Abstract
Blunt esophageal injury is an exceptionally rare condition, with complete esophageal avulsion being almost unprecedented in adults. This case study details the clinical presentation, surgical management, and postoperative course of a 50-year-old male who sustained a complete esophageal avulsion following blunt abdominal trauma. The patient presented with increasing abdominal pain two hours after falling while stepping up onto a high truck step, striking his upper abdomen on the step. CT imaging revealed pneumomediastinum and pneumoperitoneum. Emergent exploratory laparotomy and thoracotomy uncovered a complete avulsion of the esophagus from the gastroesophageal junction. The surgical repair involved resection of the damaged esophagus and gastric cardia, an esophagogastric anastomosis using a 25 mm EEA stapler, and the creation of an omental pedicle flap. Postoperative management included antibiotic prophylaxis and intensive care monitoring.
Blunt traumatic esophageal injuries, although rare, pose significant diagnostic and therapeutic challenges due to their potential for severe complications such as mediastinitis, sepsis, and multi-organ failure. Prompt recognition of the injury through imaging and clinical assessment is essential for initiating timely surgical intervention. The surgical approach must be meticulously planned to address the complexity of the injury, often requiring a combination of thoracic and abdominal procedures. Additionally, the role of a multidisciplinary team, including surgeons, intensivists, and gastroenterologists, is crucial in managing both the immediate and long-term aspects of patient care. This case emphasizes the necessity for a comprehensive and coordinated treatment strategy to optimize outcomes. It highlights the importance of continued research and education in managing such rare and severe injuries.
Keywords: Blunt trauma, Esophageal avulsion, Esophageal injury, Gastroesophageal junction, Surgical repair, Postoperative complications, Gastroesophageal reflux
Introduction
Blunt esophageal injury is a rare occurrence in trauma surgery, with incidents of 0.001 % attributed to blunt chest mechanisms [1]. Among these, the complete avulsion of the esophagus from the gastroesophageal junction is extraordinarily rare, particularly in adults [2]. The inherent anatomy and protected location of the esophagus within the thoracic cavity typically shield it from blunt trauma, making such injuries a significant clinical curiosity when they do occur [3]. The sparse literature regarding blunt esophageal avulsions, especially in adult patients, highlights the uniqueness of such cases and their challenges in diagnosis and management [2,4].
The morbidity and mortality associated with esophageal injuries remain high, with rates of up to 29.3 % for blunt trauma cases [3,5]. These injuries can lead to severe complications, including pneumonia, empyema, mediastinitis, sepsis, intra-abdominal abscesses, and esophageal stenosis [6]. Rapid identification and prompt surgical intervention are paramount in mitigating these risks [7]. The time to surgical repair is a critical determinant of patient outcomes, as delays can exacerbate the severity of complications and increase mortality rates [8]. This urgency emphasizes the need for a high index of suspicion and swift diagnostic action in patients presenting with symptoms suggestive of esophageal injury following blunt trauma [9].
Historical data on esophageal injuries predominantly focus on penetrating trauma, with studies such as the one conducted by Schellenberg et al. in 2017 highlighting that 96 % of traumatic esophageal injuries are due to penetrating mechanisms [10]. The same study noted that 12 % of these injuries involved the gastroesophageal junction [10]. This data aligns with earlier findings from a 1988 meta-analysis by Beal et al., which reported only 96 cases of blunt esophageal injuries between 1900 and 1988, with a mere five involving the lower esophagus [11]. These statistics illustrate the rarity of blunt esophageal injuries and the even greater rarity of complete esophageal avulsions [3].
Given blunt esophageal avulsion's extreme rarity and complexity, its management presents unique challenges [12]. The anatomical disruption necessitates meticulous surgical repair to reestablish gastrointestinal continuity while minimizing the risk of postoperative complications [13]. Furthermore, the long-term consequences of such injuries, including severe gastroesophageal reflux and esophagitis, must be anticipated and managed [14]. This case report aims to shed light on the clinical presentation, surgical management, and postoperative course of a rare case of blunt traumatic complete esophageal avulsion in an adult, contributing valuable insights to the limited body of literature on this topic.
Case presentation
A 50-year-old male presented to the emergency department with a chief complaint of severe abdominal pain following a fall. The patient was a semi-truck driver who reported climbing the stairs to enter the truck when he slipped and fell. The fall resulted in him striking the upper portion of this abdomen on the truck step with his full body weight. He reported immediate intense pain that he described as sharp, 10/10 in intensity, and constant. The pain was aggravated by movement, leading him to seek medical attention. He denied any associated nausea, vomiting, fever, or chills.
Initial assessment and plan
Pneumomediastinum
The presence of pneumomediastinum was noted on admission, likely tracking from the abdomen. An esophagogastroduodenoscopy (EGD) and bronchoscopy were planned to rule out additional injuries (Fig. 1).
Fig. 1.
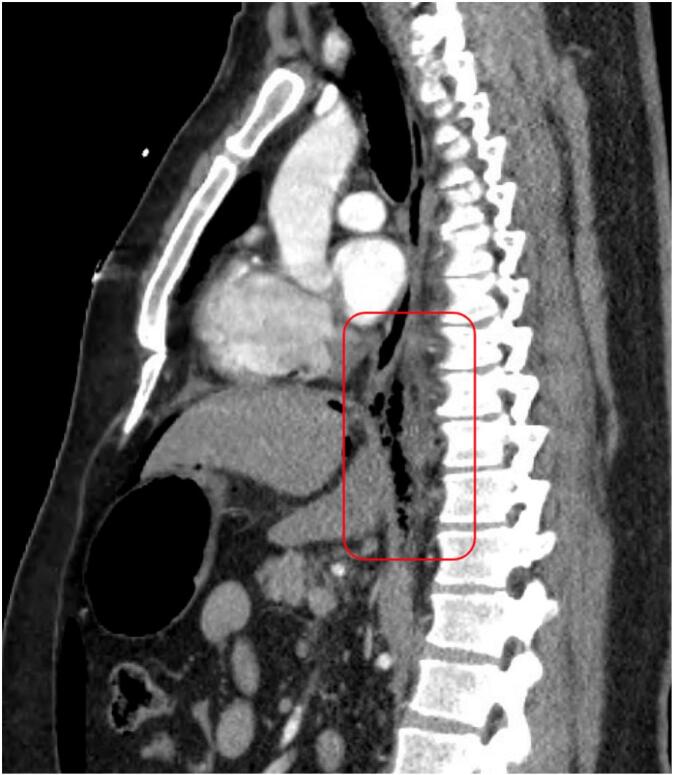
CT Chest Abdomen Pelvis with contrast (sagittal view) showing pneumomediastinum and pneumoperitoneum concerning for an esophageal injury given the preponderance of gas behind the esophagus near the GE junction (red box). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fall (initial encounter)
The patient's fall resulted in intra-abdominal free air of a moderate amount, suggesting a potential bowel perforation. Urgent surgical exploration was deemed necessary (Fig. 2).
Fig. 2.
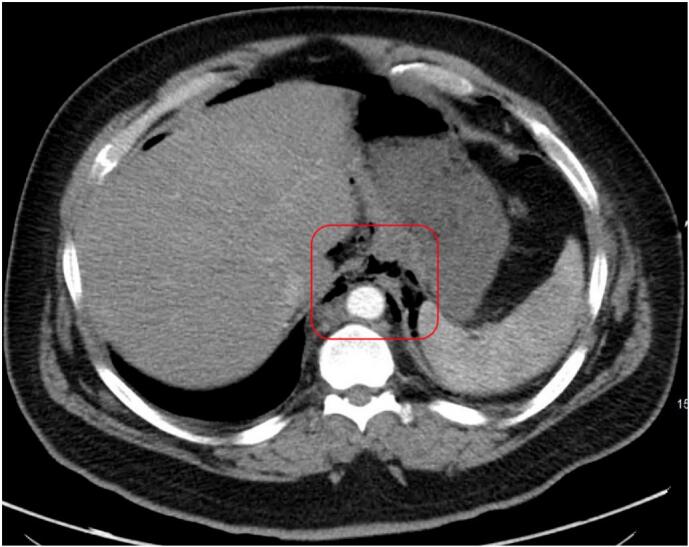
CT Chest Abdomen Pelvis with contrast (axial view) showing pneumoperitoneum with gas along the esophagus near the GE junction (red box). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Free intraperitoneal air
The presence of free intraperitoneal air was confirmed, consistent with intra-abdominal injury. Given the mechanism of injury and clinical presentation, urgent surgical intervention was planned.
Operative findings
During the exploratory laparotomy, the abdomen was entered via a midline incision, revealing complete disruption of the gastroesophageal junction with gastric contents spilling into the abdominal cavity. The esophagus was found to be completely avulsed from the stomach and had retracted into the mediastinum.
Operative intervention to repair the esophageal avulsion involved a comprehensive surgical approach to restore gastrointestinal continuity and prevent continued contamination. A left thoracotomy was performed to provide adequate visualization and access for the repair. Approximately 2 cm of the distal esophagus and the gastric cardia were resected to healthy tissue. During the procedure, it was noted that the anterior vagus nerve was completely avulsed, and the posterior vagus nerve was transected intraoperatively, resulting in a complete truncal vagotomy. An end-to-end esophagogastric anastomosis was created using a 25 mm EEA stapler inserted via a pyloromyotomy. An omental pedicle flap was fashioned around the repair site to reinforce the anastomosis and reduce the risk of leakage. Thorough irrigation of the chest and abdominal cavities was conducted to remove any contaminants and minimize the risk of postoperative infection. Postoperative management included intensive care monitoring and prophylactic antibiotic therapy with vancomycin, piperacillin-tazobactam, and micafungin to prevent sepsis and other complications. This detailed surgical strategy was crucial for addressing the complex nature of the esophageal avulsion and optimizing the patient's immediate and long-term outcomes.
Postoperative course
Postoperatively, the patient was managed in the intensive care unit and started on vancomycin, piperacillin-tazobactam, and micafungin for antibiotic prophylaxis. Despite initial stability, he required reintubation on postoperative day 5 due to respiratory distress from pain-induced splinting. He was extubated again and transferred to the general surgical flooron postoperative day 14, and subsequently discharged home on day 21, tolerating oral intake.
Follow-up and long-term management
Two months after surgery, the patient had his gastrostomy and jejunostomy tubes removed. However, at the three-month follow-up, he reported severe retrosternal burning, dysphagia, and early satiety. An esophagogram was performed and found to be unremarkable. He was prescribed pantoprazole and sucralfate, which provided temporary relief.
At the fifteen-month follow-up, the patient's symptoms had worsened, now including frequent episodes of nausea and blood‑tinged vomiting occurring 3–7 days per week. A barium swallow showed mild distal esophageal narrowing just above the lower esophageal sphincter but with no barium flow restriction (Fig. 3). Given the severity of his symptoms and their impact on his quality of life, he was referred to a tertiary center for further evaluation and consideration of additional surgical management options.
Fig. 3.
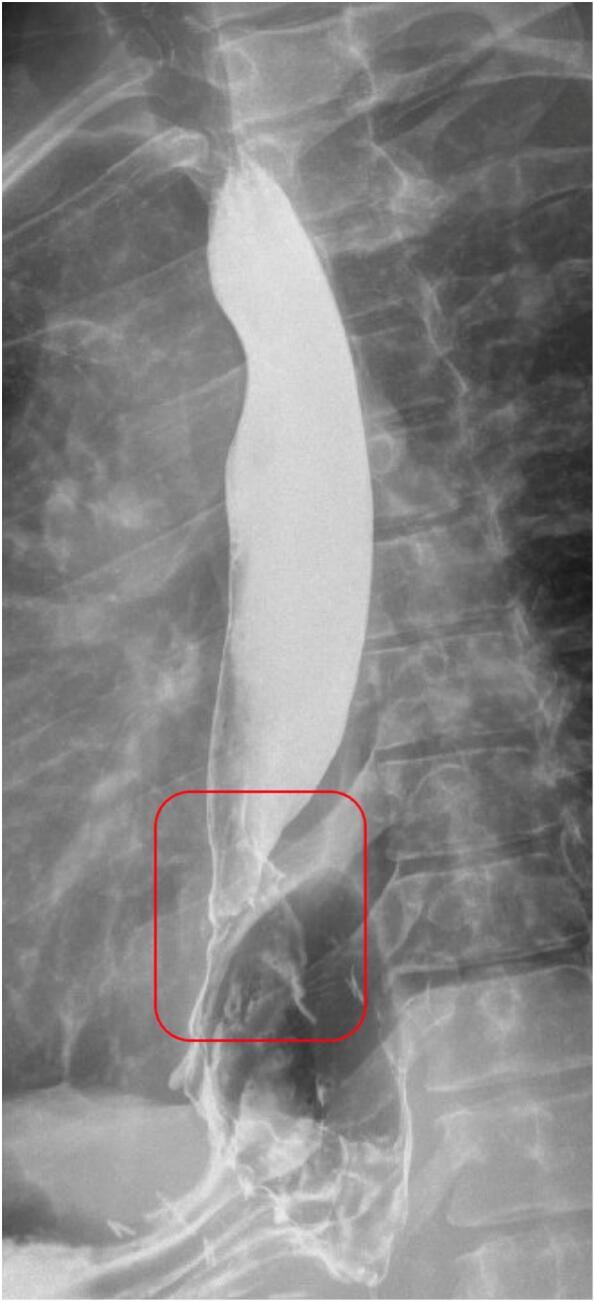
Barium swallow imaging demonstrates mild distal esophageal narrowing just above the lower esophageal sphincter. Despite the narrowing, there is no restriction in the barium flow, indicating preserved esophageal patency (highlighted in red box). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Further diagnostic evaluation included an esophagogastroduodenoscopy (EGD), which revealed erosive esophagitis beginning at 31 cm and confluent exudate covering 25–30 % of the esophageal circumference just above the gastroesophageal junction (Fig. 4). The anastomosis at 37 cm was visibly larger than expected (Fig. 5). The patient was also noted to have erosive antral gastritis. Biopsies taken during the EGD were negative for H. pylori but confirmed the presence of erosive esophagitis and the need for continued surveillance and management.
Fig. 4.
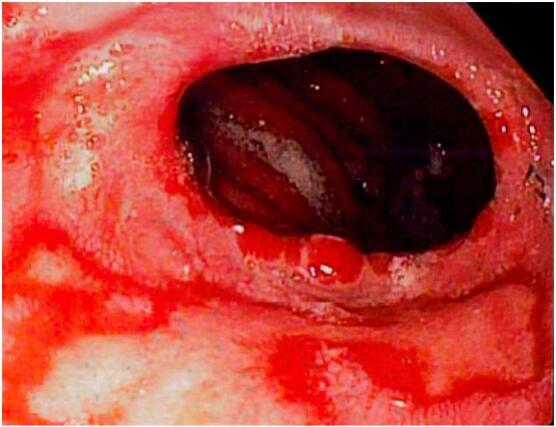
Esophagogastroduodenoscopy (EGD) photo (antegrade view) displaying erosive esophagitis with exudates at the anastomosis site, along with visible surgical staples.
Fig. 5.

Esophagogastroduodenoscopy photo (retroflex view) showing the esophagogastric anastomosis that is clearly larger than a normal anatomic esophagogastric junction.
The patient's complex postoperative course and ongoing symptoms highlighted the need for potential revision of the initial esophagogastrostomy. Options for addressing his severe gastroesophageal reflux and esophagitis included further surgical interventions such as esophagectomy with gastric conduit, colonic interposition, or Roux-En-Y gastric bypass. The patient was counseled on these options and the importance of continued follow-up to manage his symptoms and improve his quality of life.
Discussion
Traumatic esophageal injuries, though rare, present significant challenges due to their potential for severe morbidity and mortality [15]. These injuries can occur as a result of both penetrating and blunt trauma, with the latter being particularly uncommon due to the esophagus's protected location within the thoracic cavity [3]. When blunt trauma does result in esophageal injury, the mechanism often involves a sudden increase in intraluminal pressure against a closed glottis, combined with a forceful impact, leading to a “bursting” type of injury [2]. The overall incidence of blunt esophageal injuries is low, but their consequences can be severe, necessitating prompt and effective management [11].
Blunt esophageal avulsion, the complete separation of the esophagus from the gastroesophageal junction, is an exceedingly rare and severe form of esophageal injury [2,5]. Such injuries often present with nonspecific symptoms that may include severe chest or abdominal pain, dysphagia, dyspnea, and signs of systemic infection or sepsis [8]. The presence of pneumomediastinum, pneumoperitoneum, or subcutaneous emphysema on imaging studies, such as chest X-rays or computed tomography (CT) scans, can provide critical diagnostic clues. In the case presented, the patient's fall resulted in immediate severe abdominal pain, with CT imaging revealing pneumomediastinum and pneumoperitoneum, prompting urgent surgical exploration [16].
The surgical management of traumatic esophageal avulsion is complex and requires a multi-faceted approach [1]. In this case, the operative intervention included both an exploratory laparotomy and a left thoracotomy to access and repair the injury. Approximately 2 cm of the distal esophagus and the gastric cardia were resected to healthy tissue. The anterior vagus nerve was found to be completely avulsed, and the posterior vagus nerve was transected, necessitating a complete truncal vagotomy. An end-to-end esophagogastric anastomosis was performed using a 25 mm EEA stapler, reinforced with an omental pedicle flap to support the anastomosis and minimize the risk of leakage. Thorough irrigation of the chest and abdominal cavities was conducted to remove any contaminants and reduce the risk of postoperative infection.
Postoperative management of esophageal avulsion includes intensive monitoring for complications such as anastomotic leaks, strictures, and infections [9]. Antibiotic prophylaxis is critical to prevent sepsis, and in this case, the patient was treated with vancomycin, piperacillin-tazobactam, and micafungin [17]. Despite these precautions, the patient experienced significant postoperative complications, including severe gastroesophageal reflux and erosive esophagitis, which are common following such extensive surgical intervention. These complications were managed initially with proton pump inhibitors and sucralfate, but the patient required further diagnostic evaluations and consideration of additional surgical interventions due to persistent symptoms.
Long-term follow-up is essential for patients with traumatic esophageal injuries, particularly those who have undergone complex repairs like esophagogastric anastomosis [18]. Potential complications include chronic gastroesophageal reflux, esophagitis, and anastomotic strictures, which may necessitate further surgical revisions such as esophagectomy with gastric conduit or Roux-En-Y gastric bypass [6]. The importance of a multidisciplinary approach involving surgeons, gastroenterologists, and nutritional specialists cannot be overstated in managing both the immediate and extended postoperative care of these patients.
The management of traumatic esophageal injuries, particularly complete avulsions, is highly challenging and necessitates prompt diagnosis, meticulous surgical intervention, and comprehensive postoperative care [10].
Conclusion
Blunt traumatic esophageal avulsion, though exceedingly rare, presents significant challenges in both diagnosis and management due to its potential for severe morbidity and mortality. Rapid identification and immediate surgical intervention are paramount in reducing the risk of complications such as sepsis, mediastinitis, and multi-organ failure. The critical nature of these injuries necessitates that healthcare providers maintain a high index of suspicion when evaluating patients with blunt chest or abdominal trauma presenting with suggestive symptoms.
Long-term management of patients who survive such injuries requires vigilant follow-up to monitor for complications such as severe gastroesophageal reflux and esophagitis, which can significantly impact quality of life. The complexity of these cases often necessitates a multidisciplinary approach involving surgical, gastroenterological, and nutritional expertise to optimize patient outcomes.
CRediT authorship contribution statement
Nathaniel Grabill: Writing – review & editing, Validation, Supervision, Resources, Data curation. Mena Louis: Writing – original draft. Nicole Redenius: Writing – original draft, Investigation, Conceptualization. Mariah Cawthon: Investigation, Data curation. Brian Gibson: Supervision, Investigation.
Declaration of competing interest
We have nothing to declare.
Contributor Information
Nathaniel Grabill, Email: Nathaniel.grabill@nghs.com.
Mariah Cawthon, Email: Mariah.cawthon@nghs.com.
Brian Gibson, Email: brian.gibson@nghs.com.
References
- 1.Fabien J.J., McCranie D., Kington D., Dougherty-Welch S. Blunt traumatic esophageal injury: decreased mortality with urgent repair. Am. Surg. Sep 2022;88(9):2212–2214. doi: 10.1177/00031348221091947. [DOI] [PubMed] [Google Scholar]
- 2.Uygun I., Otcu S., Aydogdu B., Okur M.H., Arslan M.S. Total esophageal avulsion at the esophagogastric junction after blunt trauma. Case Rep. Surg. 2013;2013 doi: 10.1155/2013/265073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdulrahman H., Ajaj A., Shunni A., et al. Blunt traumatic esophageal injury: unusual presentation and approach. Int. J. Surg. Case Rep. 2014;5(1):16–18. doi: 10.1016/j.ijscr.2013.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mubang RN, Sigmon DF, Stawicki SP. Esophageal Trauma. StatPearls. StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [PubMed]
- 5.Bryant A.S., Cerfolio R.J. Esophageal trauma. Thorac. Surg. Clin. Feb 2007;17(1):63–72. doi: 10.1016/j.thorsurg.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Gambhir S., Grigorian A., Swentek L., et al. Esophageal trauma: analysis of incidence, morbidity, and mortality. Am. Surg. Oct 1 2019;85(10):1134–1138. [PubMed] [Google Scholar]
- 7.Bhatia N.L., Collins J.M., Nguyen C.C., Jaroszewski D.E., Vikram H.R., Charles J.C. Esophageal perforation as a complication of esophagogastroduodenoscopy. J. Hosp. Med. May 2008;3(3):256–262. doi: 10.1002/jhm.289. [DOI] [PubMed] [Google Scholar]
- 8.Ertekin C, Yanar HT, Güloğlu R, Taviloğlu K, Dilege S. [Esophageal injuries]. Ulus Travma Derg. Jan 2001;7(1):22-7. Ozofagus yaralanmalari. [PubMed]
- 9.Chirica M., Kelly M.D., Siboni S., et al. Esophageal emergencies: WSES guidelines. World J. Emerg. Surg. 2019;14:26. doi: 10.1186/s13017-019-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schellenberg M., Inaba K., Bardes J.M., et al. Defining the gastroesophageal junction in trauma: epidemiology and management of a challenging injury. J. Trauma Acute Care Surg. Nov 2017;83(5):798–802. doi: 10.1097/ta.0000000000001563. [DOI] [PubMed] [Google Scholar]
- 11.Dalal S., Dalal N., Goyal P. Isolated esophageal injury following blunt thoracic trauma: a rarity. Gastroenterology Res. Oct 2009;2(5):307–308. doi: 10.4021/gr2009.10.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sudarshan M., Cassivi S.D. Management of traumatic esophageal injuries. J. Thorac. Dis. Feb 2019;11(Suppl. 2):S172–s176. doi: 10.21037/jtd.2018.10.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaman L., Iqbal J., Kundil B., Kochhar R. Management of esophageal perforation in adults. Gastroenterology Res. Dec 2010;3(6):235–244. doi: 10.4021/gr263w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiman D.S., Walker W.A., Brosnan K.M., Pate J.W., Fabian T.C. Noniatrogenic esophageal trauma. Ann. Thorac. Surg. Apr 1995;59(4):845–849. doi: 10.1016/0003-4975(95)00008-9. discussion 849-50. [DOI] [PubMed] [Google Scholar]
- 15.Ghahremani G.G. Esophageal trauma. Semin. Roentgenol. Oct 1994;29(4):387–400. doi: 10.1016/s0037-198x(05)80052-5. [DOI] [PubMed] [Google Scholar]
- 16.Bastos R.B., Graeber G.M. Esophageal injuries. Chest Surg. Clin. N. Am. May 1997;7(2):357–371. [PubMed] [Google Scholar]
- 17.Petrone P., Kassimi K., Jiménez-Gómez M., Betancourt A., Axelrad A., Marini C.P. Management of esophageal injuries secondary to trauma. Injury. Aug 2017;48(8):1735–1742. doi: 10.1016/j.injury.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 18.Walker P.F., Galvagno S.M., Sachdeva A., Feliciano D.V., Scalea T.M., O’Connor J.V. Operative management of aerodigestive injuries: improved survival over two decades. Am. Surg. Dec 2023;89(12):5982–5987. doi: 10.1177/00031348231180917. [DOI] [PubMed] [Google Scholar]


