ABSTRACT
Measles and rubella have long been recognized as priorities for disease prevention because of their devastating consequences for child health; hence, all World Health Organization (WHO) regions currently have a goal to eliminate measles and four out of six WHO regions have a goal to eliminate rubella. Significant global progress has been made in the twenty-first century, with more than 40% of countries in the world verified by a Regional Verification Commission as having eliminated measles and more than 50% of countries having sustained rubella elimination. Making further progress will require addressing fundamental gaps in health systems, a particular challenge in the current global context where many countries face multiple barriers to both sustaining and achieving measles and rubella elimination. These challenges require a strategic shift toward a holistic approach that embeds immunization at the center of primary health care at all levels, which will have broad benefits beyond preventing measles and rubella. Progress will be supported through technological innovations such as microarray patch vaccines. Whether this holistic approach will be more effective than vertical initiatives at achieving measles and rubella elimination remains to be seen. Measles is so infectious and its immediate impact so visible on individuals and health systems that any weaknesses in global or national strategy are immediately evident. The tools exist to prevent every death from measles and every case of congenital rubella syndrome. Countries and partners – at all levels – share accountability for ensuring children are protected from these entirely preventable diseases.
Keywords: Measles, rubella, disease eradication, vaccines, immunization programs
RESUMEN
Hace tiempo que se reconoce que el sarampión y la rubéola constituyen una prioridad en materia de prevención de enfermedades debido a sus devastadoras consecuencias para la salud infantil; por ello, las seis regiones de la Organización Mundial de la Salud (OMS) se han fijado como objetivo la eliminación del sarampión, y cuatro de ellas el de la eliminación de la rubéola. En lo que va del siglo XXI se han logrado avances significativos a nivel mundial: una Comisión Regional de Verificación ha comprobado la eliminación del sarampión en más del 40% de los países del mundo y una eliminación mantenida de la rubéola en más del 50% de los países. Lograr nuevos avances implicará subsanar deficiencias fundamentales en los sistemas de salud, lo que supone un verdadero desafío en el contexto mundial actual, en el que muchos países deben hacer frente a múltiples obstáculos tanto para mantener como para lograr la eliminación del sarampión y la rubéola. Estos desafíos requieren una transformación estratégica hacia un enfoque holístico que integre la inmunización como elemento central de la atención primaria de salud en todos los niveles, lo que comportará amplios beneficios que irán más allá de la prevención del sarampión y la rubéola. Los avances se verán sustentados por innovaciones tecnológicas como las vacunas en parches de micromatrices. Queda por ver si este enfoque holístico será más eficaz que las iniciativas verticales para lograr la eliminación del sarampión y la rubéola. El sarampión es tan infeccioso, y su impacto inmediato en las personas y los sistemas de salud es tan visible, que cualquier punto débil en las estrategias nacionales o mundiales se pone inmediatamente de manifiesto. Ya hay las herramientas necesarias para evitar todas las muertes por sarampión y todos los casos de síndrome de rubéola congénita Tanto los países como los asociados —en todos los niveles— comparten la responsabilidad de garantizar la protección de la población infantil contra estas enfermedades totalmente prevenibles.
Palabras clave: Sarampión, rubéola, erradicación de la enfermedad, vacunas, programas de inmunización
RESUMO
Há muito tempo, o sarampo e a rubéola são prioridades na prevenção de doenças devido às suas consequências devastadoras para a saúde infantil. Por isso, atualmente, todas as regiões da Organização Mundial da Saúde (OMS) têm a meta de eliminar o sarampo, e quatro das seis regiões da OMS têm a meta de eliminar a rubéola. Houve progresso mundial significativo no século XXI, período no qual a eliminação do sarampo em mais de 40% dos países do mundo foi verificada por uma Comissão Regional de Verificação; além disso, mais de 50% dos países mantiveram a eliminação da rubéola. Para que haja mais progresso, será necessário abordar lacunas fundamentais nos sistemas de saúde, um desafio especial no atual contexto mundial, em que muitos países enfrentam muitas barreiras para manter ou alcançar a eliminação do sarampo e da rubéola. Esses desafios exigem uma mudança estratégica em direção a uma abordagem holística que incorpore a imunização como elemento central da atenção primária à saúde em todos os níveis, o que trará amplos benefícios que vão além da prevenção do sarampo e da rubéola. O progresso será apoiado por inovações tecnológicas, como a vacinação com adesivos de microagulhas. Ainda não se sabe se essa abordagem holística será mais efetiva do que as iniciativas verticais para alcançar a eliminação do sarampo e da rubéola. O sarampo é tão infeccioso e seu impacto imediato é tão visível nos indivíduos e nos sistemas de saúde que qualquer ponto fraco na estratégia mundial ou nacional fica imediatamente evidente. Existem ferramentas para prevenir cada morte por sarampo e cada caso de síndrome da rubéola congênita. Países e parceiros — em todos os níveis — compartilham a responsabilidade de garantir que as crianças estejam protegidas contra essas doenças totalmente preveníveis.
Palavras-chave: Sarampo, rubéola, erradicação de doenças, vacinas, programas de imunização
HISTORY AND CONTEXT
At the start of this century, many had high hopes that a global effort toward measles elimination would follow hard on the heels of polio eradication. Two decades later, the global landscape is less encouraging. After many years and a substantive investment by multiple stakeholders, polio eradication seems to remain just out of reach. Indeed, only one vaccine-preventable disease, smallpox, has been eradicated after decades of focused effort (where eradication refers to elimination in all regions).
Between 2000 and 2010, countries made steady program improvements and global coverage of routine measles immunization increased from 72% to 84%, with many programs adding a second measles vaccine dose and rubella vaccine. Progress stalled during 2011–2019 when global coverage crept up by only 2%, reaching 86% in 2019. Over time, unvaccinated children accumulated, culminating in 2019 with measles epidemics in every World Health Organization (WHO) region and every category of country from low to high income. In that year, countries reported the highest number of cases globally since 1996; accounting for under-reporting, the total was estimated at 4.5 million cases and 148 000 deaths (1). In that same year, while countries in all WHO regions were being rocked by measles outbreaks, the WHO Strategic Advisory Group of Experts on Immunization (SAGE) produced a report on the feasibility of measles eradication in response to a request from the World Health Assembly and concluded that, while technically feasible, the world was not ready for a measles eradication goal (2).
In 2019, global leadership to drive measles and rubella elimination rested with the Measles & Rubella Initiative (M&RI), a partnership of the American Red Cross, U.S. Centers for Disease Control and Prevention, UN Foundation, UNICEF, and WHO. The aspiration was for the M&RI to become to measles and rubella elimination what Global Polio Eradication Initiative (GPEI) was to polio eradication. This strategy foundered for several reasons, not just because polio eradication goals were continually delayed but also because the donor community lacked an appetite for another vertical disease program, preferring instead to direct financial support on strengthening essential immunization and primary health care systems. Furthermore, neither measles nor rubella have ever entered the political dialogue space beyond ministries of health in the way that, for example, polio and COVID-19 have done. Finally, Gavi, the Vaccine Alliance, was founded in 2000 with the goal of supporting low-income countries to accelerate new vaccine introduction and health systems strengthening. With a geographically defined mandate, Gavi cannot support the goal of measles elimination in all countries.
The evolving global landscape effectively ended the aspiration of M&RI to be the new GPEI driving measles and rubella elimination. It was reestablished as the Measles and Rubella Partnership (M&RP) with the addition of Bill and Melinda Gates Foundation (BMGF) and Gavi as partners and transitioned into a working group within the implementation apparatus of the current global strategy, Immunization Agenda 2030 (IA2030) (3).
CURRENT CHALLENGES
Eliminating measles remains a priority in every WHO region, as specified through Regional Committee resolutions and articulated in the Measles Rubella Strategic Framework (MRSF) (4). Eliminating rubella is a goal in four out of six WHO regions. Most countries (90%, 175/194) use combined measles and rubella vaccines and the fates of these two viruses are now closely entwined.
Measles elimination patterns vary widely, ranging from the Americas where all countries were verified as eliminated for rubella in 2015 and for measles in 2016 through to the African region where progress has been made but no countries have yet been verified. Every WHO region has a Regional Verification Commission, and most countries have National Verification Committees to oversee progress toward elimination. By the end of 2023, 80/194 countries (41%) had been verified as having eliminated measles and 97/194 (50%) had eliminated rubella (1).
A common challenge faced by all regions is that the path to measles elimination is bumpy. Every WHO region that has made significant progress toward measles elimination has also experienced setbacks. In contrast, so far, no country that has achieved rubella elimination has lost that status. After achieving regional verification of measles in 2016, the Americas experienced a resurgence that started in the Bolivarian Republic of Venezuela and spread to neighboring countries including Brazil, and the Americas then lost its elimination status (5). The recovery toward re-verifying the Region of the Americas is now well underway, post-COVID-19 pandemic. Great progress has also been made in the European, Western Pacific, and South-East Asia regions, but all have countries where measles transmission has been reestablished after previously being verified as eliminated.
Nevertheless, overall progress has been moving forward up to this point. Between 2000 and 2022, 57 million lives were saved by measles vaccination, and between 2010 and 2019 congenital rubella syndrome (CRS) numbers fell by 66% to an estimated 32 000 cases (6). By 2023, global measles first dose immunization coverage remained at 83% after declining from its peak of 86% in 2019 (7). The question addressed in the rest of this article is how, in this new global landscape and context, to accelerate progress toward measles and rubella elimination.
CHALLENGES FACED IN ACHIEVING AND SUSTAINING ELIMINATION
How measles and rubella biology creates challenges in achieving and sustaining elimination
Measles and rubella vaccines save lives and are both critical investments for public health. Measles vaccine has been in the Essential Program on Immunization (EPI) for 50 years and is one of the most cost-effective vaccines, contributing 75% of the overall immunization program impact on vaccine-preventable diseases for only 25% of the program costs (8, 9). Rubella causes CRS, one of the most common preventable congenital birth defects. Although measles and rubella are both fever rash illnesses, the viruses behave differently, with vastly different epidemiology and outcomes.
Measles is one of the most highly infectious viruses of humans (Table 1). To interrupt transmission, immunization coverage with two doses of vaccine must be over 95%, year after year. This is exceedingly difficult for immunization programs to achieve and sustain for every birth cohort. Although highly effective, measles vaccine is not as effective as rubella vaccine, requiring equitable and sustained high coverage with two doses to achieve measles elimination. The critical community size that can sustain transmission is also smaller for measles than rubella; clusters of unprotected children caused by inequities in coverage are more likely to lead to outbreaks of measles than rubella (Table 1).
TABLE 1. Comparing and contrasting measles and rubella characteristics relevant to elimination.
|
Characteristic |
Measles |
Rubella |
|---|---|---|
|
Infectivity |
One of the most infectious viruses of humans |
Variable according to population size, but moderate |
|
Basic reproduction number (R0) |
12–18 (10) |
Median 5.2 (11) |
|
Population immunity levels required to interrupt transmission |
93% |
Around 80% |
|
Vaccine effectiveness (VE) of single dose |
Depends strongly on age at first dose: 9 months 85% 12 months 93% |
95% |
|
VE of 2 doses |
If MCV1 at 12 months, 97% |
>95% |
|
Coverage required to interrupt transmission |
>95% two dose |
Around 80% single dose |
|
Waning immunity over time |
None following infection, slow following two doses given at 12 months and older, potentially more rapid when MCV1 given earlier than 12 months |
None observed |
|
Requirements to elimination |
Cannot eliminate with a single dose |
Can eliminate with a single dose |
|
Highest risk age group |
Infants at highest risk of severe outcomes, followed by adults. Pregnant women are at higher risk of severe outcomes. |
Developing fetus in first trimester |
|
Critical community size to sustain transmission |
250–400 000 (12) |
1 million (13) |
|
Strategy |
Immunization programs aim to protect infants, boys and girls, through herd immunity. Direct protection of infants via early doses from 6 months is offered in high-risk settings. |
Women of childbearing age are protected through herd immunity in countries where adult immunization campaigns have not been implemented. Some countries have adult catch-up strategies but women-only not recommended. |
MCV1: measles-containing vaccine, first dose.
Source: Prepared by the authors.
By contrast, rubella is not nearly as infectious as measles and the vaccine is more effective, requiring only one dose. As a result, rubella can be eliminated with more moderate coverage of around 80%. The challenge of rubella is its stealth. In smaller populations rubella outbreaks are more unpredictable than measles and may also be missed because the proportion of subclinical cases (and transmission from them) is higher for rubella than for measles. When coverage falls, measles reemerges quickly, but rubella immunity gaps may remain hidden for years and persist into adulthood. When that occurs, rubella outbreaks may affect women during pregnancy leading to fetal loss and CRS. This may happen even if recent coverage in childhood is high as a legacy of gaps in immunization systems from decades earlier.
Societal challenges, inequity, rubella, and measles as a tracer
Measles cases and outbreaks reveal children and communities who have not been reached by measles and other vaccines and can guide programmatic planning in identifying and addressing immunization system weaknesses. Within IA2030 this concept is referred to as “measles as a tracer.” Definitions of “tracer” refer to something that makes other things visible, lighting them up literally (as in a military flare) or illuminating them figuratively (as in the substance used in a medical investigation). Measles makes inequity visible, where health inequities are differences in health outcomes that are avoidable, unfair, and systematically related to social inequality and disadvantage (14, 15). “Measles as a tracer” can help identify the complex multilayered factors that influence whether a child is vaccinated (Figure 1). Measles vaccine second dose coverage is also an indicator for attaining United Nations Sustainable Development Goals (SDG) (16). Countries that have not yet introduced rubella vaccine are among the poorest in the world (17).
FIGURE 1. Multiple levels determine or influence whether a child will remain unvaccinated.
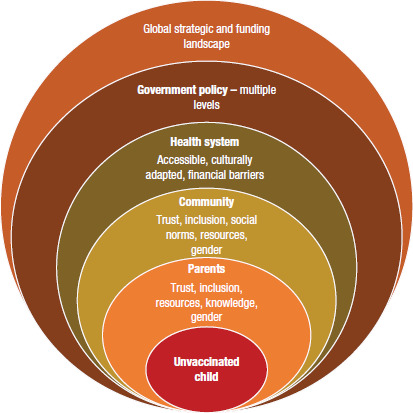
Source: Prepared by the authors.
Countries face relative inequities in their capacity to achieve elimination goals, with progress in the WHO African and Eastern Mediterranean regions lagging. In Africa, the proportion of children successfully protected from measles is too low in many countries to control measles (control defined as incidence below 5 cases per million) (18) and several countries have not yet introduced rubella vaccine. The cause is weak health systems and weak economies that have a historical legacy justifying greater support from high-income countries (19–22).
Inequity has widened for many countries due to the COVID-19 pandemic, economic crises, conflict, and mass migrations, all exacerbated by climate change. Backsliding has been particularly notable in low-income and fragile or conflict settings that have not recovered following the disruption of the pandemic or taken significant steps backward. Less than 15% of the under 5-year-old population lives in low-income countries that reported 43% of all measles cases in 2022 (7). An ongoing global initiative called “The Big Catch-Up” (BCU) aims to address this backsliding (23).
From a purely technical perspective, inequitable measles vaccination coverage makes measles elimination harder to achieve by effectively increasing the coverage needed to interrupt transmission (24). Addressing inequity is therefore not just the right thing to do but also an essential component of an effective elimination strategy.
Measles and rubella vaccines also continue to be a particular target of anti-vaccine rhetoric since the falsified link between autism and measles-containing vaccine debacle of the late 1990s (25). In addition, vaccination programs have been undermined by politicization; for example, where vaccine mandates become linked to concepts such as freedom and choice. A further corrosive impact on trust occurred during the COVID-19 pandemic.
Programmatic challenges
Achieving measles elimination solely through routine immunization is hard and can take decades; sustaining it is even harder. Eliminating measles requires immunization systems that can consistently deliver at least 95% vaccination coverage with at least two doses – i.e., reach almost every eligible child year after year. This is monumentally hard to do in any country, but particularly challenging in large decentralized countries with porous borders, security challenges, and ever-increasing birth cohorts. Countries with low coverage often rely on measles vaccination campaigns as a rescue intervention to rapidly fill gaps in levels of protection and prevent measles outbreaks. Campaigns need to be conducted in a frequency inversely related to coverage, so that a country with coverage of 60% would need a campaign every two years and with 80%, every four years to prevent outbreaks (26). Delaying campaigns in the hope of achieving higher campaign coverage increases the risk of outbreaks. All countries should provide two doses of measles and rubella vaccine, but by the end of 2023, five countries had yet to introduce a second dose of measles vaccine, and 19 countries, rubella vaccine. To be eligible to introduce rubella vaccine, current WHO policy recommendations are for countries to have measles first dose coverage of at least 80% either by routine immunization or through campaigns. A country needs to demonstrate that it will be able to sustain rubella coverage that is high enough to prevent future outbreaks of rubella. Inadequate coverage might leave immunity gaps that eventually reach women of childbearing age and potentially increase CRS (27). This policy recommendation is under review because it causes a major access barrier and inequity in the countries yet to introduce rubella vaccine.
Outbreaks not only increase morbidity and mortality but also strain healthcare systems and incur great economic costs. Countries that have improved their immunization coverage recently may face challenges with immunity gaps in older age groups causing outbreaks across wide age ranges that are difficult to bring under control. Middle-income countries often face challenges funding outbreak response and preventive campaigns, illustrating how national income, the eligibility criterion for Gavi support, does not fully align with countries’ financial ability to support vaccination activities or address in-country inequities. A global financial mechanism exists via the UN Foundation to support outbreak response costs in non-Gavi eligible countries but is not sufficient to meet current needs. Nothing exists like the International Coordinating Group (ICG) on Vaccine Provision rolling reimbursable financing mechanism available for middle-income countries for other vaccines. Additionally, there are often significant delays from when a country initially seeks international aid for an outbreak response until the time when financial support is received and disbursed to subnational levels and subsequent response activities are implemented.
Immunity gaps worsened in number and scale during the COVID-19 pandemic. If these are not filled rapidly, outbreaks will increase. More than half of all countries in the world (54%, 105/194) will be at high risk of measles outbreaks by the end of 2024 unless urgent action is taken, such as via the BCU and through strengthening capacity of countries to respond rapidly by pre-positioning vaccine stock either for outbreaks or boosted routine supply in high-risk countries and enabling no regrets use of routine stock for outbreak response. In total, 142 million children under 5 years are estimated to be susceptible to measles, 62% living in settings at highest or high risk of an outbreak by the end of 2024 (28). The Measles Outbreaks Strategic Response Plan 2021–2023 (MOSRP) was developed to strengthen the capacity of countries at high risk of measles outbreaks to prevent and respond effectively, following the devastating experience of 2018–2019 (29). The plan remains just as relevant now, as we see Large or Disruptive Outbreaks of measles (with an incidence of more than 20 per million) relentlessly increasing into 2024. In the long term, outbreak prevention should be through strong routine immunization, but in countries where health systems are weak, campaigns become the primary measure available to prevent outbreaks.
Data challenges
Vaccination programs rely on high quality data to guide decision-making, including routine immunization administrative coverage monitoring, post-campaign coverage surveys, and laboratory-supported disease surveillance. The high coverage required for measles elimination presents a specific challenge for measurement of coverage because very accurate numerators and denominators are required to determine that ≤5% of the target population has been missed. If countries are relying on out-of-date census data for denominators, coverage estimates may be wildly overestimated or underestimated. Perhaps more important is that inaccurate data make it very hard to identify and reach children who have been missed. Assessing the quality of campaigns via high quality surveys is also essential for planning.
Disease surveillance is an essential and integral part of a well-functioning immunization program and highly cost-effective. A comprehensive approach to eliminate measles includes high quality surveillance to demonstrate that measles transmission has been interrupted, track chains of transmission where they occur, and ensure preparedness for rapid outbreak response. Yet providing sustainable laboratory-supported surveillance systems is a major challenge. The existence of the Global Measles and Rubella Laboratory Network currently relies at global level on funding from one government (30). The fragility of surveillance in many countries was demonstrated when it was disrupted by COVID-19 as laboratories switched their priorities away from measles and rubella toward emergency response. Many countries found their public health infrastructure insufficient during the pandemic, yet are now standing down the additional resources, leaving systems and communities less resilient to future challenges.
DISCUSSION OF GLOBAL SOLUTIONS
Global leadership
If global goals are to be met, global and local action are needed to address fundamental causes of inequity between and within countries using measles as a tracer. The MRSF and MOSRP summarize strategies needed to align action and resources and need to be prioritized and resourced in a way that empowers countries. Immediate action to stop the rising trend in large or disruptive outbreaks requires decisive and fast outbreak prevention, response, plus recovery mechanisms via activities such as the BCU and technical assistance from WHO and partners for implementing all the elements of the MOSRP. These are largely short-term rescue activities. They can contribute to stronger immunization systems, but only with deliberate intent to do so.
Current global resources are insufficient to achieve MRSF longer-term goals. To prevent outbreaks, stronger management of measles and rubella programs is needed at all levels, including robust government commitment. To decrease the number of unprotected children, coverage needs to be increased for both routine doses of measles and rubella vaccine, and countries need policies for systematic catch-up of under-vaccinated or unvaccinated children up to 5 years of age. High quality campaigns need to be planned over multiple years in low coverage settings, as supported by an ongoing initiative from the M&RP. Tracking is needed to ensure that countries get timely support, whether at the stage of making a funding application, planning, implementing, or evaluating the campaign. Clear age-range eligibility criteria are needed to help address any immunity gaps in age groups outside the 9–59-month range. Long-term sustainable technical capacity needs to be built within countries and regions. Consideration of new approaches to campaigns include subnational and selective strategies for which interim guidance is under development. Longer planning horizons and streamlining of donor funding will also enable campaign integration with other vaccine antigens including polio.
Vertical and horizontal programs
Global goals will not be met without both disease specific and health system approaches, what has now been called a “diagonal” approach (31). This requires stronger immunization systems, and higher quality comprehensive surveillance and monitoring, including to subnational levels (32).
Countries with low coverage of the second routine measles vaccine dose need to strengthen services for children in the second year of life. This requires that health workers and parents be informed actively and positively about the need to get that second dose, and the opportunity this brings to receive other vaccines and services. All children should remain eligible for vaccination up to at least 5 years of age, reinforced through a school entry immunization check.
Implementing innovation
In settings where 10-dose measles or measles–rubella vaccine vials are used, healthcare workers are reluctant to open a vial for a single child or a few children for fear of wasting vaccine doses, even though policies allow for this. This results in children being turned away for measles vaccination, which is an example of a missed opportunity for vaccination (MOV). These children remain unprotected and may never return for this missed vaccination. A simple change to using a 5-dose vial helps to address the health worker reluctance that leads to the MOV, and this product change is now being rolled out in increasing numbers of countries (33).
Measles and rubella microarray patch vaccines (MR-MAPs) are potentially a game-changing new technology (34). Not requiring a full cold chain or trained health worker to administer, these patches are anticipated to increase the reach of routine immunization, outbreak response, and campaigns. MR-MAPs offer a chance to develop new manufacturing lines and, via technology, secure a broader base of manufacturers. Rapid diagnostic tests (RDTs) may potentially strengthen surveillance of measles and rubella in areas where laboratory testing access is weak, enabling faster outbreak detection and response (35). Both MR-MAPs and RDTs need accelerated feasibility testing and implementation research to support policy development particularly in low-income settings.
Looking to the future, a new measles vaccine strain or technology with similar effectiveness to rubella vaccine at 6 months of age or younger would increase the feasibility of achieving and sustaining measles and rubella elimination. Future trials of MR-MAPs should include administration at 6 months of age given the potential for intradermal vaccines to be more effective than subcutaneous ones.
Rubella eradication is highly feasible, conservatively requiring only 80% coverage. A global drive toward rubella eradication could help strengthen routine immunization systems, including the second year of life and school entry checks, and increase momentum toward measles elimination.
Conclusions
Goals for measles and rubella elimination require prioritization at subnational, national, and global levels. Sustainability of measles elimination relies on strong immunization systems, but progress on increasing routine measles coverage is too slow and inequitable to achieve and sustain elimination. Greater commitment – at all levels and across all partners – to operationalizing the concept of measles as a tracer for social inequity could drive stronger routine immunization and better meet the health needs of vulnerable populations. Better coordinated strategies to increase campaign quality will also potentially reduce inequities. Strategies to reduce inequity in the burden of CRS by introducing rubella vaccine in countries yet to have access to the vaccine could also support progress on measles elimination.
Sustainability is a key determinant of successful measles elimination – both important and hard to achieve. Countries can achieve elimination through heroic efforts to reach all children through regular campaigns, but sustaining elimination requires a stronger primary health care system and more equitable essential immunization services. Campaigns are a sprint in which everyone is focused on a single goal. Achieving and sustaining elimination is a team sport. Everyone at all levels – global, regional, national, and subnational – has to play their part to win this match, and if some key players are not in the game, then the goal may be lost from the start.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH and/or the Pan American Health Organization (PAHO) and/or the World Health Organization (WHO), and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Funding Statement
This article was supported by the grant or cooperative agreement NU66GH002171 by the U.S. Centers for Disease Control and Prevention.
Footnotes
Funding.
This article was supported by the grant or cooperative agreement NU66GH002171 by the U.S. Centers for Disease Control and Prevention.
REFERENCES
- 1.Minta AA, Ferrari M, Antoni S, Portnoy A, Sbarra S, Lambert B, et al. Progress Toward Measles Elimination – Worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep. 2023;72(46):1262–1268. doi: 10.15585/mmwr.mm7246a3. [DOI] [PMC free article] [PubMed] [Google Scholar]; Minta AA, Ferrari M, Antoni S, Portnoy A, Sbarra S, Lambert B, et al. Progress Toward Measles Elimination – Worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep. 2023;72(46):1262–1268. https://doi.org/10.15585/mmwr.mm7246a3. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization . Feasibility Assessment of Measles and Rubella Eradication. Report to the Strategic Advisory Group of Experts. Geneva: WHO; [8 October 2019]. 2019. [[cited 21 January 2024]]. Available from: https://terrance.who.int/mediacentre/data/sage/SAGE_Docs_Ppt_Oct2019/4_session_measles_and_rubella_vaccines/Oct2019_session4_feasibility_assessment_Measles-Rubella_eradication.pdf. [Google Scholar]; World Health Organization. Feasibility Assessment of Measles and Rubella Eradication. Report to the Strategic Advisory Group of Experts. 8 October 2019. Geneva: WHO; 2019 [cited 21 January 2024]. Available from: https://terrance.who.int/mediacentre/data/sage/SAGE_Docs_Ppt_Oct2019/4_session_measles_and_rubella_vaccines/Oct2019_session4_feasibility_assessment_Measles-Rubella_eradication.pdf.
- 3.World Health Organization . Immunization Agenda 2030: A Global Strategy to Leave No One Behind. Geneva: WHO; 2020. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030. [Google Scholar]; World Health Organization. Immunization Agenda 2030: A Global Strategy to Leave No One Behind. Geneva: WHO; 2020. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030.
- 4.World Health Organization . Measles and Rubella Strategic Framework: 2021–2030. Geneva: WHO; 2020. Available from: https://iris.who.int/handle/10665/339801. [Google Scholar]; World Health Organization. Measles and Rubella Strategic Framework: 2021–2030. Geneva: WHO; 2020. Available from: https://iris.who.int/handle/10665/339801.
- 5.Pan American Health Organization . The Challenge of Maintaining the Elimination of Measles in the Americas, 2017-2018. Immunization Newsletter, v.40, n.3, Sep. 2018. Washington, D.C.: PAHO; 2018. Available from: https://iris.paho.org/handle/10665.2/54261. [Google Scholar]; Pan American Health Organization. The Challenge of Maintaining the Elimination of Measles in the Americas, 2017-2018. Immunization Newsletter, v.40, n.3, Sep. 2018. Washington, D.C.: PAHO; 2018. Available from: https://iris.paho.org/handle/10665.2/54261.
- 6.Vynnycky E, Knapp JK, Papadopoulos T, Cutts FT, Hachiya M, Miyano S, et al. Estimates of the global burden of Congenital Rubella Syndrome, 1996-2019. Int J Infect Dis. 2023 Dec;137:149–156. doi: 10.1016/j.ijid.2023.09.003. https://doi.org/10.1016%2Fj.ijid.2023.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]; Vynnycky E, Knapp JK, Papadopoulos T, Cutts FT, Hachiya M, Miyano S, et al. Estimates of the global burden of Congenital Rubella Syndrome, 1996-2019. Int J Infect Dis. 2023 Dec;137:149–156. https://doi.org/10.1016%2Fj.ijid.2023.09.003. [DOI] [PMC free article] [PubMed]
- 7.World Health Organization . Immunization dashboard. Geneva: WHO; 2024. [[cited 15 July 2024]]. Available from: https://immunizationdata.who.int/ [Google Scholar]; World Health Organization. Immunization dashboard. Geneva: WHO; 2024 [cited 15 July 2024]. Available from: https://immunizationdata.who.int/.
- 8.Sim SY, Watts E, Constenla D, Brenzel L, Patenaude BN. Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011-30. Health Aff (Millwood) 2020;39(8):1343–1353. doi: 10.1377/hlthaff.2020.00103. [DOI] [PubMed] [Google Scholar]; Sim SY, Watts E, Constenla D, Brenzel L, Patenaude BN. Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011-30. Health Aff (Millwood). 2020;39(8):1343–1353. https://doi.org/10.1377/hlthaff.2020.00103. [DOI] [PubMed]
- 9.Carter A, Msemburi W, Sim SY, Gaythorpe KAM, Lambach P, Lindstrand A, et al. Modeling the impact of vaccination for the immunization Agenda 2030: Deaths averted due to vaccination against 14 pathogens in 194 countries from 2021 to 2030. Vaccine. 2024;42(Suppl 1):S28–S37. doi: 10.1016/j.vaccine.2023.07.033. [DOI] [PubMed] [Google Scholar]; Carter A, Msemburi W, Sim SY, Gaythorpe KAM, Lambach P, Lindstrand A, et al. Modeling the impact of vaccination for the immunization Agenda 2030: Deaths averted due to vaccination against 14 pathogens in 194 countries from 2021 to 2030. Vaccine. 2024;42(Suppl 1):S28–S37. https://doi.org/10.1016/j.vaccine.2023.07.033. [DOI] [PubMed]
- 10.Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, et al. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017;17(12):e420–e428. doi: 10.1016/s1473-3099(17)30307-9. [DOI] [PubMed] [Google Scholar]; Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, et al. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017;17(12):e420–e428. https://doi.org/10.1016/s1473-3099(17)30307-9. [DOI] [PubMed]
- 11.Lessler J, Metcalf CJE. Balancing evidence and uncertainty when considering rubella vaccine introduction. PLoS One. 2013;8(7):e67639. doi: 10.1371/journal.pone.0067639. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lessler J, Metcalf CJE. Balancing evidence and uncertainty when considering rubella vaccine introduction. PLoS One. 2013;8(7):e67639. https://doi.org/10.1371/journal.pone.0067639. [DOI] [PMC free article] [PubMed]
- 12.Keeling MJ, Grenfell BT. Disease extinction and community size: modeling the persistence of measles. Science. 1997;275(5296):65–67. doi: 10.1126/science.275.5296.65. [DOI] [PubMed] [Google Scholar]; Keeling MJ, Grenfell BT. Disease extinction and community size: modeling the persistence of measles. Science. 1997;275(5296):65–67. https://doi.org/10.1126/science.275.5296.65. [DOI] [PubMed]
- 13.Metcalf CJE, Munayco CV, Chowell G, Grenfell BT, Bjørnstad ON. Rubella metapopulation dynamics and importance of spatial coupling to the risk of congenital rubella syndrome in Peru. J R Soc Interface. 2011;8(56):369–376. doi: 10.1098/rsif.2010.0320. [DOI] [PMC free article] [PubMed] [Google Scholar]; Metcalf CJE, Munayco CV, Chowell G, Grenfell BT, Bjørnstad ON. Rubella metapopulation dynamics and importance of spatial coupling to the risk of congenital rubella syndrome in Peru. J R Soc Interface. 2011;8(56):369–376. https://doi.org/10.1098/rsif.2010.0320. [DOI] [PMC free article] [PubMed]
- 14.Durrheim DN, Crowcroft NS. The price of delaying measles eradication. Lancet Public Health. 2017;2(3):e130–e131. doi: 10.1016/s2468-2667(17)30026-9. [DOI] [PubMed] [Google Scholar]; Durrheim DN, Crowcroft NS. The price of delaying measles eradication. Lancet Public Health. 2017;2(3):e130–e131. https://doi.org/10.1016/s2468-2667(17)30026-9. [DOI] [PubMed]
- 15.Wellesley Institute . Health systems and health equity. Toronto: Wellesley Institute; [[cited 21 January 2024]]. [date unknown] Available from: https://www.wellesleyinstitute.com/streams/health-systems-and-health-equity. [Google Scholar]; Wellesley Institute. Health systems and health equity. Toronto: Wellesley Institute; [date unknown] [cited 21 January 2024]. Available from: https://www.wellesleyinstitute.com/streams/health-systems-and-health-equity.
- 16.United Nations, Department of Economic and Social Affairs . Proportion of the target population covered by all vaccines included in their national programme. Sustainable Development Goal SDG3 indicator 3b 1.3. New York: United Nations; 2024. [[cited 28 January 2024]]. Available from: https://sdgs.un.org/goals/goal3. [Google Scholar]; United Nations, Department of Economic and Social Affairs. Proportion of the target population covered by all vaccines included in their national programme. Sustainable Development Goal SDG3 indicator 3b 1.3. New York: United Nations; 2024 [cited 28 January 2024]. Available from: https://sdgs.un.org/goals/goal3.
- 17.Grant GB, Zimmerman L. Decreases in Congenital Rubella Syndrome Reflect Concerted Efforts Toward Rubella and Measles Elimination. Int J Infect Dis. 2023 Dec;137:162. doi: 10.1016/j.ijid.2023.10.012. [DOI] [PubMed] [Google Scholar]; Grant GB, Zimmerman L. Decreases in Congenital Rubella Syndrome Reflect Concerted Efforts Toward Rubella and Measles Elimination. Int J Infect Dis. 2023 Dec;137:162. https://doi.org/10.1016/j.ijid.2023.10.012. [DOI] [PubMed]
- 18.Strebel PM, Cochi SL, Hoekstra E, Rota PA, Featherstone D, Bellini WJ, et al. A world without measles. J Infect Dis. 2011 Jul;204(Suppl 1):S1–S3. doi: 10.1093/infdis/jir111. [DOI] [PubMed] [Google Scholar]; Strebel PM, Cochi SL, Hoekstra E, Rota PA, Featherstone D, Bellini WJ, et al. A world without measles. J Infect Dis. 2011 Jul;204(Suppl 1):S1–S3. https://doi.org/10.1093/infdis/jir111. [DOI] [PubMed]
- 19.Rodney W. How Europe Underdeveloped Africa. London: Bogle-L’Ouverture Publications; 1972. [Google Scholar]; Rodney W. How Europe Underdeveloped Africa. London: Bogle-L’Ouverture Publications; 1972.
- 20.United Nations Educational, Scientific and Cultural Organization . Launch of the Report on “Healing the Wounds of Trans-Atlantic Slave Trade and Slavery”. Paris: UNESCO; [21 May 2021]. 2021. [[cited 21 January 2024]]. Available from: https://www.unesco.org/en/articles/launch-report-healing-wounds-trans-atlantic-slave-trade-and-slavery. [Google Scholar]; United Nations Educational, Scientific and Cultural Organization. Launch of the Report on “Healing the Wounds of Trans-Atlantic Slave Trade and Slavery”. 21 May 2021. Paris: UNESCO; 2021 [cited 21 January 2024]. Available from: https://www.unesco.org/en/articles/launch-report-healing-wounds-trans-atlantic-slave-trade-and-slavery.
- 21.Nunn N. Vox EU. 27 February 2017. [London]: Centre for Economic Policy Research; 2017. [[cited 21 January 2024]]. Understanding the long-run effects of Africa’s slave trades. Available from: https://cepr.org/voxeu/columns/understanding-long-run-effects-africas-slave-trades. [Google Scholar]; Nunn N. Understanding the long-run effects of Africa’s slave trades. Vox EU. 27 February 2017. [London]: Centre for Economic Policy Research; 2017 [cited 21 January 2024]. Available from: https://cepr.org/voxeu/columns/understanding-long-run-effects-africas-slave-trades.
- 22.Reuters Africa seeks action plan on slavery reparations at Ghana conference. [15 November 2023]. [[cited 21 January 2024]]. Available from: https://www.reuters.com/world/africa/africa-seeks-action-plan-slavery-reparations-ghana-conference-2023-11-14/; Reuters. Africa seeks action plan on slavery reparations at Ghana conference. 15 November 2023 [cited 21 January 2024]. Available from: https://www.reuters.com/world/africa/africa-seeks-action-plan-slavery-reparations-ghana-conference-2023-11-14/.
- 23.World Health Organization . United Nations Children’s Fund, GAVI the Vaccine Alliance. Geneva: WHO; 2023. The big catch-up: an essential immunization recovery plan for 2023 and beyond. Available from: https://iris.who.int/handle/10665/371801. [Google Scholar]; World Health Organization, United Nations Children’s Fund, GAVI the Vaccine Alliance. The big catch-up: an essential immunization recovery plan for 2023 and beyond. Geneva: WHO; 2023. Available from: https://iris.who.int/handle/10665/371801.
- 24.Truelove SA, Graham M, Moss WJ, Metcalf CJE, Ferrari MJ, Lessler J. Characterizing the impact of spatial clustering of susceptibility for measles elimination. Vaccine. 2019;37(5):732–741. doi: 10.1016/j.vaccine.2018.12.012. https://doi.org/10.1016%2Fj.vaccine.2018.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]; Truelove SA, Graham M, Moss WJ, Metcalf CJE, Ferrari MJ, Lessler J. Characterizing the impact of spatial clustering of susceptibility for measles elimination. Vaccine. 2019;37(5):732–741. https://doi.org/10.1016%2Fj.vaccine.2018.12.012. [DOI] [PMC free article] [PubMed]
- 25.Deer B. How the case against the MMR vaccine was fixed. BMJ. 2011 Jan 5;342:342. doi: 10.1136/bmj.c5347. [DOI] [PubMed] [Google Scholar]; Deer B. How the case against the MMR vaccine was fixed. BMJ. 2011 Jan 5;342:c5347. https://doi.org/10.1136/bmj.c5347. [DOI] [PubMed]
- 26.de Quadros CA, Olivé JM, Hersh BS, Strassburg MA, Henderson DA, Brandling-Bennett D, et al. Measles elimination in the Americas. Evolving strategies. JAMA. 1996;275(3):224–229. doi: 10.1001/jama.1996.03530270064033. [DOI] [PubMed] [Google Scholar]; de Quadros CA, Olivé JM, Hersh BS, Strassburg MA, Henderson DA, Brandling-Bennett D, et al. Measles elimination in the Americas. Evolving strategies. JAMA. 1996;275(3):224–229. https://doi.org/10.1001/jama.1996.03530270064033. [DOI] [PubMed]
- 27.World Health Organization . Rubella vaccines: WHO position paper – July 2020. 27. Vol. 95. Wkly Epidemiol Rec.; 2020. pp. 301–324. Available from: https://www.who.int/publications/i/item/WHO-WER9527. [Google Scholar]; World Health Organization. Rubella vaccines: WHO position paper – July 2020. Wkly Epidemiol Rec. 2020;95(27):301–324. Available from: https://www.who.int/publications/i/item/WHO-WER9527.
- 28.O’Connor Patrick. Immunity profiles. [15 January 2024];Personal communication with: U.S. Centers for Disease Control and Prevention. [Google Scholar]; O’Connor, Patrick. Immunity profiles. Personal communication with: U.S. Centers for Disease Control and Prevention. 15 January 2024.
- 29.World Health Organization . Measles Outbreaks Strategic Response Plan: 2021–2023. Geneva: WHO; 2021. Available from: https://iris.who.int/handle/10665/340657. [Google Scholar]; World Health Organization. Measles Outbreaks Strategic Response Plan: 2021–2023. Geneva: WHO; 2021. Available from: https://iris.who.int/handle/10665/340657.
- 30.Mulders MN, Rota PA, Icenogle JP, Brown KE, Takeda M, Rey GJ, et al. Global Measles and Rubella Laboratory Network Support for Elimination Goals, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(17):438–442. doi: 10.15585/mmwr.mm6517a3. [DOI] [PubMed] [Google Scholar]; Mulders MN, Rota PA, Icenogle JP, Brown KE, Takeda M, Rey GJ, et al. Global Measles and Rubella Laboratory Network Support for Elimination Goals, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(17):438–442. https://doi.org/10.15585/mmwr.mm6517a3. [DOI] [PubMed]
- 31.Orenstein WA, Seib K. Beyond vertical and horizontal programs: a diagonal approach to building national immunization programs through measles elimination. Expert Rev Vaccines. 2016;15(7):791–793. doi: 10.1586/14760584.2016.1165614. [DOI] [PubMed] [Google Scholar]; Orenstein WA, Seib K. Beyond vertical and horizontal programs: a diagonal approach to building national immunization programs through measles elimination. Expert Rev Vaccines. 2016;15(7):791–793. https://doi.org/10.1586/14760584.2016.1165614. [DOI] [PubMed]
- 32.World Health Organization . Global Strategy on Comprehensive Vaccine-Preventable Disease Surveillance. Geneva: WHO; 2020. Available from: https://www.who.int/publications/m/item/global-strategy-for-comprehensive-vaccine-preventable-disease-(vpd)-surveillance. [Google Scholar]; World Health Organization. Global Strategy on Comprehensive Vaccine-Preventable Disease Surveillance. Geneva: WHO; 2020. Available from: https://www.who.int/publications/m/item/global-strategy-for-comprehensive-vaccine-preventable-disease-(vpd)-surveillance.
- 33.Krudwig K, Knittel B, Karim A, Kanagat N, Prosser W, Phiri G, et al. The effects of switching from 10 to 5-dose vials of MR vaccine on vaccination coverage and wastage: A mixed-method study in Zambia. Vaccine. 2020;38(37):5905–5913. doi: 10.1016/j.vaccine.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]; Krudwig K, Knittel B, Karim A, Kanagat N, Prosser W, Phiri G, et al. The effects of switching from 10 to 5-dose vials of MR vaccine on vaccination coverage and wastage: A mixed-method study in Zambia. Vaccine. 2020;38(37):5905–5913. https://doi.org/10.1016/j.vaccine.2020.07.012. [DOI] [PMC free article] [PubMed]
- 34.Adigweme I, Yisa M, Ooko M, Akpalu E, Bruce A, Donkor S, et al. A measles and rubella vaccine microneedle patch in The Gambia: a phase 1/2, double-blind, double-dummy, randomised, active-controlled, age de-escalation trial. Lancet. 2024;403(10439):1879–1892. doi: 10.1016/s0140-6736(24)00532-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Adigweme I, Yisa M, Ooko M, Akpalu E, Bruce A, Donkor S, et al. A measles and rubella vaccine microneedle patch in The Gambia: a phase 1/2, double-blind, double-dummy, randomised, active-controlled, age de-escalation trial. Lancet. 2024;403(10439):1879–1892. https://doi.org/10.1016/s0140-6736(24)00532-4. [DOI] [PMC free article] [PubMed]
- 35.Brown DW, Warrener L, Scobie HM, Donadel M, Waku-Kouomou D, Mulders MN, et al. Rapid diagnostic tests to address challenges for global measles surveillance. Curr Opin Virol. 2020 Apr;41:77–84. doi: 10.1016/j.coviro.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]; Brown DW, Warrener L, Scobie HM, Donadel M, Waku-Kouomou D, Mulders MN, et al. Rapid diagnostic tests to address challenges for global measles surveillance. Curr Opin Virol. 2020 Apr;41:77–84. https://doi.org/10.1016/j.coviro.2020.05.007. [DOI] [PMC free article] [PubMed]


