Abstract
Vertebro-vertebral arteriovenous fistula (VV-AVF) is an uncommon vascular disorder characterized by an abnormal direct connection between the extracranial vertebral artery (VA), as well as the first and second branches of subclavian arteries, and the draining veins of the paravertebral venous plexus. Endovascular occlusion or surgical ligation of the high-flow arteriovenous fistula is the main goal of treatment for VV-AVF, but there are no guidelines for the best treatment to date. Endovascular treatment is the primary treatment procedure due to its safety, effectiveness, and simplicity. We reported a rare clinical case of the endovascular approach used for occlusion of VV-AVF. A 52-year-old female patient with no history of trauma was presented with right neck pain for a month. Diagnostic angiography demonstrated a high-flow VV-AVF at C3-C4 level. After endovascular occlusion with detachable-balloon embolization, the fistula was completely obliterated. To our knowledge, endovascular occlusion for VV-AVF patients is safe and effective. Detachable balloon embolization can be considered a well-tolerated treatment.
Keywords: Vertebro-vertebral arteriovenous fistula, Endovascular treatment, Detachable balloon, Embolization
Introduction
Vertebro-Vertebral Arteriovenous Fistula (VV-AVF) is an uncommon vascular disorder characterized by an abnormal direct connection between the vertebral artery (VA) ostium and the adjacent vertebral venous plexus. This is the uncommon and complex lesion that can arise spontaneously or after the iatrogenic or mechanical trauma. The VV-AVF can cause headaches, pulsatile neck masses, tinnitus, neurological impairments, congestive heart failure, or no symptom. The primary objective of treatment for VV-AVF is to achieve endovascular occlusion or surgical closure of the high-flow arteriovenous fistula [1,2]. However, there are currently no established recommendations for the most effective therapeutic approach. Before the advancement of endovascular treatments, many surgical approaches were employed but often proven unsuccessful and consistently challenging due to the numerous arteriolized venous channels and the direct inaccessibility of many of the fistulas. Today, endovascular therapy is the primary treatment approach due to its simplicity, efficacy, and safety with using detachable balloons, Onyx, coils, and stenting. Endovascular treatment could be primarily achieved by sacrificing the vertebral artery provided by the anastomosis of the contralateral vertebral artery and basilar artery or by directly selective embolization in the feeding branches, but the vertebral artery is preserved [1,3]. Complications comprise of ischemic lesions in the case of the insufficient collateral supply or the clot spreading to involve intracranial circulation, and the removed high-flow shunt could cause hyperperfusion [4]. We recorded a clinical case with detachable balloons embolization for VV-AVF patient.
Case report
Patient information: A 52 year-old woman with no history of trauma, neck surgery presented with burning and pulsating pain in the right back of the neck for 1 month.
Clinical findings: She was alert [Glasgow coma scale (GCS) = 15 score], stable vital signs with blood pressure of 120/70 mmHg, regular heart rate; no limb weakness, no localized neurological signs; normal neck skin; other organs was not recorded any abnomarlity.
Diagnostic assessment: The brain Magnetic Resonance Angiography (MRA) showed loss of flow signal of right extracranial vertebral artery surrounded by multiple dilated, serpiginous of the vertebral venous plexus (Fig. 1).
Fig. 1.
Diagnostic brain MRA: loss of flow signal of right extracranial vertebral artery surrounded by multiple dilated, serpiginous of the vertebral venous plexus (green circle).
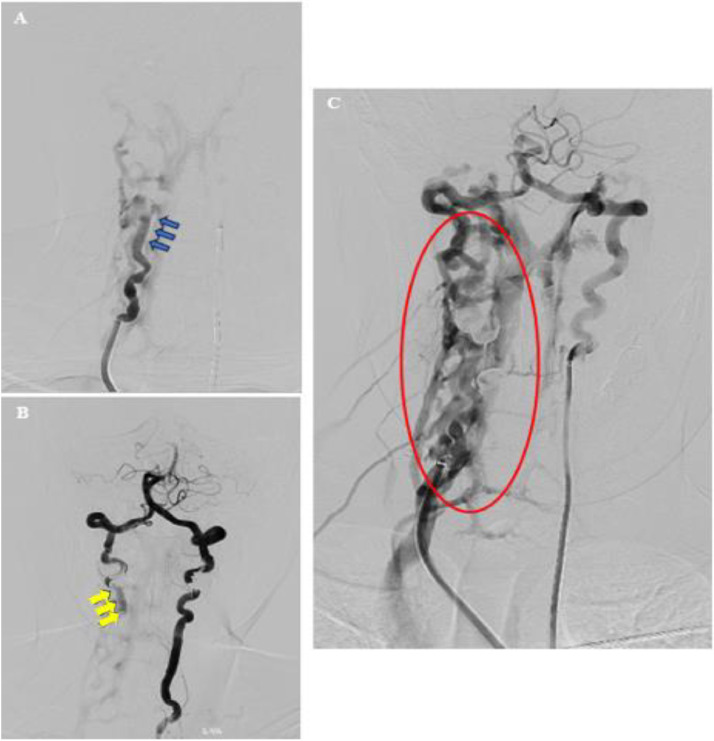
Patient was taken to the angiosuite for angiogram and endovascular intervention. The angiogram demonstrated an abnormal direct connection between the extracranial VA and the paravertebral venous plexus with high-flow VV-AVF at C3–C4 level. The fistula was fed by proximal antegrade in right VA and distal retrograde flow in left VA. And it was drained into the vertebral venous plexus. The fistula site was clearly demonstrated with fusion of bilateral VA angiography (Fig. 2).
Fig. 2.
Diagnostic cerebral angiography (A, B, C). (A) The fistula was fed by proximal antegrade in right VA (blue arrows); (B) and distal retrograde flow in left VA (yellow arrows); (C) The fistula site was clearly demonstrated with fusion of bilateral VA angiography and was drained into the vertebral venous plexus (red circle).
Therapeutic interventions
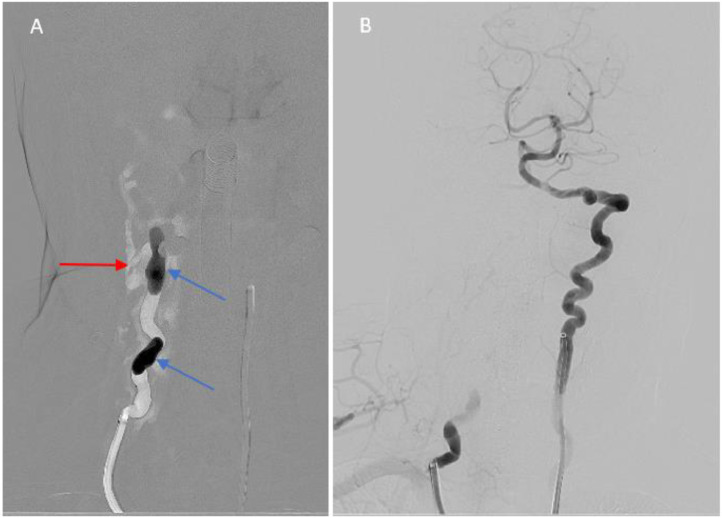
Before accessing 8F sheath in the femoral artery, the anesthesia was performed. A Neuron MAX 088 guiding catheter (Penumbra, Alameda, CA) was placed in the right vertebral artery at C5-C6 level, and a 5F Grafia diagnostic catheter (SUNGJIN-HITECH Co., Republic of Korea) was placed in the left vertebral artery at V2 segment [5]. We performed the dual roadmap technique to determine exactly the fistula location; through a guide catheter, we used a coaxial system consisting of Magic MABDTE 1.8F microcatheter (Balt) + GOLDBAL 2 (Balt) and placed inside the fistula. Then, the balloon was inflated slowly to a proper size to obliterate the fistula (4 ml contrast). A control angiogram was performed to determine the degree of obstruction. Then the second GOLDBAL 2 was placed near the first GOLDBAL 2 to increase the degree of fistula obstruction. An angiogram showed the fistula was obliterated completely (Fig, 3).
Fig. 3.
Intervention of VV-AVF (A, B). (A) Two GOLDBAL 2 balloons (blue arow) were placed inside the fistula (red arrow); (B) An angiogram showed the fistula was obliterated completely.
Follow-up and intervention outcomes
After intervention: Symptoms were released after treatment.
At discharge: 2 days after intervention, the patient's symptoms were completely released with no neck pain.
At the 3 months: the patient was normal without neck pain recurrence, and the brain MRA showed no VV-AVF recurrence and adequate supply of the posterior circulation (Fig. 4).
Fig. 4.
Diagnostic brain MRA after 3 months of intervention: No vertebro-vertebral arteriovenous fistula recurrence and adequate supply of the posterior circulation.
Disccussion
A rare vascular condition known as vertebro-vertebral arteriovenous fistula is typified by an irregular shunt between the extracranial vertebral artery and associated veins. Three distinct reasons can be identified: traumatic, iatrogenic, and spontaneous. Traumatic VV-AVF is often occurred in young men, young women are more likely to experience spontaneous type, and iatrogenic type is more prevalent in the elderly. Moreover, the fistula can be found below the C5 segment (44%), at C2 to C5 segments (11%), and between C1 and C2 segments (46%). Spontaneous VV-AVF is most commonly located between C1-C2; traumatic VV-AVF affects the lower portion of the vertebral artery (below C5) [1,2,6,7]. Our patient is a middle-aged woman with a fistula at C3-C4 and no history of head and neck trauma, so the cause is still unknown, possibly spontaneous. Several asymptomatic patients were discovered inadvertently. The tinnitus symptom results from the rapid arteriovenous shunting through the fistula. High-flow arteriovenous shunting can induce dizziness and diplopia as a result of vertebral arterial steal. The symptoms such as cervical myelopathy and radiculopathy with headache may arise from venous congestion or a direct compressive mass effect due to an engorged epidural venous pouches [2,3]. Our patient complained of right neck discomfort.
Currently, there are no established guidelines for the optimal treatment of VV-AVF. The objective of treatment is to maintain the patency of the vertebral artery and block the fistula site. Before the advancement of endovascular treatments, many surgical approaches were employed. Operative therapy of VV-AVF has often proven unsuccessful and consistently challenging due to the numerous arteriolized venous channels and the direct inaccessibility of many of the fistulas [3,8].
Today, endovascular therapy is the primary treatment approach due to its simplicity, efficacy, and safety. For almost 25 years, endovascular therapy with detachable balloons has been a safe and effective method for treating VV-AVF. Onyx or coils are more safer than the detachable balloons. Self-expanding or balloon-expandable covered stents are another emerging alternative for reconstructing damaged head and neck arteries. Nevertheless, stent reconstruction requires long-term antiplatelet therapy, which carries an elevated risk of significant bleeding, particularly when patients with traumatic fistula or subarachnoid hemorrhage require subsequent orthopedic or cerebrospinal fluid diversion surgery [1,2,4,[7], [8], [9]].
Because the V1-2 segment is straight and inflexible, the V3 segment is tortuous and flexible. In the fistula at the V1-2 segment of the VA, covered stent placement is an effective option that still maintains the ipsilateral VA flow. In the case of the fistula in the V3 segment, embolic devices such as detachable coils, NBCA glue, ... is preferable to a covered stent due to enhanced vertebral artery mobility and a high risk of fistula recurrence [4,7,9]. Our patient had a complex, high-flow vascular fistula in the V2 segment. The blood vessel in this segment was quite tortuous, so stent placement was not suitable. At this fistula location, we can only use a detachable balloon, coil, or Onyx to close the fistula. Using Onyx will be difficult to control and can cause distal vertebrobasilar artery occlusion due to a complex, high-flow fistula. Using coil is also not suitable because a large fistula with high flow will consume a large number of coils and not completely close the fistula. Therefore, we used a balloon to occlude the fistula and blood vessel in this segment. Immediately after the intervention, the patient's symptoms completely disappeared. After 3 months, a follow-up MRA scan of the brain showed complete blockage of the fistula, and the patient had no complaints of any symptoms.
Conclusion
Vertebro-Vertebral Arteriovenous Fistula (VV-AVF) is an uncommon neurovascular condition. Today, endovascular treatment is the primary treatment procedure due to its safety, effectiveness, and simplicity. Detachable balloon therapy is a cost-effective, reliable, and safe treatment option for VV-AVF, especially a large, high flow fistula.
Author contributions
Linh Hoang Duong and Giang Luu Nguyen contributed equally to this article as co-frst authors. Linh Hoang Duong, Giang Luu Nguyen, and Luan Minh Bao Tran contributed to write original draft. Linh Hoang Duong and Giang Luu Nguyen contributed to collect and interpret the imaging. Linh Hoang Duong, Giang Luu Nguyen, Thang Minh Le, and Tran Tran Nguyen made substantial contributions to collect patient data and clinical data analysis. All authors have read, revised, and approved the final published version of the manuscript. All authors were responsible for submission of our study for publication.
Ethics approval and consent to participate
Ethical approval was not necessary for the preparation of this article. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Informed consent for patient information to be published in this article was obtained.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: We would like to acknowledge our colleagues at Can Tho S.I.S General Hospital and Can Tho University of Medicine and Pharmacy for their wonderful collaboration.
References
- 1.Beaujeux RL, Reizine DC, Casasco A, et al. Endovascular treatment of vertebral arteriovenous fistula. Radiology. 1992;183(2):361–367. doi: 10.1148/radiology.183.2.1561336. [DOI] [PubMed] [Google Scholar]
- 2.Briganti F, Tedeschi E, Leone G, et al. Endovascular treatment of vertebro-vertebral arteriovenous fistula. A report of three cases and literature review. Neuroradiol J. 2013;26(3):339–346. doi: 10.1177/197140091302600315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR Am J Roentgenol. 1988;150(2):405–412. doi: 10.2214/ajr.150.2.405. [DOI] [PubMed] [Google Scholar]
- 4.Olson RW, Baker HL, Jr, Svien HJ. Arteriovenous fistula: a complication of vertebral angiography: report of a case. J Neurosurg. 1963;20:73–75. doi: 10.3171/jns.1963.20.1.0073. [DOI] [PubMed] [Google Scholar]
- 5.Minh TL, Chi CT, Hoai NN, et al. Rescue extracranial vertebral stenting in tandem occlusions: A preliminary Vietnamese study. Interv Neuroradiol. 2024 doi: 10.1177/15910199241264342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeh CH, Chen YL, Wu YM, Huang YC, Wong HF. Anatomically based approach for endovascular treatment of vertebro-vertebral arteriovenous fistula. Interv Neuroradiol. 2014;20(6):766–773. doi: 10.15274/INR-2014-10072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vinchon M, Laurian C, George B, et al. Vertebral arteriovenous fistulas: a study of 49 cases and review of the literature. Cardiovasc Surg. 1994;2(3):359–369. [PubMed] [Google Scholar]
- 8.Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: a clinical review. Eur Spine J. 2011;20(9):1405–1416. doi: 10.1007/s00586-011-1862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herrera DA, Vargas SA, Dublin AB. Endovascular treatment of traumatic injuries of the vertebral artery. AJNR Am J Neuroradiol. 2008;29(8):1585–1589. doi: 10.3174/ajnr.A1123. [DOI] [PMC free article] [PubMed] [Google Scholar]