Abstract
Objectives
Fundamental motor skills (FMS) are the foundation of children's movement, requiring tailored training and guidance for development. As an emerging training method, functional training is optimistic in promoting the development of children's fundamental motor skills. However, current studies have not assessed the effect of functional training on fundamental motor skills. This review aims to address this gap by evaluating the effects of functional training on fundamental motor skills.
Design
A search was conducted in five databases: PubMed, Scopus, ProQuest, Web of Science, and SPORT Discus, from January 2000 to June 2023.
Method
This search followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Results
The results of the search identified a total of twenty-six articles. Improvements were primarily demonstrated in the three main areas of fundamental motor skills: locomotor skills (n = 17), balance skills (n = 10), and object control skills (n = 2).
Conclusions
The results suggest that functional training programs can improve children's fundamental motor skills. Existing evidence also concludes that functional training significantly impacts locomotor and balance skills, whereas further research is required to confirm its positive effects on object control skills.
Keywords: Fundamental motor skill, Functional training, Locomotor skill, Object control skill, Balance skill, Children
1. Introduction
Fundamental motor skills (FMS) are the foundation of children's movement, comprising three key components: locomotor, object control, and balance skills [1]. Recent studies have highlighted their role in children's overall physical development and their ability to engage in various physical activities and sports. One key finding from these studies is that children with well-developed FMS tend to be more physically active. Children with a solid foundation in FMS feel more confident and competent in participating in different physical activities [2]. Moreover, increasing evidence suggests that the proficiency of FMS is bound up with an individual's health condition at all stages of life [3]. For example, children with inadequate FMS are at greater risk of developing sedentary behaviours and obesity in adolescence and adulthood [4]. In contrast, those without the opportunity to develop FMS may be susceptible to physical delays [5]. Unfortunately, the reality is that children worldwide have insufficient FMS. Many countries have reported low FMS proficiency among children, and many pre-adolescents lack the necessary mastery of these fundamental motor skills [[6], [7], [8]].
According to Gallahue's Hourglass Model of motor development theory, children learn motor skills sequentially, and the optimal age for FMS development is 5–7 years [9]. Furthermore, research indicates that children do not acquire FMS naturally as they grow older and must be trained and guided accordingly [2]. Numerous publications have demonstrated a significant positive correlation between FMS proficiency and training intervention [10]. Structured programs and targeted exercises incorporating endurance training, strength training, repetitive practice, and skill-specific drills have been commonly utilised to improve FMS. This evidence highlights the importance of implementing training interventions to improve FMS proficiency. However, several systematic reviews show that existing training methods have not demonstrated comprehensive effectiveness in improving the performance of FMS. Moreover, these methods increase injury risks, especially in children [5].
Researchers and practitioners are actively exploring more efficient ways to improve FMS. During this process, the extensive popularity of functional training has garnered significant interest from researchers. Functional training is an exercise program that aims to improve an individual's ability to perform everyday activities and movements efficiently and reduce the risk of injury [11,12]. It emphasises the development of coordination, stability, and flexibility through fundamental movement patterns and basic human body postures. Functional training is also a dynamic approach which focuses on coordinating the overall body activity of the muscles, bones, and joints to achieve specific goals [13]. According to specific training goals, the exercises and techniques used in functional training may vary significantly. Generally, it can be categorised as pure and mixed functional training [12]. In contrast, the main difference is mixed functional training integrates with various other training methods, such as functional resistance training and functional balance training [14,15]. The core principle behind them is the same: it mainly emphasises the closed kinematic chain [16]. These properties distinguish it from more conventional exercise methods, highlighting why it can make the body have the effect of one plus one being greater than two in different fields of application, including rehabilitation and sports training. It effectively enhances motor skills in children with cerebral palsy and movement disorders [17,18]. In addition, it can also improve athletic performance, promote physical fitness, and reduce the risk of sports-related injuries in healthy children [[19], [20], [21], [22]].
Functional training has many properties and advantages strongly associated with the development of FMS. This understanding has led to increased research studies using functional training as a potential intervention to improve the FMS of children. However, the current state of knowledge regarding the impact of functional training on children's ability to enhance FMS is unclear. Therefore, this systematic review was conducted to evaluate the effect of functional training on FMS in children.
2. Materials and methods
2.1. Protocol and Registration
The systematic review was structured and reported according to the Preferred Reporting Items for Reporting Systematic Reviews and Meta-Analyses guidelines [23]. The study was registered in the International Prospective Register of Systematic Reviews, CRD42022313408.
2.2. Search Strategy
The detailed literature search was conducted across five databases: PubMed, Scopus, ProQuest, Web of Science, and SPORT Discus, covering studies published between January 2000 and June 2023. The following search keywords were used: (“functional training” OR “functional exercise” OR “functional task training” OR “functional correction training” OR “functional fitness training”) AND (“fundamental motor skill” OR “fundamental movement skill” OR “basic motor skill” OR “motor competence” OR “gross motor skill”) AND (“child∗” OR “adolescent” OR “kid” OR “youth”). Additionally, this study identified other potential papers by conducting a citation search on Google Scholar. Apart from the primary systematic electronic searches, manual searches were undertaken on the reference lists of all the articles included in the study.
2.3. Eligibility criteria
The review employed PICOS (population, intervention, comparison, outcome, and study design) principles to establish the inclusion criteria [24]. Records included only pertained to functional training for children's fundamental motor skills. Studies were included when they satisfied the following criteria:
(1) Full text published in English. (2) The subjects included were children under the age of 18; (3) The study design involves randomised controlled trials (RCTs) or non-RCTs with two or more groups or a one-group design with a pre-post-test; (4) The intervention involves functional training, including the methods, modes associated with functional training, and their integration with other training methods; (5) The outcomes of the study reported the development of FMS.
Studies meeting the following criteria were not considered: (1) Studies that did not conduct functional training interventions or the experiment did not include pre-test or post-test; (2) Studies that did not report any outcomes or detailed data on FMS; (3) Research subjects are not children or age-inappropriate; (4) Reviewed articles, conference papers, abstracts, and studies published in languages apart from English.
2.4. Study selection
The entire collection of articles was integrated into Mendeley and subjected to a duplication check. In the initial stage, two independent reviewers (ZD, KS) examined the titles and abstracts following the predefined inclusion and exclusion criteria. Additionally, articles that couldn't be conclusively identified based on their title or abstract underwent a thorough full-text assessment. Subsequently, a full-text review was conducted to extract information and data from articles identified and agreed to be included. In the event of any disagreements during this process, a discussion was held to reach a consensus. If mutual agreement could not be reached, a third reviewer (YC) was included to settle the argument.
2.5. Data Extraction
Specific data was extracted from the articles and recorded in a specially designed Excel table. The recorded data included the following: (1) authors, year, and country; (2) sample characteristics (e.g., age, gender, and sample size); (3) intervention (e.g., content, duration, intensity, and frequency); (4) study design; (5) The outcomes mainly include three aspects of fundamental motor skills (e.g., locomotor, object control, balance) and their specific test results (e.g., pre and post). Two separate reviewers went through this process independently.
2.6. Quality assessment
The Physiotherapy Evidence Database (PEDro) scale was employed to examine the standard of the experimental procedures. The scale has been demonstrated to have good validity and reliability for evaluating the methodological quality of clinical trials [25,26]. It evaluates four aspects of the research method: the randomisation process, the blinding procedure, the group comparison, and the data analysis. It comprises a checklist of 11 items scored by responding with a yes (1 point) or no (0 points). Criteria 2–11 were used to calculate the PEDro score. A higher score indicates a higher level of methodological quality. It proposes that these scores may be evaluated as follows: 9–10 represents excellent quality; 6–8 represents good quality; 4–5 represents fair quality; and a score smaller than four represents poor quality. Two reviewers evaluated the articles independently. When faced with conflicting views, the reviewers discussed the issue or sought an evaluation from a third reviewer.
3. Results
The search results were reviewed and assessed by establishing specific criteria for including and excluding literature. This systematic review ultimately identified 26 articles, encompassing both RCTs and non-RCTs, that investigated the impact of functional training on children's fundamental motor skills. The publications encompassed a period from 2000 to 2023. Research in the field has seen significant advancement since 2014, resulting in an increased number of articles. 22 of the 26 articles were published within the last ten years.
3.1. Study selection
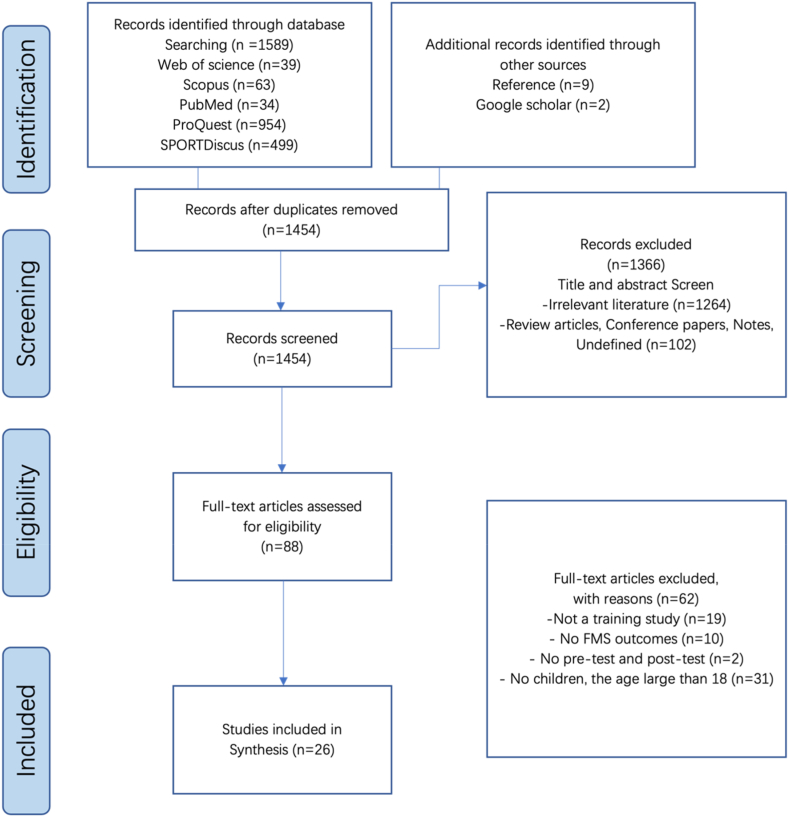
The original search yielded 1589 articles (PubMed = 34, Scopus = 63, ProQuest = 954, Web of Science = 39, SPORT Discus = 499). An additional 11 studies were included by reference checking (n = 9) and Google Scholar (n = 2). When removing duplicates (n = 146), an initial screening was conducted based on article titles and abstracts, resulting in 88 remaining articles. Subsequently, these selected articles underwent a thorough full-text review. Finally, 26 articles met the inclusion criteria and were included in the final analysis. The detailed evaluation process is depicted in Fig. 1.
Fig. 1.
Article selection process flow chart (PRISMA).
3.2. Quality assessment
All studies were evaluated according to the PEDro criteria. Table 1 presents the assessment findings. Thirteen articles achieved a score of five points, signifying acceptable quality. Meanwhile, one piece scored six points, eight articles scored seven points, and three reached eight points, all indicating good quality. Solely one study showcased excellent quality and attained a perfect score of 10. The mean score was 6.19, and no low-quality studies were included, indicating that the overall quality of the research was good. All the articles met the following five assessment criteria: similar at baseline, 15 % dropouts, intention-to-treat analysis, between-group comparisons, and point measurements and variability [27]. Furthermore, subjects and experimenters were blinded only in one study [28], and four articles blinded the assessor.
Table 1.
Summary of methodological quality assessment scores.
| Part 1 | Part 2 | Part 3 | Part 4 | Part 5 | Part 6 | Part 7 | Part 8 | Part 9 | Part 10 | Part 11 | Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Norambuena et al. (2021) [29] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Baron et al. (2020) [30] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Katsanis et al. (2021) [31] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Laurent et al. (2018) [32] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Labib (2014) [33] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Yildiz et al. (2018) [34] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Song et al. (2014) [35] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Liao et al. (2017) [36] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Marta et al. (2019) [37] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Eather et al. (2016) [38] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Carvutto et al. (2021) [39] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Baron et al. (2020) [51] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Bonney et al. (2019) [40] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Gorter et al. (2009) [17] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Mikołajczyk et al. (2014) [50] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Emara et al. (2016) [42] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Ansa et al. (2020) [43] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Surana et al. (2019) [18] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Ketelaar et al. (2001) [44] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Salavat et al. (2017) [45] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Blundell et al. (2002) [46] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Mikołajczyk et al. (2014) [50] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Ahl et al. (2005) [47] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Farrokhian et al. (2021) [48] | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Van Tittelboom et al. (2023) [49] | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Abd-Elfattah et al. (2022) [28] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
Part 1, eligibility criteria specified; Part 2, random allocation; Part 3, concealed allocation; Part 4, groups similar at baseline; Part 5, participant blinding; Part 6, therapist blinding; Part 7, assessor blinding; Part 8, fewer than 15 % dropouts; Part 9, intention-to-treat analysis; Part 10, between-group statistical comparisons; Part 11, point measures and variability data.
3.3. Participant characteristics
Participants in the 26 studies can be grouped into two categories: 12 studies on healthy children [[29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39]] and 14 on children with health conditions [17,18,28,[40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50]]. The 26 studies evaluated 1133 participants, with 834 healthy children, including 440 boys and 394 girls, with a mean age ranging from 8.54 to 17.0 years. Three hundred seventy-one children had related health conditions, including 174 boys and 193 girls, with a mean age ranging from 4.5 to 15.06 years old (Table 2). In the majority of studies, the sample size fell between 10 and 50. The minimum sample size was 5 [45], while the maximum was 321 [31]. In terms of gender distribution, four studies were conducted on girls [33,36,40,48], and six focused on boys [30,34,35,37,39], while 15 articles covered both boys and girls [17,18,28,29,31,32,38,[41], [42], [43], [44], [45], [46], [47],49], only one article did not report gender [50]. Participants in seven studies were athletes, including soccer [30,39,51], tennis [34], handball [33], baseball [35], and judo players [29]. Five studies were on ordinary children [31,32,[36], [37], [38]]. In the remaining fourteen studies of children who had health conditions, the majority of the individuals were affected by cerebral palsy [17,18,28,[42], [43], [44], [45], [46], [47],49] and intellectual disabilities [41,48,50].
Table 2.
Research specific information.
| Study | Design | Participant | Experimental | Control | Result |
|---|---|---|---|---|---|
| Norambuena et al. (2021) [29] | PPS 5 weeks |
Elite athletes Sports: Judo SS: 10 EG: 10; 8 B/2 G; Age: 15.4 ± 2.8yr; |
IV: Suspension-training INT: Intensity gradually increased Freq: 3/week Time: 20min |
No | Single-leg horizontal jumping (right leg↑; left leg↑), Sorensen↑, SAR↑, Y balance (arm↑; leg↑). Grip strength ∼; prone instability test performance ∼; |
| Baron et al. (2020) [30] | PPS 12 weeks |
Elite athletes Sports: Football SS: 20 EG: 20 B; Age: 16.8 ± 0.6yr; |
IV: Functional training Time: 70–90min |
No | Functional state (FMS1↑, FMS2↑, FMS3↑); Speed and acceleration Tests (0–5m ∼, 5–20m↑, 10–30m↑, 0–30m↑); Velocity↑. |
| Katsanis et al. (2021) [31] | PPS 8 weeks |
Ordinary children SS: 321; 158 B/163 G; Age: 16.54 ± 0.91yr; EG: 154; 76 B/78 G; Age: 16.52 ± 0.88yr; CG: 167; 82 B/85 G; Age: 16.56 ± 0.94yr; |
IV: Suspension-training INT: Increased by 50 %/2weeks. Freq: 2/week Time: 45min |
IV: Regular PE class Freq: 2/week Time: 45min |
In EG (SLJ↑ p < 0.001, Sit-ups for 30 s↑ p < 0.001, push-up↑ p < 0.001, handgrip↑ p < 0.001); in CG ∼. In EG, increased in motivation to participate in the PE class |
| Laurent et al. (2018) [32] | RCTs 6 weeks |
Ordinary children SS: 28; 46 % B/54 % G; Age: 9.3 ± 1.5yr; EG: 17; 58.5 % B/41.5 % G; Age: 9.82 ± 1.22yr; CG: 11; 27.3 % B/72.7 % G Age: 8.54 ± 1.57yr; |
IV: Suspension training Freq:2/week Time: 60min |
IV: Regular activities Freq: 2/week Time: 60min |
Pull-Up performance↑(P = 0.01) Lift↑, and FMS score↑, relative to CG. skill-related fitness (SLJ ∼, SR ∼) |
| Labib (2014) [33] | PPS 10 weeks |
Ordinary athletes Sports: Handball SS: 20 G EG: 10 G; Age: 13 ± 1.5yr; Training experience 3 ± 0.7yr CG: 10 G; Age: 14 ± 1.8yr; Training experience 3 ± 0.8yr |
IV: Functional training Freq: 3/week Time: 60min |
IV: Normal training Freq: 3/week Time: 60min |
Standing Stork Test↑, DB↑, Static strength↑ and Running shoot↑. Both Handgrip Strength↑ and Static strength test↑ improved in two group, but No Significant Difference between them. |
| Yildiz et al. (2018) [34] | PPS 8 weeks |
Ordinary athletes Sports: Tennis SS: 28 B; Age: 9.6 ± 0.7yr; Training experience 3.1 ± 1.3yr EG1: 10 B EG2: 10 B CG: 8 B |
EG1 IV: Functional training Freq:3/week Time: 65–75min EG2 IV: Traditional training Freq: 3/week Time: 65–75min |
IV: Normal tennis training Freq: 3/week Time: 65–70min |
In CG, FMS scores↓ and other parameters ∼. In EG1, DB↑ FMS↓ and other parameters ∼. In EG2, all parameters ↑, (the vertical jump performances↑, flexibility↑, agility↑, DB↑, SB↑, FMS data↑), between groups showed a significant difference, no big difference for right left DB. |
| Song et al. (2014) [35] | PPS 16 weeks |
Elite athletes Sports: Baseball SS: 62 B EG: 31 B; Age: 17.0 ± 1.06yr; CG: 31 B; Age: 16.62 ± 0.94yr; |
IV: Functional Screen training INT: NM Freq: 3 T/week Time: NM |
IV: Traditional training Freq: 3/week Time: NM |
Strength↑ and flexibility↑, hand grip strength↑ 12 %, bench-press↑ 9 % |
| Liao et al. (2017) [36] | RCTs 12 weeks |
Ordinary children SS: 144 G; Age: 12.47 ± 0.57yr EG: 72 G; CG: 72 G; |
IV: Functional strength training INT: a moderate intensity Freq: 3/week Time: 45min |
IV: Traditional strength training INT: a moderate intensity Freq: 3/week Time: 45min |
FMS data↑, deep squat↑, turn stability↑, muscular strength↑, flexibility↑ and power↑, FST is better at improving the quality of movement Curl-ups, SAR and SLJ. |
| Marta et al. (2019) [37] | RCTs 8 weeks |
Prepubescent children SS: 57 B EG1: 19 B; Age: 10.71 ± 0.43yr EG2: 20 B; Age: 10.92 ± 0.45yr CG: 18 B; Age: 10.81 ± 0.57yr |
EG1 IV: Resistance training INT: low to moderate Freq: 2/week Time: 45min EG2 IV: Suspension training INT: low to moderate Freq: 2/week Time: 45min |
IV: Regular PE course INT: low to moderate Freq: 2/week Time: 45min |
1-kg ball throw large↑ (P < 0.001, 2p = 0.463), 3-kg ball throw medium↑ (P < 0.001, 2p = 0.395), and time-at-20m test small ES. no big difference between in the CVJ or the SLJ. but in ST training the CVJ↑, SLJ↑. |
| Eather et al. (2016) [38] | RCTs 8 weeks |
Ordinary children SS: 96; 46 B/50 G; Age: 15.4 ± 0.5yr; EG: 51 CG: 45 |
IV: CrossFit Teens Freq: 2/week Time: 60min |
IV: Regular PE class Freq: 2/week Time: 60min |
SAR↑ (+3.0 cm, P < 0.001), SLJ↑ (+0.1 m.021) and SR (+10.3laps, P = 0.019) SAR↑ Curl-up test↑, push-up ↑, SLJ↑ grip strength↑, SR test ↑ |
| Carvutto et al. (2021) [39] | RCTs 8 weeks |
Ordinary children Sports: Score SS: 28 B; Age: 12.6 ± 8.8; EG: 14 B CG: 14 B |
IV: High-intensity functional training INT: High-intensity Freq: 3/week Time: Lasts 90 min |
IV: Traditional training based on technical and tactical abilities. Freq: 3/week Time: 90min |
Group x Time-agility ↑ no significant in sprint performance |
| Baron et al. (2020) [51] | PPS 12 weeks |
PT: Elite athletes Sports: Football SS: 20 B EG: 20 B; Age: 16.8 ± 0.6yr; |
IV: Functional training Time: 70–85min |
No | Functional state↑; FMS↑, FMS↑, FMS3↑; CM, power and height↑ CMJ without swing power and height↑, SQUAT Jump power and height↑ |
| Bonney et al. (2019) [40] | RCTs 14 weeks |
PT: Obesity SS: 52 G EG: 26 G Age: 14.4 ± 0.9yr CG: 26 G Age: 14.3 ± 0.8yr |
IV: Task-oriented functional training Freq: 1/week Time: 45min |
IV: Wii Fit intervention Freq: 1/week Time: 45min |
Aerobic↑, coordination↑, knee extensors strength↑, dorsiflexors↑, plantar flexors↑, anaerobic↑ in both groups. lower extremity functional strength↑, manual dexterity↑, balance↑ in both groups. These changes were not different between groups. |
| Gorter et al. (2009) [17] | PPS 9 weeks |
Cerebral Palsy SS: 13; 8 B/5 G EG: 13; 8 B/5 G; Age: 9.9 ± 1.15yr normal intelligence (n = 1), mild mental retardation (n = 12). CP and at GMFCS level 1 (n = 12) or level 2 (n = 1). |
IV: Functional physical training Freq: 1/week Time: 30min |
No | Aerobic Endurance HR6↓ T max↑; walking distance and velocity ↑, Ambulation TUDS Seconds↓. VO2max ↑ 9 %, max treadmill time↑ 23 %, walking distance ↑ 7 %, ambulation ↑ 21 %. |
| Mikołajczyk et al. (2014) [50] | PPS 12 weeks |
Intellectual disability SS: 34; 28 B/6 G; moderate ID, mean IQ 45.1 ± 3.3; Age: 15.06 ± 0.9yr; EG: 17; CG: 17; |
IV: Obligatory physical education classes + original dual-task functional training Freq: 3/week Time: 45min |
IV: Regular PE class Freq: 2/week Time: 45min |
Balance↑ (eyes open conditions, eyes closed conditions), path length of the center of pressure (eyes open conditions↓ significant shortening length by 28 %, eyes closed conditions↓, significant shortening 36 %). |
| Emara et al. (2016) [42] | RCTs 12 weeks |
Spastic diplegia SS: 20; 7 B/13 G; Age: 6–8 EG: 10; 4 B/6 G Age: 6.9 ± 0.6yr CG: 10; 3 B/7 G Age: 6.6 ± 0.7yr |
IV: Traditional therapeutic exercises + body-weight suspension training Freq: 3/week Time: 40 + 30min |
IV: Wii Fit intervention Freq: 1/week Time: 45min |
standing↑, walking↑, 10-Meter walking speed↑. five times sit to stand, walking speed, sit to stand transitional skills, no significant difference between groups |
| Ansa et al. (2020) [43] | PPS 8 weeks |
Cerebral Palsy SS: 10; 7 B/3 G SS: 10; 7 B/3 G Age: 14.4 ± 1.53yr; Type of CP: 4 Diplegia/1 Hemiplegia/5 Quadriplegia |
IV: Community-based functional aerobic exercise INT: 40–80 % max heart rate Freq: 4/week Time: 50min |
No | GMF D-standing ↑ 8.2 %, E-walking + running + jumping ↑ 5.12 %, walking distance↑ 6.09 %. physical health ↑ 105.04 %, by children parent proxy. And physical health ↑ 60.00 %, by Self-reported. |
| Surana et al. (2019) [18] | RCTs 9 weeks |
Unilateral spastic cerebral palsy SS: 24; 10 B/14 G EG: 12; 5 B/7 G Age: 5.8 ± 2.3yr GMFCS, 5 I/7 II CG: 12; 5 B/7 G Age: 5.1 ± 2.6yr GMFCS 3 I/9 II |
IV: LE intensive functional training Freq: 5/week Time: 120min |
IV: Obligatory physical education classes + NR | 1MWT↑, ABILOCO-kids↑, single-leg stance↑, fast velocity↑, 30-s chair rise↑. LIFT improved more than H-HABIT. no significant differences between LIFT and H-HABIT for self-selected walking velocity |
| Ketelaar et al. (2001) [44] | RCTs 18 months |
Spastic cerebral palsy SS: 55; 33 B/22 G; Age: 2–7yr EG: 28; 16 B/12 G Age: 54 ± 20 months; Cerebral palsy distribution: 16 Hemiplegia/5 Diplegia/6 Quadriplegia. CG: 27; 17 G/10 G; Age: 56 ± 20 months Cerebral palsy distribution: 16 Hemiplegia/6 Diplegia/6 Quadriplegia. |
IV: Functional physical therapy | IV: Traditional therapeutic exercises + the treadmill Freq: 3/week Time: 40 + 30min |
GMFM↑ and PEDI score ↑in both groups; basic gross motor abilities↑, no differ between groups. The mean scores↑ higher than in the CG. functional skills in daily situations↑, self-care and mobility activities↑. |
| Salavat et al. (2017) [45] | PPS 18 weeks |
PT: Cerebral palsy and cerebral visual impairment SS: 5 2 B/3 G; Cerebral palsy; Age:114 ± 52 month; distribution: 5 Spastic, GMFCS classified levels: 2 I/1 II/1 V/1 IV; |
IV: Functional therapy programmed Freq: 3/week Time: 30min |
No | Gross motor functioning↑, Functional Skills↑ |
| Blundell et al. (2002) [46] | PPS 4 weeks |
PT: Cerebral palsy SS: 8; 7 B/1 G EG: 8; 7 B/1 G; Age: 6.3 ± 1.3yr Cerebral palsy distribution: 7 spastic Diplegia/1 Quadriplegia. |
IV: Functional strength training +a group circuit training INT: intensive repetitive practice Freq: 2/week Time: 60min |
IV: Hand-Arm Bimanual Intensive Therapy Freq: 5/week Time: 120min |
Isometric strength↑; Left and right Lateral Step-up ↑; time of 10-m walk↑; stride length↑. |
| Mikołajczyk et al. (2014) [50] | RCTs 12 weeks |
Moderate mental disabilities SS: 34 Age: 15.06 ± 0.9yr; EG: 17 CG: 17 |
IV: Unstable-surface functional exercises Freq: 3/week Time: 45min |
IV: Did not perform any exercises | Static balance - COP deviation range↑, Path length↓, Path area↓. Eye open and eye closed. |
| Ahl et al. (2005) [47] | PPS 5 months |
PT: Children with cerebral palsy SS: 14; 11 B/3 G; Age: 1 year 6 months to 6 years. With diplegia and tetraplegia cerebral palsy; EG: 8; 7 B/1 G; GMFCS classified between levels II–V; |
IV: Goal-directed functional therapy Freq: 2/week Time: NM |
IV: Reference normalisation | 76 goals fulfilled completely, 19 partially completed; gross motor function↑; self-care performance↑; mobility ↑; social function↑ |
| Farrokhian et al. (2021) [48] | RCTs 5 weeks |
Intellectual disability SS: 30 Gender: G EG: 15; CG: 15 Age: Elementary school students(Not specific) |
IV: Functional training Freq: 3/week Time: 45–60min |
IV: Did not perform any exercises | SB↑, DB↑, flexibility↑, and student performance are statistically significant. |
| Van Tittelboom et al. (2023) [49] | PPS 4 weeks |
PT: A diagnosis of bilateral spastic CP SS: 36 Gender: 19 B/17 G; Age: 8.58 ± 1.96yr QFT: 24 Gender: 10 B/14 G; GMFCS level II: 15, GMFCS level III: 9; Age: 8.5 ± 1.84yr FT: 12 Gender: 9 male/3 female; GMFCS level II: 7, GMFCS level III: 5; Age: 8.83 ± 2.23yr |
IV: Functional training INT: NR Freq: 5/week Time: 4.5 h |
IV: Qualitative functional training INT: NR Freq: 5/week Time: 4.5 h |
QFM: ↑ with qualitative functional training (QFT), but not improved with function training. GM88-D and E ↑ (QFT) TCMS: static and dynamic balance ↑ (QFT) |
| Abd-Elfattah et al. (2022) [28] | RCTs 12 weeks |
PT: Spastic hemiplegic cerebral palsy Sports: NR SS: 66 Gender: 42 B/24 G. EG: 24 Gender: 22 B/11G; GMFCS level I: 10, GMFCS level II: 23; Age: 11.31 ± 0.62yr HT: 142.55 ± 4.1 cm; BM: 38.31 ± 3.93 kg; CG: 12 Gender: 20 B/13 G; GMFCS level I: 13, GMFCS level II: 20; Age: 11.11 ± 0.63yr HT: 142.41 ± 4.21 cm; BM: 37.12 ± 2.83 kg; |
IV: loaded functional strengthening exercises INT: NR Freq: 3/week Time: 60 min |
IV: physical therapy INT: NR Freq: 3/week Time: 60 min |
6MWT: the 6MWT in EG (20.09 %) and CG (9.69 %) ↑, EG > CG. |
Abbreviation: PT, participant; SS, sample size; EG, experiment group; CG, control group; PPS, pre-post-test; HT, height; BW, body weight; IV, Interventions; INT, intensity; Freq, frequency; ES: effect size; GFT, general physical fitness; LS, locomotor skills; Bs, balance skill; OCS, objective control skills; B, boy; G, girl; NM, not mentioned; FMS, functional movement screen; GMFCS, gross motor function classification system. DB, dynamic balance; SB, Static balance; SAR, sit-and-reach; SLJ, standing long jumping; T, times; FST, functional strength training; ST, Suspension training. SR, shuttle run; CVJ: countermovement vertical jump; QFM: Qualitative functional training; 6MWT: 6-min walk test.
Most studies reported data on the participants' height and weight but did not include information on their body mass index (BMI). In eight articles, the weight and height of the subjects were not specified or provided. These eight articles were about children with cerebral palsy [17,18,[44], [45], [46], [47], [48], [49]]. Seventeen articles did not report the subject's BMI data [17,18,28,[33], [34], [35],37,[41], [42], [43], [44], [45], [46], [47], [48], [49], [50]]. In the remaining nine articles, participants in eight studies were classified as normal weight (BMI 19.2–24 kg/m2) [[29], [30], [31], [32],36,38,39,51]. One research showed children as overweight (BMI 27.7 ± 3.9 kg/m2) [40]. Table 2 presents the specific information of these studies.
3.4. Intervention characteristics
The intervention characteristics were divided, focusing on the following dimensions: type of functional training, training duration, frequency, and intensity.
The effects of functional training are the targeted topic of this systematic review. All the intervention groups in the studies employ functional training programs. These interventions can be classified into two categories. The first category encompassed pure functional training programs [12] without any combination with other training methods. It was used in 12 studies [17,28,30,33,34,39,41,44,45,47,48]. The other type used a hybrid programming of functional training methods. Three studies used functional strength training [36,46,49], while suspension training was used in five studies [29,31,32,37,42]. The other six used CrossFit [38], Lower-Extremity intensive functional training [18], task-oriented functional training [40], original dual-task functional training [41], functional movement screen training [35], and functional aerobic exercise [43].
The intervention duration varied between four weeks [46,49] and eighteen months [44]. In most of the studies, the duration of the intervention was eight [31,34,[37], [38], [39],43] or twelve weeks [18,30,36,41,42,49,51]. Furthermore, the shortest intervening time of each session is 20 min, while the longest intervention time can be up to 120 min [18], with 45 [31,36,37,[40], [41], [42], [43],48,50] to 60 min [28,[32], [33], [34],38,46] being the most common. Only two articles did not report the intervention duration for each session [35,44]. The weekly intervention frequency in most studies is two [17,31,32,37,38,46,47] to three times [29,[33], [34], [35], [36],39,41,42,45,48,50] per week. Three articles implemented an intervention frequency ranging from 4 to 5 times [18,43,49]. Notably, three studies did not provide the frequency information [30,44]. Training intensity is a crucial aspect of the training process, as well as duration and frequency. Only four articles explicitly reported training intensity. Three of these studies reported low to moderate-intensity interventions [36,37,43], while one utilised a high-intensity approach [39]. The rest of the articles did not clearly state the intensity of their interventions.
3.5. Outcomes
The effects of functional training on fundamental motor skills were grouped and analysed in terms of locomotor skill performance, balance skill performance, object control skill performance, and fundamental movement screen score.
3.5.1. Effects of functional training on locomotor skills
Locomotor skill is the primary measure of the children's proficiency in FMS. The effect of functional training on locomotor skills was mainly reflected by data such as walking and running distance, speed, acceleration, agility, and jump performance. These data were evaluated using a series of test methods, including a walking test (30s, 1 min, 2 min, 6 min) [18,28,42,43,46,49], shuttle run (10m, 25m) [32,38], sprints test (10m, 20m, 50m) [34,36,39], standing long jump test [31,32,[36], [37], [38]], and timed up and downstairs test [17] to test the level of locomotor skills. Moreover, the Gross Motor Function (GMF) Measure test was the most commonly utilised evaluation tool for children with health conditions, which uses a four-point scale response format with 66 [43,47] and 88 [28,42,46] items separated into five dimensions. It has sufficient validity and reliability to test FMS in children aged 4–12 with cerebral palsy [52] and has been confirmed in children from different regions and countries [53,54].
In this review, seventeen studies reported findings on locomotor skills [17,18,28,[30], [31], [32],34,[37], [38], [39],[42], [43], [44], [45], [46], [47],49], most showing improvements in the variables. Children performed better on jumping tests [[29], [30], [31],38]. One study revealed a mean difference of the single-leg horizontal jump changed by 29.6 cm, and the effect size (EF) of Cohen's d is 1.4 [29]. The mean length of the standing long jump increased in the experimental group by 36 cm in the research that focused on untrained girls [29], and in another study that focused on prepubescent boys, the mean difference changed by 11 cm [31]. The mean of the test results in the countermovement vertical jump reached an improvement of 1.79 cm [31]. Improvements in running performance were most evident in the reduction of sprint test time [17,30,34,38,39]. One research pointed out a 0.3-s decrease in mean time of 12-13-year-old girls on the 50-m sprint test [36]. Another study showed that prepubertal tennis players performed better in the functional training group during the 10-m acceleration test, with a mean time of 0.9 s faster than the baseline [34]. The mean number of laps of shuttle run for girls increased by 18.3 laps with an EF of 0.1, and for girls by 14.1 laps with an EF of 1.5 during the same period after the intervention with Australian adolescents [38]. Furthermore, subjects with cerebral palsy demonstrated an improvement in their walking abilities in the GMF test [42,43,45,47,49] and the 6-min walk test (6 MWT) after the functional training intervention [17,18].
However, the analysis of specific variables from the three included studies showed no statistically significant differences between groups. Examples include standing long jump distance (p = 0.16) and countermovement vertical jump height (p = 0.29) for boys aged 10–11 [37], shuttle running speed (p = 0.12) for children aged 7–12 years who regularly train in at least one sport [32], and walking speed (p = 0.079) for children with cerebral palsy [46].
3.5.2. Effects of functional training on balance skills
Balance skills are an essential component of fundamental motor skills. When it comes to testing balance skills, the options are extensive. Single-leg stance tests [18,48], five-times sit-to-stand tests for kids [42], prone instability tests [29], 5 m timed up-and-go tests [33], Y-balance tests [34], stabiliser platform ALFA tests [41] and trunk control measurement scale (TCMS) are among the tests used. These tests measure coordination ability, joint stability, dynamic balance, and static balance.
Ten studies assessed the balance skills of children [18,29,[33], [34], [35],[40], [41], [42],48,50]. Depending on the statistics, when testing with the Y-balance test, one study indicated that the test results of both legs and arms experienced significant improvements after five weeks. The maximum increase was 11.8 %, and the EF was 1.8 [29]. Another study concentrating on athletics discovered that the dynamic balance was enhanced, with a mean score difference of 11 between the pre and post-test [34]. Static balance is an essential part of rehabilitation and exercise. One research study found that intellectually disabled children improved in single-leg standing. The mean time of the experimental group improved by 4.73s following the test, much more than the control group's [48]. When using the stable platform ALFA to assess the static balance skill of children with cerebral palsy, regardless of whether the eyes were open or closed, the path length test results indicated that the static balance skill level varied significantly after the experiment [42].
However, one study did not discover a statistically significant difference between the groups on the mean sway of the centre of pressure (COP) along the medio-lateral (M/L) (p = 0.39) and anterior-posterior (A/P) (p = 0.75) in individuals with intellectual disability [41].
3.5.3. Effects of functional training on object control skills
Data on the efficacy of object control skills were limited. Only two studies measured object control skills. One employed the medicine ball throw test [37], demonstrating that children could throw balls of different weights better after functional training. The performance for the 1-kg ball throw increased by 5.94 %, with a mean difference of 22.25 cm, while that for the 3-kg ball throw increased by 8.82 %, with a mean difference of 21.3 cm. According to another study that used the Nine-Hole Peg Test [46], which measures how well children with cerebral palsy can reach and put things down, children took less time to perform the same task after functional training. The results of the studies demonstrate a positive impact of functional training on object control skills. However, more is required to support the findings due to the small sample size.
3.5.4. Functional movement screen test results
Functional movement screening is an innovative action pattern evaluation tool that may be broadly applied to examining the fundamental motor function of varied populations. It can correctly reflect the FMS of children. A total of six studies utilised the Functional Movement Screen scale to assess the FMS state of children [30,32,[34], [35], [36],51]. The test findings demonstrated that the functional training group's test scores had significantly increased, and there were significant differences between the inter-group outcomes after the training intervention. Baron et al. (2020) used three tests of the Functional Movement Screen. The results show significant differences before and at the end of the 12-week functional program: deep squat (p = 0.004), hurdle step (p = 0.012), and in-line lunge (p = 0.001) [30]. Meanwhile, three studies utilised all seven test items (The Deep Squat, Hurdle Step, In‐Line Lunge, Shoulder Mobility, Straight Leg Active Raise, Trunk Stability Push Up, and Rotational Stability) of the Functional Movement Screen and compared the total scores between groups. Laurent et al. (2021) reported that after six weeks of intervention, the total score of the seven tests in the functional training group increased to a higher level [32]. Yildiz et al. (2018) found a significant difference in Functional Movement Screen scores between the traditional training group and functional training group (p < 0.001) [34]. Similarly, Liao et al. (2017) also observed that there is a significant difference in the total score between the traditional strength training group and the functional strength training group (p < 0.05) [36].
4. Discussion
This study differs from other published reviews because it aims to evaluate the effect of functional training programs on improving children's FMS. Furthermore, there is a lack of prior reviews comprehensively summarising the effects of functional training on FMS. Therefore, the current study explored and summarised the effects. The results give a general insight into the development of FMS and the impact of functional training on children's FMS. The primary findings suggest that functional training has a positive effect on enhancing children's FMS.
The positive results of functional training in helping children improve their fundamental motor skills are consistent with previous research using functional training in other areas, such as motor development, sports training, and functional therapy. The effectiveness could be due to functional training, which is purposeful training for specific target muscle groups to improve the neuromuscular system [55]. Unlike traditional methods solely concentrating on muscle shape or volume, functional training emphasises the coordination between motor nerves and muscle groups [56]. Therefore, functional training may be a more effective and promising approach.
This systematic review found the greatest improvements in locomotor skills in running performance (speed and agility) and jumping performance, such as long jumping and countermovement vertical jumping. Such results indicate that functional training does improve children's locomotor skills. These results align with a systematic review of functional training on sprinting and jumping in athletes [57]. It is also consistent with detailed research on specific sports that improved adult basketball players' and runners' speed and agility [58,59]. Furthermore, older people with disabilities can improve their mobility with functional training, while those undergoing rehabilitation can benefit from targeted strengthening and movement patterns [60]. The consistent positive outcomes of functional training across various populations indicate that its efficacy on locomotor skills among children is not occasional.
Additionally, another observation suggests that functional training may affect specific locomotor skills differently. Among the six locomotor tests involving jumping movements, the mean growth rates for hopping, leaping, and jumping [31,32,[36], [37], [38]] were comparatively lower than those observed for running and galloping [28,42,46,49] after functional training. The observation aligns with similar studies on children from Hong Kong [61] and Japan [62]. Specific research analyses suggest that this discrepancy could be attributed to the increased demand for adequate muscle strength in the lower limbs during jumping [63]. Furthermore, within the included studies, a minority suggest that children did not demonstrate improvements in their locomotor skills [32,37,46]. This contrasts with our initial expectations and the findings typically seen in mainstream research. The reasons may be multifaceted and complex. Variations in sample size, experimental design, training intensity, and duration will impact the outcomes. For instance, one research used a non-randomised controlled trial as the experimental design and mixed functional training with other training methods [46], and a few had a duration of just 4–8 weeks [32,37,46]. In contrast, studies that implemented interventions lasting 12 weeks [30,36] or longer [40,45], as well as those that employed pure functional training [39,47], achieved positive results. Additionally, the characteristics of the participants may potentially impact the outcomes. When considering the subjects' baseline skill level and BMI percentile, the results between the groups were not significant [32]. The findings suggest that while functional training can enhance children's locomotor skills, certain factors should also be considered, including the individual's current athletic proficiency, physical fitness, and anthropometric indicators [64]. More importantly, future research should address these factors by designing rigorous, well-controlled studies with larger sample sizes, ensuring highly reliable results.
Good balance is essential in various activities, from daily tasks to physical activities and sports. Children with proficient balance skills can better control their body movements, allowing them to coordinate their movements and perform various physical activities more efficiently and accurately [65]. Of the ten studies that assessed balance skills, static and dynamic balance skills were the two most common aspects of balance that improved. Such results suggest that functional training does improve children's balance skills. Research on unique populations, such as teenage athletes [29,34,35] and children with medical conditions [28,40,48], further evidences the effectiveness of functional training in promoting the development of balance skills. It also implies that functional training may be more effective and safer than other methods for improving balance skills [66]. This is because functional training prioritises enhancing multi-joint movement and dynamic stability while emphasising core muscle group training [67]. It is the core mechanism through which functional training promotes the development of balance skills. Similar observations have been reported in previous studies explicitly focusing on balance skills [68,69], suggesting that our current understanding builds upon a relatively complete and reliable body of knowledge. However, only a few studies have displayed disparate results. It could be attributed to the heterogeneity of the study participants. The health status of children can vary widely, potentially influencing the research results. In the studies [41,48,50], the main participants were children with intellectual disabilities, who have significant individual differences in cognitive ability, adaptive behaviour, and neurodevelopment [70] may have different baseline balance capabilities and improvement trajectories compared to healthy children [71]. Furthermore, age plays a crucial role in influencing the progression of balance skills, but children with intellectual disabilities may have restricted advancement by age [72]. The study reported no significant differences between the groups focusing on dual-task functional exercise. The mean age of the participants was 15.06 years [41], which is much older than the age of participants in similar studies. However, the number of studies on this age group is limited. More in-depth and detailed research is needed in the future.
Compared to locomotor skills, object control skills entail more intricate movement patterns that involve visual tracking, hand-eye coordination, and motor planning coordination [73]. Consequently, achieving proficiency in these skills can be challenging. As a result, the number of studies on object control skills in this review is limited. However, It is well known that more advanced forms of object control skills are skills in specific sports, manifested in the precise manipulation and control of objects such as balls or sports equipment [74]. In previous studies, most of the research exploring the effects of functional training has concentrated on specific skilled sports. A study conducted with soccer players found that a functional training program enhanced their dribbling, shooting, and passing performance [75]. Similarly, when functional training is combined with technical training designed explicitly for badminton, it has been shown to enhance the performance of hitting skills in badminton [76]. The positive outcomes observed in these studies are promising and support the idea that functional training can effectively facilitate the advancement of object control skills. Nevertheless, acquiring object control skills is a complex and continuous progression [77]. In addition to extensive practice and experience, a focused training method is crucial for promoting their development. To further explore the effect of functional training on improving object control skills, a more detailed and personalised training plan should be developed considering different children's specific physical conditions and athletic abilities. At the same time, longitudinal studies are also necessary to track the long-term effects of functional training on object control skills.
Although there are differences in the effects of functional training on locomotor, object control, and balance skills, it generally has a favourable impact on children's improvement in fundamental motor skills. Furthermore, research using controlled experimental designs demonstrated that there was also an improvement in children's FMS within the control group. However, the magnitude of this improvement was notably smaller than the significant effect observed in the group undergoing functional training. The results highlight the significance of the intervention approach in determining the effectiveness of FMS, with functional training proving to be more effective than other training methods. This is mainly because the core principles of functional training align closely with the movement patterns involved in fundamental motor skills [16]. Moreover, functional training focuses on the theory of dynamic chain and the synergistic effect of joints in the human body during movement [55]. A closed-chain action helps maintain the joints' stability [78] and potentially activates additional muscles and joints in different planes and axes, enhancing strength, endurance, flexibility, balance, coordination, and depth perception [79]. Undoubtedly, functional training has its unique advantages. To guarantee the efficacy of the intervention, it is crucial to carefully consider the intervention design while also considering the children's characteristics and health conditions.
The results of this review supported the association between functional training and FMS in children. However, there are some limitations. The first limitation is that limited existing studies focus on object control skills. Additionally, individual differences in the study participants, variances in the design, duration, and intensity of the functional training programs, and a lack of standardised methods for evaluating fundamental motor skills complicate the interpretation of the results and make it challenging to use quantitative analysis to summarise the effects. Finally, the absence of long-term follow-up data poses a challenge in assessing the enduring impact of functional training on fundamental motor skills. In summary, future studies on the current limitations are therefore recommended.
5. Practical Implications
-
•
The review contributes to the understanding of the development of fundamental motor skills in children and the potential benefits of functional training for promoting these skills, as well as providing helpful guidance in education, rehabilitation, sport, and community sectors.
-
•
This review could guide schools and educational institutions in designing more effective education and physical education programs to better promote the development of children's fundamental motor skills and participation in physical activity and maintain a healthy condition
6. Conclusion
The primary observation from this review is that functional training-based programs benefit children's fundamental motor skills, especially locomotor and balance skills. For object control skills, existing evidence concludes that further research is required to confirm its positive effects on object control skills. These results contribute significantly to the knowledge of the relationship between functional training and FMS and highlight the importance of providing children with opportunities to engage in functional training intervention. In addition, future research should focus on exploring individual characteristics and factors that influence the effects of functional training on fundamental movement skills.
CRediT authorship contribution statement
Dong Zhang: Writing – review & editing, Writing – original draft, Visualization, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Kim Geok Soh: Writing – review & editing, Validation, Supervision, Project administration, Conceptualization. Yoke Mun Chan: Writing – review & editing, Validation, Data curation. Xiaowei Feng: Software. Marrium Bashir: Software. Wensheng Xiao: Software.
Data availability
Data will be made available on request.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Dong Zhang, Email: brandondong001@gmail.com.
Kim Geok Soh, Email: kims@upm.edu.my.
Yoke Mun Chan, Email: cym@upm.edu.my.
Xiaowei Feng, Email: fengxiaowei@std11.cn.
Marrium Bashir, Email: gs61096@student.upm.edu.my.
Wensheng Xiao, Email: xiaowensheng33@gmail.com.
References
- 1.Rudd J.R., Barnett L.M., Butson M.L., Farrow D., Berry J., Polman R.C. Fundamental movement skills are more than run, throw and catch: the role of stability skills. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0140224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’ Brien W., Belton S., Issartel J. Fundamental movement skill proficiency amongst adolescent youth. Phys. Educ. Sport Pedagog. 2015;21(6):557–571. [Google Scholar]
- 3.Robinson L.E., Stodden D.F., Barnett L.M., Lopes V.P., Logan S.W., Rodrigues L.P., D'Hondt E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015;45:1273–1284. doi: 10.1007/s40279-015-0351-6. [DOI] [PubMed] [Google Scholar]
- 4.Taunton S.A., Brian A., True L. Universally designed motor skill intervention for children with and without disabilities. J. Dev. Phys. Disabil. 2017;29:941–954. [Google Scholar]
- 5.Morgan P.J., Barnett L.M., Cliff D.P., Okely A.D., Scott H.A., Cohen K.E., Lubans D.R. Fundamental movement skill interventions in youth: a systematic review and meta-analysis. Pediatrics. 2013;132(5):e1361–e1383. doi: 10.1542/peds.2013-1167. [DOI] [PubMed] [Google Scholar]
- 6.Bolger L.E., Bolger L.A., O'Neill C., Coughlan E., O'Brien W., Lacey S., Burns C. Age and sex differences in fundamental movement skills among a cohort of Irish school children. J. Mot. Learn. Dev. 2018;6(1):81–100. [Google Scholar]
- 7.Pienaar A., Visagie M., Leonard A. Proficiency at object control skills by nine-to ten-year-old children in South Africa: the NW-Child Study. Perceptual and motor skills. 2015;121(1):309–332. doi: 10.2466/10.PMS.121c15x8. [DOI] [PubMed] [Google Scholar]
- 8.Valentini N.C., Logan S.W., Spessato B.C., de Souza M.S., Pereira K.G., Rudisill M.E. Fundamental motor skills across childhood: age, sex, and competence outcomes of Brazilian children. J. Mot. Learn. Dev. 2016;4(1):16–36. [Google Scholar]
- 9.Bardid F. Ghent University; 2016. Early Childhood Motor Development: Measuring, Understanding and Promoting Motor Competence. [Google Scholar]
- 10.Costello K., Warne J. A four-week fundamental motor skill intervention improves motor skills in eight to 10-year-old Irish primary school children. Cogent Social Sciences. 2020;6(1) [Google Scholar]
- 11.Plisk S.S. Strength and Conditioning for Sports Performance. Routledge; 2016. Effective needs analysis and functional training principles; pp. 223–242. [Google Scholar]
- 12.Santana J.C. Human Kinetics; 2015. Functional Training. [Google Scholar]
- 13.Li Z., Zhao H., Chang Y. Analysis on the connotation purport, structure function and essential attributes of functional training to strength and conditioning. Journal of TUS. 2019;34:227–231. [Google Scholar]
- 14.Weiss T., Kreitinger J., Wilde H., Wiora C., Steege M., Dalleck L., Janot J. Effect of functional resistance training on muscular fitness outcomes in young adults. Journal of Exercise Science & Fitness. 2010;8(2):113–122. [Google Scholar]
- 15.Cassemiro B.M., Lemes Í.R., Figueiredo MPFd, Vanderlei F.M., Pastre C.M., Netto J. Effects of functional resistance training on muscle strength and musculoskeletal discomfort. Fisioterapia Em Movimento. 2017;30:347–356. [Google Scholar]
- 16.Boyle M. Human Kinetics Publishers; 2004. Functional Training for Sports. [Google Scholar]
- 17.Gorter H., Holty L., Rameckers E.E., Elvers H.J., Oostendorp R.A. Changes in endurance and walking ability through functional physical training in children with cerebral palsy. Pediatr. Phys. Ther. 2009;21(1):31–37. doi: 10.1097/PEP.0b013e318196f563. [DOI] [PubMed] [Google Scholar]
- 18.Surana B.K., Ferre C.L., Dew A.P., Brandao M., Gordon A.M., Moreau N.G. Effectiveness of Lower-Extremity Functional Training (LIFT) in young children with unilateral spastic cerebral palsy: a randomised controlled trial. Neurorehabilitation Neural Repair. 2019;33(10):862–872. doi: 10.1177/1545968319868719. [DOI] [PubMed] [Google Scholar]
- 19.Wang C., Feng G. Effect of functional training on body morphology and body composition in children aged 5-6. SPORT SCIENCE AND TECHNOLOGY. 2021;43:60–62. [Google Scholar]
- 20.Wei L, Wei Y: Experimental research on functional training for the development of children from 9 to 10 years old. Physical Health, 41:96-98.
- 21.Liu C-j, Shiroy D.M., Jones L.Y., Clark D.O. Systematic review of functional training on muscle strength, physical functioning, and activities of daily living in older adults. European review of aging and physical activity. 2014;11:95–106. [Google Scholar]
- 22.Xingxing G. Experimental study on the effect of functional training on children's balance ability. Master’s thesis. 2018 Beijing Sport University. [Google Scholar]
- 23.Uman L.S. Systematic reviews and meta-analyses. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2011;20(1):57. [PMC free article] [PubMed] [Google Scholar]
- 24.Amir-Behghadami M., Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria. systematic reviews. Emergency Medicine Journal. 2020 doi: 10.1136/emermed-2020-209567. [DOI] [PubMed] [Google Scholar]
- 25.De Morton N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust. J. Physiother. 2009;55(2):129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 26.Albanese E., Bütikofer L., Armijo‐Olivo S., Ha C., Egger M. Construct validity of the Physiotherapy Evidence Database (PEDro) quality scale for randomised trials: item response theory and factor analyses. Res. Synth. Methods. 2020;11(2):227–236. doi: 10.1002/jrsm.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kong L.J., Fang M., Zhan H.S., Yuan W.A., Pu J.H., Cheng Y.W., Chen B. Tuina-focused integrative Chinese medical therapies for inpatients with low back pain: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine 2012. 2012 doi: 10.1155/2012/578305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abd-Elfattah H.M., Ameen F.H., Elkalla R.A., Aly S.M., Abd-Elrahman N.A.F. Loaded functional strength training versus traditional physical therapy on hip and knee extensors strength and function walking capacity in children with hemiplegic cerebral palsy: randomised comparative study. Children. 2022;9(7):946. doi: 10.3390/children9070946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norambuena Y., Winkler L., Guevara R., Llavados P., Uarac M.M., Campillo R.R., Valenzuela T.H., Burgos R.G. 5-week suspension training program increase physical performance of youth judokas: a pilot study. Retos: nuevas tendencias en educación física, deporte y recreación. 2021;(39):137–142. [Google Scholar]
- 30.Baron J., Bieniec A., Swinarew A.S., Gabryś T., Stanula A. Effect of 12-week functional training intervention on the speed of young footballers. Int. J. Environ. Res. Publ. Health. 2020;17(1):160. doi: 10.3390/ijerph17010160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Katsanis G., Chatzopoulos D., Barkoukis V., Lola A.C., Chatzelli C., Paraschos I. Effect of a school-based resistance training program using a suspension training system on strength parameters in adolescents. Journal of Physical Education and Sport. 2021;21(5):2607–2621. [Google Scholar]
- 32.Laurent C.W.S., Masteller B., Sirard J. Effect of a suspension-trainer-based movement program on measures of fitness and functional movement in children: a pilot study. Pediatr. Exerc. Sci. 2018;30(3):364–375. doi: 10.1123/pes.2016-0278. [DOI] [PubMed] [Google Scholar]
- 33.Labib L. Effect of functional strength training on certain physical and physiological variables among young female handball players. Ovidius Univ. Ann. - Ser. Phys. Educ. Sport/Sci. Mov. Health. 2014;14(1) [Google Scholar]
- 34.Yildiz S., Pinar S., Gelen E. Effects of 8-week functional vs. traditional training on athletic performance and functional movement on prepubertal tennis players. J. Strength Condit Res. 2019;33(3):651–661. doi: 10.1519/JSC.0000000000002956. [DOI] [PubMed] [Google Scholar]
- 35.Song H.-S., Woo S.-S., So W.-Y., Kim K.-J., Lee J., Kim J.-Y. Effects of 16-week functional movement screen training program on strength and flexibility of elite high school baseball players. Journal of exercise rehabilitation. 2014;10(2):124. doi: 10.12965/jer.140101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao T., Li L., Wang Y.T. Effects of functional strength training program on movement quality and fitness performance among girls aged 12–13 years. J. Strength Condit Res. 2019;33(6):1534–1541. doi: 10.1519/JSC.0000000000002190. [DOI] [PubMed] [Google Scholar]
- 37.Marta C., Alves A.R., Esteves P.T., Casanova N., Marinho D., Neiva H.P., Aguado-Jimenez R., Alonso-Martínez A.M., Izquierdo M., Marques M.C. Effects of suspension versus traditional resistance training on explosive strength in elementary school-aged boys. Pediatr. Exerc. Sci. 2019;31(4):473–479. doi: 10.1123/pes.2018-0287. [DOI] [PubMed] [Google Scholar]
- 38.Eather N., Morgan P., Lubans D. Improving health-related fitness in adolescents: the CrossFit Teens randomised controlled trial. J. Sci. Med. Sport. 2015;19 doi: 10.1080/02640414.2015.1045925. [DOI] [PubMed] [Google Scholar]
- 39.Carvutto R., Damasco C., De Candia M. 2021. Non-traditional Training in Youth Soccer Players: Effects on Agility and on Sprint Performance. [Google Scholar]
- 40.Bonney E., Ferguson G., Burgess T., Smits-Engelsman B. Benefits of activity-based interventions among female adolescents who are overweight and obese. Pediatr. Phys. Ther. 2019;31(4):338–345. doi: 10.1097/PEP.0000000000000636. [DOI] [PubMed] [Google Scholar]
- 41.Mikolajczyk E., Jankowicz-Szymanska A. Does extending the dual-task functional exercises workout improve postural balance in individuals with ID? Res. Dev. Disabil. 2015;38:84–91. doi: 10.1016/j.ridd.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 42.Emara H.A., El-Gohary T.M., Al-Johany A.A. Effect of body-weight suspension training versus treadmill training on gross motor abilities of children with spastic diplegic cerebral palsy. Eur. J. Phys. Rehabil. Med. 2016;52(3):356–363. [PubMed] [Google Scholar]
- 43.Ansa O.E.O., Mprah K.W., Moses M.O., Owusu I., Acheampong E. Effect of community-based functional aerobic training on motor performance and quality of life of children with spastic cerebral palsy. Ethiopian journal of health sciences. 2021;31(2) doi: 10.4314/ejhs.v31i2.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ketelaar M., Vermeer A., Hart Ht, van Petegem-van Beek E., Helders P.J. Effects of a functional therapy program on motor abilities of children with cerebral palsy. Phys. Ther. 2001;81(9):1534–1545. doi: 10.1093/ptj/81.9.1534. [DOI] [PubMed] [Google Scholar]
- 45.Salavati M., Rameckers E., Waninge A., Krijnen W., van der Schans C., Steenbergen B. Evaluating the outcome of an individual functional therapy program focused on children with cerebral palsy and cerebral visual impairment: a multiple case study. European Journal of Physiotherapy. 2018;20(2):92–100. [Google Scholar]
- 46.Blundell S., Shepherd R., Dean C., Adams R., Cahill B. Functional strength training in cerebral palsy: a pilot study of a group circuit training class for children aged 4–8 years. Clin. Rehabil. 2003;17(1):48–57. doi: 10.1191/0269215503cr584oa. [DOI] [PubMed] [Google Scholar]
- 47.Ahl L.E., Johansson E., Granat T., Carlberg E.B. Functional therapy for children with cerebral palsy: an ecological approach. Dev. Med. Child Neurol. 2005;47(9):613–619. [PubMed] [Google Scholar]
- 48.Farrokhian S., Hemati Alamdarloo G., Asadmanesh E. The effectiveness of functional training on static balance, dynamic balance and flexibility of females with intellectual disability. Baltic J. Health Phys. Act. 2021;13(3):8. doi: 10.4081/hpr.2020.9116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Tittelboom V., Heyrman L., De Cat J., Algoet P., Peeters N., Alemdaroğlu-Gürbüz I., Plasschaert F., Van Herpe K., Molenaers G., De Bruyn N. Intensive therapy of the lower limbs and the trunk in children with bilateral spastic cerebral palsy: comparing a qualitative functional and a functional approach. J. Clin. Med. 2023;12(12):4078. doi: 10.3390/jcm12124078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mikołajczyk E., Jankowicz-Szymańska A. The effect of unstable-surface functional exercises on static balance in adolescents with intellectual disability–a preliminary report. Medical Studies/Studia Medyczne. 2014;30(1):1–5. [Google Scholar]
- 51.Baron J., Bieniec A., Swinarew A., Skalski D., Stanula A. The effects of twelve-week functional training on the power of the lower limbs of young footballers. Acta Kinesiol. 2020;14(1):70–76. [Google Scholar]
- 52.Salavati M., Krijnen W., Rameckers E., Looijestijn P., Maathuis C., van der Schans C., Steenbergen B. Reliability of the modified gross motor function measure-88 (GMFM-88) for children with both spastic cerebral palsy and cerebral visual impairment: a preliminary study. Res. Dev. Disabil. 2015;45:32–48. doi: 10.1016/j.ridd.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Almeida K.M., Albuquerque K.A., Ferreira M.L., Aguiar S.K., Mancini M.C. Reliability of the Brazilian Portuguese version of the gross motor function measure in children with cerebral palsy. Braz. J. Phys. Ther. 2016;20(1):73–80. doi: 10.1590/bjpt-rbf.2014.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rivera-Rujana D.M., Muñoz-Rodríguez D.I., Agudelo-Cifuentes M.C. Reliability of the gross motor function measure-66 scale in the evaluation of children with cerebral palsy: validation for Colombia. Boletín médico del Hospital Infantil de México. 2022;79(1):33–43. doi: 10.24875/BMHIM.21000094. [DOI] [PubMed] [Google Scholar]
- 55.Hao T., Yuxi L. Analysis on the reasons why functional training is superior to physical training. Frontiers in Sport Research. 2020;2(3):10–12. [Google Scholar]
- 56.Washabaugh E.P., Augenstein T.E., Krishnan C. Functional resistance training during walking: mode of application differentially affects gait biomechanics and muscle activation patterns. Gait Posture. 2020;75:129–136. doi: 10.1016/j.gaitpost.2019.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bashir M., Soh K.G., Samsudin S., Akbar S., Luo S., Sunardi J. Effects of functional training on sprinting, jumping, and functional movement in athletes: a systematic review. Front. Physiol. 2022;13:2449. doi: 10.3389/fphys.2022.1045870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bhardwaj A., Kathayat L.B. Effect of 6-week functional training on speed and agility of basketball players. Indian Journal of Physiotherapy & Occupational Therapy Print- 2021;15(4):11–16. (ISSN 0973-5666) and Electronic–(ISSN 0973-5674) [Google Scholar]
- 59.Fathir L.W., Hartanto S., Kusnanik N.W. Strength, endurance and speed development using functional strength training (FST) program for recreational runners performance. Journal of Physical Education and Sport. 2021;21:2453–2457. [Google Scholar]
- 60.Gaedtke A., Morat T. TRX suspension training: a new functional training approach for older adults–development, training control and feasibility. International journal of exercise science. 2015;8(3):224. doi: 10.70252/SWSX2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pang A.W.-Y., Fong D.T.-P. Fundamental motor skill proficiency of Hong Kong children aged 6–9 years. Res. Sports Med. 2009;17(3):125–144. doi: 10.1080/15438620902897516. [DOI] [PubMed] [Google Scholar]
- 62.Aye T., Kuramoto-Ahuja T., Sato T., Sadakiyo K., Watanabe M., Maruyama H. Gross motor skill development of kindergarten children in Japan. J. Phys. Ther. Sci. 2018;30(5):711–715. doi: 10.1589/jpts.30.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kotzamanidis C., Chatzopoulos D., Michailidis C., Papaiakovou G., Patikas D. The effect of a combined high-intensity strength and speed training program on the running and jumping ability of soccer players. J. Strength Condit Res. 2005;19(2):369–375. doi: 10.1519/R-14944.1. [DOI] [PubMed] [Google Scholar]
- 64.Sutapa P., Pratama K.W., Rosly M.M., Ali S.K.S., Karakauki M. Improving motor skills in early childhood through goal-oriented play activity. Children. 2021;8(11):994. doi: 10.3390/children8110994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rudd J. Victoria University; 2016. The Efficacy of Gymnastics to Improve Movement Skill Competence in Children. [Google Scholar]
- 66.Sadeghi H., Norouzi H., Karimi Asl A., Montazer M. Functional training program effect on static and dynamic balance in male able-bodied elderly. Iranian Journal of Ageing. 2008;3(2):565–571. [Google Scholar]
- 67.Qin Y-k, Zeng J., Peng L. Short term functional training improves completion quality of body difficulty of juvenile rhythmic gymnasts. Revista Brasileira de Ciências do Esporte. 2021;43 [Google Scholar]
- 68.Uzun S. The effect of long-term training program on balance in children with cerebral palsy: results of a pilot study for individually based functional exercises. Educ. Res. Rev. 2013;811 [Google Scholar]
- 69.Park J.-W., Kim W.-B. The effect of functional training using a sliding rehabilitation machine on the mobility of the ankle joint and balance in children with CP. Journal of Korean Society of Physical Medicine. 2014;9(3):293–299. [Google Scholar]
- 70.Sajewicz-Radtke U., Jurek P., Olech M., Łada-Maśko A.B., Jankowska A.M., Radtke B.M. Heterogeneity of cognitive profiles in children and adolescents with mild intellectual disability (MID) Int. J. Environ. Res. Publ. Health. 2022;19(12):7230. doi: 10.3390/ijerph19127230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ma Y., Wang L., Li M., Wang T. Meta-analysis of the effects of exercise programs in improving the balance ability of children with intellectual disabilities. J. Intellect. Dev. Disabil. 2020;45(2):144–154. [Google Scholar]
- 72.Pitetti K., Miller R.A., Loovis E.M. Balance and coordination proficiency of age-matched male and female children and adolescents with intellectual disabilities. Adapt. Phys. Act. Q. (APAQ) 2018;35(2):175–195. doi: 10.1123/apaq.2017-0077. [DOI] [PubMed] [Google Scholar]
- 73.Haningsih WO, Ihsan N, Gusril RB, Zarya F: Object Control Abilities of Kindergarten Students: Impact of Eye-Hand Coordination, Nutritional Status, Gender.
- 74.Zuvela F., Bozanic A., Miletic D. POLYGON-A new fundamental movement skills test for 8 year old children: construction and validation. J. Sports Sci. Med. 2011;10(1):157. [PMC free article] [PubMed] [Google Scholar]
- 75.Sebastian M. Effects of plyometric with functional training on selected physical fitness physiological and skill performance variables of intercollegiate male football players. International Journal of Physical Education, Sports and Health. 2018;5(6):22–25. [Google Scholar]
- 76.Kong M-m, Liu Q. 2013 International Conference on Educational Research and Sports Education (ERSE 2013) 2013. The interpretation of functional training and its application in badminton; pp. 160–163. 2013: Atlantis Press. [Google Scholar]
- 77.Donath L., Faude O., Hagmann S., Roth R., Zahner L. Fundamental movement skills in preschoolers: a randomised controlled trial targeting object control proficiency. Child: care, health and development. 2015;41(6):1179–1187. doi: 10.1111/cch.12232. [DOI] [PubMed] [Google Scholar]
- 78.Mikkelsen C., Werner S., Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg. Sports Traumatol. Arthrosc. 2000;8(6) doi: 10.1007/s001670000143. [DOI] [PubMed] [Google Scholar]
- 79.Zırhlı O., Demirci N. The Influence of functional training on biomotor skills in girl tennis players aged 10–12. Baltic J. Health Phys. Act. 2020;12(4):33–45. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.