Abstract
Patient: Male, 48-year-old
Final Diagnosis: Ectopic thyroid tissue
Symptoms: Dysphagia • swelling in neck
Clinical Procedure: —
Specialty: Endocrinology and Metabolic • Gastroenterology and Hepatology • Histology and Embryology • Otolaryngology • Surgery
Objective:
Rare coexistence of disease or pathology
Background:
We present a rare case of an ectopic thyroid nodule hyperplasia, confirmed postoperatively after excision and histopathological examination of a chronic cervical mass. We discuss the different clinical and therapeutic features of this rare thyroid dysgenesis caused by a defect of migration of the gland along its normal way of descent.
Case Report:
A 48-year-old man with a history of hypertension and asthma presented with dysphagia and a progressively growing firm mass at the anterior part of his neck over the past 6 months. Ultrasound and computed tomography suggested that the mass was attached only to the anterior part of the larynx, without connection to the thyroid, and with a multinodular gland in normal position. A complete surgical excision was performed under general anaesthesia through an external cervical approach. The mass, measuring 60×40 mm, was sent for a histological assessment, which concluded a fully encapsulated ectopic thyroid mass attached only to the soft tissues of the anterior part of the larynx, not showing any sign of malignancy transformation. The outcome of the surgery was marked by a quick recovery, with an improvement of the initial symptoms, proper healing of the surgical scar, and durable normal thyroid functioning after a regular follow-up of 6 months.
Conclusions:
Nonspecific symptoms can reveal ectopic thyroid tissue growth. Appropriate neck imaging combined, when available, with fine needle aspiration help to determine the extent of the mass and predict its nature. Surgical excision and histological analysis are required to confirm the diagnosis and to exclude any thyroid neoplasm.
Key words: Pathology, Surgical; Thyroid Dysgenesis; Thyroid Neoplasms; Tomography Scanners, X-Ray Computed
Introduction
Ectopic thyroid nodules are a rare entity referring to the presence of thyroid tissue out of the normal position at the lower part of the cervical area, in front of the cricoid and thyroid cartilages of the larynx and the first rings of the trachea [1,2]. This represents the most common organogenesis defect of the gland, even if the prevalence is still low, ranging between 1 per 100 000 and 1 per 300 000 [3–6]. It is known that the primitive thyroid derives from the endoderm epithelium around the center of the primitive digestive tract [7]. Usually, the thyroid primordium penetrates the underlying mesoderm and migrates anteriorly as a diverticulum attached to the base of the pharynx by the thyroglossal canal [3–5]. Around the seventh week of gestation, the thyroid primordium migrates anteriorly to the hyoid bone and the larynx toward its normal position at the lower anterior part of the neck [1,8]. Usually, ectopic thyroid tissue lies along the path of the thyroglossal canal, as a result of default or interruption of gland migration, between the base of the tongue and the mediastinum [2,7,9]. Some authors have suggested that thyroid follicular cells derive from a median and a lateral thyroid bud, and that aberrant thyroid tissues found in the submandibular and lateral neck regions originate from a defective lateral thyroid component that could not migrate and fuse with the median thyroid part [6,7]. More than 90% of the ectopic thyroid nodules were found at the lingual and sublingual areas [2]. Few cases have been reported in other regional sites, including the trachea, submandibular area, lateral cervical region, and mediastinum [4,8,9]. Some authors reported the presence of an ectopic thyroid tissue in some locations away from the head and neck area [3,7,10]. The coexistence of multiple synchronous ectopic thyroid nodules is still an exceptional clinical finding [6,8]. We present in this observation a case of an ectopic thyroid nodule hyperplasia, presenting as nonspecific chronic cervical mass, and discuss the different clinical and therapeutic features of this entity.
Case Report
A 48-year-old man presented with a history of difficulty in swallowing noticed 2 months before his consultation, along with a slowly growing mass at the anterior part of his neck over the past 6 months. The patient was examined first by the gastroenterology consultant for his symptoms of dysphagia and was then referred to the ENT Department. The medical history revealed controlled hypertension and bronchial asthma but no personal nor family cases of goitres or thyroiditis.
Clinical examination found a firm mass in front of the larynx, slightly deviated to the left and mobile superiorly with swallowing, but not with tongue protrusion. No cervical lymph nodes were palpated, and no thyroid gland enlargement was noticed. Flexible endoscopy of the larynx and hypopharynx was within normal findings.
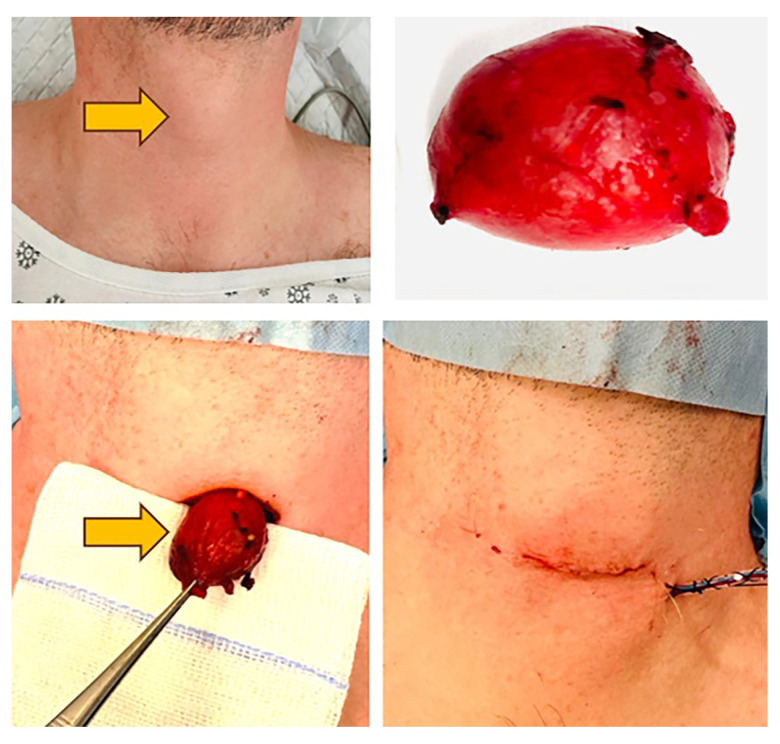
Cervical ultrasound (Figure 1) revealed a subcutaneous well-defined mass at the anterior part of the neck, slightly hypoechoic, measuring 62×33×19 mm, and with mixed vascularity on Doppler. The thyroid gland was in place, enlarged in size, and showing multiple nodules on both sides, variable in size but less than 5 mm. No enlarged cervical lymph nodes were noted.
Figure 1.
Neck ultrasound showing subcutaneous well-defined mass at the anterior part of the neck.
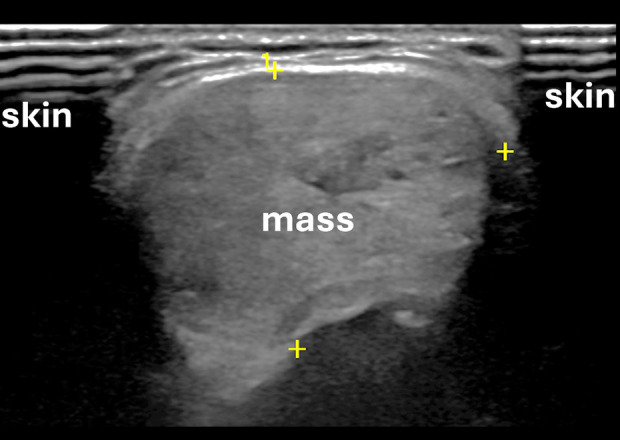
A computed tomography (CT) scan of the neck with contrast (Figure 2) showed a well-defined anterior midline heterogeneous mass with avid enhancement after intravenous contrast injection. The mass measured 62×25×22 mm and was just attached to the subcutaneous soft tissues in front of the larynx, without obvious connections to the thyroid or to the cervical blood vessels. No other masses or significant abnormal findings were reported by the radiologist. Considering the above clinical data and investigations, no clear diagnosis could be assessed, and we suspected that the mass could be derived from the larynx, lymph nodes, or subcutaneous soft tissues.
Figure 2.
Axial neck computed tomography showing a well-defined anterior midline heterogenous mass (A) with avid enhancement after intravenous contrast injection (B). The thyroid gland was in place (C).
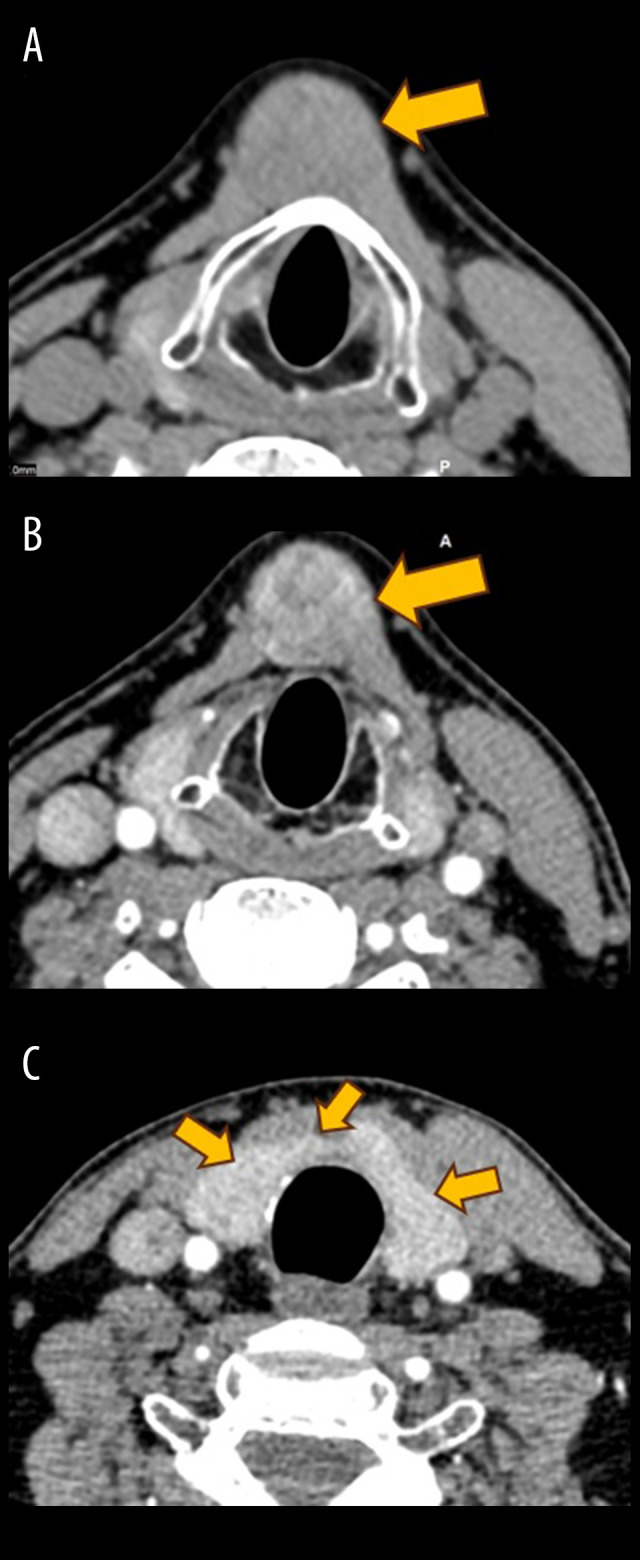
An open surgical excision of the mass was performed under general anaesthesia through a horizontal infrahyoid approach (Figure 3). The mass was just below the subcutaneous tissues of the anterior part of the neck in front of the larynx. It was a well-encapsulated mass, reddish in color, without connections to the adjacent structures, except to the fatty tissues in front of the thyroid cartilage of the larynx. A drainage was kept in place and removed after 24 h, just before the patient’s discharge from the hospital.
Figure 3.
Surgical mass excision.
Histopathological examination of the specimen (Figure 4) identified a well-encapsulated thyroid tissue with variable-sized follicles and foci of hyperplasia, hemorrhage, and fibrosis. No atypical or malignant cells were seen in examined sections.
Figure 4.
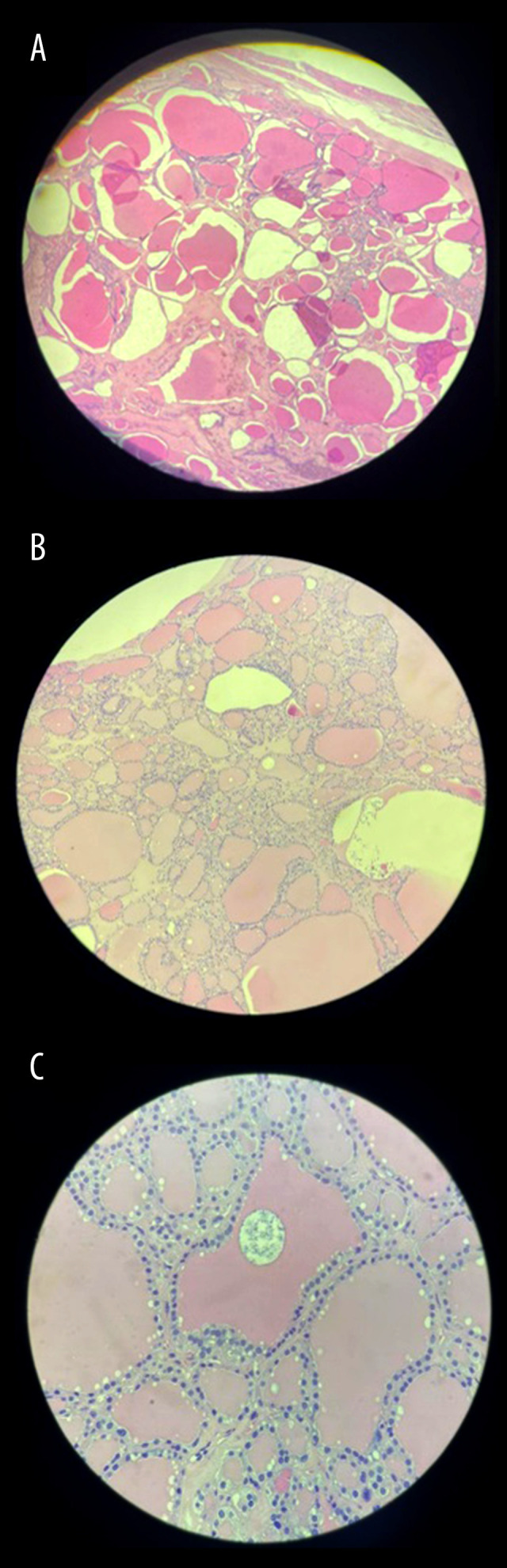
Microscopic picture of the tissue: (A) at 2× magnification showing well-circumscribed capsulated thyroid nodule; (B) at 10× magnification showing bland thyroid follicles filled with colloid; and (C) at 20× magnification showing bland thyroid follicular cells, with absence of malignancy.
The postoperative monitoring of the patient noted an appropriate healing of the surgical scar and the disappearance of the dysphagia reported before the surgery. Thyroid nodules remained stable in size after a follow-up of 9 months, and the regular thyroid hormones tests were within normal limits, comparable to the normal levels of the thyroid-stimulating hormone found preoperatively.
Informed Consent
A written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Discussion
Ectopic thyroid nodules can become goitrous and be associated with clinically evident thyroid dysfunction, which could be either hypofunction or hyperfunction [5]. The ectopic thyroid tissue is subject to malignant transformation and can be accompanied by similar features in the eutopic gland or not [7,10].
Thus, tissue sample analysis is required to rule out this possibility [8]. Papillary, follicular, mixed, and medullary carcinomas have been reported [11,12]. Rarely, malignant ectopic tumors can present with metastasis to lymph nodes. Ectopic thyroid tissues located laterally in the neck were initially thought to be metastatic lymphadenopathies of thyroid neoplasms, but most of those masses were benign at the histopathology assessment [6]. No symptoms are associated with ectopic thyroid nodules in most of the cases, and some cases were discovered accidentally, when radiology examinations for other chest and neck diseases were being performed [2,10,13]. In symptomatic cases, the symptoms are either related to the pressure of the surrounding organs by the nodule or to a hormonal thyroid disturbance [3,4].
The main symptoms reported in cases of large nodules are swelling, hoarseness of voice, difficulty swallowing, dry cough, and, rarely, shortness of breath [5,8,9]. Only massive nodules can cause trachea or larynx obstruction and abnormal breathing sounds [4,14], while one-third of the patients have evidence of hypothyroidism. Sleep apnea and respiratory obstruction in adult patients with lingual thyroid have been reported [6]. The differential diagnosis of ectopic thyroid nodules depends on the location and the findings of radiology, lymph node enlargement, congenital cysts, other cutaneous cysts, and tumors and metastasis [2,5]. On the lateral side of the neck, many other diagnoses should be discussed, such as salivary gland enlargements and neoplasms or reactive and metastatic lymph node enlargements [10,14].
In patients presenting with chronic neck masses, high resolution ultrasound is the preferred first investigation to be requested. It is known to be noninvasive, cost-effective, and without radiation exposure for the patient, and allows to confirm that a thyroid gland is well-located at its normal position [12]. The accuracy of the examination is improved using the color Doppler technique, analyzing the vascular flow of the mass. Ultrasound findings might be suspect for the malignancy of a mass when it shows signs of hypoechogenicity, irregular borders, microcalcifications, and increased vascularity on Doppler [2,6].
Radionuclide imaging using technetium-99m pertechnetate, iodine-131, or iodine 123 is useful in the evaluation of ectopic thyroid [4,12]. Thyroid tissue takes up the radioisotope, and this helps in localizing the ectopic thyroid and, at the same time, in determining the presence of a eutopic thyroid gland [11]. Technetium-99 pertechnetate offers better quality imaging and delivers lower body radiation than does iodine-131 [8]. At the same time, the disadvantage of technetium-99 pertechnetate is that it is not specific to the ectopic thyroid tissue but can spread to the surrounding areas, reducing its accuracy in the detection of tiny nodules. Iodine-123 has been described mainly among the pediatric population, even if it is less available in most centers because of its high cost [6,13]. Scintigraphy coupled with CT is a reliable and valuable tool to diagnose ectopic thyroid masses, as it combines the accuracy of CT in precisely identifying the shape, density, and size of the mass to the advantages of scintigraphy, which provides information about the structure, position, and function of the thyroid tissue [4,8,11].
CT scanning and magnetic resonance imaging (MRI) are very efficient examinations, especially if a contrast agent is injected [3,9,15]. When the ultrasound does not show a normal thyroid gland in place, CT and MRI are much more important diagnostic tools, and their contribution is valuable [4]. The usual description of the ectopic thyroid nodule is a high-attenuated mass on non-contrast CT, and high T1 and T2 mass on MRI, in contrast with the muscle [2,5]. MRI is less irradiating than CT and is very helpful, especially when it comes to differentiating the ectopic thyroid nodules from surrounding soft tissues and organs. Its major inconvenience is still the high cost, which limits its use and availability in many centers, and some difficulties in patients with claustrophobia, who do not tolerate the examination. Arteriography and some techniques of embolization before surgery have been described by some authors as an important step in the diagnostic and pre-surgical process for a better characterization of the mass and reduction of bleeding during surgery, especially for some specific locations at surgical risk [3,6,13,14].
When available, fine needle aspiration cytology (FNAC) is an important diagnostic tool of chronic neck masses and strongly predicts the nature of the mass and the possible existence of malignancy [5,12]. The issue is to collaborate only with a trained cytologist to maximize the efficiency of the examination and to reduce the rate of false-negative cases [11].
The management of ectopic thyroid tissue depends on the clinical presentation. Asymptomatic euthyroid patients do not usually require therapy but are kept under observation. For those with symptoms, treatment depends on the gland dimensions, nature of symptoms, thyroid function status, and histological findings [2]. Paucisymptomatic patients with normal thyroid function can be treated by exogenous thyroid hormone to reduce the size of the ectopic tissue gradually. However, the efficiency of this method is not guaranteed, and the time required to get a notable reduction in the size of the mass cannot be predicted [6]. Surgery is still the main treatment option, especially when serious compressive signs are noted to result in alteration of breathing, speech function, or swallowing. Surgery is also required in cases of an enlarged obvious mass or suspicion of neoplastic transformation [12,15]. Before the surgery of the ectopic thyroid nodule, we must ensure the presence of a normally located gland in order to avoid any risk of hypothyroidism [13]. The ectopic gland may be the only functional thyroid, and complete excision is followed by lifelong hormone replacement. Procedures described to retain some degree of thyroid function in the patients are the transposition of the ectopic thyroid, with a vascular pedicle flap into the muscle space at the floor of the mouth [6]. Ectopic nodules located on the cervical areas are usually superficial, and the swelling is rapidly symptomatic, with signs of surrounding organ irritation. Surgery is usually indicated in those patients to relieve the patient’s symptoms and rule out any malignancy [12]. Depending on its location, many external or endoscopic approaches have been described to remove the ectopic gland, depending on the availability of equipment, characteristics of the mass, and skills of the surgeon. Intrathoracic ectopic goitres usually require thoracotomy or sternotomy [6,15], and a team combining otolaryngologists and cardiothoracic surgeons is the best solution in this case, to get a better exposure of the gland and to minimize perioperative complications. Robotic excision of some thoracic ectopic goitres was also reported in the literature [2,12]. Radioactive iodine-131 cures have been also described for patients who are not fit for invasive procedures, those who refuse operation, and where surgical resection is not feasible due to anatomical difficulties. It is contraindicated in pregnant women and avoided in younger pediatric patients [2,6]. When the diagnosis of ectopic goitre is assessed before surgery, and the patient is with hyperthyroidism, the intervention is conducted after ensuring an euthyroid state by using drugs, such as methimazole or iodine [4,13].
When FNAC is performed for an ectopic thyroid tissue, the cytological findings can be very helpful to assess the nature of the mass and plan the surgery accordingly [6,7]. However, the final confirmation always requires a tissue biopsy for histology, especially in case of suspicion of neoplasms [7]. Unfortunately, in our center, we do not have a cytologist that can help us in this regard. Thus, a FNAC was not attempted before surgery.
The biopsy can be performed by an endoscopic approach in case of endoluminal locations, or through an external surgical resection, especially when the ectopic thyroid tissue lies on the cervical area [13]. When the presence of an ectopic thyroid tissue is assessed after the excision of a chronic cervical mass, further investigations are requested to confirm the presence of a normally located gland and to rule out any hormonal dysfunction following the removal of the ectopic gland. The ultimate management will depend on the outcome of those investigations [6].
Regular follow-up after surgery is required to detect changes in the thyroid function or any recurrence of the disease [5,7]. Long-term monitoring is also required, as delayed recurrences of ectopic thyroid tissue enlargements can be present [2].
Conclusions
Ectopic thyroid tissue remains a rare disease, and most of the cases are asymptomatic. However, when obstructive symptoms occur because of gland enlargement, radiological and biological tests are required to characterize the mass, confirm the presence of a eutopic gland, and assess thyroid function. Different surgical procedures have been described according to the location of the ectopic gland, and histopathology assessment is the unique way to confirm the diagnosis and rule out any transformation.
Acknowledgments
We gratefully acknowledge the valuable contribution and support provided by the Continuing Professional Development Committee of West Bay Medicare Hospital for the guidance and the peer review of this manuscript.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Rosen RD, Sapra A. StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2023. Embryology, thyroid. [Updated 2023 May 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551611/ [PubMed] [Google Scholar]
- 2.Wang J, Fang J. Ectopic thyroid mass in the left lateral neck and anterior mediastinum: A case report. J Med Case Rep. 2014;8:351. doi: 10.1186/1752-1947-8-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sato D, Hayashi S, Sakata S, et al. Intrapericardial ectopic goiter: A very unusual presentation. Ann Thorac Cardiovasc Surg. 2022;28:72–74. doi: 10.5761/atcs.cr.19-00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nistor C, Ciuche A, Motaş C, et al. Cervico-mediastinal thyroid masses – our experience. Chirurgia (Bucur) 2014;109(1):34–43. [PubMed] [Google Scholar]
- 5.Kola E, Gjata A, Kola I, et al. Ectopic thyroid tissue in the anterior mediastinum along with a normally located gland. Radiol Case Rep. 2021;16(11):3191–95. doi: 10.1016/j.radcr.2021.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ibrahim NA, Fadeyibi IO. Ectopic thyroid: Etiology, pathology and management. Hormones. 2011;10(4):261–69. doi: 10.14310/horm.2002.1317. [DOI] [PubMed] [Google Scholar]
- 7.Kola E, Musa J, Guy A, et al. Ectopic thyroid papillary carcinoma with cervical lymph node metastasis as the initial presentation, accompanied by benign thyroid gland. Med Arch. 2021;75(2):154–57. doi: 10.5455/medarh.2021.75.154-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagireddy TV, Vaidya AA, Gupta S, et al. A rare case of double ectopic thyroid in the superior mediastinum: A case report. J Surg Case Rep. 2023;2023(2) doi: 10.1093/jscr/rjad058. rjad058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metere A, De Giacomo T, Vergine M, et al. Diagnosis and management of a mediastinal ectopic thyroid laying on the right bronchus: Case report and review of literature. BMC Surg. 2018;18(1):19. doi: 10.1186/s12893-018-0354-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nambiar G, Eshwarappa H, Kini H, Chidanand D. Isolated thyroid carcinoma in an ectopic thyroid tissue. BMJ Case Rep. 2021;14(2):e239738. doi: 10.1136/bcr-2020-239738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carsote M, Ciobica ML, Sima OC, et al. personalized management of malignant and non-malignant ectopic mediastinal thyroid: a proposed 10-item algorithm approach. Cancers. 2024;16(10):1868. doi: 10.3390/cancers16101868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melinte A, Saftoiu A, Vlaicu-Melinte A, et al. Robotic resection of ectopic thyroid tissue of the mediastinum – case report and literature review. Chirurgia. 2023;118(1):96–102. doi: 10.21614/chirurgia.2832. [DOI] [PubMed] [Google Scholar]
- 13.Hummel J, Wachsmann J, Carrick K, et al. Ectopic thyroid tissue in the mediastinum characterized by histology and functional imaging with I-123 SPECT/CT. Case Rep Radiol. 2017;2017:9084207. doi: 10.1155/2017/9084207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bianchi D, Scamporlino A, Costantini M, et al. A case of cervico-mediastinal paraganglioma mimicking an ectopic goiter. Int J Surg Case Rep. 2021;86:106357. doi: 10.1016/j.ijscr.2021.106357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Crescenzo V, Vitale M, Valvano L, et al. Surgical management of cervico-mediastinal goiters: Our experience and review of the literature. Int J Surg. 2016;28(Suppl. 1):S47–53. doi: 10.1016/j.ijsu.2015.12.048. [DOI] [PubMed] [Google Scholar]