensively mapped and characterised. Organisations including the Joint Commission and the National Academy of Medicine have called for effective strategies to improve TiC among patients with cancer.4 24 Therefore, our objective is to identify, synthesise and map existing literature examining TiC among patients with cancer. This scoping review will allow us to understand the body of literature on TiC among patients with cancer and provide a foundation for additional research examining the quality of TiC throughout the cancer continuum.
Methods
Study design
This study used scoping review methodology to map and characterise existing evidence and identify knowledge gaps around TiC among patients with cancer.25 26 Scoping review methodology is useful for understanding the extent, volume and characteristics of a body of research; especially in under-researched areas, such as TiC among patients with cancer.25 26 This review followed the Joanna Briggs Institute methodology and the Preferred Reporting Items for Systematic Reviews—Scoping Review Extension (PRISMA-ScR).27 28 Ethical approval was not required because all data are published.
This scoping review protocol has been previously reported.29
Search strategy
The search strategy, developed by DL, combined language, keywords and synonyms for the patients with cancer and TiC were with Boolean operators. A pre-existing PubMed cancer filter and search terms from a previously published scoping review were adapted to each unique database.30 The search strategy was run in MEDLINE, EMBASE, APA PsycINFO, CINAHL, Cochrane CENTRAL and the Cochrane Database of Systematic Reviews (online supplemental appendix A). Grey literature (conference proceedings, viewpoints, editorials and organisational reports) were also evaluated. The search occurred on 14 June 2023.
Eligibility criteria
Evidence sources were included if they described TiC among adult cancer patients throughout the cancer continuum. Evidence sources were eligible if they included eligible (cancer) and non-eligible (non-cancer) populations but stratified results so data on only patients with cancer could be abstracted. There were no restrictions on study design, language or year of publication. Evidence sources were excluded if they were focused on changes to TiC during COVID-19, did not describe TiC throughout the cancer continuum, described TiC among patients without cancer; only included paediatric patients; or examined the TiC between paediatric to adult care (which differs from adult TiC due to familial involvement, resources and autonomy).31
Selection of evidence sources
There were two phases for evidence source screening: title and abstract and full-text. Both were performed in duplicate by two independent reviewers to determine evidence source eligibility, with Covidence being used for data management.32 Reliability between reviewers (JK, KS, SK, AT) was calibrated before both phases of screening, with reviewers screening the same 20 potential evidence sources separately and comparing their decisions. This process was performed before starting each phase and repeated until an 80% agreement between reviewers was reached. Disagreements were not solved in the title/abstract screening phase, with evidence sources deemed eligible by one reviewer being included. Conflicts during the full-text screening phase were resolved through consensus through discussion or a neutral third reviewer.
Data charting process
Data abstraction was completed by one reviewer (JK, SK, SI, AT, AH) and reviewed by another reviewer (JK, SK). A standardised data abstraction form was pilot-tested using 20 evidence sources. This form was modified after the pilot test and throughout the data abstraction process to extract all relevant information from the evidence sources. We abstracted bibliographic data, and information about the TiC, setting and included population. For any evidence sources describing interventions targeting TiC, we abstracted an intervention description, measurement, outcome and recommendations. Quality assessment of the evidence sources was not completed. The final data abstraction form is provided in online supplemental appendix B.
Data synthesis
Quantitative data were summarised using frequencies and qualitative data were summarised using thematic analysis.33
For quantitative analysis, the type of cancer was categorised, with evidence sources that examined more than one cancer type being categorised as ‘multiple’ (online supplemental appendix B). Similarly, TiC was categorised using ‘from’ and ‘to’, and if an evidence source broadly examined TiC or multiple TiC, TiC was categorised as ‘multiple’ (online supplemental appendix B). Outcomes were categorised as patient-related, system-related, or both. The research objectives for included evidence sources were also categorised (online supplemental appendix B).
Thematic analysis of the qualitative evidence sources was iterative and collaborative. Two analysts (JK, SK) reviewed the evidence source and identified emerging themes; analysed the data and reviewed the themes. Quotations were aggregated by themes and focused on the experiences, perceptions and understanding of patients, families, carers or healthcare providers with TiC. If there were discrepancies aggregating quotes, they were resolved through consensus by discussion.
Patient and public involvement
Patients were not involved in the conception, conduct or interpretation of the findings.
Results
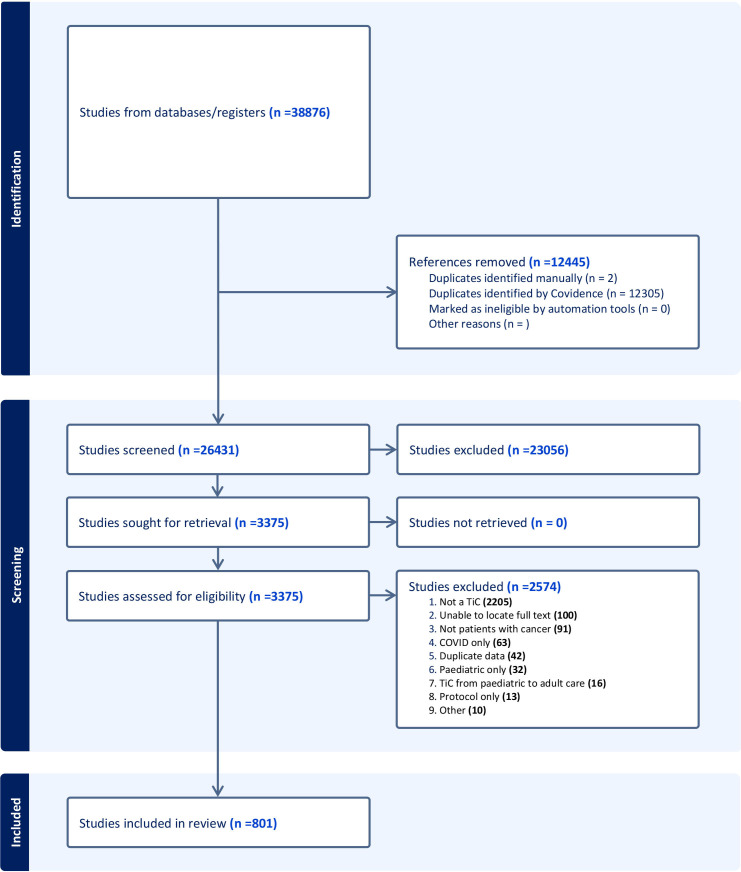
The search strategy yielded 38 876 evidence sources with 3375 full-texts being assessed for eligibility, resulting in 801 included evidence sources (figure 1).
Figure 1. The Preferred Reporting Items for Systematic Reviews (PRISMA) flow diagram for the scoping review. The PRISMA diagram details the database searches and selection process applied to the evidence sources during title/abstract screening and full-text screening. The vertical arrows show the flow of the selection process, and the horizontal arrows show the evidence sources that were removed or considered irrelevant. TiC, Transitions in Care.
Characteristics of included studies
A detailed description of included evidence source characteristics is provided in online supplemental table 1. Included evidence sources were primarily journal articles (n=611, 76.2%) and conference proceedings (n=169, 21.1%). Evidence sources were published between 1987 and 2023 and predominately originated from the United States of America (n=370, 46.2%) and Canada (n=94, 11.7%). Most included evidence sources were published in English (n=732, 91.4%). Over time, the focus of research on TiC among patients with cancer has shifted; earlier evidence sources were predominantly focused on the transition from active treatment to survivorship, whereas recently there was a notable increase in quantitative research focussing on delays in access to healthcare, particularly from diagnosis to treatment.
Cancer and TiC
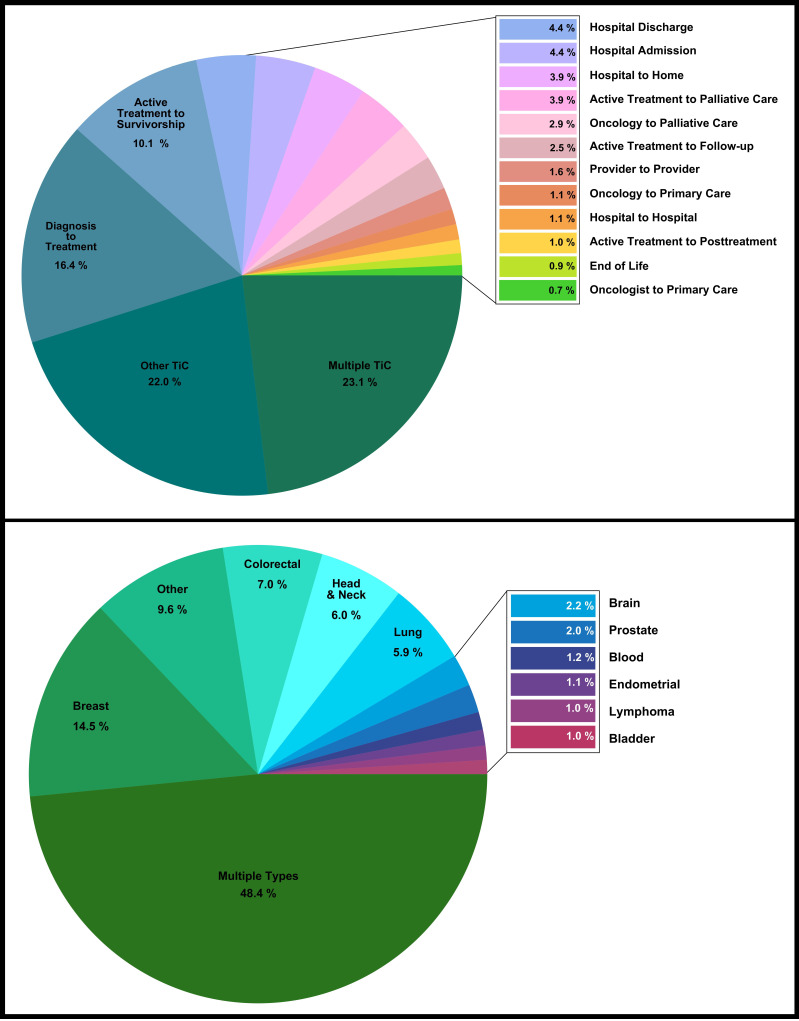
Many evidence sources examined multiple types of cancer (n=388, 48.6%), followed by breast (n=60, 14.4%), colorectal (n=56, 7.0%), head and neck (n=36, 6.0%) and lung cancer (n=28, 5.8%) (figure 2). Many evidence sources examined multiple TiC (n=185, 23.0%), the transition from diagnosis to treatment (n=132, 16.4%) and from active treatment to survivorship (n=81, 10.1%) (figure 2). The outcomes examined in the included evidence sources were patient-related (n=488, 60.7%), system-related (n=156, 19.4%) or both (n=156, 19.4%) (online supplemental table 1).
Figure 2. Pie charts that categorise cancer type (top) and Transitions in Care (TiC) type (bottom) of the included evidence sources. Different colours describe different categories. The total percentage of the categorised cancer type or TiC type is listed below the category (in the pie chart) and beside the side boxes. The thin black lines connected to the coloured boxes denote any cancer or TiC types that were unable to fit within the pie chart. The TiC diagnosis to treatment contains diagnosis to treatment and diagnosis to surgery. Discharge includes any discharge from a healthcare provider, facility or institution. Readmission includes any readmission to a healthcare facility or institution.
Interventions to improve TiC
Of the included evidence sources 165 described (12.7%, n=21), implemented or evaluated interventions (87.3%, n=144) to improve TiC. There is an increasing trend to develop, implement and implement intervention; the median year publication was 2020 (IQR=2016, 2021). Most intervention studies were from the USA (40.0%, n=66), Canada (13.9%, n=23), Australia (9.7%, n=16) and the UK (8.4%, n=14); and 4.6% were from low-middle income countries (n=9). The majority of the interventions were designed for patients with multiple types of cancer (53.7%, n=88), breast (13.4%, n=22) and colorectal cancer (6.1%, n=10). Many interventions were designed to address the transition from treatment to survivorship (23.2%, n=38), from the hospital to home (20.7%, n=34) and from oncologists to general practitioners (10.4%, n=17).
Thematic analysis from the qualitative data
Many (n=249, 31.0%) of the included evidence sources qualitatively explored how patients/families/carers (n=208, 83.5%) and healthcare providers (n=60, 24.1%) experienced TiC during the cancer continuum (some evidence sources included patients/families/carers and healthcare providers so the estimates sum to greater than 100.0%). From 249 qualitative evidence sources, the following six themes were identified: emotional impacts, transfer of information, continuity of care, patient-related factors, healthcare provider-related factors and health system-related factors.
Emotional impact
The emotional impact (psychological effects of emotional distress) of TiC during cancer care was explored in 84 evidence sources. This theme mostly focused on breast (26.2%), colorectal (10.7%) and multiple types of cancer (36.9%). The emotional impact of TiC often stems from patients with cancer experiencing ineffective TiC. Negative psychological effects were linked to the transition from active care to survivorship and diagnosis to treatment, causing feelings of abandonment, heightened anxiety, stress, fear and uncertainty. A patient with cancer expanded on their declining mental state after experiencing a TiC:
I went into a depression I think a little bit, because you experience a lot of anxiety, it’s very emotional, there is a lot of fear and being overwhelmed, things happening right behind each other.34
Another patient described the emotions surrounding their transition out of active care:
It’s a bit like throwing a bird up that had a broken wing to see if it can fly and some of them soar and others are like oh oh maybe I want to go back into the cocoon… you know it’s a warm cozy place where you feel safe.35
Patients with cancer and providers reflected on the absence of opportunities to discuss emotional and psychological needs and the lack of psychological support services and resources during challenging TiC. A patient described this gap in care:
One of the unmet needs that I didn’t realize I needed was the emotional aspect of going home and trying to cope with the family, and I had a real hard time. And finally, they called the doctor and put me on some emotion pills and something to calm me down.36
Transfer of information
Transfer of information was discussed in 123 evidence sources and refers to the process of transferring or communicating a patient’s healthcare information between patients, general practitioners, specialists and other healthcare providers. These evidence sources examined the transfer of information during TiC mainly targeting breast (34.5%), colorectal (11.3%) and multiple types of cancer (41.5%). Patients described effective transfers of information as those that occurred when healthcare providers took the time to clearly explain their prognosis, treatment plans and health system procedures. Ineffective transfers of information resulted from having information withheld, inadequate explanations or a lack of interaction between patients and their healthcare providers. Patients also described the amount of information delivered as overwhelming and hard to understand. Patients shared their experiences of inadequate transfer of information between healthcare providers:
In terms of handoff, there were none, physician to physician, it was me. It was all up to me to carry information forward. Providers need to talk to each other, so we don’t hear different things from different providers.37
Sometimes my doctor had no information of the treatments provided by another doctor. Even the specialist told me that they have not sent it…38
Another patient addressed the overwhelming amount of information given to a patient,
I wish that things were explained to me a bit more. You know, I had a lot of information thrown at me at once.39
The evidence sources illustrated that the siloed nature of healthcare hindered the transfer of information, often contributing to communication difficulties between healthcare providers. General practitioners often felt excluded from the discussion about their patient’s care.
We see this a lot with other specialties too, but I think oncology probably might be even worse than anybody else in terms of keeping it to themselves and not feeling like they have to integrate things back to what’s going on in the primary care doctor’s office.79
Continuity of care
Continuity of care, the extent of connectedness, integration and coordination of care experienced by patients and healthcare providers,40 was addressed in 96 evidence sources. These evidence sources concentrated on breast (21.9%), colorectal (7.3%) and multiple types of cancer (44.8%). While some evidence sources reported high levels of continuity of care, the majority found that delays, lack of support services and improper referrals led to fragmented care. Low continuity of care often occurred during the transition from active treatment to survivorship:
The support system falls apart once women complete treatment. They lose their entire support system at the medical level.41
Well, they cut me open, ‘fixed me’… and then sent me on my way. Didn't hear a peep [from the medical team]just left to my own devices for years now.42
Disconnection between different healthcare providers was also observed during TiC, where other healthcare providers were isolated and unaware of the oncological care processes:
I feel like the whole [breast cancer] treatment process was disconnected from my primary care physician. My primary care physician was not involved at all.43
Patient-related factors
Patient-related factors such as their characteristics (eg, age, sex, gender and ethnicity) healthcare expectations, existing support networks and independence level shaped their perception of TiC. This theme was referred to in 70 evidence sources, often concerning breast (25.7%), colorectal (8.6%) and multiple types of cancer (40.0%). Patients with cancer believed that the rigid structure and procedures of the healthcare system gave rise to a lack of personalised healthcare. Patients preferred healthcare plans, tailored towards their unique wishes, capacities, languages, cultural norms and religious values. A patient highlighted the contrasting physical capabilities between themselves and other patients during a hospital discharge when stating,
Some women can go back after 23 hours, and some cannot, and you should not be made to feel there is something wrong with you if you do not.44
Collectively, patients and providers felt that tailoring healthcare towards the individual patient was of utmost importance.
Patients’ preconceived expectations affected how satisfied they were with their healthcare experiences. If expectations were informed by knowledge about the healthcare system, satisfaction was higher.44,47 Frequently, patients had high expectations (perhaps due to inadequate information about their care and the healthcare system), which led to dissatisfaction.
A patient’s support network of friends, family and healthcare providers also influenced their experiences with TiC during their care. While patients in some studies commended the strong relationships that they developed with their healthcare providers, which they viewed as very supportive during TiC, others commented on the loss of support from healthcare providers, family or friends once they were discharged from a care setting or declared cancer free:
I used to be this guy that had a sense of purpose and a reason for going all of a sudden all of that is taken away and no-one’s telling you what to do next, it’s just come and see me in 3 months' time… for me, a massive sense of loss. It’s a loss of purpose and identity.48
This is described in greater detail in the next theme, healthcare provider-related factors.
Healthcare provider-related factors
Healthcare provider-related factors were described in 43 evidence sources and refer to the knowledge, capabilities and position of healthcare providers within a healthcare organisation within healthcare can impact TiC among patients with cancer. These evidence sources discussed this theme, with many evidence sources targeting breast (23.2%), lung (9.3%), colorectal (9.3%) and multiple types of cancer (39.5%). This theme demonstrated that many patients with cancer had confidence in their healthcare provider’s capabilities. However, patients had reduced trust in their general practitioner’s capabilities when compared with a specialist:
I went there [GP] lots of times, he read the protocols of the hospital, but he didn’t add anything… I think it’s a lack of knowledge. I think that they [GP’s] are not prepared when it concerns serious illnesses. I have the impression that they are not educated on how to react.
The hierarchy structure of the healthcare system affects the patient-provider and provider-provider relationships. A patient discussed the unequal patient-provider power dynamic stating:
When you are a patient, you are not equal; the hierarchy shifts. Then you are a little beggar.49
Healthcare providers, including nurses and general practitioners, felt undervalued and pressured to follow the healthcare system hierarchy, leading to difficulty in discussing medical decisions with other healthcare providers. A general practitioner expressed this sentiment in the following quote:
As a GP I am constantly being instructed by specialists’ secretaries to order tests, prescribe antibiotics, write referrals, and see post-op patients when it’s inconvenient for the specialist.50
Health system-related factors
Health system-related factors refer to the healthcare system’s capacity to meet the needs of patients with cancer. This theme appeared in 67 evidence sources and largely covered breast (22.4%), colorectal (6.0%) and multiple types of cancer (38.8%). Health system-related factors focused on access to care, available resources, timeliness and safety. Patients residing in rural areas had restricted access to care due to transportation and limited healthcare facility hours. The lack of resources for patients with cancer was also noticed during care, as a patient stated:
I curse at times… but you seem to be left to battle your way throughout in yourself… But then once you come home, then it’s like, you’re left on your own… well knowledge of these services (stoma care)… I found out through my daughter going on the internet… it wasn’t offered to me. No, I went straight on that myself.51
Although evidence described healthcare efficiency during information transfers and referrals, timeliness during TiC such as delays to and between treatments was also criticised by patients with cancer:
I sat for a day and a half day in the dayroom taken to a ward overnight and brought back the next day.52
The concept of safety differed between patients with cancer and healthcare providers, with patients gravitating towards healthcare system factors that made them feel comfortable and therefore ‘safe’. A patient felt safe when under the care of a specialist:
I have my doctor but she is not a specialist. She does what I tell her to and orders a mammogram every year. But, I don’t go to the oncologist anymore, and so I worry. With the specialist, I feel protected.41
Healthcare providers were concerned about the lack of standardisation among TiC workflows, processes and procedures, especially during discharges:
It’s all over the place, you [have] so many things to do, you don’t know where to start, what to do, what is done, what is not done… and you have to rush… it’s haywire. There is no process, to begin with.53
Discussion
This scoping review identified a large body of evidence examining TiC among patients with cancer. Despite the abundance of evidence sources, there were still evidence gaps identified. A large proportion of included evidence sources focused on a few types of cancer (breast and colorectal), a few TiC (diagnosis to treatment and active treatment to survivorship) and originated from high-income countries leaving a gap in our understanding of other TiC (including TiC during active treatment) and types of cancer. The call-to-action from the Institute of Medicine in 2006 and the Joint Commission in 20124 24 likely contributed to a spike in research on TiC, with 97.9% of the included evidence sources being published in 2006 or after. Similarly, there has been a shift in the type of research and the TiC explored since the COVID-19 pandemic—research after the pandemic is focused on delays in transitions, especially from diagnosis to treatment, and is largely quantitative rather than qualitative. This surge in research is likely a response to the extensive healthcare delays caused by the COVID-19 pandemic.54 There were numerous qualitative studies, conducted mostly pre-pandemic, that explored patient, family and provider perspectives during TiC, resulting in six main themes: transfer of information, emotional impacts of TiC, continuity of care, patient-related factors, healthcare provider-related factors and healthcare system-related factors.
Understanding TiC within the cancer continuum is an important step towards minimising the potential negative outcomes associated with TiC (increased medical errors, adverse events and healthcare expenditure).2055,57 Ineffective TiC can have an economic impact on the healthcare system, such that patients who experience three or more transitions after hospital discharge increase Medicare expenses by $15 billion.20 24 Medical errors during TiC may partly contribute to the increase in TiC and consequently the increased cost. Previous research shows that 49% of hospitalised patients experience at least one medical error during the transition from inpatient care to outpatient care contributing to the $20 billion annual cost of medical errors in the USA.58,60 This is particularly relevant for patients with cancer; Christiansen et al found that 50% of adverse events experienced by patients with cancer were related to TiC, with 46% of them causing physical harm to the patient and nearly half (43.5%) being preventable.61 As many TiC-related adverse events are preventable,61,63 there is a clear opportunity to reduce adverse events and improve patient health by strategically targeting ineffective TiC. Additional research is needed to identify and understand specific TiCs where there are opportunities for improvement.
This scoping review revealed a paucity of evidence among certain types of cancer and certain types of TiC. Few evidence sources examined TiC among patients with prostate, blood, gynecologic, brain and head and neck cancers. Based on the evidence identified in this study, TiC are unique to each type of cancer; likely due to specific treatment plans and approaches for each type of cancer.4,664 65 Sisler et al found that 71% of patients with colorectal cancer felt they were adequately prepared to experience the transition from active treatment to follow-up care.66 While Jones et al reported that during the same transition, patients with endometrial cancer were inadequately prepared, facing difficulties communicating with healthcare providers and accessing information and resources.67 Similarly, this study revealed that each TiC has unique challenges. Suryanarayana et al found that patients with cancer transitioning from oncology to palliative care wanted appropriate counselling resources, and adaptability from their healthcare providers towards their unique cultural, linguistic and religious inclinations68; whereas Carrillo et al identified that when transitioning from hospital to home, patients with cancer experienced uncertainty, craved control and yearned for home.69 Given that each TiC is unique, and different types of cancer have specific needs, additional evidence around each TiC among a variety of cancer types is needed, particularly for understudied cancers and high-risk TiC identified among other patient populations.2170,76 Patients with cancer require customised support and resources to successfully navigate each unique TiC, highlighting the necessity to develop and tailor interventions that address these challenges.
Interventions to improve TiC can successfully mitigate negative outcomes related to ineffective TiC among patients with cancer.77 78 This study identified 168 evidence sources that explored interventions to improve TiC among patients with cancer, some of which successfully improved TiC and care for patients with cancer. Implementing tailored survivorship care plans during the transition from active treatment to survivorship is effective in reinforcing follow-up plans, transferring information, reducing symptom burden and improving both patient satisfaction and quality of life.79,82 Similarly, developing and implementing an Electronic Medical Record-based handoff tool effectively conveyed necessary information prevented errors, and reduced ineffective TiC for patients with cancer.83 Additional strategies included assigning a designated healthcare professional to provide continued support during these TiCs and providing psychosocial support to patients with cancer and their families through establishing formal protocols.84 85 Many of the interventions identified in this study were related to the transition from active treatment to survivorship, and the evaluation of the effectiveness of interventions was commonly lacking. Further research into the development of interventions, scalable strategies and rigorous evaluations for a broad range of TiC (including a systematic review of the interventions) is crucial, especially for understudied cancers and TiC.
This scoping review was conducted using rigorous and transparent methodology to map and synthesise evidence on TiC among patients with cancer. One limitation of the methodology was that potentially relevant evidence sources may have been missed. To mitigate this potential limitation, this review employed a robust search strategy with no restrictions on language, publication type or publication date. This also allowed for the inclusion of a wide range of study designs and methodologies as well as grey literature, published and unpublished material. This study included data for all TiC and types of cancer, which was limited to previous reviews on TiC,86 and provides a broad understanding of TiC among patients with cancer, but this could also be viewed as a limitation because granular details were challenging to report due to the size and scope of the review. For that reason, additional systematic reviews should be done to explore the efficacy of methods for information transfer during TiC, the emotional impacts of TiC and interventions for TiC among patients with cancer.
Conclusion
This scoping review reveals ample literature on TiC among patients with cancer but also identifies evidence gaps for certain types of cancer (ie, prostate, bowel, liver, pancreatic, oesophageal) and TiC (ie, home to the emergency department, between different levels of healthcare or different healthcare providers), highlighting the need for more targeted evidence. Broadly, patients with cancer express being ill-equipped to transfer between healthcare settings and providers, due to unsuccessful transfer of information and poor communication.2087,91 Patient-oriented interventions including tailored survivorship care plans and nurse coordinators are beneficial in reducing unintended consequences of TiC on patient outcomes and the healthcare system.
supplementary material
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-078210).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Data availability free text: Data will be made available upon reasonable request to the corresponding author.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Jaling Kersen, Email: jaling.kersen1@ucalgary.ca.
Stefan Kurbatfinski, Email: stefan.kurbatfinsky@ucalgary.ca.
Abigail Thomas, Email: abigail.thomas2@ucalgary.ca.
Seremi Ibadin, Email: seremi.ibadin1@ucalgary.ca.
Areej Hezam, Email: areej.hezam@ucalgary.ca.
Diane Lorenzetti, Email: dllorenz@ucalgary.ca.
Shamir Chandarana, Email: shamir.chandarana@ucalgary.ca.
Joseph C Dort, Email: jdort@ucalgary.ca.
Khara M Sauro, Email: kmsauro@ucalgary.ca.
Data availability statement
Data are available upon reasonable request.
References
- 1.Wild CP. The global cancer burden: necessity is the mother of prevention. Nat Rev Cancer. 2019;19:123–4. doi: 10.1038/s41568-019-0110-3. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: An overview. Int J Cancer. 2021;149:778–89. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 3.Kash KM, Sharma S, Goldfarb NI. Is disease management right for oncology? Popul Health Manag. 2009;12:337–43. doi: 10.1089/pop.2009.0029. [DOI] [PubMed] [Google Scholar]
- 4.Medicine Io, Council NR . From cancer patient to cancer survivor: lost in transition. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 5.Choi Y. Care Coordination and Transitions of Care. Med Clin North Am. 2017;101:1041–51. doi: 10.1016/j.mcna.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Lorenzini E, Boell JEW, Oelke ND, et al. Care transition from hospital to home: cancer patients’ perspective. BMC Res Notes. 2020;13:267. doi: 10.1186/s13104-020-05099-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Transitions of care. 2016.
- 8.Howard ED. Transitions in Care: Risk, Recovery, and Best Practices. J Perinat Neonatal Nurs. 2018;32:7–11. doi: 10.1097/JPN.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 9.WHO Technical Series on Safer Primary Care. Transitions of Care Licence: CC BY-NC-SA 3.0 IGO ed. 2016. pp. 1–28.
- 10.Canadian Institutes of Health Research Transitions in care: overview. https://cihr-irsc.gc.ca/e/50972.html n.d. Available.
- 11.Naylor MD. Transitional care of older adults. Annu Rev Nurs Res. 2002;20:127–47. [PubMed] [Google Scholar]
- 12.Trindade LF, Boell JEW, Lorenzini E, et al. Effectiveness of care transition strategies for colorectal cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2022;30:6251–61. doi: 10.1007/s00520-022-07033-2. [DOI] [PubMed] [Google Scholar]
- 13.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 14.Taplin SH, Clauser S, Rodgers AB, et al. Interfaces across the cancer continuum offer opportunities to improve the process of care. J Natl Cancer Inst Monogr . 2010;2010:104–10. doi: 10.1093/jncimonographs/lgq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3:159–66. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leith BA. Transfer stress and medical intensive care patients and family members. Dynamics. 2001;12:22–7. [PubMed] [Google Scholar]
- 17.Chaboyer W, Kendall E, Kendall M, et al. Transfer out of intensive care: a qualitative exploration of patient and family perceptions. Aust Crit Care. 2005;18:138–41. doi: 10.1016/s1036-7314(05)80026-8. [DOI] [PubMed] [Google Scholar]
- 18.Niès J, Colombet I, Zapletal E, et al. Effects of automated alerts on unnecessarily repeated serology tests in a cardiovascular surgery department: a time series analysis. BMC Health Serv Res. 2010;10:70. doi: 10.1186/1472-6963-10-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malley A, Kenner C. Transitions in care a critical review of measurement. J Perioper Crit Intensiv Care Nurs. 2016;2:132. doi: 10.4172/2471-9870.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–6. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 21.Naylor M, Keating SA. Transitional care. Am J Nurs. 2008;108:58–63. doi: 10.1097/01.NAJ.0000336420.34946.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Labson MC. Adapting the joint commission’s seven foundations of safe and effective transitions of care to home. Home Healthc Now. 2015;33:142–6. doi: 10.1097/NHH.0000000000000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ontario HQ Transitions in Care. https://www.hqontario.ca/Portals/0/documents/evidence/quality-standards/transitions-in-care-what-we-heard-en.pdf Available.
- 24.Commission MPA, Book AD . Healthcare spending and the medicare program. Washington, DC: MedPAC; 2012. [Google Scholar]
- 25.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 27.Peters MD, Godfrey CM, McInerney P, et al. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. 2015.
- 28.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 29.Sauro K, Maini A, Machan M, et al. Are there opportunities to improve care as patients transition through the cancer care continuum? A scoping review protocol. BMJ Open. 2021;11:e043374. doi: 10.1136/bmjopen-2020-043374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stelfox HT, Lane D, Boyd JM, et al. A scoping review of patient discharge from intensive care: opportunities and tools to improve care. Chest. 2015;147:317–27. doi: 10.1378/chest.13-2965. [DOI] [PubMed] [Google Scholar]
- 31.Castillo C, Kitsos E. Transitions From Pediatric to Adult Care. Glob Pediatr Health. 2017;4:2333794X17744946. doi: 10.1177/2333794X17744946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Covidence Systematic Review Software [program]. Melbourne, Australia. 2022.
- 33.Clarke V, Braun V, Hayfield N. Thematic analysis. Qual Psychol A Pract Guide to Res Methods. 2015;222:248 [Google Scholar]
- 34.Mollica M, Nemeth L. Transition from patient to survivor in African American breast cancer survivors. Cancer Nurs. 2015;38:16–22. doi: 10.1097/NCC.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 35.Hackett F, Dowling M. Lymphoma survivors’ experiences at the end of treatment. J Clin Nurs. 2019;28:400–9. doi: 10.1111/jocn.14658. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman AJ, Brintnall RA, von Eye A, et al. The voice of postsurgical lung cancer patients regarding supportive care needs. Lung Cancer (Auckl) 2014;5:21–31. doi: 10.2147/LCTT.S59703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mayer DK, Gerstel A, Leak AN, et al. Patient and provider preferences for survivorship care plans. J Oncol Pract. 2012;8:e80–6. doi: 10.1200/JOP.2011.000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ko E, Cardenas V, Zúñiga ML, et al. Challenges for Latina Breast Cancer Patient Survivorship Care in a Rural US-Mexico Border Region. Int J Environ Res Public Health. 2021;18:7024. doi: 10.3390/ijerph18137024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duggleby WD, Penz K, Leipert BD, et al. “I am part of the community but.” The changing context of rural living for persons with advanced cancer and their families. Rural Remote Health. 2011;11:1733. [PubMed] [Google Scholar]
- 40.Gulliford M, Naithani S, Morgan M. What is “continuity of care”? J Health Serv Res Policy. 2006;11:248–50. doi: 10.1258/135581906778476490. [DOI] [PubMed] [Google Scholar]
- 41.Napoles AM, Ortiz C, Santoyo-Olsson J, et al. Posttreatment survivorship care needs of Spanish-speaking Latinas with breast cancer. J Community Support Oncol . 2017;15:20–7. doi: 10.12788/jcso.0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mazariego CG, Laidsaar-Powell R, Smith DP, et al. Avoiding the “survivorship abyss”: Qualitative insights from 15-year prostate cancer survivors. Psychooncology. 2021;30:1745–55. doi: 10.1002/pon.5738. [DOI] [PubMed] [Google Scholar]
- 43.Burke NJ, Napoles TM, Banks PJ, et al. Survivorship Care Plan Information Needs: Perspectives of Safety-Net Breast Cancer Patients. PLoS One. 2016;11:e0168383. doi: 10.1371/journal.pone.0168383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woods A, McNamara C. The experience of mastectomy patients on the 23-hour pathway. Cancer Nurs Pract. 2019;18:27–35. doi: 10.7748/cnp.2018.e1496. [DOI] [Google Scholar]
- 45.Nissim R, Rodin G, Schimmer A, et al. Finding new bearings: a qualitative study on the transition from inpatient to ambulatory care of patients with acute myeloid leukemia. Support Care Cancer . 2014;22:2435–43. doi: 10.1007/s00520-014-2230-3. [DOI] [PubMed] [Google Scholar]
- 46.Camateros P, Wang Y, Cheung WY. Young adult cancer survivors’ expectations of physicians for follow-up and general health care: Implications for health services delivery. J C O. 2015;33:6564. doi: 10.1200/jco.2015.33.15_suppl.6564. [DOI] [Google Scholar]
- 47.Muktar S, Thiruchelvam PXR, Hadjiminas D. Patients’ Views of Follow-Up Care After Treatment for Breast Cancer: A Comparison of 2 Approaches. J Oncol Navig Surviv. 2015;6:22–9. [Google Scholar]
- 48.Thompson J, Coleman R, Colwell B, et al. Preparing breast cancer patients for survivorship (PREP) - a pilot study of a patient-centred supportive group visit intervention. Eur J Oncol Nurs. 2014;18:10–6. doi: 10.1016/j.ejon.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 49.Kyte K, Ekstedt M, Rustoen T, et al. Longing to get back on track: Patients’ experiences and supportive care needs after lung cancer surgery. J Clin Nurs. 2019;28:1546–54. doi: 10.1111/jocn.14751. [DOI] [PubMed] [Google Scholar]
- 50.Lizama N, Johnson CE, Ghosh M, et al. Keeping primary care “in the loop”: General practitioners want better communication with specialists and hospitals when caring for people diagnosed with cancer. Asia Pac J Clin Oncol. 2015;11:152–9. doi: 10.1111/ajco.12327. [DOI] [PubMed] [Google Scholar]
- 51.Beaver K, Latif S, Williamson S, et al. An exploratory study of the follow-up care needs of patients treated for colorectal cancer. J Clin Nurs. 2010;19:3291–300. doi: 10.1111/j.1365-2702.2010.03407.x. [DOI] [PubMed] [Google Scholar]
- 52.Lafferty J, Rankin F, Duffy C, et al. Continuity of care for women with breast cancer: a survey of the views and experiences of patients, carers and health care professionals. Eur J Oncol Nurs. 2011;15:419–27. doi: 10.1016/j.ejon.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 53.Tan YY, Blackford J. “Rapid discharge”: issues for hospital-based nurses in discharging cancer patients home to die. J Clin Nurs. 2015;24:2601–10. doi: 10.1111/jocn.12872. [DOI] [PubMed] [Google Scholar]
- 54.Mogharab V, Ostovar M, Ruszkowski J, et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: a panel of systematic review and meta-analyses. Global Health. 2022;18:58. doi: 10.1186/s12992-022-00836-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jošt M, Knez L, Mrhar A, et al. Adverse drug events during transitions of care : Randomized clinical trial of medication reconciliation at hospital admission. Wien Klin Wochenschr. 2022;134:130–8. doi: 10.1007/s00508-021-01972-2. [DOI] [PubMed] [Google Scholar]
- 56.Freund Y, Goulet H, Bokobza J, et al. Factors associated with adverse events resulting from medical errors in the emergency department: two work better than one. J Emerg Med. 2013;45:157–62. doi: 10.1016/j.jemermed.2012.11.061. [DOI] [PubMed] [Google Scholar]
- 57.Pham JC, Aswani MS, Rosen M, et al. Reducing medical errors and adverse events. Annu Rev Med. 2012;63:447–63. doi: 10.1146/annurev-med-061410-121352. [DOI] [PubMed] [Google Scholar]
- 58.Andel C, Davidow SL, Hollander M, et al. The economics of health care quality and medical errors. J Health Care Finance. 2012;39:39–50. [PubMed] [Google Scholar]
- 59.Rodziewicz TL, Houseman B, Hipskind JE. Medical error reduction and prevention. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 60.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–51. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Christiansen AH, Lipczak H, Knudsen JL. Attention to cancer patients’ safety after primary treatment is needed. Dan Med J. 2015;62:A5090. [PubMed] [Google Scholar]
- 62.de Vries EN, Ramrattan MA, Smorenburg SM, et al. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–23. doi: 10.1136/qshc.2007.023622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Safaee MM, Morshed RA, Spatz J, et al. Interfacility neurosurgical transfers: an analysis of nontraumatic inpatient and emergency department transfers with implications for improvements in care. J Neurosurg. 2019;131:281–9. doi: 10.3171/2018.3.JNS173224. [DOI] [PubMed] [Google Scholar]
- 64.National Cancer Institute Types of Cancer Treatment. 2023. https://www.cancer.gov/about-cancer/treatment/types#:~:text=The%20types%20of%20treatment%20that,with%20chemotherapy%20and%20radiation%20therapy Available.
- 65.Goldsbury DE, Yap S, Weber MF, et al. Health services costs for cancer care in Australia: Estimates from the 45 and Up Study. PLoS One. 2018;13:e0201552. doi: 10.1371/journal.pone.0201552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sisler JJ, Nugent Z, Carpenter-Kellett T, et al. Comparative study of the perceptions of continuity of care of CRC survivors transitioned to primary care. J C O. 2017;35:96. doi: 10.1200/JCO.2017.35.5_suppl.96. [DOI] [Google Scholar]
- 67.Jones JM, Ferguson S, Edwards E, et al. Experiences of care delivery: endometrial cancer survivors at end of treatment. Gynecol Oncol. 2012;124:458–64. doi: 10.1016/j.ygyno.2011.10.037. [DOI] [PubMed] [Google Scholar]
- 68.Suryanarayana Deo S, Thejus T. Curative to palliative care-transition and communication issues: surgeons perspective. Indian J Palliat Care. 2013;19:120–3. doi: 10.4103/0973-1075.116706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carrillo GM, Carreño S, Lopez R, et al. Looking for Control at the End of Life Through the Bond: A Grounded Theory on the Hospital Discharge Process in Palliative Care. J Pain Symptom Manage. 2018;56:e44. doi: 10.1016/j.jpainsymman.2018.10.468. [DOI] [PubMed] [Google Scholar]
- 70.Broderick JP, Abir M. Transitions of Care for Stroke Patients: Opportunities to Improve Outcomes. Circ Cardiovasc Qual Outcomes. 2015;8:S190–2. doi: 10.1161/CIRCOUTCOMES.115.002288. [DOI] [PubMed] [Google Scholar]
- 71.Transitions in care: signovers in the emergency department. Proceedings of the Human Factors and Ergonomics Society Annual Meeting; 2004; Los Angeles, CA: SAGE Publications Sage CA; [Google Scholar]
- 72.Reay G, Norris JM, Nowell L, et al. Transition in Care from EMS Providers to Emergency Department Nurses: A Systematic Review. Prehosp Emerg Care. 2020;24:421–33. doi: 10.1080/10903127.2019.1632999. [DOI] [PubMed] [Google Scholar]
- 73.Patterson ME, Foust JB, Bollinger S, et al. Inter-facility communication barriers delay resolving medication discrepancies during transitions of care. Res Soc Adm Pharm. 2019;15:366–9. doi: 10.1016/j.sapharm.2018.05.124. [DOI] [PubMed] [Google Scholar]
- 74.Valverde PA, Ayele R, Leonard C, et al. Gaps in Hospital and Skilled Nursing Facility Responsibilities During Transitions of Care: a Comparison of Hospital and SNF Clinicians’ Perspectives. J Gen Intern Med. 2021;36:2251–8. doi: 10.1007/s11606-020-06511-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Johnson A, Guirguis E, Grace Y. Preventing medication errors in transitions of care: A patient case approach. J Am Pharm Assoc (2003) 2015;55:e264–74. doi: 10.1331/JAPhA.2015.15509. [DOI] [PubMed] [Google Scholar]
- 76.Safety WP, Organization WH . Conceptual framework for the international classification for patient safety version 1.1: final technical report. World Health Organization; 2009. [Google Scholar]
- 77.Schnipper JL, Samal L, Nolido N, et al. The Effects of a Multifaceted Intervention to Improve Care Transitions Within an Accountable Care Organization: Results of a Stepped-Wedge Cluster-Randomized Trial. J Hosp Med. 2021;16:15–22. doi: 10.12788/jhm.3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Earl T, Katapodis N, Schneiderman S. Care transitions. Making healthcare safer III: A critical analysis of existing and emerging patient safety practices. Agency for Healthcare Research and Quality (US); 2020. [PubMed] [Google Scholar]
- 79.Nahm E-S, Miller K, McQuaige M, et al. Testing the Impact of a Cancer Survivorship Patient Engagement Toolkit on Selected Health Outcomes. Oncol Nurs Forum. 2019;46:572–84. doi: 10.1188/19.ONF.572-584. [DOI] [PubMed] [Google Scholar]
- 80.Nordly M, Skov Benthien K, Soelberg Vadstrup E, et al. Accelerated transition from oncological treatment to specialized palliative care at home: Domus-A randomized controlled trial. Palliat Med. 2018;32 doi: 10.1177/0269216318769196. [DOI] [Google Scholar]
- 81.Rosenberg CA, Flanagan C, Brockstein B, et al. Promotion of self-management for post treatment cancer survivors: evaluation of a risk-adapted visit. J Cancer Surviv. 2016;10:206–19. doi: 10.1007/s11764-015-0467-6. [DOI] [PubMed] [Google Scholar]
- 82.Axelsen KR, Nafei H, Jakobsen SF, et al. Case managers experience improved trajectories for cancer patients after implementation of the case manager function. Ugeskr Laeger. 2015;177:1175–7. [PubMed] [Google Scholar]
- 83.Pandya C, Clarke T, Scarsella E, et al. Ensuring Effective Care Transition Communication: Implementation of an Electronic Medical Record-Based Tool for Improved Cancer Treatment Handoffs Between Clinic and Infusion Nurses. J Oncol Pract. 2019;15:e480–9. doi: 10.1200/JOP.18.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Raeymaekers B, Vandezande L, Leyn AM, et al. A feasible nurse-led project to improve the continuity in breast cancer care. Eur J Cancer. 2014;50 doi: 10.1016/S0959-8049(14)70079-6. [DOI] [Google Scholar]
- 85.Tepper S. A model for care: A transitions program designed to provide comprehensive care in treating individuals with malignant brain tumors. Smith Coll Stud Soc Work. 2003;73:337–57. doi: 10.1080/00377310309517689. [DOI] [Google Scholar]
- 86.Rochester-Eyeguokan CD, Pincus KJ, Patel RS, et al. The Current Landscape of Transitions of Care Practice Models: A Scoping Review. Pharmacotherapy . 2016;36:117–33. doi: 10.1002/phar.1685. [DOI] [PubMed] [Google Scholar]
- 87.Weaver SJ, Jacobsen PB. Cancer care coordination: opportunities for healthcare delivery research. Transl Behav Med. 2018;8:503–8. doi: 10.1093/tbm/ibx079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.vom Eigen KA, Walker JD, Edgman-Levitan S, et al. Carepartner Experiences With Hospital Care. Med Care. 1999;37:33–8. doi: 10.1097/00005650-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 89.Harrison A, Verhoef M. Understanding coordination of care from the consumer’s perspective in a regional health system. Health Serv Res. 2002;37:1031–54. doi: 10.1034/j.1600-0560.2002.64.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Coleman EA, Smith JD, Frank JC, et al. Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2:e02. :e02. doi: 10.5334/ijic.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Levine C. Rough Crossings: Family Caregivers’ Odysseys through the Health Care System (United Hospital Fund) Contemp Longterm Care. 1999;22:17 [Google Scholar]