Abstract
Household food insecurity (HFI) has been related to adverse maternal‐child health outcomes and mental health worsening during pregnancy. Few studies evaluated the temporal association between HFI and anxiety and depressive symptoms in pregnant women, and this association remains not completely understood. This study aimed to systematically review the association between HFI and symptoms of depression and anxiety in pregnant individuals. The systematic review protocol was registered in the International Prospective Register of Systematic Reviews (CRD42022373615). Systematic searches were conducted on 10 electronic databases and grey literature. Two researchers independently conducted the study selection, data extraction process, and the risk of bias assessment. Random‐effects meta‐analysis models were used, and I2 > 40% indicated high heterogeneity across studies. Eighteen articles were included for the systematic review, comprising n = 27,882, and a total of 18,987 pregnant individuals aged between 14 and 45 years were included in the meta‐analysis. The prevalence of HFI reported in studies ranged from 12.6% to 62.1% (n = 17). The prevalence of depressive and anxiety symptoms ranged from 18% to 49% (n = 11) and 23% to 34% (n = 2), respectively. HFI during pregnancy was associated with increased odds of experiencing symptoms of depression [(OR: 2.52; 95% CI: 2.11–3.02), I2 = 73.23%]. The quality of evidence was very low due to high heterogeneity. Our findings highlighted the association between HFI and depression symptoms during pregnancy. Findings from this study suggest the importance of assessing HFI and mental health during pregnancy.
Keywords: anxiety, depression, household food insecurity, pregnancy
This study aimed to systematically review the association between HFI and symptoms of depression and anxiety in pregnant individuals. The systematic review protocol was conducted according to PRISMA. Eighteen articles were included in the systematic review and 18,987 pregnant individuals aged between 14 and 45 years old were included in the meta‐analysis. The prevalence of HFI reported in studies ranged from 12.6% to 62.1%. The depressive and anxiety symptoms ranged from 18% to 49%, and 23% to 34%, respectively. The HFI during pregnancy was associated with increased odds of experiencing symptoms of depression [(OR: 2.52; 95% CI: 2.11–3.02), I2 = 73.23%].
Key messages
Increased anxiety and depressive symptoms frequently manifest in households with lower income levels, highlighting a notable correlation between socioeconomic status and mental health challenges.
Household food insecurity (HFI) is associated with increased odds of experiencing depressive symptoms during pregnancy, presenting the intricate relationship between insufficient access to food resources and the exacerbation of mental health issues during pregnancy.
Improving public policies focused on ensuring food security for pregnant individuals holds the potential to enhance positive psycho‐emotional health outcomes during pregnancy.
1. INTRODUCTION
Maternal health during pregnancy is essential during foetal development, with lasting implications for the child's health, growth and development. There is a growing acknowledgement that the development of future generations should begin at preconception and continue throughout pregnancy. Aligned with the Sustainable Development Goals (SDGs), these initiatives underscore the importance of investing in early life to achieve the health, wellbeing, and human capital development of next generations (Black et al., 2021).
Several psychological and social changes are experienced during pregnancy (Hill et al., 2020; Lockitch, 2008; Soma‐Pillay et al., 2016), such as genetic factors, previous history of mental disorders, pregnancy‐related stress and anxiety, traumatic events, and lack of social and family support, and those may give rise to adverse mental health outcomes during pregnancy (Ayyub et al., 2018; Bedaso et al., 2021; Hromi‐Fiedler et al., 2011). The low‐income status and household food insecurity (HFI) may be considered psychosocial stressors, which are associated with worsening mental health in pregnant women (Abrahams et al., 2018; Hromi‐Fiedler et al., 2011; Izano et al., 2020; Khoshgoo et al., 2020).
HFI refers to the condition in which a home or family faces restrictions without access to adequate and nutritious food to meet the dietary needs of all family members (FAO, 2023b). About 30% of the population globally are facing the highest levels of HFI in 2022 (FAO, 2023a). It is important to note that the global prevalence of moderate or severe HFI was higher among women, with 27.8% of women facing moderate or severe HFI while 25.4% of men in the same situation (FAO, 2023a). HFI during pregnancy is an important factor to be investigated because poor access to food leads to a high intake of processed food, rich in energy density but poor in nutrients. This type of food is associated with increased chances of malnutrition, overweight, and obesity (FAO, 2020), excessive and inadequate weight gain (Arzhang et al., 2022; Biltoft‐Jensen et al., 2022; FAO, 2020), and inadequate baby outcomes such as growth deficits at birth (Karbin et al., 2022). Recent articles show that HFI is associated with symptoms of depression and anxiety during pregnancy (Khoshgoo et al., 2020; van Heyningen et al., 2017). Depression is characterised by depressive mood, in which the individual presents sadness, irritability, a feeling of emptiness, and loss of pleasure, accompanied by other symptoms. Anxiety is characterised as fear and external anxieties related to behavioural disorders, presenting serious symptoms that result in losses in the personal, family, social, educational, and occupational spheres (World Health Organisation, 2023). It is emphasised that during pregnancy, women undergo significant physiological and social changes that may play a role in the development of depressive symptoms (Mazza et al., 2023).
Studies have reported the association between symptoms of depression in pregnant women and HFI (Abrahams et al., 2022; Abrahams & Lund, 2022). It is important to emphasise that the COVID‐19 pandemic has led to an increase in poverty, food and nutritional insecurity, and a worsening of health outcomes. In this context, families with children and pregnant individuals require support and protection to ensure food security for all (Pérez‐Escamilla et al., 2020).
Recent evidence suggests that HFI is related to adverse mental health outcomes (Abrahams et al., 2018; Ayyub et al., 2018; Hromi‐Fiedler et al., 2011; Laraia et al., 2015), but the investigation of symptoms of depression and anxiety in pregnant women has not been evaluated through a systematic review. Elucidating the relationship between HFI and maternal depression and anxiety is important to develop public policy and practice‐based interventions aimed at optimising women's mental health and ensuring the correct development of pregnancy. The aim of this study is to conduct a systematic review to evaluate the association between HFI and symptoms of depression and anxiety during pregnancy.
2. METHODS
2.1. Registration and protocol
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist 2020 (Page et al., 2021) (Appendix S1). The systematic review was registered in the international Prospective Register of Systematic Reviews (PROSPERO) (CRD42022373615). The Population, Exposure, Comparison, Outcome, and Study design was used to elaborate the guiding study question as follows: ‘Is there an association between HFI and symptoms of depression and anxiety in pregnant women?’
2.2. Eligibility criteria
The inclusion criteria for this review were studies that evaluated pregnant women of any age and observational studies, with no restrictions on language, country, or publication date published in indexed and grey literature. The exclusion criteria were reviews or qualitative studies, abstracts or book chapters, and studies focused on pregnant women with pre‐existing comorbidities.
2.3. Exposure
The key exposure was the HFI measured by validated instruments or surveys. Food insufficiency and maternal hunger were characterised as severe HFI considering the United States Department of Agriculture Questions to assess Food Security Status during pregnancy in the Maternal Infant Health Assessment Survey (Blumberg et al., 1999; Coleman‐Jensen, 2010). The highest level of HFI was included in the meta‐analysis when selected studies categorised the different levels of food insecurity. Eligible studies that did not report adequate data for meta‐analysis were qualitatively assessed during the systematic review.
2.4. Outcome
The outcomes examined in this systematic review encompassed symptoms of depression and anxiety, which were measured by studies using various assessment instruments.
2.5. Search strategy
The searches were performed on 29 May 2023, and updated on 27 November 2023, in the following databases: Medline, Scopus, Embase, Web of Science, PsycINFO, Scielo, Lilacs, and BVS. Furthermore, grey literature studies that met the eligibility criteria established in this review were performed using ProQuest Dissertations and Theses Global and Google Scholar (limited to the first 200 most relevant results) (Pizato et al., 2017). Also, reference lists of selected articles were manually searched to identify studies that had not been retrieved from the databases. Missing data or not being available in full text were sought via e‐mail to the corresponding authors. Records were downloaded to a Microsoft Excel spreadsheet, added to a standardised data collection form, and duplicates were removed using Mendeley® software. Rayyan® software was used to check possible duplicate references and to triage potentially eligible studies.
The primary approach involved the utilisation of the following terms and Boolean operators: (pregnancy OR pregnancies OR gestate OR gestated OR gestates OR gestating OR gestational OR gestations OR pregnant OR 'pregnant woman' OR 'pregnant women' OR 'woman pregnant' OR 'women pregnant' OR maternally OR maternities OR maternity OR mothers OR mother OR maternal OR antenatal OR antenatally OR 'maternal exposure') AND ('food insecurity' OR 'food insecurities' OR 'insecurity food' OR 'food rationing' OR 'rationing food' OR 'nutrition insecurity' OR 'food and nutrition insecurity' OR 'food and nutrition insecurity' OR 'food supply' OR 'food supplies' OR 'supplies food' OR 'supply food' OR 'food security' OR 'security food' OR 'food insecurity scale' OR 'household food insecurity measurement scale' OR 'food insufficiency') AND (depressed OR depression OR depressions OR 'depressive disorder' OR depressively OR depressive OR depressiveness OR depressives OR 'depressive symptoms' OR 'depressive symptom' OR 'symptom depressive' OR 'symptoms depressive' OR 'emotional depression' OR 'depression emotional' OR 'health mental' OR 'mental health' OR 'depressive disorders' OR anxiety OR anxieties OR anxiousness OR nervousness OR 'social anxieties' OR 'anxiety social' OR stress OR stressed OR stresses OR stressful OR stressfulness OR stressing OR 'psychological distress' OR 'mental ill‐health' OR 'antepartum depression' OR 'prenatal depression' OR 'prenatal anxiety' OR 'common mental disorder'). The search strategy for the systematic review was reviewed by a researcher with extensive experience in conducting systematic reviews according to the Peer Review of Electronic Search Strategies (PRESS checklist) (McGowan et al., 2016). Search strategies are detailed in Appendix S1.
2.6. Studies selection
The duplicates were identified and removed using the reference management tool Mendeley Desktop (version 1.19.8), and the Rayyan QCRI software (Qatar Computing Research Institute®, Doha, Qatar) was used to screen articles. The study selection process was carried out in two steps. First, two researchers independently (C.B. and A.B.) screened the abstracts and the titles of all citations in the databases. Those that did not meet the delimited inclusion criteria were excluded. Then, the selected potentially eligible studies were submitted for full‐text analysis by two researchers (C.B and A.B), and those articles that met the eligibility criteria were included in the review. Divergences about the eligibility of the articles were resolved by consensus.
2.7. Data extraction
The data were extracted by one author (C.B) and cross‐checked by the second author (A.B) using a standardised spreadsheet, including the author's name, year of study, year of publication, country, study design, place of data collection, age of the pregnant women, sample size, gestational age, HFI, depression, and anxiety scale, measures of effect size with confidence interval (CI).
Different instruments were identified in the included studies to evaluate HFI. Most instruments were originally conceived in English and held dichotomous responses, resulting in cutoff points or evaluations by ordinal scales. The instruments are detailed in Table 1 and presented cutoff points to characterise household food insecurity and symptoms of anxiety and depression. Therefore, the characterisation of HFI and symptoms of anxiety and depression in this review considered the cutoff point determined in each study.
Table 1.
Summary of included studies’ characteristics.
| First author, year | Country | Study Design | Age (range or mean) | Gestational age (range or mean) | Sample size (n) | Exposure | Measure of exposure | Cut‐off exposure | Outcome | Measure of Outcome | Cut‐off outcome | Main Results | Adjusted Variables |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ayyub et al., (2018) | Pakistan | Cross‐sectional | 18 to 45 | 1st, 2nd and 3rd Trimester | 367 | Household food insecurity | Household food insecurity access scale (HFIAS) | NR | Depression | Edinburgh Postnatal Depression Scale (EPDS) | Cut‐off score depression ≥12 | Food insecurity increases the odds of antenatal depression (OR 2.96; 95% CI 1.920–4.570; AOR 2.58; 95% CI 1.641–4.075) | Adjusted for unwanted pregnancy |
| Dias et al., (2011) | Brazil | Cross‐sectional | 25.1 (6.7) | 1st, 2nd and 3rd Trimester | 94 | Household food insecurity | Brazilian Food Insecurity Scale (EBIA) | NR | Anxiety and depression |
Hamilton Anxiety Scale: HAMA Beck Depression Inventory: (BDI) |
NR Cut‐off score depression ≥10 |
Food insecurity variable (overall score) related to HAMA (p = 0.00; r = 0.508) and BDI (p = 0.00; r = 0.445) | NR |
| Dibaba et al., (2013) | Ethiopia | Cross‐sectional | 15 to >35 | 2nd and 3rd Trimester | 627 | Household food insecurity | Household food insecurity was measured with a six‐item scale based on previously validated measures in developing countries. | Two or more of the six household food security questions. | Depression | Edinburgh Postnatal Depression Scale (EPDS) | Cut‐off score depression ≥13 |
Food insecurity x Depressed mood (OR: 6.79; 95% CI: 4.31–10.72)* (AOR: 4.60; 95% CI: 2.75–7.70)* *p < 0.001 |
Adjusted for education, wealth tertile, occupation, perceived work burden, food security status, history of miscarriage of still birth and partner physical violence during pregnancy |
| Doglikuu et al., (2023) | Ghana | Cross‐sectional | 10 to 20 | NR | 225 | Household food insecurity | Household Food Insecurity Access Scale (HFIAS) | NR | Depression | Revised Children's Anxiety and Depression Scale (RCADS‐25) | NR |
High food Insecurity x High Depression (OR: 0.43; 95% CI: 0.17–1.11; p 0.082 AOR: 0.27; 95% CI: 0.11–0.71 p 0.008) |
Adjusted for education level, and parental occupation |
| Eick et al., (2020) | USA | Prospective cohort | 32 (5.4) | 2nd Trimester | 510 | Household food insecurity | Questionnaires designed psychosocial stress, work‐related stress, and the physical environment. | NR | Depression | Center for Epidemiologic Studies‐Depression (CES‐D) | NR | Strong correlation between food insecurity x depression (point biserial r = 0,65) | NR |
| Grilo et al., (2015) | USA | Cross‐sectional | 18.6 (1.7) | 2nd and 3rd Trimester | 881 | Household food insecurity | Questionnaire developed by the State of California Health and Human Services Agency, WIC Supplemental Nutrition Branch. | If participants answered 'no' during both the second and third trimesters of pregnancy, they were considered Food Secure. If they answered 'yes' at one time point, they were considered Acute Food Insecure and if they answered 'yes' at both time points, they were considered Chronic Food Insecure. | Anxiety and depression |
Generalised Anxiety Disorder Scale (GAD‐7) Center for Epidemiologic Studies‐Depression (CES‐D) |
NR Cut‐off score depression ≥16 |
Path Model Acute Food Insecurity x depressive symptoms 1.21 (0.55)* Acute Food Insecurity x anxiety 1.27 (0.56)* Chorinic Food Insecurity x Depressive Symptoms 4.01 (0.69)** Chorinic Food Insecurity x Anxiety 1.73 (0.52)** **p ≤ 0.001, *p ≤ 05 |
Analysis controlled for the effects of intervention, pre‐pregnancy BMI, mother's age, born outside the US, financial support, living situation, housing insecurity, smoking during pregnancy, and drinking during pregnancy on all mediators and birth outcomes. |
| Gross et al., (2018) | USA | Prospective cohort | >18 years | 2nd and 3rd Trimester | 410 | Household food insecurity | Food Security Module from the United States Department of Agriculture | Women were classified as food secure if they reported 2 or less food insecure conditions and food insecure if they reported 3 or more. | Depression | Patient Health Questionnaire (PHQ‐9) | Cut‐off score depression ≥5 | Food insecurity increases the odds of prenatal depressive symptoms (OR: 2.96; 95% CI: 1.91–4.59) | NR |
| Harrison et al., (2008) | USA | Cross‐sectional | 17 to >30 | NR | 1386 | Household food insecurity | Food Security Scale of the U.S. | Each of the 4 items retained is scored 0–2. A total of 6–8 points is scored as High Risk; a score of 3–5 is scored as Moderate Risk. | Depression | Patient Health Questionnaire (PHQ‐9) | Cut‐off score depression ≥10 | Food Insecurity is correlated to depression (Pearson correlation coefficient = 0.267*, *p < 0.0001) | NR |
| van Heyningen et al., (2017) | South Africa | Cross‐sectional | mean age 27 years; SD 5.8 | 1st, 2nd and 3rd Trimester | 376 | Household food insecurity | US Household Food Security Survey Module (HFSSM) | NR | Anxiety | Mini‐International Neuropsychiatric Interview (MINI Plus) | NR |
Meets criteria for food insecurity x diagnosis with any anxiety disorder (OR 2.49 CI 95% 1.52–4.08 p ≤ 0.001) Meets criteria for food insufficiency x diagnosis with any anxiety disorder (OR 2.91 CI 95% 1.56–5.43 p 0.001) |
NR |
| Khoshgoo et al., (2020) | Iran | Cross‐sectional | 28.59 ± 7.28 | 1st, 2nd and 3rd Trimester | 394 | Household food insecurity | Persian version of the Household Food Security Survey Module (HFSSM) |
Households without children under 18 years (total score: 10 points) Food secure (0–2) Food insecure without hunger (3–5) Food insecure with moderate hunger (6–8) Food insecure with severe hunger (9–10) Households with children under 18 years (total score: 18 points) Food secure (0–2) Food insecure without hunger (3–7) Food insecure with moderate hunger (8–12) Food insecure with severe hunger (13–18) |
Depression | Persian version of the Beck Depressive Inventory‐II (BDI‐II) questionnaire | Cut‐off score depression ≥14 | Household food insecurity increases the odds of antenatal depression (OR 4.08; 95% CI 2.65–6.30; p < 0.05; AOR 3.31; 95% CI 2.07–5.29; p < 0.05) | NR |
| Laraia et al., (2006) | USA | Cross‐sectional | 27.2 ± 5.6 | Before 20 wk gestation | 606 | Anxiety and Depression |
Spielberger's Trait Anxiety Inventory Center for Epidemiologic Studies Depression (CES‐D) |
NR Cut off score ≥30 |
Household food insecurity | USDA food security module | It was defined a household as 'marginally food secure' if 1 or 2 questions were answered in the affirmative. It was defined a household as food insecure (with or without hunger) if ≥3 questions were answered in the affirmative. |
Trait anxiety score increases the odds of Food insecurity (AOR 2.14; 95% CI 1.55–2.96) Depression symptoms score increases the odds of food insecurity (AOR 1.87; 95% CI 1.40–2.51) |
Adjusted for income, race, education, marital status, age and number of children |
| Laraia et al., (2022) | USA | Cross‐sectional | 15 to >35 | NR | 14274 | Household food insecurity | Security scale developed by the United States Department of Agriculture | More than one affirmative response indicated food insecurity, further defined as low food security (2–4 affirmative responses) or very low food security (5–6 affirmative responses) | Depression | NR | NR | OR 2.784; 95% CI 2.574–3.012 | NR |
| Mak (2019) | Canada | Cross‐sectional | 18 to 49 | NR | 4817 | Household food insecurity | U.S. Household Food Security Survey Module (HFSSM) |
Food‐secure: No items affirmed Marginally food‐insecure: 1 item affirmed Moderate‐severely food‐insecure: 2–10 items affirmed |
Diagnosis of anxiety disorder Diagnosed mood disorder (depression, bipolar disorder, mania or dysthymia) |
Interview in which the interviewee should report disorders if they were diagnosed by a health professional and lasted or is expected to last for 6‐months or longer. | NR |
Diagnosed anxiety disorder and Mod‐Sev Food Insecure: (AOR 3.2; 95% CI 1.92–5.43; p <0.001 Diagnosed mood disorder and Mod‐Sev Food Insecure: AOR 4.82; 95% CI 2.80–8.28; p < 0.001 |
Adjusted for household income, age, postsecondary education, indigeneity, 2‐year cycle |
| Matlwa et al., (2021) | South Africa | Cross‐sectional | NR | NR | 584 | Maternal hunger | Telephonic survey provided more detail on hunger. | At least 1 day reported going to bed hungry | Depression | Patient Health Questionnaire ‐9 (PHQ‐9) | Cut‐off score depression ≥10 | Respondents who reported they had gone to bed hungry at least once in the seven nights preceding the survey were twice as likely (OR 2.17; 95% CI 1.51–3.13; p < 0.05) to report high symptomatology on the Phq‐9 (score ≥10) | NR |
| Oladeji et al., (2022) | Nigeria | Cross‐sectional | 14 to 20 | Gestational age (mean [sd]): 23.78 (5.36) | 1359 | Household food insecurity | Food insecurity was defined as the number of days the respondent had gone to bed hungry in the previous 7 days because there was no food to eat. The type of instrument used was not reported. | At least 1 day reported going to bed hungry | Depression | Edinburg Postnatal Depression (EPDS) | Cut‐off score depression ≥12 |
A day or more gone bed with hungry x depression OR (95% CI) 2.82 (1.96, 4.05), p < 0.001 |
NR |
| Pobee et al., (2022) | Gana | Prospective cohort | 27.1 ± 5.2 years | 1st, 2nd and 3rd Trimester | 116 | Household food insecurity | US Household Food Security Survey Module | NR | Anxiety and depression |
Beck Anxiety Inventory (BAI) Center for Epidemiologic Studies‐Depression (CES‐D) |
Cut‐off score anxiety ≥14 Cut‐off score depression ≥10 |
Generalised Estimating Equation (GEE) model Depressive symptoms x Food insecurity: 0.594 (0.428, 0.761), p < 0.001 Total Anxiety symptoms x Food insecurity: 0.619 (0.389, 0.849), p < 0.001 |
NR |
| Sidebottom et al., (2014) | USA | Prospective cohort | <25 and > 25 | NR | 87 | Household food insecurity | Food Security Scale of the U.S. | It was created a summary score and classified a score between 0 and 2 as low risk and between 3 and 8 points as moderate/high risk. | Depression | Patient Health Questionnaire (PHQ‐9) | Cut‐off score depression ≥10 |
Food insecurity Moderate/high x depressive symptom levels (OR 2.44; 95% CI 1.43, 4.16, p 0.001) |
NR |
| Tsai et al., (2016) | South Africa | Prospective cohort | NR | NR | 769 | Food insufficiency | Food insufficiency was measured using a single‐item question, 'How many days in the past week have you gone hungry?' | At least 1 day reported hungry | Depression | Xhosa version of Edinburgh Postnatal Depression Scale (EPDS) | Cut‐off score depression ≥13 |
Hungry days and EPDS case: AOR 1.74; z 3.31; p > z 0.001; 95% CI 1.25–2.43 |
NR |
Abbreviations: AOR, Adjusted Odds Ratio; OR, Crude Odds Ratio; NR, Not reported.
2.8. Assessment of methodological quality
Two researchers evaluated The risk of bias independently, using the checklist for critical appraisal of cohort and cross‐sectional studies developed by the Joanna Briggs Institute (JBI) (Aromataris, 2020) as a reference. The cross‐sectional studies checklist comprises eight questions, and the cohort studies checklist consists of 11 questions. These tools consist of questions answered as 'yes', 'no', 'unclear', or 'not applicable'. The questions are described in Figure 2. The studies were classified as low risk of bias when presented one 'yes' as a response to all items on the checklist, while studies with high risk of bias were those that presented at least one 'no' or 'unclear' item on the checklist. Notably, the risk of bias analysis was not used as a criterion for the exclusion of the article. However, it enabled the evaluation and discussion regarding the heterogeneity of the studies included in the review and meta‐analysis.
Figure 2.
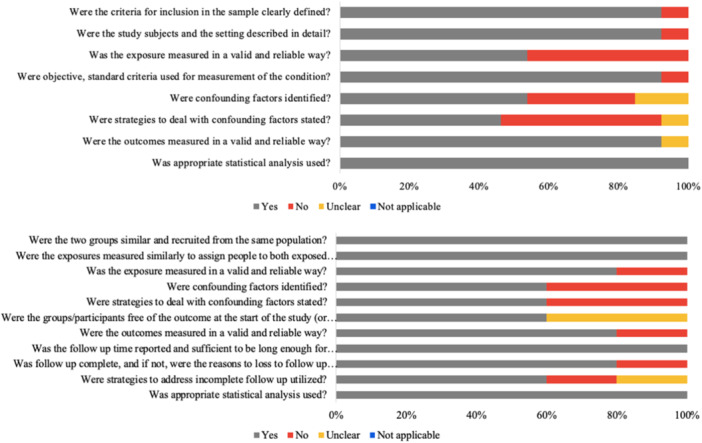
Risk of bias of the cross‐sectional articles included according to The Joanna Briggs Institute Critical Appraisal checklist.
2.9. Data analysis
2.9.1. Descriptive analysis
Description of the characteristics of the included studies, such as type of study, sample size, age, gestational trimester, income, education, instruments used to measure exposure and outcome, and key findings (severity, prevalence, and association between HFI and depression and anxiety). Regarding country classification by income level, the countries in which the studies were conducted were classified according to the World Bank Open Data.
2.9.2. Effect size
The primary outcomes evaluated were symptoms of depression and anxiety in pregnant women, along with their respective 95% CI. For the quantitative analysis between HFI and depression, the AOR was extracted to conduct the metanalysis. If AOR was not available, the extracted measure was crude OR. We calculate the crude OR from the available frequency data for studies that do not report the association measure. If studies reported a measure of the regression's beta coefficient (B), it was converted to OR using the methods proposed by Zhang and Yu (1998). To standardise the measurements used, the crude odds ratio was considered for the meta‐analysis.
Additionally, if a study presented association measures considering different categories of food insecurity (mild, moderate, and severe), the measure associated with the highest‐level category (severe) was considered. The highest level of HFI was chosen because this category is considered to have a higher impact on mental health in the pregnancy group. Also, some studies do not categorise HFI as moderate or severe; they just presented data evaluating if the pregnant group was or was not facing HFI.
2.9.3. Meta‐analysis
Meta‐analysis was conducted when at least three studies reported data that could be included in the statistical combination of results. Overall associations were analysed using the 'meta' command for DerSimonian and Laird random‐effect models. Based on data availability, the OR and 95% CI were measured for the outcome of pregnancy depressive symptoms. Statistical heterogeneity between studies was measured using I‐square (I2). Heterogeneity was considered important if I2 values were >40% (Deeks et al., 2022). Publication bias analyses were performed when at least 10 studies were available for an outcome measure using Egger's test with a 5% significance level and funnel plot visual inspection (Deeks et al., 2022). Subgroup analysis was performed to verify the source of heterogeneity in the studies included in the systematic review. The following covariables were used: country, local (peri‐urban, rural, urban, and urban slam), study design (cross‐sectional and prospective cohort), trimester (all trimesters, second and third trimester), and course life (adolescent and adult). Participants from 10 to 19 years of age were considered adolescents, and women over 19 years old were considered adults (World Health Organisation, 2005). Data analysis was performed using the Stata software (StataCorp. 2019. Stata Statistical Software: Release 16.1. College Station, TX, USA; StataCorp, LLC).
2.9.4. Certainty assessment
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system was used to assess the certainty of the evidence based on the main domains of study limitations. The quality of evidence was downgraded based on five criteria: risk of bias, inconsistency of results, indirectness of evidence, imprecision, and publication bias (Schünemann et al., 2013).
3. RESULTS
3.1. Selected studies
A PRISMA flowchart of the selection process is summarised in Figure 1. The total of 1,749 articles were screened by title and abstract. Of these screened articles, 197 were selected for full‐text review. Three articles were identified, in addition to those identified by electronic databases, through the following approaches: analysis of bibliographic citations of selected articles, search on websites, and location through another systematic review. At the end of the process, 18 articles were included in the systematic review (Ayyub et al., 2018; Dias, 2011; Dibaba et al., 2013; Doglikuu et al., 2023; Eick et al., 2020; Grilo et al., 2015; Gross et al., 2018; Harrison & Sidebottom, 2008; Khoshgoo et al., 2020; Laraia et al. 2006, 2022; Mak, 2019; Matlwa et al., 2021; Oladeji et al., 2022; Pobee et al., 2022; Sidebottom et al., 2014; Tsai et al., 2016; van Heyningen et al., 2017), and of these, 10 (Ayyub et al., 2018; Dibaba et al., 2013; Gross et al., 2018; Khoshgoo et al., 2020; Laraia et al., 2022; Matlwa et al., 2021; Oladeji et al., 2022; Pobee et al., 2022; Sidebottom et al., 2014; Tsai et al., 2016) were selected for the meta‐analysis between HFI and depressive symptoms since they presented all the data necessary for the analyses. The list of reasons for excluding articles from the review is presented in Appendix S3.
Figure 1.
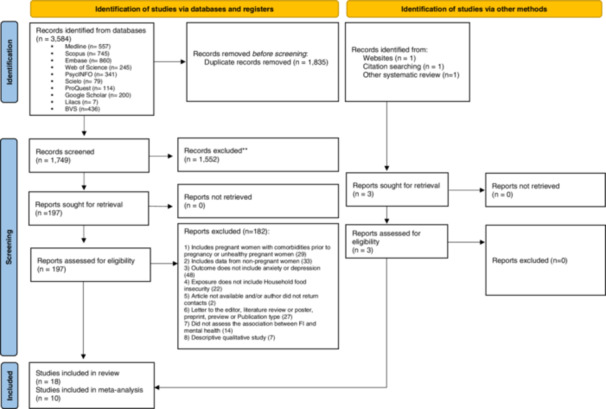
'Flowchart of the selection process according to PRISMA'. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi:10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/.
3.2. Characteristics of the studies
Among the studies included in this systematic review, 13 were cross‐sectional studies (Ayyub et al., 2018; Dias, 2011; Dibaba et al., 2013; Doglikuu et al., 2023; Grilo et al., 2015; Harrison & Sidebottom, 2008; Khoshgoo et al., 2020; Laraia et al., 2006, 2022; Mak, 2019; Matlwa et al., 2021; Oladeji et al., 2022; van Heyningen et al., 2017), and five were cohort studies (Eick et al., 2020; Gross et al., 2018; Pobee et al., 2022; Sidebottom et al., 2014; Tsai et al., 2016). These articles were published between 2006 (Laraia et al., 2006) and 2023 (Doglikuu et al., 2023) and carried out in the following countries: Pakistan (Ayyub et al., 2018), Brazil (Dias, 2011), Ethiopia (Dibaba et al., 2013), United States (Eick et al., 2020; Grilo et al., 2015; Gross et al., 2018; Harrison & Sidebottom, 2008; Laraia et al., 2006, 2022; Sidebottom et al., 2014), South Africa (Matlwa et al., 2021; Tsai et al., 2016; van Heyningen et al., 2017), Iran (Khoshgoo et al., 2020), Canada (Mak, 2019), Nigeria (Oladeji et al., 2022) and Ghana (Doglikuu et al., 2023; Pobee et al., 2022). The number of pregnant women analysed in this review totalled 27,882 women, with the sample varying from 94 (Dias, 2011) to 14,274 (Laraia et al., 2022). The average age of pregnant women ranged between 18.3 ± 1.0 (Oladeji et al., 2022) and 32 ± 5.4 years (Eick et al., 2020). Three studies included only adolescents (Doglikuu et al., 2023; Grilo et al., 2015; Oladeji et al., 2022) four studies (Ayyub et al., 2018; Dias, 2011; Khoshgoo et al., 2020; van Heyningen et al., 2017) included pregnant women in all gestational trimesters, and eight studies did not inform the participants’ gestational period (Doglikuu et al., 2023; Harrison & Sidebottom, 2008; Laraia et al., 2022; Mak, 2019; Matlwa et al., 2021; Sidebottom et al., 2014; Tsai et al., 2016). The majority of pregnant women were low‐income (Ayyub et al., 2018; Dias, 2011; Dibaba et al., 2013; Gross et al., 2018; Laraia et al., 2006, 2022; Matlwa et al., 2021; Oladeji et al., 2022; van Heyningen et al., 2017) and an average educational background, primarily at the high school level (Dias, 2011; Khoshgoo et al., 2020; Laraia et al., 2006, 2022; Oladeji et al., 2022). The study by Tsai et al. (2016) evaluated pregnant women with and without human immunodeficiency virus (HIV) and was included considering the eligibility criteria, however, only pregnant women without HIV baseline data were used in this review.
3.3. HFI across studies
The prevalence of HFI found in studies considering all gestational trimesters ranged between 12.6% in Canada (Mak, 2019) and 62.1% in the United States of America (Sidebottom et al., 2014). Among pregnant women evaluated only in the first trimester, Harrison and Sidebottom (2008) obtained a prevalence of HFI of 32% in the USA, while Pobee et al. (2022) found a prevalence of 50% in Ghana.
HFI was assessed using the following instruments: validated HFI scales (e.g., Household Food Insecurity Access Scale [HFIAS]) (Ayyub et al., 2018; Doglikuu et al., 2023), Brazilian Food Insecurity Scale (EBIA) (Dias, 2011), US Household Food Security Survey Module (HFSSM) (Gross et al., 2018; Harrison & Sidebottom, 2008; Khoshgoo et al., 2020; Laraia et al., 2006, 2022; Mak, 2019; Pobee et al., 2022; Sidebottom et al., 2014; van Heyningen et al., 2017), and questionnaire developed with specific question (Eick et al., 2020; Grilo et al., 2015; Matlwa et al., 2021; Oladeji et al., 2022; Tsai et al., 2016). Most of these specific questions assessed food insecurity, defined as food insufficiency or hunger as the number of days the respondent had gone to bed hungry in the previous 7 days because there was no food to eat. Some examples of questions: 'In the last 7 nights did you ever go to bed hungry? Do you ever run out of money or food stamps to buy food? How many days in the past week have you gone hungry? Did you or other adults in the household skip meals? Are you worried about food running out? Was there not enough money to buy food?' Dibaba et al. (2013) presented a six‐item scale questionnaire based on previously validated measures in developing countries. Women were asked whether because food ran out or money was not enough to buy food, in the last 3 months. It is noteworthy to detail that the study conducted by Tsai et al. (2016) assessed food insufficiency (Tsai et al., 2016), and Matlwa et al. (2021) and Oladeji et al. (2022) evaluated maternal hunger (Matlwa et al., 2021; Oladeji et al., 2022), both characterised in the literature as severe food insecurity (Blumberg et al., 1999).
3.4. Depression and anxiety symptoms across studies
Thirteen articles evaluated depression in pregnant women as the main outcome (Ayyub et al., 2018; Dibaba et al., 2013; Doglikuu et al., 2023; Eick et al., 2020; Fuller et al., 2018; Harrison & Sidebottom, 2008; Khoshgoo et al., 2020; Laraia et al., 2022; Matlwa et al., 2021; Oladeji et al., 2022; Sidebottom et al., 2014; Tsai et al., 2016), five assessed depression and anxiety (Dias, 2011; Grilo et al., 2015; Laraia et al., 2006; Mak, 2019; Pobee et al., 2022) and one assessed only anxiety symptoms (van Heyningen et al., 2017). The prevalence of depressive symptoms ranged from 18% in the United States (Harrison & Sidebottom, 2008) to 49% in Ghana (Pobee et al., 2022), and the prevalence of anxiety symptoms ranged from 23% in South Africa (van Heyningen et al., 2017) to 34% in Ghana (Pobee et al., 2022). Table 1 presents the main characteristics of the studies included in the review.
The following instruments assessed the depressive symptoms: 25% (n = 4) Edinburgh Postnatal Depression Scale (EPDS) (Ayyub et al., 2018; Dibaba et al., 2013; Oladeji et al., 2022; Tsai et al., 2016), 6.25% (n = 1) Revised Children's Anxiety and Depression Scale (RCADS‐25) (Doglikuu et al., 2023), 25% (n = 4) Center for Epidemiologic Studies‐Depression (CES‐D) (Eick et al., 2020; Grilo et al., 2015; Laraia et al., 2006; Pobee et al., 2022), 12.5% (n = 2) Beck Depressive Inventory‐II (BDI‐II) questionnaire (Dias, 2011; Khoshgoo et al., 2020) and 25% (n = 4) Patient Health Questionnaire‐9 (PHQ‐9) (Gross et al., 2018; Harrison & Sidebottom, 2008; Matlwa et al., 2021; Sidebottom et al., 2014). The article by Mak (2019) used an interview model (Mak, 2019), so the interviewee should report the disorder if a health professional diagnosed it. It is noteworthy that the article conducted by Mak (2019) assessed the mental health of pregnant women by investigating the diagnosed mood disorder, which includes depression, bipolar disorder, mania, or dysthymia. The exposure by Laraia et al., (2022) was HFI, and this study entered meta‐analysis. Laraia et al., (2006) presented anxiety and depressive symptoms as exposure and was included in the systematic review but was not eligible to be entered in the meta‐analysis.
The following instruments assessed the anxiety symptoms: 16.66% (n = 1) Hamilton Anxiety Scale (HAMA) (Dias, 2011), 16.66% (n = 1) Generalised Anxiety Disorder Scale (GAD‐7) (Grilo et al., 2015), 16.66% (n = 1) Mini‐International Neuropsychiatric Interview (MINI Plus) (van Heyningen et al., 2017), 16.66% (n = 1) Spielberger's Trait Anxiety Inventory (Laraia et al., 2006), and 16.66% (n = 1) Beck Anxiety Inventory (BAI) (Pobee et al., 2022). Mak (2019) used the interview model to assess anxiety (Mak, 2019), while Laraia et al. (2022) did not report the instrument used to measure anxiety during pregnancy.
3.5. Description of the relationship between HFI and depression/anxiety symptoms
Regarding cohort studies, all of them (n = 5) evaluated the association between HFI and depression symptoms. In the USA, Sidebottom et al. (2014) identified a greater chance of depression in pregnant women exposed to moderate/high food insecurity (OR 2.44; 95% CI 1.43–4.16) and Eick et al. (2020) showed a strong correlation between the presence of HFI and depression (point biserial r = 0.65). Tsai et al. (2016) evaluated food insufficiency and identified an association with symptoms of prenatal depression in South Africa (aOR 1.74; 95% CI 1.25–2.43).
Similarly, 11 cross‐sectional studies (Ayyub et al., 2018; Dias, 2011; Dibaba et al., 2013; Grilo et al., 2015; Harrison & Sidebottom, 2008; Khoshgoo et al., 2020; Laraia et al., 2006, 2022; Mak, 2019; Matlwa et al., 2021; Oladeji et al., 2022) included in this systematic review identify an association between HFI and symptoms of depression. Laraia et al. (2006) (Laraia et al., 2006) investigated the prevalence and predictors of HFI among pregnant women from middle and low‐income families. Therefore, HFI was assessed as an outcome and not exposure. The authors identified stress, anxiety, and depressive symptoms as predictors of HFI in pregnant women, in addition to socioeconomic and demographic indicators. All pregnant adolescents evaluated by Doglikuu's study presented some level of HFI. Thus, its results were in the opposite direction showing protection and not a risk since the authors identified that girls with low food insecurity presented a reduced risk of depression when compared to high food insecurity girls.
Regarding anxiety symptoms, five cross‐sectional studies evaluated the association with HFI (Dias, 2011; Grilo et al., 2015; Laraia et al., 2006; Mak, 2019; van Heyningen et al., 2017). All of them presented a positive association between HFI and anxiety symptoms. Mak et al. (2019) (Mak, 2019) assessed the mental health of pregnant women from Canada by investigating the diagnosis of anxiety disorder, which includes phobia, obsessive‐compulsive disorder, or panic disorder. Only one cohort study carried out in Ghana showed the association between HFI and anxiety symptoms (Pobee et al., 2022).
3.6. Methodological quality of individual studies
After analysing the methodological quality, the studies were considered heterogeneous, as the majority (88.8%; n = 16) presented a high risk of bias, as illustrated in Figure 2 (detail in Tables S1 and S2). The sampling, follow‐up, and statistical analysis parameters were met in 100% of the studies. However, the parameter that presented the least adequacy was related to strategies to deal with confounding factors, with 46% of cross‐sectional studies presenting inadequacy or unclear in the study. The same parameter showed a high percentage of inadequacy in cohort studies, as 40% of the studies obtained a 'no' answer. Only two articles met all adequacy parameters and were considered low risk of bias (Dias, 2011; Doglikuu et al., 2023).
3.7. Meta‐analysis of HFI and symptoms of depression
A total of 10 studies were pooled in the meta‐analysis, covering a sample consisting of 18,987 pregnant women. Meta‐analysis showed that pregnant women's exposure to HFI was associated with increased odds of experiencing symptoms of depression [(OR: 2.52; 95% CI: 2.11–3.02) I2 = 73.23%] (Figure 3). Subgroup analysis demonstrated no statistical difference among study design, life course, and gestational trimester. However, considering the subgroup analysis for country, a difference between the effect size was observed in the study carried out in Ghana, when compared to Ethiopia. Rural local also presented a difference when compared to peri‐urban localisation (Table 2). The funnel graph (Figure 4) presented no publication bias, as confirmed by the Eagger test (p = 0.2932).
Figure 3.
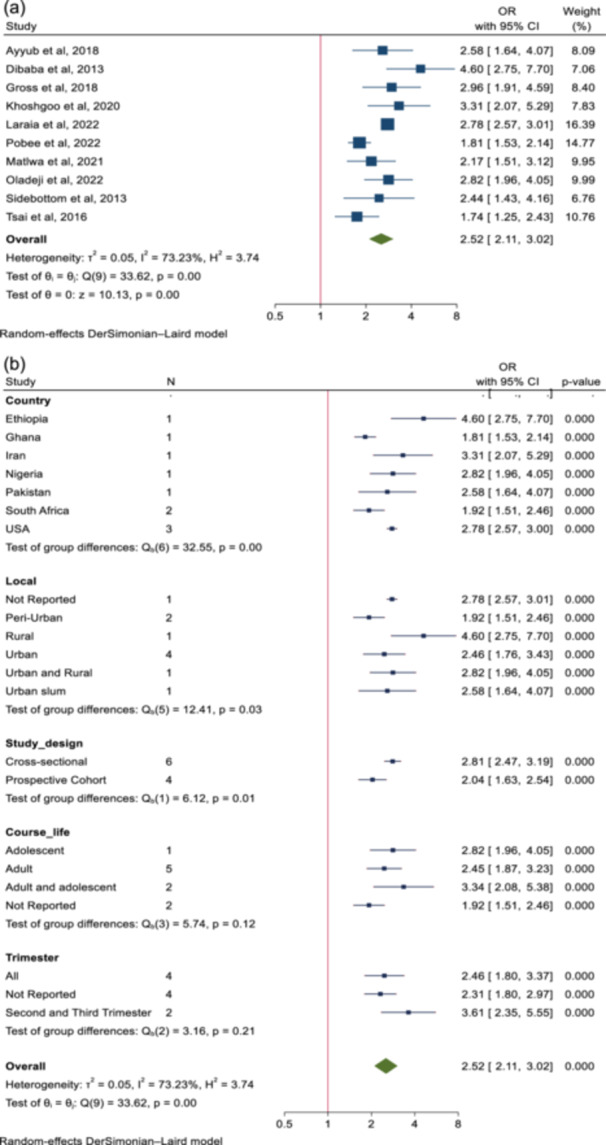
(a) Pooled effect size of the association between household food insecurity and depression symptoms. (b) Pooled effect size of the association between household food insecurity and depression symptoms—Subgroup meta‐analysis.
Table 2.
Association between household food insecurity and depression symptoms and heterogeneity in subgroups analysis.
| Subgroups | Number of studies | Number of participants | Odds ratio | 95% CI | p‐value |
|---|---|---|---|---|---|
| Country | |||||
| Ethiopia | 1 | 627 | 4.60 | 2.75–7.70 | 0.000 |
| Ghana | 1 | 116 | 1.81 | 1.53–2.14 | 0.000 |
| Iran | 1 | 394 | 3.31 | 2.07–5.29 | 0.000 |
| Nigeria | 1 | 1359 | 2.82 | 1.96–4.05 | 0.000 |
| Pakistan | 1 | 367 | 2.58 | 1.64–4.07 | 0.000 |
| South Africa | 2 | 1353 | 1.92 | 1.51–2.46 | 0.000 |
| USA | 3 | 14,771 | 2.78 | 2.57–3.00 | 0.000 |
| Local | |||||
| Not Reported | 1 | 14,274 | 2.78 | 2.57–3.01 | 0.000 |
| Peri‐Urban | 2 | 1353 | 1.92 | 1.51–2.46 | 0.000 |
| Rural | 1 | 627 | 4.60 | 2.75–7.70 | 0.000 |
| Urban | 4 | 1007 | 2.46 | 1.76–3.43 | 0.000 |
| Urban and Rural | 1 | 1359 | 2.82 | 1.96–4.05 | 0.000 |
| Urban slum | 1 | 367 | 2.58 | 1.64–4.07 | 0.000 |
| Study design | |||||
| Cross‐sectional | 6 | 17,605 | 2.81 | 2.47–3.19 | 0.000 |
| Prospective cohort | 4 | 1382 | 2.04 | 1.63–2.54 | 0.000 |
| Course life | |||||
| Adolescent | 1 | 1359 | 2.82 | 1.96–4.05 | 0.000 |
| Adult | 5 | 1374 | 2.45 | 1.87–3.23 | 0.000 |
| Adult and adolescent | 2 | 14,901 | 3.34 | 2.08–5.38 | 0.000 |
| Not Reported | 2 | 1353 | 1.92 | 1.51–2.46 | 0.000 |
| Trimester | |||||
| All | 4 | 2236 | 2.46 | 1.80–3.37 | 0.000 |
| Not Reported | 4 | 15,714 | 2.31 | 1.80–2.97 | 0.000 |
| Second and Third | 2 | 1037 | 3.61 | 2.35–5.55 | 0.000 |
Figure 4.
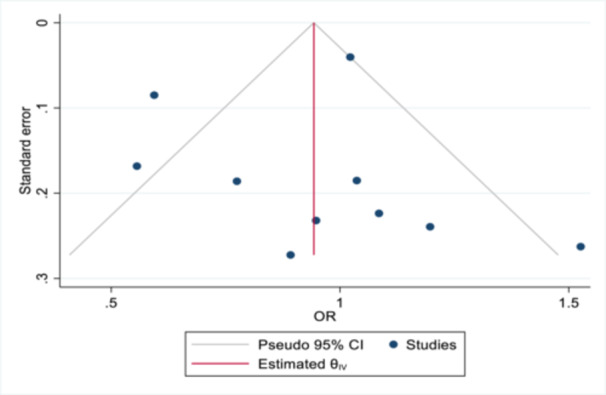
Publication bias Funnel graph.
3.8. Certainty of evidence
In evaluating the certainty of the evidence by considering the primary domains of study limitations, the overall quality of the evidence was characterised as 'very low' (⊕◯◯◯), as presented in Table 3.
Table 3.
GRADE evidence profile for HFI and depression symptoms in pregnancy woman.
| Certainty assessment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | No. of studies | Study design | Risk of biasa | Inconsistency b | Indirectness c | Imprecision d | Publication bias e | Certainty |
| Depression | 10 | observational studies | very serious | very serious | not serious | not serious | none |
⊕◯◯◯ Very low |
Risk of bias assessed using JBI. Downgrade 2 levels, considering the high risk of bias of the studies evaluated.
Downgrade 1 level if I2 was 50% to 75%, and 2 levels if I2 was 75% to 100%.
No downgrade for indirectness because all studies directly measure the outcomes.
No downgrade for imprecision because of >2000 participants for each outcome.
Publication bias was considered when significance of p < 0.05. No downgrade because p = 0.2932.
4. DISCUSSION
The current systematic review identified an association between HFI and depressive and anxiety symptoms during pregnancy. Specifically, the meta‐analysis showed that HFI is associated with higher odds of depression symptoms. However, the association between HFI and anxiety could not be conducted due to the restricted number of studies eligible for this review.
The meta‐analysis and meta‐regression conducted in this systematic review revealed a high heterogeneity among studies between HFI and depression symptoms in pregnant individuals. This elevated level of heterogeneity may be attributed to the diversity in study designs, varying sample sizes, and regional differences, as well as the use of different instruments to assess both exposure and outcome. Thus, robust methodological quality is important to reduce heterogeneity among studies, facilitate comparison with other data, and strengthen the conclusions’ validity and reliability.
In situations of poverty, families face persistent challenges in accessing sufficient, nutritious food. In this context, the intertwining of HFI with social disparities and the inadequacy of effective public policies highlight the importance of discussing the topic. Limited access to food, a global phenomenon exacerbated by economic disparities, not only contributes to malnutrition but also has direct implications for individuals’ mental health (Cain et al., 2022; Maynard et al., 2018; Pourmotabbed et al., 2020). Based on the results of this systematic review, depression stands out as an outcome related to this scenario.
Yin et al. (2021) estimated the prevalence of depression during pregnancy with a rate of 20.7% (95% CI 19.4%–21.9%, p = 0.000, I2 = 98.4%) for any prenatal depression and 15% (95% CI 13.6%–16.3%, p = 0.000, I2 = 97.8%) specifically for major prenatal depression, and the authors also showed a higher prevalence of prenatal depression was observed in low‐income countries (Yin et al., 2021). The prevalence of pregnant women with symptoms of depression varied between 18% and 49%, with the highest prevalence observed in Ghana, a low‐middle‐income country. The study conducted by Oladeji et al. (2022) in Nigeria with pregnant adolescents presented a significant association between HFI and depressive symptoms (OR 2.82, 95% CI 1.96–4.05, p < 0.001) (Oladeji et al., 2022). Protective factors identified by Santos et al. (2021) against postpartum depression in socially vulnerable families were higher maternal and paternal schooling, the presence of a husband or partner, and having received support from the child's father and the family during the pregnancy, highlighting the importance of screening for maternal depression. Laraia et al. (2022) showed that prenatal depressive symptoms were the most common maternal hardship (54.4%) for any category of food insecurity status during pregnancy, and one‐third of women with low or moderate food security reported those symptoms (34.8% and 31.8%, respectively) (Laraia et al., 2022).
The meta‐analysis conducted by Dennis et al. (2017) estimated the prevalence of prenatal anxiety in pregnant women, considering a clinical diagnosis of any anxiety disorder, of 15.2% (95% CI 9.0–21.4) and 4.1% (95% CI 1.9–6.2) for a generalised anxiety disorder (Dennis et al., 2017). Despite the absence of sufficient articles to support the meta‐analysis for HFI and anxiety symptoms in pregnant women, six articles (Dias, 2011; Grilo et al., 2015; Laraia et al., 2006; Mak, 2019; Pobee et al., 2022; van Heyningen et al., 2017) showed a positive association for anxiety.
The occurrence of maternal mental disorders, such as anxiety and depression, during pregnancy, should be better investigated by health professionals since it is related to adverse outcomes in maternal and child health (Grigoriadis et al., 2018; Szegda et al., 2014). The study carried out by Laraia et al. (2006) showed that depression and anxiety symptoms were associated with HFI in a dose–response relationship(Laraia et al., 2006). Theoretically, HFI reduces the opportunity for adequate nutrition in pregnant women, but depression may lead to HFI by impairing the mother's decision to choose better foods and her abilities to shop, cook, or work (Melchior et al., 2009).
This study has several strengths. To date, this is the first study conducted with a meta‐analysis showing the association between HFI and depression symptoms during pregnancy, and we consider these findings to have important implications for healthcare professionals. The Cochrane Handbook and PRISMA guidelines were followed to perform a robust and comprehensive search in 10 databases to assure methodological quality. A large number of pregnant women was included in this study, increasing the generalisability of the results. In addition, the methodological quality of the studies was assessed independently, and the GRADE system assessed the certainty of the evidence of the exposure‐outcome association.
It is important to highlight some limitations of the present study. First, high heterogeneity was observed between the studies analysed, considering the diverse characteristics of subjects and the variance between exposure and outcome assessment methods. Second, the crude odds ratio was used to perform the meta‐analysis instudies that not provided the adjusted odds ratio. Third, some studies were not included in the meta‐analysis because they did not present all the data necessary for the analyses, and the authors did not respond to contact attempts. Fourth, a small number of longitudinal studies have examined the relationship between HFI and symptoms of depression and anxiety in pregnant women, indicating the need for further studies with robust methodological quality. Lastly, people in vulnerable situations usually face poverty, and it is difficult to separate the effects of poverty and HFI on mental health. Encouragement is needed for researchers to deepen their investigations into the association between HFI and mental health during pregnancy, as it will provide a solid basis to support future decisions to benefit mental health and propositions for more assertive health public policies and health strategies for this vulnerable population.
5. CONCLUSIONS
This study identified that HFI is associated with a 2.52‐fold increase in the odds of depression symptoms during pregnancy. Due to the limited number of articles found, it was not possible to assess the association between HFI and anxiety symptoms through meta‐analysis. This finding showed the relationship between HFI and maternal mental health, highlighting the importance of effective policies to reduce food insecurity and strengthen mental health in pregnant groups.
AUTHOR CONTRIBUTIONS
Conceptualisation, C.B., A.B., V.S.S.G. G.B, and N.P.; methodology, C.B., V.S.S.G. and N.P.; conducting the systematic literature search, C.B. and A.B.; performed the data extraction and quality assessment, C.B. and A.B.; formal analysis, E.S.O.P. and V.S.S.G.; writing—original draft preparation, C.B. and A.B.; writing—review and editing, C.B., A.B, E.S.O.P., V.S.S.G., G.B and N.P.; supervision, N.P. All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
The following Supporting Information is available through the online version of this article at the publisher's website.
Appendix S1 Prisma checklist.
Appendix S2 Search strategy.
Appendix S3 Excluded articles and reasons for exclusion.
Table S1 Risk of bias for each individual study assessed by Joanna Briggs Institute critical appraisal checklist for Analytical Cross‐Sectional studies.
Table S2 Risk of bias for each individual study assessed by Joanna Briggs Institute critical appraisal checklist for Cohort studies.
ACKNOWLEDGEMENTS
We would like to thank Eliane Said Dutra, Wanessa de Oliveira Rocha and Lilian Siboney Xavier for carrying out PRESS. We would also like to thank all the authors who contributed by sending articles, clarifying information and sending data to compose this review. This research was funded by the University of Brasilia and by Federal District Research Support Foundation (FAP/DF).
Biete, C. , Biete, A. , Patriota, E. S. O. , Gonçalves, V. S. S. , Buccini, G. , & Pizato, N. (2025). Household food insecurity and symptoms of anxiety and depression during pregnancy: Systematic review and meta‐analysis. Maternal & Child Nutrition, 21, e13714. 10.1111/mcn.13714
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the supplementary material of this article.
REFERENCES
- Abrahams, Z. , Boisits, S. , Schneider, M. , Prince, M. , & Lund, C. (2022). The relationship between common mental disorders (CMDs), food insecurity and domestic violence in pregnant women during the COVID‐19 lockdown in Cape Town, South Africa. Social Psychiatry and Psychiatric Epidemiology, 57(1), 37–46. 10.1007/s00127-021-02140-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahams, Z. , & Lund, C. (2022). Food insecurity and common mental disorders in perinatal women living in low socio‐economic settings in Cape Town, South Africa during the COVID‐19 pandemic: A cohort study. Global Mental Health, 9, 49–60. 10.1017/gmh.2022.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahams, Z. , Lund, C. , Field, S. , & Honikman, S. (2018). Factors associated with household food insecurity and depression in pregnant South African women from a low socio‐economic setting: A cross‐sectional study. Social Psychiatry and Psychiatric Epidemiology, 53(4), 363–372. 10.1007/s00127-018-1497-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aromataris, E. M. Z. (Eds.). (2020). JBI manual for evidence synthesis. JBI Manual for Evidence Synthesis. 10.46658/JBIMES-20-01 [DOI] [Google Scholar]
- Arzhang, P. , Ramezan, M. , Borazjani, M. , Jamshidi, S. , Bavani, N. G. , Rahmanabadi, A. , & Bagheri, A. (2022). The association between food insecurity and gestational weight gain: A systematic review and meta‐analysis. Appetite, 176, 106124. 10.1016/J.APPET.2022.106124 [DOI] [PubMed] [Google Scholar]
- Ayyub, H. , Sarfraz, M. , Mir, K. , & Salam, F. T. (2018). Association of antenatal depression and household food insecurity among pregnant women: A crosssectional study from slums of Lahore. Journal of Ayub Medical College, Abbottabad: JAMC, 30(3), 366–371. [PubMed] [Google Scholar]
- Bedaso, A. , Adams, J. , Peng, W. , & Sibbritt, D. (2021). The relationship between social support and mental health problems during pregnancy: A systematic review and meta‐analysis. Reproductive Health, 18(1), 162. 10.1186/S12978-021-01209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biltoft‐Jensen, A. , Matthiessen, J. , Hess Ygil, K. , & Christensen, T. (2022). Defining energy‐dense, nutrient‐poor food and drinks and estimating the amount of discretionary energy. Nutrients, 14(7), 1477. 10.3390/nu14071477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, M. M. , Behrman, J. R. , Daelmans, B. , Prado, E. L. , Richter, L. , Tomlinson, M. , Trude, A. C. B. , Wertlieb, D. , Wuermli, A. J. , & Yoshikawa, H. (2021). The principles of Nurturing Care promote human capital and mitigate adversities from preconception through adolescence. BMJ Global Health, 6(4), e004436. 10.1136/bmjgh-2020-004436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg, S. J. , Bialostosky, K. , Hamilton, W. L. , & Briefel, R. R. (1999). The effectiveness of a short form of the Household Food Security Scale. American Journal of Public Health, 89(8), 1231–1234. 10.2105/AJPH.89.8.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain, K. S. , Meyer, S. C. , Cummer, E. , Patel, K. K. , Casacchia, N. J. , Montez, K. , Palakshappa, D. , & Brown, C. L. (2022). Association of food insecurity with mental health outcomes in parents and children. Academic Pediatrics, 22(7), 1105–1114. 10.1016/J.ACAP.2022.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman‐Jensen, A. J. (2010). U.S. food insecurity status: Toward a refined definition. Social Indicators Research, 95(2), 215–230. 10.1007/S11205-009-9455-4 [DOI] [Google Scholar]
- Deeks, J. J. , Higgins, J. P. T. , & Altman, D. G. (2022). Analysing data and undertaking meta‐analyses. In Higgins J. P. T., Thomas J., Chandler J., Cumpston M., Li T., Page M. J., & Welch V. A. (Eds.), Cochrane handbook for systematic reviews of interventions. Wiley. [Google Scholar]
- Dennis, C. L. , Falah‐Hassani, K. , & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta‐analysis. British Journal of Psychiatry, 210(5), 315–323. 10.1192/BJP.BP.116.187179 [DOI] [PubMed] [Google Scholar]
- Dias, F. M. V (2011). Transtornos psiquiátricos e gestação: associação entre parâmetros clínicos e biológicos em uma comunidade rural de baixa renda. Tese (Doutor Em Neurociências). Universidade Federal de Minas Gerais, Minas Gerais, 2011.
- Dibaba, Y. , Fantahun, M. , & Hindin, M. J. (2013). The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: Evidence from rural Southwestern Ethiopia. BMC Pregnancy and Childbirth, 13, 135. 10.1186/1471-2393-13-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doglikuu, D. B. I. , Annan, J. K. , Asare, S. , Yawson, H. , Takyi, O. , Dzidzornu, F. A. , Koram, H. O. , & Johnson, E. A. (2023). Household food insecurity, family size and their interactions on depression prevalence among teenage pregnant girls in Ghana, a population based cluster survey. BMC Women's Health, 23(1), 527. 10.1186/s12905-023-02674-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eick, S. M. , Goin, D. E. , Izano, M. A. , Cushing, L. , DeMicco, E. , Padula, A. M. , Woodruff, T. J. , & Morello‐Frosch, R. (2020). Relationships between psychosocial stressors among pregnant women in San Francisco: A path analysis. PLoS One, 15(6), e0234579. 10.1371/journal.pone.0234579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO . (2020). The State of Food Security and Nutrition in the World 2020. The State of Food Security and Nutrition in the World 2020. 10.4060/CA9692EN [DOI]
- FAO . (2023a). Food security and nutrition in the world 2023. In The State of Food Security and Nutrition in the World 2023 (Vol. 10, Issue 9). 10.1016/S2213-8587(22)00220-0 [DOI] [Google Scholar]
- FAO . (2023b). Monitoring access to food and household food security1. Monitoring Access to Food and Household Food Security. https://www.fao.org/3/U8050t/u8050t02.htm
- Fuller, A. , Messito, M. J. , Mendelsohn, A. L. , Oyeku, S. O. , & Gross, R. S. (2018). Prenatal material hardships and infant regulatory capacity at 10 months old in low‐income Hispanic mother‐infant Pairs. Academic Pediatrics, 18(8), 897–904. 10.1016/j.acap.2018.04.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoriadis, S. , Graves, L. , Peer, M. , Mamisashvili, L. , Tomlinson, G. , Vigod, S. N. , Dennis, C. L. , Steiner, M. , Brown, C. , Cheung, A. , Dawson, H. , Rector, N. A. , Guenette, M. , & Richter, M. (2018). Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: Systematic review and meta‐analysis. The Journal of Clinical Psychiatry, 79(5), 17r12011. 10.4088/JCP.17R12011 [DOI] [PubMed] [Google Scholar]
- Grilo, S. , Earnshaw, V. , Jessica, B. L. , Emily, C. S. , Urania, M. , Jonathan, T. , & Jeannette, R. I. (2015). Food matters: Food insecurity among pregnant adolescents and infant birth outcomes. The Journal of Applied Research on Children, 6(2):4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9014646/ [PMC free article] [PubMed] [Google Scholar]
- Gross, R. S. , Mendelsohn, A. L. , & Messito, M. J. (2018). Additive effects of household food insecurity during pregnancy and infancy on maternal infant feeding styles and practices. Appetite, 130, 20–28. 10.1016/j.appet.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, P. A. , & Sidebottom, A. C. (2008). Systematic prenatal screening for psychosocial risks. Journal of Health Care for the Poor and Underserved, 19(1), 258–276. 10.1353/hpu.2008.0003 [DOI] [PubMed] [Google Scholar]
- van Heyningen, T. , Honikman, S. , Myer, L. , Onah, M. N. , Field, S. , & Tomlinson, M. (2017). Prevalence and predictors of anxiety disorders amongst low‐income pregnant women in urban South Africa: A cross‐sectional study. Archives of Women's Mental Health, 20(6), 765–775. 10.1007/s00737-017-0768-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, B. , Skouteris, H. , Boyle, J. A. , Bailey, C. , Walker, R. , Thangaratinam, S. , Sundseth, H. , Stephenson, J. , Steegers, E. , Redman, L. M. , Montanaro, C. , Lim, S. , Jorgensen, L. , Jack, B. , Borges, A. L. V. , Bergmeier, H. J. , Baxter, J. A. B. , Harrison, C. L. , & Teede, H. J. (2020). Health in reconception, pregnancy and postpartum global alliance: International network pregnancy priorities for the prevention of maternal obesity and related pregnancy and long‐tTerm complications. Journal of Clinical Medicine, 9(3), 822. 10.3390/JCM9030822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hromi‐Fiedler, A. , Bermúdez‐Millán, A. , Segura‐Pérez, S. , & Pérez‐Escamilla, R. (2011). Household food insecurity is associated with depressive symptoms among low‐income pregnant Latinas. Maternal & Child Nnutrition, 7(4), 421–430. 10.1111/J.1740-8709.2010.00266.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izano, M. A. , Cushing, L. J. , Lin, J. , Eick, S. M. , Goin, D. E. , Epel, E. , Woodruff, T. J. , & Morello‐Frosch, R. (2020). The association of maternal psychosocial stress with newborn telomere length. PLoS One, 15, e0242064. 10.1371/journal.pone.0242064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karbin, K. , Khorramrouz, F. , Farkhani, E. M. , Sobhani, S. R. , Mosalmanzadeh, N. , Shahriari, Z. , & Ranjbar, G. (2022). Household food insecurity during pregnancy as a predictor of anthropometric indices failures in infants aged less than 6 months: A retrospective longitudinal study. Public Health Nutrition, 25(4), 1005–1012. 10.1017/S1368980021003591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshgoo, M. , Eslami, O. , Khadem Al‐Hosseini, M. , & Shidfar, F. (2020). The relationship between household food insecurity and depressive symptoms among pregnant women: A cross sectional study. Ncbi.Nlm.Nih.Gov. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7215255/ [PMC free article] [PubMed]
- Laraia, B. , Vinikoor‐Imler, L. C. , & Siega‐Riz, A. M. (2015). Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity, 23(6), 1303–1311. 10.1002/oby.21075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia, B. A. , Gamba, R. , Saraiva, C. , Dove, M. S. , Marchi, K. , & Braveman, P. (2022). Severe maternal hardships are associated with food insecurity among low‐income/lower‐income women during pregnancy: Results from the 2012–2014 California maternal infant health assessment. BMC Pregnancy and Childbirth, 22(1), 138. 10.1186/S12884-022-04464-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia, B. A. , Siega‐Riz, A. M. , Gundersen, C. , & Dole, N. (2006). Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. The Journal of Nutrition, 136(1), 177–182. 10.1093/jn/136.1.177 [DOI] [PubMed] [Google Scholar]
- Lockitch, G. (2008). Clinical biochemistry of pregnancy. Critical Reviews in Clinical Laboratory Sciences, 34(1), 67–139. 10.3109/10408369709038216 [DOI] [PubMed] [Google Scholar]
- Mak, J. (2019). Food insecurity during pregnancy in Canada By a thesis submitted in conformity with the requirements for the degree of master of science department of nutritional sciences © Copyright By Jordan Mak 2019 .
- Matlwa, M. , Laurenzi, C. , Menyatsoe, M. , Gemmell, K. , Manda, S. , & Tomlinson, M. (2021). Impact of COVID‐19 on wellbeing of pregnant women in 7 neighbourhoods in the Western Cape. CoCare Maternal Support Study. Johannesburg, Grow Great Campaign, March 2021, March.
- Maynard, M. , Andrade, L. , Packull‐McCormick, S. , Perlman, C. M. , Leos‐Toro, C. , & Kirkpatrick, S. I. (2018). Food insecurity and mental health among females in high‐income countries. International Journal of Environmental Research and Public Health, 15(7), 1424. 10.3390/ijerph15071424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza, M. , Avallone, C. , Kotzalidis, G. D. , Marano, G. , Moccia, L. , Serio, A. M. , Balocchi, M. , Sessa, I. , Janiri, D. , De Luca, I. , Brisi, C. , Spera, M. C. , Monti, L. , Gonsalez del Castillo, A. , Angeletti, G. , Chieffo, D. , Rinaldi, L. , Janiri, L. , Lanzone, A. , … Sani, G. (2023). Depressive symptoms during pregnancy: Prevalence and correlates with affective temperaments and psychosocial factors. Journal of Personalized Medicine, 13(2), 211. 10.3390/JPM13020211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan, J. , Sampson, M. , Salzwedel, D. M. , Cogo, E. , Foerster, V. , & Lefebvre, C. (2016). PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of Clinical Epidemiology, 75, 40–46. 10.1016/J.JCLINEPI.2016.01.021 [DOI] [PubMed] [Google Scholar]
- Melchior, M. , Caspi, A. , Howard, L. M. , Ambler, A. P. , Bolton, H. , Mountain, N. , & Moffitt, T. E. (2009). Mental health context of food insecurity: A representative cohort of families with young children. Pediatrics, 124, e564–e572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oladeji, B. D. , Bello, T. , Ayinde, O. , Idowu, P. , & Gureje, O. (2022). Prevalence and correlates of depression among pregnant adolescents in primary maternal care in Nigeria. Archives of Women's Mental Health, 25(2), 441–450. 10.1007/s00737-021-01198-1 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez‐Escamilla, R. , Cunningham, K. , & Moran, V. H. (2020). COVID‐19 and maternal and child food and nutrition insecurity: A complex syndemic. Maternal & child nutrition, 16(3), 8–11. 10.1111/mcn.13036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizato, N. , Botelho, P. , Gonçalves, V. , Dutra, E. , & de Carvalho, K. (2017). Effect of grazing behavior on weight regain post‐bariatric surgery: A systematic review. Nutrients, 9(12), 1322. 10.3390/NU9121322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pobee, R. A. , Setorglo, J. , Kwashie Klevor, M. , & Murray‐Kolb, L. E. (2022). High levels of depressive symptoms and low quality of life are reported during pregnancy in Cape Coast, Ghana; a longitudinal study. BMC Public Health, 22(1), 894. 10.1186/s12889-022-13299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmotabbed, A. , Moradi, S. , Babaei, A. , Ghavami, A. , Mohammadi, H. , Jalili, C. , Symonds, M. E. , & Miraghajani, M. (2020). Food insecurity and mental health: A systematic review and meta‐analysis. Public Health Nutrition, 23(10), 1778–1790. 10.1017/S136898001900435X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann, H. , Brożek, J. , Guyatt, G. , Oxman, A. (2013). Quality of evidence. In H. Schünemann, J. Brożek, G. Guyatt, & A. Oxman (Eds.), GRADE Handbook. GRADE Working Group.
- Sidebottom, A. C. , Hellerstedt, W. L. , Harrison, P. A. , & Hennrikus, D. (2014). An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Archives of Women's Mental Health, 17(1), 27–40. 10.1007/s00737-013-0378-3 [DOI] [PubMed] [Google Scholar]
- Soma‐Pillay, P. , Nelson‐Piercy, C. , Tolppanen, H. , & Mebazaa, A. (2016). Physiological changes in pregnancy. Cardiovascular journal of Africa, 27(2), 89–94. 10.5830/CVJA-2016-021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos, I. S. , Munhoz, T. N. , Blumenberg, C. , Barcelos, R. , Bortolotto, C. C. , Matijasevich, A. , Júnior, H. G. S. , Marques Dos Santos, L. , Correia, L. L. , de Souza, M. R. , Lira, P. I. C. , Altafim, E. , Marino, E. , Macana, E. C. , da Silva, R. S. , Ohana, E. F. , Fontes, M. T. A , Victora, C. G. (2021). Post‐partum depression: A cross‐sectional study of women enrolled in a conditional cash transfer program in 30 Brazilian cities. Journal of Affective Disorders, 281, 510–516. 10.1016/j.jad.2020.12.042 [DOI] [PubMed] [Google Scholar]
- Szegda, K. , Markenson, G. , Bertone‐Johnson, E. R. , & Chasan‐Taber, L. (2014). Depression during pregnancy: A risk factor for adverse neonatal outcomes? A critical review of the literature. The Journal of Maternal‐Fetal & Neonatal Medicine: The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 27(9), 960–967. 10.3109/14767058.2013.845157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, A. C. , Tomlinson, M. , Comulada, W. S. , & Rotheram‐Borus, M. J. (2016). Food insufficiency, depression, and the modifying role of social support: Evidence from a population‐based, prospective cohort of pregnant women in peri‐urban South Africa. Social Science & Medicine, 151, 69–77. 10.1016/j.socscimed.2015.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2005). Nutrition in Adolescence‐Issues and Challenges for the Health Sector Issues in Adolescent Health and Development. World Health Organization: Geneva, Switzerland.
- World Health Organization . (2023). ICD‐11 for Mortality and Morbidity Statistics. https://icd.who.int/browse11/l-m/en#/http%3A%2F%2Fid.who.int%2Ficd%2Fentity%2F1336943699
- Yin, X. , Sun, N. , Jiang, N. , Xu, X. , Gan, Y. , Zhang, J. , Qiu, L. , Yang, C. , Shi, X. , Chang, J. , & Gong, Y. (2021). Prevalence and associated factors of antenatal depression: Systematic reviews and meta‐analyses. Clinical Psychology Review, 83, 101932. 10.1016/J.CPR.2020.101932 [DOI] [PubMed] [Google Scholar]
- Zhang, J. , Yu, K. F. (1998). What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA, 280(19), 1690–1691. 10.1001/jama.280.19.1690 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The following Supporting Information is available through the online version of this article at the publisher's website.
Appendix S1 Prisma checklist.
Appendix S2 Search strategy.
Appendix S3 Excluded articles and reasons for exclusion.
Table S1 Risk of bias for each individual study assessed by Joanna Briggs Institute critical appraisal checklist for Analytical Cross‐Sectional studies.
Table S2 Risk of bias for each individual study assessed by Joanna Briggs Institute critical appraisal checklist for Cohort studies.
Data Availability Statement
The data that support the findings of this study are available in the supplementary material of this article.


