Abstract
Purpose
Asthma and depression are prevalent conditions with significant comorbidity, impacting patients’ quality of life. This bibliometric study aims to analyze research trends and hotspots in the field from 2000 to 2023, identifying key contributions and predicting future directions.
Methods
We conducted a systematic search in the Web of Science Core Collection (WoSCC) for articles on asthma and depression, published between 2000 and 2023. Bibliometrics, which involves the application of mathematical and statistical methods to analyze scholarly literature, was employed in this study to systematically assess the research trends and hotspots in the field of asthma and depression. VOSviewer and CiteSpace software were utilized for visual analysis and data visualization, enabling us to map collaboration networks and identify research hotspots and trends within the asthma and depression literature.
Results
Our analysis retrieved 3067 papers from 937 journals, involving 14,631 authors and 4006 institutions across 106 countries. The United States, Columbia University, the Journal of Asthma, and Christer Janson were the most prolific contributors. Six primary research themes emerged: quality of life, childhood asthma, primary care, substance P, intervention, and emotion. Additionally, Burst detection analysis identified emerging topics, including severe asthma, other respiratory diseases, and oxidative stress.
Conclusion
This bibliometric analysis has revealed significant insights into the research trends and hotspots in the field of asthma and depression. The primary findings indicate a growing body of research highlighting the impact of depression on asthma control and patients’ quality of life, the need for psychological interventions in treating comorbid asthma and depression, and the emerging focus on severe asthma and oxidative stress mechanisms. These findings underscore the importance of continued research in these areas to advance our understanding and improve clinical outcomes for patients with these comorbid conditions.
Keywords: asthma, depression, bibliometric analysis, hotspots, research trends
Introduction
Asthma, a prevalent chronic respiratory condition, poses a significant threat to human health, affecting an estimated 300 million individuals globally.1 In 2019, approximately 461,000 deaths were attributed to asthma.2 In 2022, the United States reported asthma prevalence rates of 8.7% among adults and 6.2% among children, with 39.6% of adults and 38.7% of children experiencing acute asthma attacks within the preceding year.3 Furthermore, asthma patients frequently exhibit comorbidities, including rhinitis, gastroesophageal reflux disease, obesity, and depression.4 Given its chronic and episodic nature, asthma significantly affects patients’ emotional well-being. Research indicates that asthma patients exhibit a higher likelihood of depression compared to healthy individuals.5 Moreover, studies link corticosteroid use in asthma treatment to an elevated risk of depression.6
Depression, a prevalent mental disorder, affects over 300 million individuals globally.7 A retrospective analysis of adults aged 18–74 across 28 countries revealed an average lifetime prevalence rate of 10.6% for depression.8 Depression frequently co-occurs with asthma in patients, with a wide range of estimated prevalence, from 2.24% to 24.9% among asthma patients.9 This variation in prevalence estimates may stem from inconsistencies in diagnostic tools across studies, and the varying severity of disease and cultural contexts of the participants. In Canada, depression is the most prevalent chronic comorbidity associated with asthma.10 A national health survey in Israel reported that 37.4% of asthmatic individuals had depression, contrasting with 21.8% of non-asthmatic individuals.11 Adolescents with asthma exhibit a 2.09-fold higher risk of developing depression compared to the healthy control group.12 Respiratory symptoms in asthma patients are significantly associated with depressive states.13 Depression frequently results in suboptimal asthma management and diminished Asthma Control Test scores, as well as elevated hospitalization and emergency department visitation rates attributable to inadequate asthma control, which significantly degrades the quality of life for asthma patients.14–16 Relative to healthy controls, patients with depression exhibit a significantly elevated risk of asthma development, with asthma prevalence in this population ranging from 7.6% to 20.2%.9 Individuals with severe depression are at a 1.91-fold higher risk for asthma development compared to those without depression.17
The academic community is increasingly focusing on the comorbidity of asthma and depression, despite numerous studies, many questions persist. A complex interrelationship is suggested between asthma and depression, although the precise nature of this connection remains undefined. The elevated comorbidity rate of asthma and depression implies the presence of shared pathological mechanisms, the specifics of which remain elusive. Moreover, there is currently a lack of sufficient high-quality evidence to support treatment plans for asthma combined with depression. Bibliometrics utilizes mathematical and statistical methods to quantitatively and qualitatively analyze various characteristics of literature, aiming to objectively assess the impact and value of research findings, thereby helping researchers quickly understand the evolution of knowledge, research hotspots, and future development trends in specific fields.18,19 VOSviewer and CiteSpace are two widely used tools in bibliometric analysis.20,21 VOSviewer can display a visual collaboration network based on elements such as countries/regions, institutions, and authors.21,22 CiteSpace, developed by Chaomei Chen, is a Java-based application facilitating data analysis and visualization. CiteSpace analyzes time slices through timeline analysis and identifies burst keywords through burst detection, helping researchers identify trends in the field.23,24 Although there are bibliometric analyses on depression25–28and on asthma,29–32 there are few bibliometric studies reported in the field of asthma combined with depression. Over the past two decades, an extensive body of literature has emerged on the comorbidity of asthma and depression, complicating manual information extraction. Thus, a systematic bibliometric synthesis of research findings in this domain is particularly warranted. This study collected a total of 3067 documents on asthma and depression published from January 1, 2000, to December 31, 2023, and used CiteSpace 6.3.R1 and VOSviewer 1.6.19 for bibliometric analysis to explore the research hotspots and emerging research frontiers of asthma and depression.
Materials and Methods
Data Retrieval and Collection
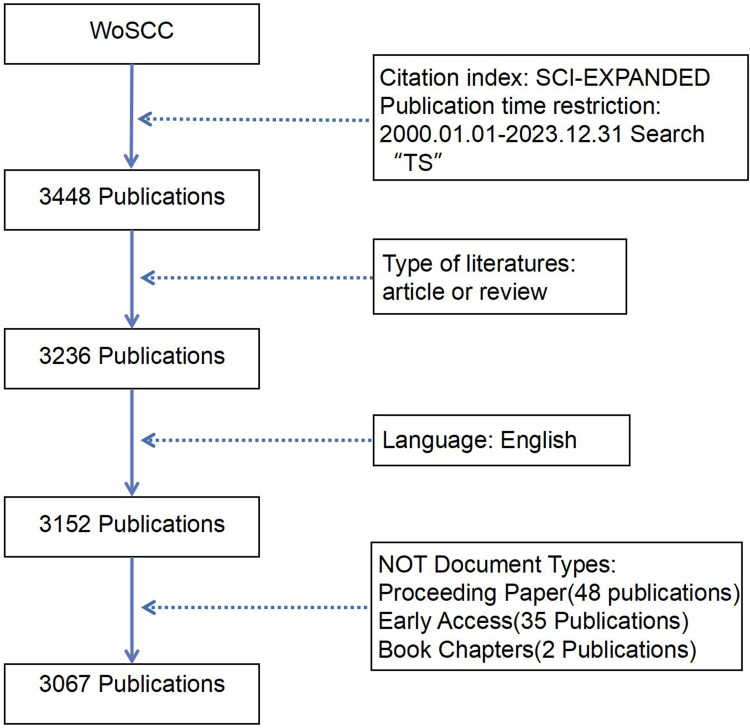
This study utilizes the Web of Science Core Collection (WoSCC) as the primary data source. The WoSCC was selected as the primary data source due to its comprehensive coverage and the compatibility of its data structure with the bibliometric analysis tools VOSviewer and CiteSpace, which are essential for conducting a systematic and visually informative analysis. The retrieval strategy for this study is ”TS=((asthma OR asthmas OR asthmatic OR ”bronchial asthma” OR ”bronchial asthmas”) AND (depression OR depressions OR melancholia OR melancholias OR ”depressive symptom” OR ”depressive symptoms” OR ”depressive syndrome” OR ”depressive syndromes” OR ”depressive disorder” OR ”depressive disorders”). The search was restricted to the Science Citation Index Expanded (SCI-EXPANDED). Papers published between January 1, 2000, and December 31, 2023, were included, focusing on articles categorized as original research or reviews, and limited to English-language publications, excluding conference papers, early online publications, and book chapters. A total of 3067 papers were identified and exported in plain text format, which included full records and cited references. The process of literature identification is depicted in Figure 1. Data extraction was completed within a single day, on January 7, 2024, to mitigate potential bias from subsequent database updates.
Figure 1.
Literature identification flowchart.
Data Analysis and Visualization Methods
CiteSpace 6.3.R1 and VOSviewer 1.6.19 were selected as the bibliometric analysis tools for a comprehensive bibliometric analysis of the literature on asthma and depression ranging from January 1, 2000, to December 31, 2023, to thoroughly assess research progress and academic contributions. To comprehensively gauge the contributions of various countries/regions, research institutions, and authors, we utilized VOSviewer 1.6.19 to generate a co-occurrence map depicting collaboration networks. To delineate the trajectory of research hotspots and forecast trends, we applied CiteSpace 6.3.R1 for keyword clustering and burst detection. The keyword clustering analysis was not merely a direct output from the software but rather a result of a systematic approach. CiteSpace was utilized to perform co-citation analysis on the identified keywords, which involved setting specific parameters such as time slices and term frequency to identify clusters. This methodological approach allowed us to categorize keywords into meaningful groups, revealing the thematic structure of the research field over the past two decades. The clusters were then interpreted based on the contextual knowledge of the field, ensuring that the analysis reflects a nuanced understanding of the research trends and hotspots. The journal impact factor was retrieved from the 2022 Journal Citation Reports.
Results
Analysis of Publications and Trends
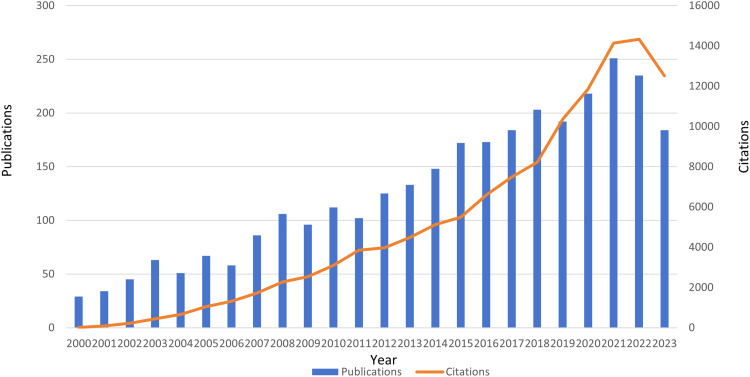
The trends and pace of the field can be determined by the number of publications published each year and their citation frequency. From January 1, 2000, to December 31, 2023, a total of 3067 publications related to asthma and depression were retrieved, with a total citation frequency of 121,880 times, an average of 39.74 citations per article, and an H-index of 147. Among the 3067 papers, 2661 were original research articles and 406 were review articles. As shown in Figure 2, over the past 20 years, there has been a significant upward trend in both the number of publications and their citation frequency in this field. Since 2010, the annual number of publications has been more than 100 for 14 consecutive years, peaking in 2021 with 251 articles. The increase in this data not only reflects the continued interest of the academic community in the research field of asthma and depression but also shows that this research field is increasingly receiving widespread attention and importance.
Figure 2.
The trend of growth in the number of global publications and their citation frequency from 2000 to 2023.
Collaboration Network
Country/Region Collaboration Network
We identified influential countries/regions in this field by analyzing publication output and mapped the resultant collaboration network. Between January 1, 2000, and December 31, 2023, 106 countries/regions contributed to the publication of papers on asthma and depression. Quantitative analysis of published academic papers revealed the top ten contributing countries/regions, as detailed in Table 1. The United States, being the most prolific and influential, contributed 1292 papers, amassing 64,021 citations with an average of 49.55 citations per paper. This underscores the United States’ preeminent position in the field and indicates the global recognition of its research contributions. The disparity in academic output between the United States and other countries/regions is substantial, affirming its dominant standing in the field.
Table 1.
The Top 10 Countries/Regions with the Highest Number of Published Papers
| Country/Region | Documents | Total citations | Average citations | Total link strength |
|---|---|---|---|---|
| USA | 1292 | 64,021 | 49.55 | 626 |
| England | 372 | 20,069 | 53.95 | 616 |
| Australia | 239 | 9507 | 39.78 | 264 |
| Canada | 196 | 8045 | 41.05 | 175 |
| China | 182 | 3781 | 20.77 | 157 |
| Germany | 158 | 7234 | 45.78 | 293 |
| Italy | 126 | 6007 | 47.67 | 353 |
| Spain | 124 | 5300 | 42.74 | 354 |
| Netherlands | 117 | 6620 | 56.58 | 312 |
| Sweden | 114 | 4558 | 39.98 | 183 |
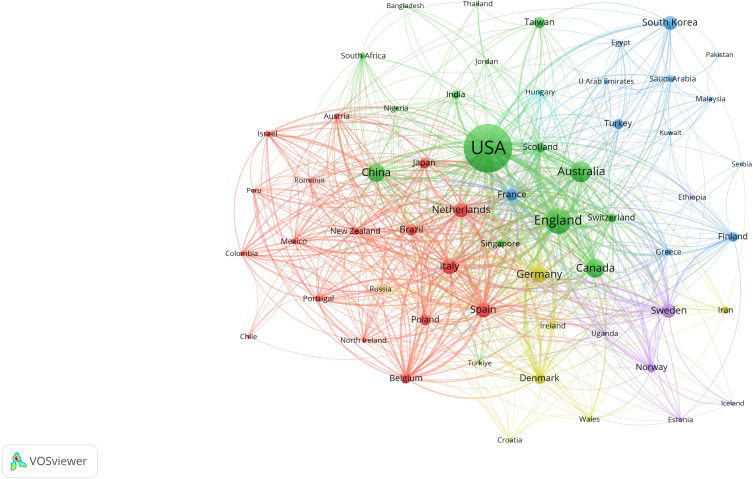
International collaboration is essential for advancing this field. The co-occurrence map, generated VOSviewer software, illustrates significant contributions from countries including the United States, England, Spain, Italy, the Netherlands, Germany, and Australia (Figure 3). The map’s nodes, representing individual countries, are sized relative to each country’s publication output. Lines connecting nodes denote collaborative ties, with line number and thickness indicating the intensity of academic cooperation. The intensity of cooperation is quantified by the metric of total link strength. With a total link strength of 626, the United States is positioned as a central actor in the field, exerting substantial academic influence. England and Australia exhibit the closest cooperation with the United States. Chinese scholars have contributed 182 papers to this field, accumulating 3781 citations, averaging 20.77 citations per paper. China’s academic cooperation exhibits a total link strength of 157 with other countries/regions. Despite a considerable publication output, China’s citation metrics and international collaboration strength suggest opportunities for enhancement. This suggests a need to augment the citation impact of Chinese publications and to broaden international collaborative efforts.
Figure 3.
Collaborative research in the field of asthma and depression among various countries/regions.
Institution Collaboration Network
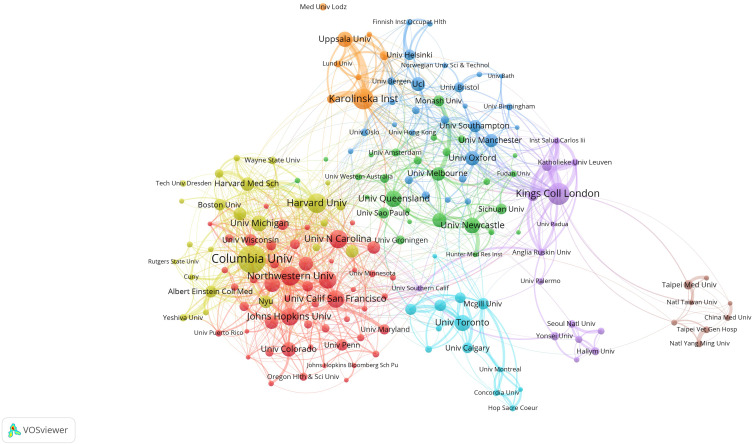
Between January 1, 2000, and December 31, 2023, a total of 4006 global institutions contributed to papers on asthma and depression. Table 2 lists the top 10 institutions by publication volume, with seven being United States-based. Columbia University leads with 80 published academic papers. Harvard University, with 52 published papers and 4258 total citations, is the most frequently cited institution overall. The University of Washington has the highest average citations per paper at 83.49, based on 45 publications. Figure 4 depicts the collaboration network of institutions with more than five publications. Each node represents a research institution, with the node size corresponding to the institution’s publication count, and lines between nodes illustrate collaborative ties. The line number and thickness denote the collaboration intensity, assessable through total link strength. King’s College London, with 60 papers, exhibits a total link strength of 226 with other institutions, marking it as the most collaboratively engaged institution.
Table 2.
The Top 10 Institutions with the Most Published Papers
| Institution | Country/Region | Documents | Total citations | Average citations |
Total link strength |
|---|---|---|---|---|---|
| Columbia University | USA | 80 | 3128 | 39.10 | 194 |
| King’s College London | England | 60 | 1521 | 25.35 | 226 |
| Karolinska Institutet | Sweden | 56 | 1579 | 28.20 | 171 |
| Harvard University | USA | 52 | 4258 | 81.88 | 113 |
| Northwestern University | USA | 51 | 3428 | 67.22 | 141 |
| University of North Carolina | USA | 48 | 3745 | 78.02 | 103 |
| Johns Hopkins University | USA | 46 | 1634 | 35.52 | 117 |
| University of California, San Francisco | USA | 45 | 2194 | 48.76 | 136 |
| University of Washington | USA | 45 | 3757 | 83.49 | 81 |
| University of Queensland | Australia | 43 | 1650 | 38.37 | 63 |
Figure 4.
According to the VOSviewer, the institutional collaboration network for papers on asthma and depression with more than five publications.
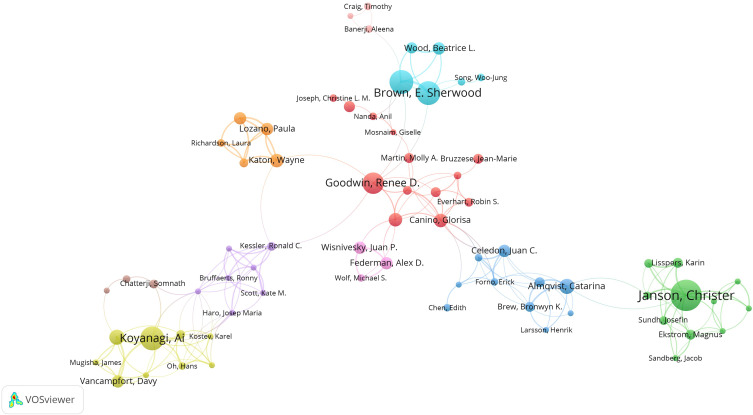
Author Collaboration Network
Between January 1, 2000, and December 31, 2023, it is estimated that 14,631 authors contributed to the publication of papers on asthma and depression. It is important to note that this figure is subject to some uncertainty due to the limitations of the CiteSpace software in distinguishing between authors with the same name or different name representations. Analysis of the top 10 most prolific authors (Table 3) revealed that four scholars are from the United States, further underscoring the significant contributions of American scholars in this field. Christer Janson of Uppsala University, Sweden, published 25 papers and exhibits a total link strength of 155 with other authors, which positions him as the most published scholar and a prominent collaborator. Janson’s research is concentrated on examining the impact of depression on the quality of life of asthma patients, advocating for incorporating standard assessment tools such as the Asthma Control Test and the Hospital Anxiety and Depression Scale in clinical practice to comprehensively evaluate asthma patients’ quality of life.13,33 Ai Koyanagi of the University of Barcelona, Spain, published 19 papers, amassing 959 total citations with an average of 50.47 citations per paper, which makes him the scholar with the highest citation metrics. Koyanagi primarily investigates the relationship between asthma and mental health through epidemiological surveys, demonstrating that there is a high correlation between self-reported asthma diagnosis and the likelihood of reporting emotional disorders.34 Furthermore, among elderly individuals with depression, asthma is significantly correlated with reduced physical activity, underscoring the necessity of considering the comorbidity’s impact on physical activity and overall health in clinical settings.35 Figure 5 illustrates the collaborative network among authors with more than five publications in the asthma and depression field. E Sherwood Brown and David A Khan, both affiliated with the University of Texas, exhibit a robust cooperative relationship in this domain.
Table 3.
The Top 10 Authors with the Most Published Papers
| Author | Country/ Region |
Institution | Documents | Total citations | Average citations |
Total link strength |
|---|---|---|---|---|---|---|
| Christer Janson | Sweden | Uppsala University | 25 | 623 | 24.92 | 155 |
| E Sherwood Brown | USA | University of Texas | 19 | 415 | 21.84 | 106 |
| David A Khan | USA | University of Texas | 19 | 390 | 20.53 | 121 |
| Ai Koyanagi | Spain | University of Barcelona | 19 | 959 | 50.47 | 117 |
| Renee D Goodwin | USA | Columbia University | 17 | 816 | 48.00 | 63 |
| Kim L Lavoie | Canada | University of Montreal | 16 | 433 | 27.06 | 74 |
| Peter G Gibson | Australia | University of Newcastle | 14 | 200 | 14.29 | 100 |
| Thomas Ritz | USA | Southern Methodist University | 14 | 352 | 25.14 | 51 |
| Catarina Almqvist | Sweden | Karolinska Institutet | 12 | 145 | 12.08 | 78 |
| Simon L Bacon | Canada | University of Montreal | 12 | 329 | 27.42 | 62 |
Figure 5.
Authors who have published more than five papers on asthma and depression according to the VOSviewer co-authorship graph.
Journal Analysis
Between January 1, 2000, and December 31, 2023, a total of 3067 publications concerning asthma and depression were published across 937 academic journals. Table 4 enumerates the top 10 journals by publication count. As classified by the Journal Citation Reports (JCR), the majority of these top 10 journals fall within Q2 (60%) and Q1 (30%) quartiles. The JOURNAL OF ASTHMA, with a 2022 impact factor of 1.9, leads in publication count in this field, totaling 154 articles. It is succeeded by ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY, with a 2022 impact factor of 5.9, which published 84 articles, and the JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY-IN PRACTICE, with a 2022 impact factor of 9.4, publishing 78 articles. CHEST, with the highest impact factor of 9.6 in 2022 among the top 10, is recognized for its significant contribution to the field.
Table 4.
The Top 10 Journals with the Highest Number of Papers Published in the Field of Asthma and Depression
| Journal | Publication Count |
H-Index | 2022 JIF | JIF Quartile |
|---|---|---|---|---|
| JOURNAL OF ASTHMA | 154 | 64 | 1.9 | Q4 |
| ANNALS OF ALLERGY ASTHMA & IMMUNOLOGY | 84 | 100 | 5.9 | Q2 |
| JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY-IN PRACTICE | 78 | 40 | 9.4 | Q1 |
| PLOS ONE | 70 | 268 | 3.7 | Q2 |
| RESPIRATORY MEDICINE | 66 | 108 | 4.3 | Q2 |
| BMJ OPEN | 41 | 69 | 2.9 | Q2 |
| JOURNAL OF PSYCHOSOMATIC RESEARCH | 39 | 141 | 4.7 | Q2 |
| PSYCHOSOMATIC MEDICINE | 36 | 171 | 3.3 | Q2 |
| JOURNAL OF AFFECTIVE DISORDERS | 30 | 165 | 6.6 | Q1 |
| CHEST | 29 | 267 | 9.6 | Q1 |
Keyword Analysis
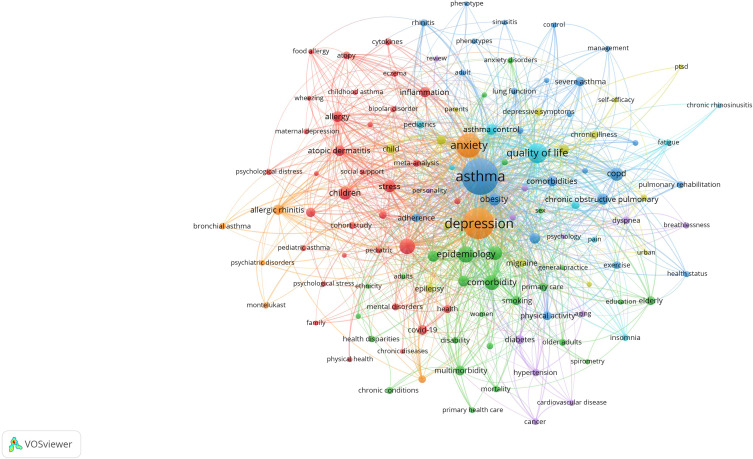
Most Common Keywords
Extracted from academic papers, keywords reveal the primary focus and developmental trends within a specific research domain. A total of 4931 keywords were identified from 3067 documents concerning asthma and depression. The keyword co-occurrence network map for this field, constructed using VOSviewer software, displays keywords appearing more than 10 times, with node size indicative of keyword frequency (Figure 6).
Figure 6.
According to VOSviewer, a co-occurrence analysis map of keywords that appear at least 10 times.
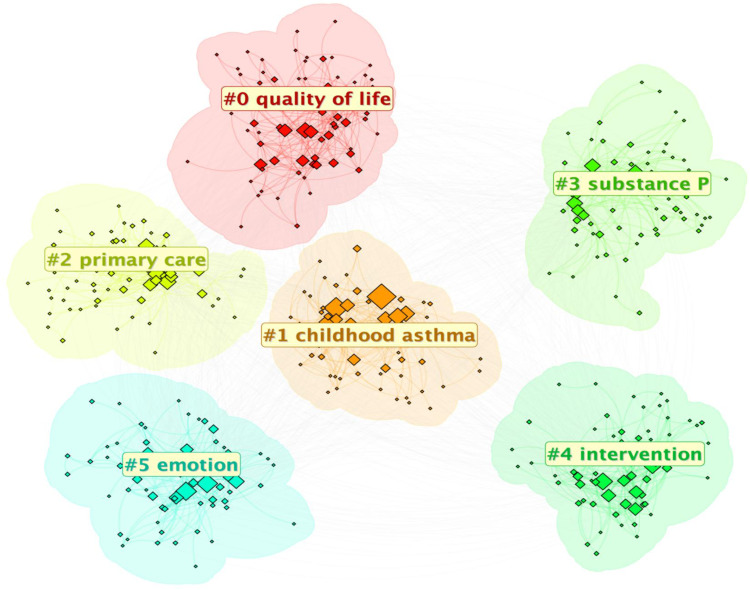
The most frequent top 10 keywords are asthma, depression, anxiety, quality of life, epidemiology, mental health, comorbidity, chronic disease, chronic obstructive pulmonary disease (COPD), and children (Table 5). For an in-depth examination of research themes in this field over the past two decades, cluster analysis was conducted on the keywords using CiteSpace software. The analysis categorized keywords into six principal clusters (Figure 7): quality of life, childhood asthma, primary care, substance P, intervention, and emotion. The numbers preceding the tags represent the number of keywords within each cluster, listed in ascending order, with cluster #0 containing the most keywords.
Table 5.
The Top 10 Keywords with the Highest Frequency of Occurrence
| Keyword | Count | Total link strength |
|---|---|---|
| Asthma | 703 | 1803 |
| Depression | 507 | 1510 |
| Anxiety | 286 | 931 |
| Quality of life | 189 | 501 |
| Epidemiology | 126 | 332 |
| Mental health | 110 | 299 |
| Comorbidity | 104 | 320 |
| Chronic disease | 83 | 209 |
| Chronic obstructive pulmonary disease | 79 | 217 |
| Children | 73 | 185 |
Figure 7.
According to the keyword clustering map from CiteSpace.
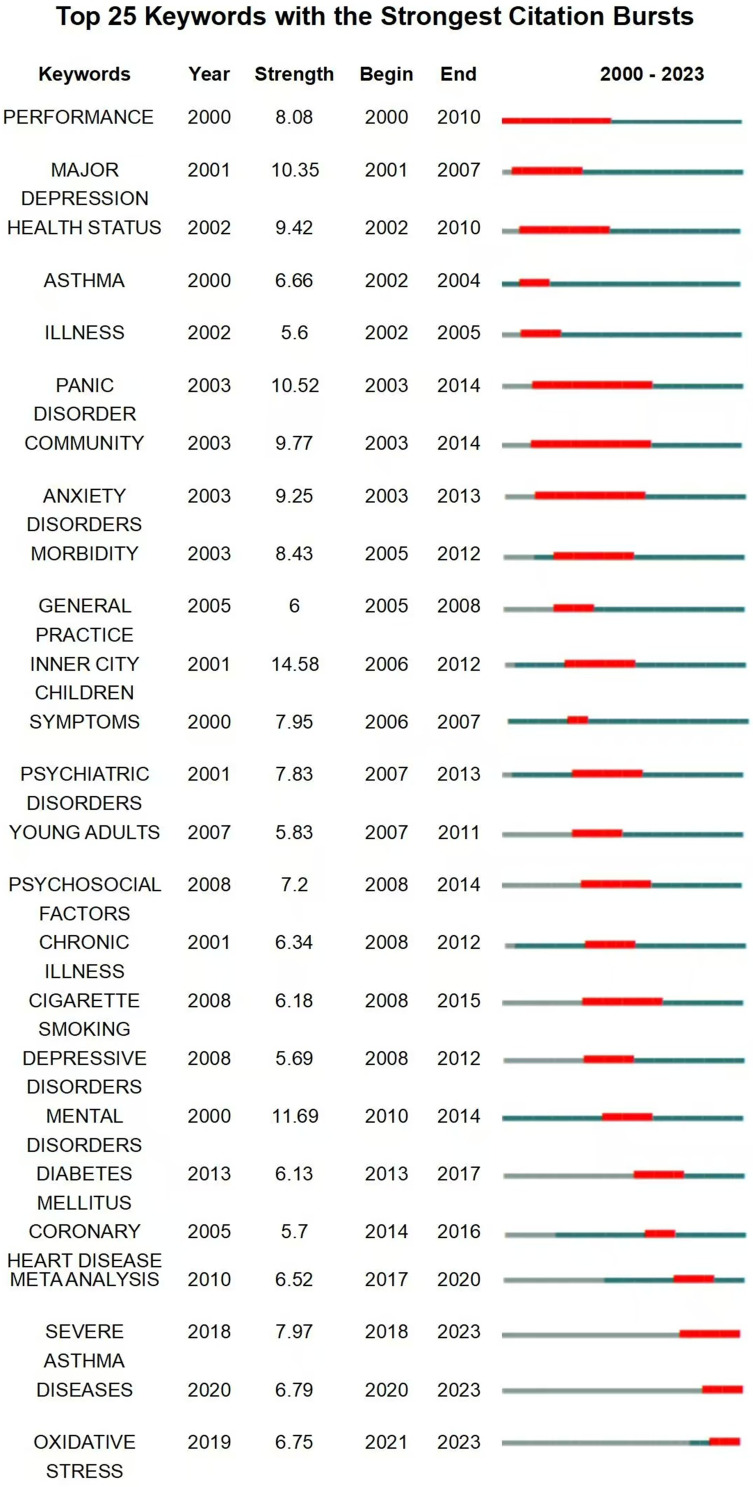
Burst Keywords
Burst keywords are terms that frequently emerge and garner substantial interest from scholars within a defined period. They often indicate the prevailing focus of research efforts at that time. Figure 8 presents the top 25 keywords exhibiting the most significant citation bursts. Notably, “health status” from 2002 to 2010, “anxiety disorders” from 2003 to 2013, and “morbidity” from 2005 to 2012 have remained prominent topics for several years. More recent terms such as “severe asthma” between 2018 and 2023, “diseases” from 2020 to 2023, and “oxidative stress” from 2021 to 2023 have demonstrated a marked escalation in usage, suggesting their potential to shape forthcoming research in the asthma and depression domain.
Figure 8.
Burstness map of keywords on asthma and depression.
Discussion
This study conducted a bibliometric analysis of literature in the field of the comorbidity of asthma and depression from 2000 to 2023. The results were visualized using the software CiteSpace and VOSviewer, which quantitatively and intuitively displayed the developmental trajectory and research hotspots of the field. Furthermore, we performed a quantitative analysis across countries/regions, authors, and research institutions. The findings reveal that U.S.-based researchers lead in both the number of publications and academic influence, underscoring the significant role of the United States in asthma and depression research.
This study employed keyword clustering analysis to identify research hotspots in the field of asthma and depression comorbidity over the past two decades, focusing on quality of life, childhood asthma, primary care, substance P, intervention, and emotion. We summarize the research hotspots as follows:(1) Impact of depression on asthma control and patients’ quality of life. There is a correlation between depressive symptoms and adverse health outcomes such as increased asthma severity and the risk of hospitalization due to asthma.36 Sandhya Khurana et al37 found that an increase in the severity of depressive symptoms in patients with severe eosinophilic asthma is associated with poorer respiratory quality of life and worsened asthma control. Depression may affect patients’ sensitivity to symptoms, making them more vulnerable when dealing with asthma symptoms, leading to more frequent acute attacks.38 (2) Assessing the impact of depression on the quality of life of children with asthma. Asthma is a chronic inflammatory disease of the airways with a high prevalence in children. Poor asthma control may negatively affect children’s mental state, adding to their mental stress. Depression has also been found to be associated with poor asthma control, and parental depressive symptoms can affect children’s asthma control through family dysfunction.39 Research indicates that alleviating caregiver depression positively impacts the onset and progression of depression in children with asthma.40 Therefore, in addition to optimizing asthma control strategies, addressing depression in children and their caregivers is as important, which helps to improve the quality of life related to childhood asthma.41 (3) Primary care strategies and interventions for asthma and depression comorbidity. Clinically, patients with asthma and comorbid depression often do not receive appropriate treatment.42 The reasons for the lack of proper treatment can be complex, such as patients often lacking understanding or having misconceptions about depression, feeling stigmatized by the diagnosis of depression, worrying about social isolation, and concerns about the side effects of antidepressant treatment; there is also a lack of professional doctors conducting psychological and psychiatric assessments for these patients, resulting in missed diagnoses of depression in asthma patients. Therefore, timely and effective intervention for these patients is necessary. A randomized, double-blind, placebo-controlled trial conducted by E Sherwood Brown et al43 showed that escitalopram improved asthma and depressive symptoms in patients with severe depression comorbid with asthma, with side effects comparable to the placebo group, offering another treatment option for asthma patients with depression. However, a meta-analysis by Liem Tran et al44 which included four studies (n=158), found no evidence that selective serotonin reuptake inhibitors (citalopram or escitalopram) affected the reduction of psychological distress in adult asthma patients. Similarly, in treating psychological distress in asthma patients, the anticonvulsant drug (levetiracetam) was not better than placebo. The reporting rate of adverse events in all studies was low, but the adverse events in the intervention group were slightly higher than in the control group. This indicates that there’s not enough evidence right now to say whether pharmacological treatment is a good idea for asthma patients with psychological distress. Therefore, further confirmatory trials are necessary to provide clearer guidance for clinical practice.45 (4) Clarifying the role of substance P in the pathogenesis of asthma and depression. Substance P is a bioactive peptide, a member of the tachykinin family of neuropeptides, acting as a neurotransmitter and neuromodulator in the central nervous system.46 Substance P plays a role in the pathophysiological mechanisms of both asthma and depression.47 The dysregulation of substance P may be a potential mechanism for the comorbidity of asthma and depression.48 (5) The efficacy of psychological interventions for asthma and depression comorbidity. Research has found that psychological interventions show positive effects in improving depressive symptoms in children and adolescents with asthma, effectively reducing the frequency of medical contacts and the number of asthma attacks.49 However, although psychological interventions show potential in improving symptoms of asthma comorbid with depression, more high-quality randomized controlled trials are still necessary to further verify their long-term effects and optimal implementation strategies.50 (6) The relationship between emotions and asthma management. There is a close association between emotional regulation ability and asthma control. Studies show that patients with emotional instability and poor regulation ability are more likely to experience psychological distress, which in turn affects their self-management behaviors and symptom control of asthma. Psychological flexibility and adaptive emotional regulation strategies can significantly improve the quality of life of asthma patients while reducing psychological distress.51
Based on the burst keywords continuing up to 2023, we predict the following future research frontiers: (1) An exploration of the interrelationship between severe asthma and depression. Depression frequently comorbid with severe asthma is particularly evident in patients with a history of early-onset allergic asthma.52 Evidence from real-world studies on refractory asthma treatments with Omalizumab and Mepolizumab indicates that comorbid depression may diminish the efficacy of these biological agents. Hence, it is advisable to incorporate depression intervention strategies alongside biological agent treatments.53 (2) Investigating the role of oxidative stress in the comorbidity of asthma and depression. Research indicates that the antidepressant Duloxetine HCl modulates oxidative stress-related signaling pathways, thereby potentially improving airway inflammation and oxidative stress responses in asthma patients. This suggests its potential therapeutic efficacy in treating both conditions.54
While the research on asthma and depression has advanced significantly over the past two decades, several challenges remain for future development: Firstly, the underlying mechanisms of the interplay between asthma and depression remain partially understood, necessitating further exploration. The NOD-like receptor family pyrin domain-containing 3 (NLRP3) inflammasome is integral to pulmonary pathological processes, increasing the serum levels of pro-inflammatory cytokines, such as IL-1β, IL-6, and TNF-α, which in turn activate the hypothalamic-pituitary-adrenal axis. This activation leads to elevated glucocorticoid release in asthma patients.55 Long-term exposure to high levels of glucocorticoids may lead to neuronal atrophy, inhibit neurogenesis in the hippocampus and prefrontal cortex, and reduce synaptic plasticity. Additionally, IL-1β overexpression can further decrease brain-derived neurotrophic factor production and neurogenesis in the hippocampus. These factors may collectively contribute to a predisposition for depressive symptoms.56 The association between NLRP3 and pyroptosis implicates pyroptosis in the comorbidity of asthma and depression, indicating a need for further investigation. Secondly, current clinical treatments for comorbid asthma and depression lack effective, widely recognized interventions. Urgently needed is patient-centered, multidisciplinary research to develop more efficacious treatment strategies, addressing the complex needs of patients with asthma and depression, and enhancing their mental health and overall quality of life.
Limitations
The limitations of this study are as follows: Firstly, the bibliometric analysis of this study only retrieved publications from the WoSCC database, potentially excluding other literature of academic significance. Secondly, due to the continuous updating of the database, the obtained data, such as the number of articles and citation frequency, may exhibit a certain degree of timeliness bias; Thirdly, the quality of the articles collected in this study is uneven, which may also affect the study’s reliability; Lastly, this study used CiteSpace software to analyze author collaboration, but because the software cannot distinguish between authors with the same name or different expressions of the same author, the number of authors may not be accurate.
Conclusion
In conclusion, our comprehensive bibliometric analysis has delineated the key research trends and hotspots in the field of asthma and depression over the past two decades. The study’s main findings underscore the profound impact of depression on asthma control and the quality of life of patients, the critical need for effective psychological interventions in managing the comorbidity, and the emerging significance of severe asthma and oxidative stress mechanisms. These insights not only provide a multifaceted knowledge structure map of the field but also highlight promising avenues for future research, potentially leading to improved clinical management and patient outcomes.
Funding Statement
This study was supported by the Hunan Provincial Department of Education Outstanding Youth Project (No. 22B0383), Postgraduate Scientific Research Innovation Project of Hunan Province (No. CX20230819), Postgraduate Innovation Project of Hunan University of Chinese Medicine (No. 2023CX117), Hunan University of Chinese Medicine–Micomme Medical Technology Development Co., Ltd. Joint Fund Project (No. 2022MKZJ08), and Changsha Natural Science Foundation (No. kq2208184).
Abbreviations
WoSCC, Web of Science Core Collection; SCI-EXPANDED, Science Citation Index Expanded; JCR, Journal Citation Reports; COPD, chronic obstructive pulmonary disease; NLRP3, NOD-like receptor family pyrin domain-containing 3.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Disclosure
The authors have no conflicts of interest to declare.
References
- 1.Fergeson JE, Patel SS, Lockey RF. Acute asthma, prognosis, and treatment. J Allergy Clin Immunol. 2017;139(2):438–447. doi: 10.1016/j.jaci.2016.06.054 [DOI] [PubMed] [Google Scholar]
- 2.GBD. Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel KB, Mims JW, Clinger JD. The Burden of Asthma and Allergic Rhinitis: epidemiology and Health Care Costs. Otolaryngol Clin North Am. 2024;57(2):179–189. doi: 10.1016/j.otc.2023.09.007 [DOI] [PubMed] [Google Scholar]
- 4.Kaplan A, Szefler SJ, Halpin DMG. Impact of comorbid conditions on asthmatic adults and children. NPJ Prim Care Respir Med. 2020;30(1):36. doi: 10.1038/s41533-020-00194-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hurtado-Ruzza R, Iglesias ÓÁC, Dacal-Quintas R, et al. Asthma, much more than a respiratory disease: influence of depression and anxiety. Rev Assoc Med Bras. 2021;67(4):571–576. doi: 10.1590/1806-9282.20201066 [DOI] [PubMed] [Google Scholar]
- 6.Opolski M, Wilson I. Asthma and depression: a pragmatic review of the literature and recommendations for future research. Clin Pract Epidemiol Ment Health. 2005;1:18. doi: 10.1186/1745-0179-1-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rost T, Stein J, Löbner M, Kersting A, Luck-Sikorski C, Riedel-Heller SG. User Acceptance of Computerized Cognitive Behavioral Therapy for Depression: systematic Review. J Med Internet Res. 2017;19(9):e309. doi: 10.2196/jmir.7662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herrman H, Patel V, Kieling C, et al. Time for united action on depression: a Lancet-World Psychiatric Association Commission. Lancet. 2022;399(10328):957–1022. doi: 10.1016/S0140-6736(21)02141-3 [DOI] [PubMed] [Google Scholar]
- 9.Jiang M, Qin P, Yang X. Comorbidity between depression and asthma via immune-inflammatory pathways: a meta-analysis. J Affect Disord. 2014;166:22–29. doi: 10.1016/j.jad.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 10.Prosser R, Carleton B, Smith A. The comorbidity burden of the treated asthma patient population in British Columbia. Chronic Dis Can. 2010;30(2):46–55. doi: 10.24095/hpcdp.30.2.03 [DOI] [PubMed] [Google Scholar]
- 11.Goral A, Lipsitz JD, Muhsen K, Gross R. Depressive symptoms, risk factors and sleep in asthma: results from a national Israeli health survey. Gen Hosp Psychiatry. 2012;34(1):17–23. doi: 10.1016/j.genhosppsych.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 12.Lu Y, Mak KK, van Bever HPS, et al. Prevalence of anxiety and depressive symptoms in adolescents with asthma: a meta-analysis and meta-regression. Pediatr Allergy Immunol. 2012;23(8):707–715. doi: 10.1111/pai.12000 [DOI] [PubMed] [Google Scholar]
- 13.Leander M, Lampa E, Rask-Andersen A, et al. Impact of anxiety and depression on respiratory symptoms. Respir Med. 2014;108(11):1594–1600. doi: 10.1016/j.rmed.2014.09.007 [DOI] [PubMed] [Google Scholar]
- 14.Ciprandi G, Schiavetti I, Rindone E, Ricciardolo FLM. The impact of anxiety and depression on outpatients with asthma. Ann Allergy Asthma Immunol. 2015;115(5):408–414. doi: 10.1016/j.anai.2015.08.007 [DOI] [PubMed] [Google Scholar]
- 15.Zhang L, Zhang X, Zheng J, et al. Co-morbid psychological dysfunction is associated with a higher risk of asthma exacerbations: a systematic review and meta-analysis. J Thorac Dis. 2016;8(6):1257–1268. doi: 10.21037/jtd.2016.04.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lomper K, Chudiak A, Uchmanowicz I, Rosińczuk J, Jankowska-Polanska B. Effects of depression and anxiety on asthma-related quality of life. Pneumonol Alergol Pol. 2016;84(4):212–221. doi: 10.5603/PiAP.2016.0026 [DOI] [PubMed] [Google Scholar]
- 17.Shen TC, Lin CL, Liao CH, Wei CC, Sung FC, Kao CH. Major depressive disorder is associated with subsequent adult-onset asthma: a population-based cohort study. Epidemiol Psychiatr Sci. 2017;26(6):664–671. doi: 10.1017/S2045796016000664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellegaard O, Wallin JA. The bibliometric analysis of scholarly production: how great is the impact? Scientometrics. 2015;105(3):1809–1831. doi: 10.1007/s11192-015-1645-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson DF, Walker CK. A descriptive and historical review of bibliometrics with applications to medical sciences. Pharmacotherapy. 2015;35(6):551–559. doi: 10.1002/phar.1586 [DOI] [PubMed] [Google Scholar]
- 20.Chen C, Song M, Glanzel W. Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS One. 2019;14(10):e0223994. doi: 10.1371/journal.pone.0223994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Eck NJ, Waltman L, van Eck NJ. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi: 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arruda H, Silva ER, Lessa M, Proença Jr. D, Bartholo R. VOSviewer and Bibliometrix. J Med Libr Assoc. 2022;110(3):392–395. doi: 10.5195/jmla.2022.1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Synnestvedt MB, Chen C, Holmes JH. CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu Symp Proc. 2005;2005:724–728. [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C, Chen Y. Searching for clinical evidence in CiteSpace. AMIA Annu Symp Proc. 2005;2005:121–125. [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Z, Yang Y, Kong W, et al. A Bibliometric and Visual Analysis of Single Nucleotide Polymorphism Studies in Depression. Curr Neuropharmacol. 2024;22(2):302–322. doi: 10.2174/1570159X21666230815125430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu Q, Wang Z, Li Z, Liu X, Oteng Agyeman F, Wang X. Hierarchical Structure of Depression Knowledge Network and Co-word Analysis of Focus Areas. Front Psychol. 2022;13:920920. doi: 10.3389/fpsyg.2022.920920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo XJ, Wu P, Jia X, et al. Mapping the structure of depression biomarker research: a bibliometric analysis. Front Psychiatry. 2022;13:943996. doi: 10.3389/fpsyt.2022.943996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang H, Tian X, Wang X, Wang Y. Evolution and Emerging Trends in Depression Research From 2004 to 2019: a Literature Visualization Analysis. Front Psychiatry. 2021;12:705749. doi: 10.3389/fpsyt.2021.705749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun J, Bai S, Zhao J, et al. Mapping knowledge structure and research of the biologic treatment of asthma: a bibliometric study. Front Immunol. 2023;14:1034755. doi: 10.3389/fimmu.2023.1034755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhen G, Yingying L, Weifang X, Jingcheng D. A bibliometric and scientific knowledge map study of the drug therapies for asthma-related study from 1982 to 2021. Front Pharmacol. 2022;13:916871. doi: 10.3389/fphar.2022.916871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qu Y, Zhang C, Hu Z, et al. The 100 most influential publications in asthma from 1960 to 2017: a bibliometric analysis. Respir Med. 2018;137:206–212. doi: 10.1016/j.rmed.2018.03.014 [DOI] [PubMed] [Google Scholar]
- 32.Fontanella S, Cucco A, Custovic A. Machine learning in asthma research: moving toward a more integrated approach. Expert Rev Respir Med. 2021;15(5):609–621. doi: 10.1080/17476348.2021.1894133 [DOI] [PubMed] [Google Scholar]
- 33.Sundbom F, Malinovschi A, Lindberg E, Alving K, Janson C. Effects of poor asthma control, insomnia, anxiety and depression on quality of life in young asthmatics. J Asthma. 2016;53(4):398–403. doi: 10.3109/02770903.2015.1126846 [DOI] [PubMed] [Google Scholar]
- 34.Oh H, Stickley A, Singh F, Koyanagi A. Self-reported asthma diagnosis and mental health: findings from the Collaborative Psychiatric Epidemiology Surveys. Psychiatry Res. 2019;271:721–725. doi: 10.1016/j.psychres.2018.12.046 [DOI] [PubMed] [Google Scholar]
- 35.Vancampfort D, Stubbs B, Veronese N, Mugisha J, Swinnen N, Koyanagi A. Correlates of physical activity among depressed older people in six low-income and middle-income countries: a community-based cross-sectional study. Int J Geriatr Psychiatry. 2018;33(2):e314–e322. doi: 10.1002/gps.4796 [DOI] [PubMed] [Google Scholar]
- 36.Eisner MD, Katz PP, Lactao G, Iribarren C. Impact of depressive symptoms on adult asthma outcomes. Ann Allergy Asthma Immunol. 2005;94(5):566–574. doi: 10.1016/S1081-1206(10)61135-0 [DOI] [PubMed] [Google Scholar]
- 37.Khurana S, Lyness JM, Mallett S, et al. Association of depressive symptoms with health status and markers of uncontrolled severe asthma. Allergy Asthma Proc. 2019;40(4):230–239. doi: 10.2500/aap.2019.40.4229 [DOI] [PubMed] [Google Scholar]
- 38.Fong WCG, Rafiq I, Harvey M, et al. The Detrimental Clinical Associations of Anxiety and Depression with Difficult Asthma Outcomes. J Pers Med. 2022;12(5):686. doi: 10.3390/jpm12050686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinstein SM, Pugach O, Rosales G, Mosnaim GS, Walton SM, Martin MA. Family Chaos and Asthma Control. Pediatrics. 2019;144(2):e20182758. doi: 10.1542/peds.2018-2758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown ES, Palka JM, Lehman HK, et al. The Impact of Caregiver Depression on Child Asthma Outcomes: pathways and Mechanisms. J Allergy Clin Immunol Pract. 2023;11(1):200–209. doi: 10.1016/j.jaip.2022.09.016 [DOI] [PubMed] [Google Scholar]
- 41.Gwak DY, Tea JC, Fatima FN, et al. Contribution of caregiver and child anxiety and depressive symptoms to child asthma-related quality of life. Ann Allergy Asthma Immunol. 2024;133(3):295–301. doi: 10.1016/j.anai.2024.02.026 [DOI] [PubMed] [Google Scholar]
- 42.Connolly MJ, Yohannes AM. The impact of depression in older patients with chronic obstructive pulmonary disease and asthma. Maturitas. 2016;92:9–14. doi: 10.1016/j.maturitas.2016.07.005 [DOI] [PubMed] [Google Scholar]
- 43.Brown ES, Sayed N, Van Enkevort E, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Escitalopram in Patients with Asthma and Major Depressive Disorder. J Allergy Clin Immunol Pract. 2018;6(5):1604–1612. doi: 10.1016/j.jaip.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tran L, Sharrad K, Kopsaftis Z, et al. Pharmacological interventions for the treatment of psychological distress in patients with asthma: a systematic review and meta-analysis. J Asthma. 2021;58(6):759–769. doi: 10.1080/02770903.2020.1731826 [DOI] [PubMed] [Google Scholar]
- 45.Thoma N, Pilecki B, McKay D. Contemporary Cognitive Behavior Therapy: a Review of Theory, History, and Evidence. Psychodyn Psychiatry. 2015;43(3):423–461. doi: 10.1521/pdps.2015.43.3.423 [DOI] [PubMed] [Google Scholar]
- 46.Harrison S, Geppetti PS. Substance p. Int J Biochem Cell Biol. 2001;33(6):555–576. doi: 10.1016/s1357-2725(01)00031-0 [DOI] [PubMed] [Google Scholar]
- 47.Herpfer I, Lieb K. Substance P and Substance P receptor antagonists in the pathogenesis and treatment of affective disorders. World J Biol Psych. 2003;4(2):56–63. doi: 10.3109/15622970309167952 [DOI] [PubMed] [Google Scholar]
- 48.Rosenkranz MA. Substance P at the nexus of mind and body in chronic inflammation and affective disorders. Psychol Bull. 2007;133(6):1007–1037. doi: 10.1037/0033-2909.133.6.1007 [DOI] [PubMed] [Google Scholar]
- 49.Sharrad KJ, Sanwo O, Cuevas-Asturias S, Kew KM, Carson-Chahhoud KV, Pike KC. Psychological interventions for asthma in children and adolescents. Cochrane Database Syst Rev. 2024;1(1):CD013420. doi: 10.1002/14651858.CD013420.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooley C, Park Y, Ajilore O, Leow A, Nyenhuis SM. Impact of interventions targeting anxiety and depression in adults with asthma. J Asthma. 2022;59(2):273–287. doi: 10.1080/02770903.2020.1847927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hussain S, Khawar R, Amin R, Hamdani A, Majeed A. Psychological flexibility, cognitive emotion regulation and mental health outcomes among patients with asthma in Pakistan. PeerJ. 2023; 11:e15506. doi: 10.7717/peerj.15506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Porsbjerg C, Menzies-Gow A. Co-morbidities in severe asthma: clinical impact and management. Respirology. 2017;22(4):651–661. doi: 10.1111/resp.13026 [DOI] [PubMed] [Google Scholar]
- 53.Fong WCG, Azim A, Knight D, et al. Real-world Omalizumab and Mepolizumab treated difficult asthma phenotypes and their clinical outcomes. Clin Exp Allergy. 2021;51(8):1019–1032. doi: 10.1111/cea.13882 [DOI] [PubMed] [Google Scholar]
- 54.Peng C, Xue L, Yue Y, Chen W, Wang W, Shen J. Duloxetine HCl Alleviates Asthma Symptoms by Regulating PI3K/AKT/mTOR and Nrf2/HO-1 Signaling Pathways. Inflammation. 2023;46(6):2449–2469. doi: 10.1007/s10753-023-01892-5 [DOI] [PubMed] [Google Scholar]
- 55.Ma M, Li G, Qi M, Jiang W, Zhou R. Inhibition of the Inflammasome Activity of NLRP3 Attenuates HDM-Induced Allergic Asthma. Front Immunol. 2021;12:718779. doi: 10.3389/fimmu.2021.718779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sf S, Rm S. An inflammatory review of glucocorticoid actions in the CNS. Brain Behav Immunity. 2007;21(3). doi: 10.1016/j.bbi.2006.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.