Introduction
In recent years, the management of obesity has evolved substantially with the introduction of long-acting glucagon-like peptide-1 (GLP-1) receptor agonists, also known as third-generation antiobesity medications. These pharmacotherapies have demonstrated remarkable efficacy, not only in promoting weight loss but also in improving metabolic outcomes. However, with obesity affecting more than 42% of adults in the United States,1 these advancements bring challenges related to access, long-term management, and the broader implications for health care systems. In this expert panel discussion, The Permanente Journal gathered experts from across the field of obesity medicine to share their insights on the clinical, systemic, and societal impacts of these new therapies. Together, we aim to explore the opportunities and challenges in optimizing patient care and advancing equitable, sustainable solutions for the treatment of obesity.
Expert Panel Discussion
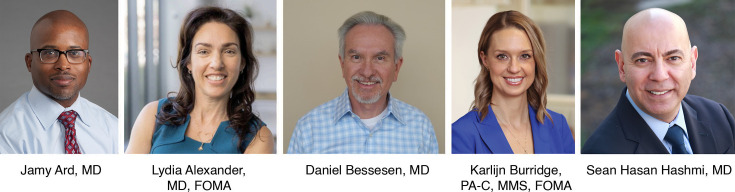
Jamy Ard
I will start by saying it is great to have the opportunity to convene this panel to discuss the use of antiobesity medications in health care. I am Jamy Ard. I am a professor of epidemiology and prevention at Wake Forest University School of Medicine in Winston-Salem, NC, where I codirect our weight management center. I also have the pleasure of serving as president of The Obesity Society.
Right now, the world is clamoring to hear how clinicians practicing in this space are thinking about GLP-1 agonists and antiobesity medications. Because each of you on this panel is an expert in this space, I look forward to engaging with you for this conversation.
Karlijn Burridge
I'm Karlijn Burridge, and I'm a physician associate. I appreciate the invitation to this panel. I am a cofounder and the immediate past president of the official American Academy of Physician Associates caucus, PAs in Obesity Medicine. I am also the secretary on the board of the Illinois Obesity Society, and I'm a trustee of the Obesity Medicine Association. Clinically, I work at an obesity specialty practice for adults and adolescents in Westmont, IL, in the Chicago area. I also own a business that provides resources and support to clinicians to start or optimize an obesity program.
Lydia Alexander
I'm Lydia Alexander and I am the chief medical officer for Enara Health, a San Francisco–area telehealth platform. My organization provides medical practices with evidence-based lifestyle and obesity interventions alongside medications approved by the US Food and Drug Administration (FDA) under the care of obesity-specialized physicians and health coaches via video visits and in-person care. It is also my pleasure to serve as the current president of the Obesity Medicine Association. By training, I am an internal medicine physician also certified in obesity medicine, lifestyle medication, and educated as a medical chef. I am passionate about culinary medicine, nutrition, and reversing chronic disease by treating obesity first. Prior to Enara, I worked as part of the Kaiser Permanente Medical Weight Management Program.
Sean Hasan Hashmi
I'm Sean Hashmi. I'm the regional director of the lifestyle and obesity medicine division for the Southern California Permanente Medical Group. I also chair Kaiser Permanente’s national interregional clinical practice group, which brings all the Kaiser Permanente medical groups together with regards to lifestyle and obesity medicine. My background is nephrology and obesity medicine.
Daniel Bessesen
I'm Daniel Bessesen. I'm a professor in the division of endocrinology, metabolism, and diabetes at the University of Colorado (CU). I do my clinical work at Denver Health Medical Center. I'm the director of the Anschutz Health and Wellness Center on the campus of the CU School of Medicine. I do research on appetite and body weight regulation. I'm the director of the obesity medicine fellowship program at CU, and I'm a past president of The Obesity Society.
Jamy Ard
Thank you to all for the introductions. As we can see, we have some great leadership present for this expert panel discussion.
What do you think has changed in clinical practice with the introduction of the third-generation antiobesity medications, including once-weekly semaglutide, tirzepatide, and the like? These are the weight loss medications that everybody is talking about right now. What do you think has changed with the introduction of these products into clinical practice from the patient perspective, from your perspectives as clinicians, from a health care system perspective, or even from a societal level, with awareness growing among the general public about these types of medications?
Karlijn Burridge
One thing that has changed is that a lot of people are talking about these medications, as Dr Ard mentioned. Up until the past few years, nobody was talking about antiobesity medications, and if we mentioned using them, people often would look at you strangely and wonder what you're talking about. The general awareness now that these medications exist and the increasing discussion around them, whether good or bad, accounts for a major shift within the general public.
From my perspective as a clinician, it’s been great to have these medications available as a more powerful tool in treating obesity and preobesity. We are seeing percentage weight changes that we weren't previously seeing with other medications. Of course, with this comes the improvement or resolution of other associated disease states or diseases that are directly caused by obesity.
The payer perspective comes to mind as well, but what stands out to me most is the impact I can directly observe within clinical practice with my patients. We can see substantial changes in body weight that we could not attain previously. The effect that these third-generation antiobesity medications have had on obesity-related complications and quality of life has been impressive.
Jamy Ard
Dr Hashmi, I am interested in your perspective, given that you are part of Kaiser Permanente’s large integrated health system. What changes have you observed with the third-generation antiobesity medications from a health system perspective?
Sean Hasan Hashmi
Years ago, physicians fought to get obesity classified as a disease. What was interesting was that, for many years, the prevailing knowledge was that if a person simply exercised more and ate less, that would be the end of obesity and its related complications. Paying proper attention to obesity and putting it on the same level as other diseases such as diabetes, hypertension, heart disease, and other major diseases, never seemed to be on the map.
These drugs have opened a new wave of understanding of obesity. They have helped to legitimize the field of obesity medicine. We have so many colleagues and amazing candidates who want to go into obesity care from a board certification perspective, whereas before these medications were on the scene, there was a major shortage of interest.
Now, we can build entire service lines. Kaiser Permanente is working to build divisions of obesity medicine in all regions. Within the Southern California region, all 13 medical centers now have lifestyle and obesity medicine divisions.
As we begin to talk about new treatments, one of the challenges we have with the health care system is the issue of equity. In other words, the patients who absolutely need our care are at times the ones who do not ask for it, or who can't afford care. As a result, we see that a lot of the folks who jump on the bandwagon of GLP-1 agonists as a solution to weight loss concerns are the ones who may not necessarily need priority-level treatment to the same degree as other patients who truly need the medications to manage health issues. Balancing quality, affordable, evidence-based medicine is important, but it is also important to ensure equitable care.
Jamy Ard
Dr Bessesen, from a clinician standpoint, what do you see as the challenge or the benefit? What’s changed in the clinical space regarding equity issues and patients coming in to ask for treatment?
Daniel Bessesen
It is hard to generalize, but I think it’s fair to say that most physicians right now are getting questions about antiobesity medications from their patients. The development of these highly effective medications has been accompanied by evidence not just for weight loss, but benefits for cardiovascular risk, pulmonary disease, fatty liver disease, emerging evidence in renal disease, and, obviously, type 2 diabetes.
Cardiologists and nephrologists, to name a couple, are being asked to think about these drugs and about treating the problem of obesity, along with a number of different specialty physicians who either were uncomfortable talking about weight or didn't feel like these antiobesity medications were safe and effective therapies. For many clinicians who don’t specialize in obesity, these drugs present a new area for them. They may wonder, “Why would a cardiologist be talking about a weight loss medication?” I feel we are at an inflection point as more and more clinicians become aware of the potential importance of treating obesity.
I was in practice during the fenfluramine/phentermine (fen-phen) era in the 1990s. That was an interesting time because, for the first time in my professional life, I had patients coming to a clinic appointment requesting specific doses of these antiobesity medications. They would even go as far as to provide the phone number for their pharmacy. What’s interesting is that nothing like that happens with, let’s say, Lasix or insulin. Nobody comes into a physician’s practice and specifically requests 20 mg of Lasix or to be put on 40 units of insulin glargine. But that was what was happening with fen-phen back then, and a similar phenomenon is happening now around the newest antiobesity medications.
I am seeing patients who are coming to my office in response to media advertisements they’ve seen about new highly effective antiobesity medications. It’s exciting because it means they're thinking about their weight as a health problem. They want to do something about it, but they often have incomplete information. This can be frustrating to the clinician because limited availability, insurance coverage, and the costs of these antiobesity medications persist as major barriers. If the clinician is all that stands between a patient who may be incompletely informed and a health care system that is not supportive of these interventions, the clinician may feel inadequately prepared. This makes it a challenging time for most clinicians right now.
Jamy Ard
Those are really great points, Dr Bessesen. Building on top of that, we have a growing number of patients who are interested in treatments and a growing workforce interested in providing these treatments, although the frustrations that many clinicians experience are valid. It can feel like there will be a breaking point when the system is going to totally implode, and yet there persists a sense of optimism and hope when, for instance, celebrity figures such as Oprah Winfrey are advocating that obesity can be treatable. Broadly speaking, where do you see things going with the introduction of these medications?
Lydia Alexander
There are pros and cons to all of what you have just said. It’s a double-edged sword. Having Oprah Winfrey speak publicly about taking GLP-1s after seeing her grapple with her weight over the past 40 years has helped to reduce the stigma and bias of the disease of obesity. Even as a celebrity with personal access to chefs and trainers, it was still incredibly difficult for her to manage her weight health, and it’s great to see her speak publicly about obesity and antiobesity drugs. As clinicians, we know how difficult it is for patients to talk to their primary care practitioners about something often considered to be more in the domain of personal willpower and effort. Patients over the decades have received the signal that obesity is simply because they're just not trying hard enough.
We have made strides in treating obesity with intensive lifestyle interventions in combination with antiobesity medications, but weight bias and stigma still persist. I have patients who will not speak about matters related to weight or obesity in public, who hide the fact that they are taking antiobesity medications while openly discussing the lifestyle changes they are making.
A decade ago, we as clinicians were getting excited when our patient attained 5% or 10% weight loss. With third-generation antiobesity medications, we're seeing weight reductions nearly on par with those who have undergone a sleeve gastrectomy. We know through prior metabolic bariatric surgery studies the many benefits conferred with this degree of weight loss (such as remission in type 2 diabetes and decreases in certain types of cancer), and we can extrapolate these benefits to weight loss achieved with second- and third-generation medications. Antiobesity medication studies will continue to be published, confirming the promise of these same health benefits with pharmacotherapy, such as a 20% risk reduction in major adverse cardiovascular (MACE) events, defined as a composite of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke from the Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial.2 This clinical trial was specifically designed to evaluate whether semaglutide 2.4 mg, a GLP-1 receptor agonist approved for weight management, could reduce the risk of MACE in individuals with overweight or obesity and established cardiovascular disease without type 2 diabetes. This primary endpoint was reached over a mean follow-up of 39.8 months.
Jamy Ard
From a clinical perspective, do you think these antiobesity treatments, as they currently stand, should be considered first-line therapy?
Karlijn Burridge
The discussion around first-line treatments for obesity is tricky. One of the reasons it’s tricky is because obesity is such a heterogeneous disease, and there are so many different levels of severity of obesity and related complications that it’s hard to say that any one medication should be first-line, especially when you consider the cost and accessibility of some of these medications.
If we could take cost and accessibility out of the equation, it might be a different discussion, but those are issues that we are grappling with today. Do I think that a GLP-1 agonist should be the first line for every patient with obesity given the current environment? No, not necessarily. I think there are patients who may be great candidates for oral medications that have been around for a long time and are more affordable and more accessible. We need to take all those factors into consideration and that’s where personalized medicine comes into play. We as clinicians should be treating the individual patient who is in front of us and remembering that not all our patients need to achieve a 15% or 20% body weight reduction.
We clinicians need to take those different factors into consideration when we're deciding which medication may be a good fit for which patient. These factors are the reason we don't have a first-line agent in obesity care right now. Unfortunately, right now, cost and access are still 2 of the top barriers to contend with when making decisions around pharmacotherapy.
Lydia Alexander
I would concur with Ms Burridge. There are several dozen different antiobesity medications in various phases of trials happening at this moment.3 This tells us there will be a whole new wave of medications coming to market at some point soon. Medication-related decisions will really depend on the patient’s disease state and the complications from obesity the patient is being treated for.
Clinicians should work toward how they can help their patients make the most progress and determine how much weight they need to lose. This process needs to take into consideration any other disease processes occurring that can be concurrently addressed and, from there, which medication would be first-line can be determined for that specific patient.
Jamy Ard
Dr Bessesen, because you are an endocrinologist, I’d like to ask whether you think we will get to a point where we treat obesity in a similar fashion as we do type 2 diabetes.
Daniel Bessesen
Right now, we have medications that are more effective than anything we've had before. To Dr Alexander’s point, there are a large number of even newer antiobesity medications in the development pipeline, some of which are likely to give up to 25% weight loss in some individuals.4,5 This raises the question: What is the goal of antiobesity therapy? In diabetes, we have a clear goal to achieve an A1C of < 7. For blood pressure, we have clear evidence-based targets. For low-density lipoprotein (LDL) cholesterol, we have targets of therapy.
So far, because our therapies have been so ineffective, our guidelines have focused on who should be offered therapy, rather than what the goals of therapy should be. A 5% weight loss is considered clinically meaningful, but should the goal be 10%, 15%, or 20% in some people? Is there such a thing as too much weight loss? Additionally, our goals thus far have focused on weight rather than a holistic view that integrates other health problems. In a person with multiple weight-related health problems, how do we prioritize medications for weight in the context of their other diagnoses? Diabetes care is evolving and becoming more sophisticated. Treatment of a patient with diabetic nephropathy could involve 4 or 5 different medications. Patients with hyperlipidemia, hypertension, and arthritis could end up being prescribed 4 or 5 medications for these problems. How do we decide the “best medications” to use in patients like these, and who will make these decisions, specialists or primary care practitioners?
I think the biggest challenge is understanding the goals of therapy and knowing how to integrate comorbid conditions with weight management in a treatment plan that is efficient, cost-effective, and reaches targets. We have major work to do to achieve that goal.
Jamy Ard
Dr Hashmi, are there any other considerations that you have in mind when you're thinking about initiating therapy? What about safety and long-term treatment?
Sean Hasan Hashmi
Taking a step back, I ask the question, “When is too much of a good thing really good?” or when do we start to get into that trouble spot and when we start to talk about certain patients, for example, our elderly population.
There’s this thing called an obesity paradox, which is very simple. Suppose you had an elderly patient, a patient on dialysis, and a patient with cancer. After each of them goes through weight loss, their chance of mortality goes up, not down. Part of that reason is because of lean body mass loss. When we compare the new generation of weight loss drugs (ie, GLP-1s) to the older generation (oral agents such as metformin, phentermine, topiramate, Wellbutrin, and naltrexone), we find that lean muscle loss is actually greater.
In other words, the reason our department is called the division of lifestyle and obesity medicine is because lifestyle is so important, and it’s easy to forget that. What we found time and time again is that when we couple lifestyle modification with pharmaceutical or surgical therapy, we get far greater and more sustainable results.
We have patients now who have been combining lifestyle and medical therapies for several years, starting with the earlier days of Victoza, moving on to things like Saxenda, then moving on to the newer GLP-1 agonists, such as Ozempic, Wegovy, and tirzepatide. The issue we were dealing with was: What happens when a member fails the drug? We're so focused on the idea that we haven't seen these weight losses before, but what happens is you see this major weight loss and the patient’s former habits start to return. They have no appetite, no cravings, at the start of using antiobesity medications, but little by little the weight returns.
When we look at bariatric surgery, we take roughly 80% of a patient’s stomach when using the sleeve method. When we do the bypass method, we're actually causing not just restriction but also malabsorption. And yet at 10 years postsurgery, they're only able to keep off about 25% of the weight that they initially lost.
So with GLP-1s, the importance is not so much their initial effectiveness from a cost, safety, or health perspective. It’s more about the longer-term effectiveness. As Dr Alexander mentioned, we have about 25 new agents that are in phase 2 trials or phase 3 trials. We have 150 potential agents that may reach the market in the next 5 to 10 years, so there will be no shortage of drugs on the market in the next several years. The real problem is getting on a hamster wheel that once you get on, you become somewhat stuck and have to continue to use more potent drugs to continue the weight loss journey or to prevent regaining the weight. To step off the hamster wheel, health care practitioners need to look at the entire spectrum of obesity as a disease. This will require that clinicians stop blaming the patients, build the infrastructure for the onramp of these medications, build the infrastructure for the offramp, and always use lifestyle as the foundation for all treatments.
For many of us, when we look at high blood pressure medications, for example, the idea of patients ever coming off these drugs has escaped us. We have forgotten about the idea of ever taking anybody off their blood pressure medications, so often when we put someone on a drug like this, it becomes a lifelong endeavor, even when we do know there are some patients we can safely take off and that we can modify some of their risk factors to keep them safe.
From an equity perspective, that’s a whole other challenge we have yet to look at. Some of our most vulnerable populations don't even know what GLP-1s are. We haven't done a good enough job of reaching out to them yet.
Jamy Ard
Those are all important points, so thanks for raising them. I’d like to extend that line of thinking a little bit. Dr Hashmi, you talked about some of the components of safety and things that still need to be addressed. What do you see as the most important unmet needs we haven't quite addressed, even with these newest therapies? In what areas do you feel we still don't quite understand what we're doing with these newer medications or with what we currently have available?
Daniel Bessesen
I think some of it comes down to how we know what we know. Most of the information we have on the treatment of obesity comes from studies that are either funded by the National Institutes of Health (NIH) or by industry. Studies stemming from these funders answer certain kinds of questions. Studies funded by the NIH tend to answer physiologic questions or very rigorous methodologic studies of lifestyle treatment of obesity. Industry studies tend to provide data in support of bringing drugs to the market and justify their use in FDA-defined clinical settings.
Many questions do not fall into these 2 categories and yet are tremendously important. These range from “What is the real cost-effectiveness of antiobesity medications in real clinical environments?” to “How do we actually use lifestyle modification effectively either alone or in conjunction with medications?” and “How do we incorporate older medications into regimens alongside newer, more effective but more expensive medications?” Practical clinical questions like these could be answered by pragmatic trials conducted in real clinical environments by creating partnerships between large health care organizations, researchers with expertise in conducting clinical trials, pharmaceutical companies that could provide medication, and federal agencies with an interest in answering these questions, such as the US Department of Health and Human Services, the FDA, the NIH, and the Patient-Centered Outcomes Research Institute. It may be productive to develop and fund obesity clinical trial infrastructure much like we developed and funded cancer centers and AIDS clinical trial groups in the past to address these large public health problems.
Karlijn Burridge
I think there are still a lot of questions that are unanswered and a lot of research to be done. There is a lot more we don't know. But I think there is a lot that we do know. We've been using GLP-1s since Byetta, which was around 2005.6 We have also had the option for bariatric surgery for many years, and there’s a lot we can learn from bariatric surgery.
One of the things we don’t know right now is the impact of these types of medications on things like body composition and muscle mass loss, for instance. This remains something requiring further investigation. There are still a lot of questions around these aspects, but we do have some data from metabolic and bariatric surgery. Of course, these are not one and the same, especially when you're talking about procedures like the Roux-en-Y gastric bypass.
However, take the sleeve gastrectomy, for instance. We know that metabolic and bariatric surgery teams provide certain standard recommendations regarding nutrition and physical activity to minimize that loss. These points are very standardized, such as the bare minimum of 60 g of protein per day and making sure patients are doing exercise (especially resistance exercise) to minimize muscle mass loss. We have body composition analysis, so let’s use the tools we have so we can create better guidance around those lifestyle components.
I think lifestyle is changing. The recommendations for lifestyle used to be to try to create a caloric deficit either through nutrition or by adding physical activity or both. Now I think the focus on lifestyle is more about how to optimize nutrition with these medications where the appetite is substantially suppressed. How do clinicians ensure patients receive appropriate nutrition, sufficient protein, and the right type of physical activity to minimize muscle mass loss? Additionally, we must focus not just on muscle mass loss, but also on the function of the muscle and strength of the muscle.
Considering sarcopenic obesity, especially in some of the populations that we're talking about such as our elderly patients, these are answers that we need to have. But I think we can look to metabolic and bariatric surgery for some of those answers, and we have had GLP-1s and other medications for a long time.
We need more studies for sure, but in the interim, I think we can learn a lot from some of the tools we already have. I think that’s really where primary care practitioners need a lot more guidance around using these medications alongside lifestyle modification to really optimize the health of the patient. One concern I have is that we now have tools that are so powerful they are approaching bariatric surgery–level outcomes, but we don't yet have the support system around these tools like we do with metabolic and bariatric surgery. I think the bigger concern is around how we can provide guidance to primary care clinicians on how to use these tools safely and effectively.
Jamy Ard
Dr Hashmi mentioned long-term treatment strategies. I'm interested to hear what each of the panelists thinks we need to do in terms of a long-term treatment strategy. As Dr Hashmi said, maybe we need an offramp for these medications. Some people may be more of the mindset that with chronic disease, maybe an offramp is unnecessary because long-term treatment is preferable. Where do you think we go and what is your perspective on how we address the issue of long-term treatment?
Lydia Alexander
That is a great question. To piggyback off what Ms Burridge previously mentioned in terms of using a multimodal approach to manage obesity and all the different complications we see and treat as clinicians. When we start thinking about what to do with our patients, we need tools and support for comprehensive care of the patient. For instance, in the bariatric surgery setting, clinicians can offer patients nutrition support, physical activity support, and behavioral modification as part of a multimodal approach to care. We can optimize each of these components in addition to medication and medical interventions.
When we optimize our approach, at some point there can be an offramp for some patients, albeit a smaller subset and perhaps for a period when in remission. The National Weight Control Registry demonstrated that some people are treatable employing intensive lifestyle intervention measures without antiobesity medications and they can maintain a healthy weight over the years.7 Now, is this the majority of people? No. Are there some people who are going to be fortunate enough to reverse their inflammation and the different factors impacting their weight setpoint to achieve good overall health and meet their weight goals? Sure, some people are going to have that. Perhaps their adiposity is less severe and their metabolic weight regulation system is not yet permanently broken.
By optimizing all 4 pillars of treating weight and obesity, are we going to be able to take some people off these medications once they’ve been stable for several years or to have some type of stepdown therapy over time? I think this will be the case for some. We will need studies to understand who may be able to go off antiobesity medication therapy as well as criteria for establishing remission and for weaning. However, this is likely the exception, not the rule, and more likely to happen when we treat adiposity early on. Also, you never want to stop therapy when somebody is still in what I call part A, which is the weight loss portion of this journey that everybody tends to focus on. But if somebody has been well-maintained at a healthy weight for, say, 3 or 4 years, finding it relatively manageable without much fluctuation, a clinician might ask the patient if they’ve found it to be easy or difficult to stay where they are. If the answer is that it’s been fairly doable using the tools provided during follow-up care, then maybe deprescribing medication with close follow-up could be considered.
We will soon start to see that and it will be a next-generation conversation, which may be popular or unpopular for many reasons, where we think about obesity and treat it the same way we do a lot of other chronic, progressing, relapsing conditions.
Treating depression can serve as a good example. We physicians don't put patients on an antidepressant for just a couple of months but generally recommend a course of at least 6 to 12 months after achieving remission from depression, even if the patient feels better, because the maintenance phase helps prevent relapse. Once remission appears achieved, deprescribing will be fine for some patients, at least for a period of time, whereas others need to remain on the medication for life because symptoms return when deprescribed.
Ultimately, we need to calibrate the medication and treatment pathway to treat the individual disease state.
Jamy Ard
Dr Hashmi, if you could fund one research project that addresses a major or critical issue in this space, and pretend you had an unlimited budget, what research would you fund?
Sean Hasan Hashmi
Thanks for the question, Dr Ard. Let’s think about it this way. Right now, we know the effectiveness of drugs, but we don’t know the effectiveness of drugs within a multimodality specialty approach. In other words, when Dr Alexander talks about the 4 pillars, when we start to look at what makes obesity treatment more successful, what we really want to understand is how to best guide the decisions surrounding starting medication for success.
Although we have a good deal of experience with GLP-1 agonists, we lack that same level of experience when it comes to doubling the dosages, which we are now prescribing for weight loss. What are the impacts on the rest of people’s lives that we need to be aware of? If you look at social media, people will talk about the side effects, including a delay in gastric emptying. We are seeing now cases of patients having gastroparesis when taking GLP-1 agonists and the stomach motility has not returned upon drug cessation.
There have also been reported cases of depression affiliated with taking GLP-1 agonists. FDA data at 9 months of GLP-1 usage show that in terms of depression and suicidal ideation, it’s very low. But you also have very vulnerable active populations that you're starting on these drugs and in the first few months where you're taking their pleasure away, you're blocking something and you don’t have a replacement for it.
So the question that is really top of mind is what makes an effective antiobesity strategy, and I would argue that it is not GLP-1s in isolation. Rather, I feel it is an approach that we need to figure out as practitioners. There are no set data that guide us when we take somebody off GLP-1s. There are no real indications regarding an effective behavioral management therapy.
How do you deal with the underlying trauma that some patients are dealing with, where the only comfort they feel they have at their disposal is food? These are very complex questions. We have patients who come into our offices knowing they want to be able to eat less, but they can't stop. It’s not at all uncommon for people to overeat; all of us have done it at one point or another.
If I had a blank check, I would want to look at the key tools that, when combined, provide a synergistic outcome for long-term success. In my mind, that is not a single tool. It is not a magic pill or injection.
Daniel Bessesen
If I had an unlimited budget to fund one study to help mitigate the various challenges of obesity, it would be a well-designed prospective cost-benefit analysis of antiobesity medications. To me, the biggest obstacle to the broader use of newer antiobesity medications is insurance coverage and payment. Because obesity is so common and the costs of the newer medications are so high currently, the financial implications of treatment are a tremendous challenge. I think progress will be stalled until there is ample evidence of cost-effectiveness, and right now we simply do not have a good cost-effectiveness database.
If I were to design such a study, we would have a group propose a “best approach for treating obesity” in a population using all the tools we have: lifestyle, older medications, newer medications, and surgery. In this model, the intensity of treatment would be tailored to the level of severity of obesity, with more severely affected individuals receiving more intensive and costly treatment. Such a study would attempt to obtain real cost-effectiveness data on all the meaningful costs and benefits. I think this is important because some of the cost savings will relate to downstream benefits, such as reductions in cancer, sleep apnea, diabetes, and heart disease. Data could be collected on disability, work attendance, and productivity. If you really look at the broad economic benefits as well as the actual costs (which include not only the cost of the drug, but ongoing monitoring, side effects, adverse events, and so forth), if we had a robust cost-benefit study with prospectively collected data in a real-world clinical environment, I think that would move the needle.
Jamy Ard
We are at an inflection point in which many of us in clinical practice are excited about the direction we are headed regarding obesity care. Five years ago, conversations like this were not happening, whereas now, everybody is talking about antiobesity medications. Given where we are now, I’d like to ask what you see as the biggest threat to the continued acceptance of obesity treatment. Is there anything in the back of your mind that makes you feel a little bit cautious here?
Lydia Alexander
I agree with Dr Bessesen. The cost of the medication is a valid concern. Affordability, accessibility, and equity all pose their own unique challenges. I am fortunate to live and practice in California where MediCal has covered all antiobesity medications since 2022, and there are not plan exclusions, which I think is wonderful because these are many of the patients who have severe obesity, many disease complications, and need antiobesity medications the most.
I have had patients who are placed on antiobesity medications only to later become disqualified for MediCal because their health has improved. Then, when they join another health plan, they can't get these medications covered. I have also grappled with what happens to a patient who is on GLP-1 treatment, retires from their job, and ends up going on Medicare, but who does not have a preexisting cardiovascular disease and may not qualify for GLP-1s through Medicare. So what happens to patients who fall into those types of situations? They’re often left hanging because of the way that our health care system is structured.
Do we want socialized medicine? Not necessarily. I listened to the Senate hearings with Bernie Sanders and the CEO of Novo Nordisk, but at the same time, we need to have some way forward. I worry that there will be plan exclusions with insurance companies not properly providing all FDA-approved medical treatment to the people they insure, trying to pass the buck, which is the cost for comprehensive treatment down the line, and that it’s going to really be hard to do right by our patients in the long term because of payment and reimbursement challenges.
In addition to that, weight bias and the related stigma really continue to be ongoing issues. Weight is being viewed as the patient’s fault for not trying hard enough in the same way we thought about depression 40 to 50 years ago. Back then, the sentiment was that if someone could just smile more or make more of an effort to be upbeat, then depression could be kept at bay. It was only later we realized a chemical dysregulation in the body causes major depressive disorder and that it’s not the same as sadness.
We also know the body has a regulatory system for weight that can malfunction. Metabolic weight dysregulation isn’t the same thing as going away on vacation and coming home 2 or 3 pounds heavier for a week before returning to baseline. When our weight regulatory system isn’t broken, the body can manage a transient environmental stimulus increase, eventually returning to a weight setpoint. When the system is broken, that is not the case. It is a metabolic malfunction. Now we have the disease state. There is obesity, adiposity, and it is a medical issue, not simply a personal choice to be one way vs another.
I see stigma and bias even in the discussions and concern for the safety of GLP-1 medications. GLP-1s have a relatively good safety profile compared with many other medications we prescribe. GLP-1s have been on the market since 2005. The black box warning for GLP-1s, multiple endocrine neoplasia, type 2 (MEN2) and medullary thyroid carcinoma, are extremely rare conditions. Yet overall, there is a lot of worry about the safety profile for GLP-1s. This is in contrast to selective serotonin reuptake inhibitors, which have a black box warning for suicidality.
Jamy Ard
Dr Hashmi, do you anticipate any threats to continued acceptance of obesity treatments?
Sean Hasan Hashmi
I think one way or another, obesity treatments are going to be accepted. What we have learned from the days of fen-phen, lorcaserin, and rimonabant, which never got the FDA nod but was approved in Europe, is that even if we look at data for certain measures at 4 to 5 years after the release of a drug, it doesn’t mean that future data won’t supplant current knowledge. Longer-term data is needed to know more about the full safety profile. This was the case with the previous drugs (fen-phen, lorcaserin, rimonabant), which were considered safe early on but after several years, they showed dangerous side effects, requiring their withdrawal from the market.
We, as practitioners, have an obligation to our patients to ensure the highest-possible level of safety with the treatments we provide. This is why our approach always has been to start with agents that have the best long-term safety data and then move to other agents, if necessary.
Our process involves following patients on their journeys and using a multimodal approach, including with the prescribing physician, behavioral therapist, dietitians, or any other clinician involved in a patient’s care.
We know that, looking into the future, there will be far greater treatments available for obesity. The challenge that we have at present is to ensure we are following evidence-based or evidence-informed practice so that we're maintaining a balancing approach without getting distracted by the hype. We still need to weigh the benefits against the cost and side effects for every patient. Always remaining evidence-based, quality-driven, and fiscally accountable are the 3 sides of the triangle, a 3-legged stool that would be impossible to sustain if one of its legs were missing.
We can't forget quality, we can't forget evidence, and we can't forget cost. All 3 must be part of the equation.
Jamy Ard
Cost is certainly one of the biggest threats to being able to sustain current momentum in treating obesity and related diseases.
There is some sentiment that if the price of medications in this class doesn’t come down, more competition can be anticipated, which in turn will reduce the price point. However, I've also heard some people who feel that some other classes of medications haven't provided the same level of cost reduction when newer options have entered the market.
Now that we have talked about cost and cost-effectiveness, are there any other threats you envision to continued support of these types of antiobesity medications? What else concerns you about our ability to continue seeing the widescale acceptance of obesity treatment?
Daniel Bessesen
I do think cost is a major issue because unlike other diseases that involve high-cost drugs for treatment, obesity affects 35% of adults in the United States.8 When multiplying the cost of these drugs by the population taking them, the numbers just become astronomical.
Additionally, we have a history of antiobesity medications that have been pulled off the market here in the United States because of adverse events and side effects. I feel that drugs in this class are held to a different standard.
Another threat to the wider dissemination of antiobesity medications is the possibility that, despite the extensive studies that have been done, an unexpected side effect could appear. The emergence of a previously unexpected and unknown, even rare, side effect could be blown out of proportion, especially by people who continue to see obesity as a personal failing rather than a medical condition, leading people to believe that this risk negates any of the benefits of these drugs. Similar situations have happened with antiobesity medications in the past.
Karlijn Burridge
I agree with what everybody has said so far. One of my concerns is that we now have these powerful tools that require regular follow-up. Patients using these drugs require ongoing counseling. With other medications, we may not need to follow up with the patient until 6 months later or longer.
However, with these antiobesity medications, patients require a gradual escalation of the dose, so they need to be followed-up more frequently. We need to be managing side effects appropriately and counsel our patients through this. We need to assess tolerability and the rate of weight reduction while also ensuring that they are consuming sufficient nutrients to sustain healthy weight loss. All these things need to be monitored much more closely with the disease of obesity. A multimodal, multipronged approach, including nutrition, physical activity, and other lifestyle components, must be used.
I am concerned that many patients are now even able to access these medications through online services, even if they are not following up with a clinician. I worry because we really do need to have a comprehensive approach with these medications.
Another thing I am concerned about is that it seems like in the past few years there has been an increased focus on cosmetic weight loss. Because of the widespread attention given to these medications on social media, the emphasis hasn’t been on how these are powerful medications used to treat the disease of obesity, which needs to be the message. These drugs are not just casual weight loss supplements, which is sometimes what our patients hear throughout social media. We need to be careful that we stay away from advancing any messaging around how these drugs are cosmetic in nature when they are intended to treat a serious chronic disease.
Jamy Ard
I’d like to discuss combination therapy involving antiobesity medications and bariatric metabolic surgery. We have new, more effective medications now, with more undergoing clinical trials. As a result, some of the patients who would have theoretically gone to surgery now perhaps will not. This creates some opportunities and new ways to think about treating patients with the highest BMIs and the most severe diseases, potentially. Also, this calls into consideration those patients who, despite undergoing surgery, experience weight regain. So how are you all thinking about combination therapy? Are you using combination therapy strategies in your practice?
Lydia Alexander
In June of 2024, I gave a talk entitled “A Rising Tide Lifts All Boats” at the American Society for Metabolic and Bariatric Surgery conference.9 There can be win-win opportunities for patients, payers, and clinicians alike when we employ a multimodal treatment approach.
We know that compared with the level of severe obesity that exists, there are relatively few metabolic bariatric surgerical procedures performed in the United States. There will always be people who will not be candidates for the medications in our obesity treatment toolbox or best suited for metabolic bariatric surgery. We cannot and should not attempt to implement a one-size-fits-all approach to weight management. It is important to collaborate across the field for this reason.
Preoperative and postoperative bariatric surgery care is also important. As Dr Hashmi mentioned, it is possible, for instance, that a patient may require additional comprehensive obesity management, including reinstitution of behavioral modification 10 years after surgery. Every patient should receive long-term follow-up and evaluation after metabolic bariatric surgery to determine whether an additional adjunctive therapy, such as third-generation antiobesity treatments, may be warranted. This is the longitudinal and multidisciplinary way in which we manage cancer. We don’t often think about choosing one type of treatment, chemotherapy, radiation, or surgery alone, for many kinds of cancer but often use combined treatments for best outcomes.
We, as health care practitioners, should be clear regarding what direction we are heading in terms of providing care using these medications. All of our efforts should be considered under one umbrella in terms of what tools at our disposal we decide to reach for.
Sean Hasan Hashmi
Innovation is not a bad thing. Innovation drives further innovation. When I give talks to the bariatric surgeons across the country, I hear a lot of the discourse around GLP-1s focusing on how they are brand-new in the field and serve as a potential threat. However, there are also many new innovations, such as the emerging field of endobariatrics.
Five years ago, nobody knew what endobariatrics was. But now, there are actually many new procedures filling the gap between sleeve gastrectomy and gastric bypass, such as endobariatric procedures. Our colleagues in gastroenterology are offering endobariatrics procedures that offer a much safer approach for patients who have failed sleeve gastrectomy and are not candidates to go into Roux-en-Y gastric bypass. In other words, this brand-new field is exploding with innovation. To Dr Alexander’s point earlier, this is indeed the rising tide and it will absolutely lift all boats. We will be able to have a dialogue on nutrition. Who prescribes nutrition? How can we stop fighting about all the individual diets and start to come to the common principles in all of them? The same is true for exercise training. We all like to think we're experts in everything so we create these elaborate schemes, and yet the principles of exercise training are so basic and simple.
I started out as a trainer and a Taekwondo instructor, so I've been around the field for a long time, and I can tell you everyone thinks they are an expert. And yet, nobody does the research needed. We now have an opportunity to finally see the light in this field of obesity that no one knew about. So why not jump into the research here? Why not take the opportunity to start to lift the entire field and start to educate people on the entire thing? And while we're at it, why don't we start with the schools first? If we could educate the trainees and learners early on, that would make such a tremendous difference; maybe not in our lifetimes, but for the next generation of leaders coming up.
Jamy Ard
Ms Burridge, what are you seeing in your practice and the applications for that type of thinking?
Karlijn Burridge
I have spent most of my career working in and alongside metabolic and bariatric surgery, so I've been using this combination therapy of surgery and medications for over 10 years. Combination therapy is beneficial and needed. Dr Alexander’s example of cancer treatment is perfect. If you were a surgeon in oncology, you would not bemoan the fact that there are new chemotherapies or adjunctive therapies available. Those of us practicing in obesity care need to adopt a similar acceptance of an expansion of our available set of tools.
I think having such a mindset allows us to individualize care for patients based on their own unique needs. Also, we know there is a huge variance in how individual patients respond to different treatments. We know there is a percentage of patients who won't respond to medications or to these newer GLP-1s. When we look at how undertreated obesity currently is, we know only 1% of individuals who qualify for metabolic and bariatric surgery are having these surgerical procedures.
Also, a very small percentage, maybe 2% or 3%, of individuals with obesity are being treated with medical therapy.
There is such an opportunity here to increase the treatment for patients living with obesity. It is great to have multiple tools at our disposal and to be able to find the right tool for the right patient, just like so many other specialties can do. For some patients, combination therapy may be best; for others, endoscopic procedures or medications alone may be best. It’s about finding the right fit for each patient at the right time.
We know that obesity is a progressive disease and we know that we do not have a cure. Surgery is not a cure, and we know hormone levels are altered over time after surgery. We need tools for different patients in different parts of their journey. I see these new antiobesity drugs as a wonderful opportunity to be able to combine these tools to provide optimal patient care.
Daniel Bessesen
I think combination therapy is best used now by patients with insufficient weight loss with surgery or weight regain after surgery. To Dr Alexander’s point about neoadjuvant therapy and adjuvant therapy, we need studies in this area. In the analogy of treating a patient with cancer, does the clinician perform chemotherapy first and then do surgery later? How do you sequence the treatment plan? Is the surgical route explored before the medication route? Do you use medications, then stop the medication, and then do surgery? We need good data to help answer some of these questions.
Jamy Ard
I would like to thank you all for participating in this expert panel discussion. You all have been gracious in providing such wonderful and thoughtful responses. Thank you.
Disclaimer.
The thoughts, ideas, and positions expressed by the panelists in this discussion are their own, do not necessarily reflect the positions of their respective organizations or employers, and do not reflect the position of The Permanente Journal or The Permanente Federation LLC.
Footnotes
Conflicts of Interest: None declared
Funding: None declared
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief, No. 360. National Center for Health Statistics; 2020. [PubMed] [Google Scholar]
- 2.Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389(24):2221–2232. 10.1056/NEJMoa2307563 [DOI] [PubMed] [Google Scholar]
- 3.Melson E, Ashraf U, Papamargaritis D, Davies MJ. What is the pipeline for future medications for obesity? Int J Obes. 10.1038/s41366-024-01473-y [DOI] [PubMed] [Google Scholar]
- 4.Jastreboff AM, Kaplan LM, Frías JP, et al. Triple–hormone-receptor agonist retatrutide for obesity — A phase 2 trial. N Engl J Med. 2023;389(6):514–526. 10.1056/NEJMoa2301972 [DOI] [PubMed] [Google Scholar]
- 5.Kokkorakis M, Chakhtoura M, Rhayem C, et al. Emerging pharmacotherapies for obesity: A systematic review. Pharmacol Rev. 2024:PHARMREV-AR-2023-001045. 10.1124/pharmrev.123.001045 [DOI] [PubMed] [Google Scholar]
- 6.US Food & Drug . Drug Approval Package. April 28, 2005. Accessed 12 November 2024. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/021773_byettatoc.cfm#:~:text=Approval%20Date%3A%204%2F28%2F2005
- 7. The National Weight Control Registry. Accessed 8 October 2024. http://www.nwcr.ws/
- 8.New CDC data show adult obesity prevalence remains high. CDC Newsroom. September 12, 2024. Accessed 23 October 2024. https://www.cdc.gov/media/releases/2024/p0912-adult-obesity.html
- 9.ASMBS/OMA collaborative session the obesity epidemic: A rising tide lifts all boats. Presented at: ASMBS Annual Meeting 2024; June 11, 2024; San Diego, CA. Accessed 25 November 2024. https://2024.asmbsmeeting.com/session/oma/ [Google Scholar]