Abstract
Inoculation with viable, but not inactivated, Coxiella burnetii resulted in the increased expression of transferrin receptors (TfR) in the murine macrophage-like cell line J774A.1. This upregulation was evident in immunoblots as early as 6 h postinfection, with TfR levels continuing to increase through the first 24 h of infection. Fluorescent labeling revealed that TfR upregulation occurred throughout infected monolayers, eliminating the possibility that it reflected a response by a minor subset of host cells. In addition, TfR trafficking did not appear to be affected by C. burnetii infection. Consistent with the increase in TfRs, inoculation with viable C. burnetii resulted in a 2.5-fold increase in total cellular iron by 12 h postinoculation. Our further findings that the chelation of intracellular iron arrests C. burnetii replication and that C. burnetii metabolic activities in vitro are affected by iron concentration suggest that TfR upregulation is a salient factor in C. burnetii infection, and we speculate that it may represent a significant virulence mechanism.
Intracellular pathogens obtain shelter from the immune response and access to intracellular nutrients from within their hosts. However, to exploit this niche, these parasites must be able to evade the innate destructive mechanisms of their host cells. Organisms such as Mycobacteria tuberculosis (17), Chlamydia psittaci (14, 55), and Legionella pneumophila (26) achieve this evasion by preventing phagolysosomal fusion, while Shigellae (20, 49) and Listeria monocytogenes (18) escape from endosomes into the cytoplasm. Both mechanisms allow these bacteria to survive by avoiding the low pH, oxygen radicals, and degradative proteases of the phagolysosome.
Coxiella burnetii, however, employs no mechanisms to avoid the phagolysosome and indeed requires this harsh environment for replication. Vacuoles containing C. burnetii have characteristics of typical phagolysosomes, as shown by the presence of lysosomal membrane markers in vacuole membranes (23) as well as staining positively for the lysosomal enzymes, 5′-nucleotidase (8), and acid phosphatase (1, 8). The internal pH of vacuoles containing C. burnetii, about 4.8 (35), is identical to that of phagolysosomes. This acidic pH appears to be essential for C. burnetii metabolic activity. In vitro experiments find that C. burnetii is able to catabolize glucose and glutamate, generate ATP, and synthesize nucleic acids and proteins at low but not neutral pH. This is consistent with the in vivo observation that C. burnetii replication is inhibited by raising the phagolysosomal pH with lysomotrophic amines (19). Thus, C. burnetii is adapted to a phagolysosomal environment where it is able to flourish by means that are as yet poorly understood.
Current evidence indicates that upon infection C. burnetii is able to modify responses that accompany phagocytosis, perhaps ameliorating its environment to some degree. C. burnetii infection is known to reduce the respiratory burst of macrophages, an integral part of the bactericidal response during infection (3). Phagolysosomes containing C. burnetii appear to be more fusion permissive than phagolysosomes inhabited by another obligate intracellular pathogen, Leishmania amazonensis (42, 52, 53). Additionally, phagolysosomes containing C. burnetii coalesce into a single large vacuole, indicating fusion permissibility (22).
The present study documents another consequence of C. burnetii infection, an increase in transferrin receptor (TfR) expression. The significance of these observations is twofold. First, we find that intracellular iron is essential for C. burnetii replication, and thus upregulation of TfR may facilitate C. burnetii sequestration of this vital nutrient. Second, an increase in the intracellular iron in macrophages is known to depress killing of intracellular pathogens (37), and thus upregulation of TfR may promote C. burnetii survival.
MATERIALS AND METHODS
Host cell lines and bacterial propagation.
J774A.1, a murine macrophage-like cell line (TIB-67; American Type Culture Collection, Rockville, Md.), was maintained in RPMI 1640 medium (RPMI; Gibco BRL, Grand Island, N.Y.) supplemented with 10% heat-inactivated fetal bovine serum (FBS) in 5% CO2 at 37°C. C. burnetii Nine Mile phase I (48) was propagated in J774A.1 cells in the same conditions as noted above. C. burnetii was harvested by differential centrifugation of cell culture supernatants first at 5,500 × g for 10 min to pellet host cell debris and then at 15,000 × g for 1 h to pellet the bacteria. Numbers of C. burnetii were estimated by measuring the turbidity of bacterial suspensions with a Klett Summerson photoelectric colorimeter (Klett Manufacturing Company Incorporated, New York, N.Y.), using a no. 42 filter (40); for a given experiment, densities were adjusted to provide the desired multiplicity of infection (MOI). C. burnetii was inactivated either chemically, by incubation for 12 h at room temperature with vigorous shaking in 2% glutaraldehyde–2% paraformaldehyde, or physically, by incubation for 2 h at 80°C. C. burnetii inactivated by both these methods were compared in all experiments, and no differences were seen (results not shown).
Immunoblotting.
J774A.1 cells were seeded onto six-well Falcon plates (VWR Scientific Products, Seattle, Wash.) at 106 cells per well, allowed to adhere for 12 h, and then incubated for 1 h with viable or inactivated C. burnetii at 108 per ml in RPMI–10% FBS. Extracellular C. burnetii was removed by three washes with medium at 37°C. At designated time points, the medium was removed, cells were washed three times with phosphate-buffered saline (PBS; 0.1 M NaPO4, 0.1 M NaCl [pH 7.4]), and cell numbers were determined. Cells were pelleted, suspended to 5 × 106 per ml in deionized distilled water containing 2 mM phenylmethylsulfonyl fluoride, and frozen. Samples of 5 × 104 cells were denatured by boiling in Laemmli’s buffer (30), resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) on 10% polyacrylamide gels, then electrotransferred to polyvinylidene difluoride membranes by standard techniques. Membranes were blocked in Blotto (PBS with 10% skim milk powder and 0.1% Tween 20) for 1 h following protein transfer and then probed with rat anti-mouse TfR monoclonal antibodies (kindly provided by R. Hyman, Salk Institute, San Diego, Calif.) (32) followed by goat anti-rat immunoglobulin G conjugated to horseradish peroxidase (Pierce, Rockford, Ill.). Signal was visualized with an enhanced chemiluminescence kit (Amersham, Cleveland, Ohio), and images were analyzed with an Image Master scanning densitometer and associated software (Pharmacia Biotech, Uppsala, Sweden).
Fluorescent labeling of TfR.
Confocal microscopy was used to compare TfR expression seen during C. burnetii infection with that seen in response to soluble factors in conditioned medium. J774A.1 cells were seeded on 15-mm-diameter Thermonox cover slips (Fisher Scientific, Santa Barbara, Calif.) in 24-well plates at 2.5 × 105 per well and allowed to adhere for 12 h. Then they were inoculated with 108 viable or inactivated C. burnetii (both in RPMI–10% FBS) or exposed to filter-sterilized conditioned medium (harvested from a 3-day culture of persistently infected J774A.1 cells) for an additional 16 h. At the end of this period, more than 95% of the cells were found to have taken up the inoculum. Following treatment, coverslips were rinsed with PBS, fixed in 0.1 M lysine HCl–2% paraformaldehyde–7.25 mM sodium periodate in 0.1 M NaPO4 buffer (pH 7.4) for 1 h, and washed three times in PBS. The samples were then blocked and permeabilized with 0.1% gelatin–0.3% saponin in PBS for 15 min, incubated with rat anti-mouse TfR monoclonal antibody for 1 h, washed three times, and probed with a fluorescein isothiocyanate-labeled rat secondary antibody (Organon Teknika Corp., West Chester, Pa.) for 1 h. Secondary antibody was washed off once for 10 min with blocking solution and twice for 10 min with PBS. Samples were fixed for 1 h at room temperature in PBS containing 4% paraformaldehyde. A Prolong antifade kit (Molecular Probes Inc., Eugene, Oreg.) was used as directed. A Bio-Rad 1024 laser scanning confocal microscopy imaging system equipped with a krypton-argon laser (Bio-Rad) on a Nikon inverted microscope with a 60× objective was used for laser scanning confocal microscopy. Images were processed with Adobe Photoshop 4.0 (Adobe Systems, Inc., Mountain View, Calif.).
Determination of intracellular iron content.
J774A.1 cells were seeded onto six-well plates at 106 cells per well, allowed to adhere for 12 h, and then incubated for 1 h with viable or inactivated C. burnetii at 108 per ml in RPMI–10% FBS. Removal of extracellular C. burnetii was facilitated by three washes with 37°C medium. At designated time points, the medium was removed, cells were washed three times with 0.7% saline solution, and cells were removed by scraping. Following determination of cell numbers and viability, cells were pelleted, saline was removed, and cells were stored at −80°C. For analysis, samples were suspended in 100 μl of 6 N HNO3 at 5 × 106 cells per ml, incubated at room temperature for 12 h, heated to 90°C for 3 h, and then diluted to 1 ml with deionized distilled H2O. Iron content was then determined by inductively coupled plasma emission, using a Jobin Yvon JY24 instrument (Instrumental Services, Livermore, Calif.).
Chelation of intracellular free iron.
J774A.1 cells were seeded at 4 × 105 cells per well onto six-well plates and allowed to adhere for 12 h. Cells were incubated for 24 h with C. burnetii resuspended at 108 per ml in RPMI–10% FBS containing fresh 0, 20, or 100 μM desferrioxamine (DfX; Sigma, St. Louis, Mo.). Extracellular C. burnetii was removed by washing, and incubations continued in medium containing DfX. Cultures were evaluated at 24, 48, and 72 h postinfection. Cells were stained with the viability indicator trypan blue, and total cell numbers were determined by hemocytometer. Infection levels were determined by examining J774A.1 cells stained with Gimenez reagent (16) that were mounted on glass slides with a Cytospin centrifuge (Shandon Inc., Pittsburgh, Pa.). For each treatment, at least 300 cells were scored as having 0, 0 to 10, 10 to 20, 20 to 50, 50 to 100 or more than 100 C. burnetii bacteria per cell. From these numbers, the C. burnetii count per well was estimated for each treatment. Cell numbers and viability were also determined for identically maintained uninoculated J774A.1 cells.
Incorporation of [35S]methionine-[35S]cysteine in vitro.
C. burnetii bacteria harvested from the supernatant of persistently infected cell cultures were divided equally into six samples (approximately 109/sample). Each sample was incubated at 37°C in citrate buffer (25 mM citric acid, 100 mM glycine, 65 mM KCl, 10 mM NaCl, 5 mM glutamate, 150 μM K2HPO4, 150 μM MgCl2, 500 μM glucose, 20 μM proline, 50 μg cycloheximide/ml [pH 4.5 or 7.0]) containing FeSO4 at 0, 0.1, or 0.2 mM. After 1 h, buffers were replaced and 50 μCi of [35S]methionine-[35S]cysteine (Express; NEN, Boston, Mass.) was added to each incubation and incubated a further 2 h. Bacteria were washed in PBS and precipitated in acetone–1 mM HCl.
RESULTS
TfR expression in macrophages during infection by C. burnetii.
Intracellular trafficking of iron in mammalian systems utilizes the iron carrier protein transferrin. Certain extracellular parasites such as Neisseria and Haemophilus spp. exploit this system by producing their own receptors for transferrin, through which they harvest sufficient iron to meet their metabolic needs (11). More recently, the intracellular parasite Ehrlichia chaffeensis was found to inhabit an endosome that accumulates TfRs in conjunction with an increase in TfR mRNA (5). In the present study, immunoblot analysis of SDS-PAGE-resolved lysates from uninfected and C. burnetii-infected cells were examined by using a monoclonal antibody specific for the murine TfR to determine if C. burnetii similarly modified TfR expression.
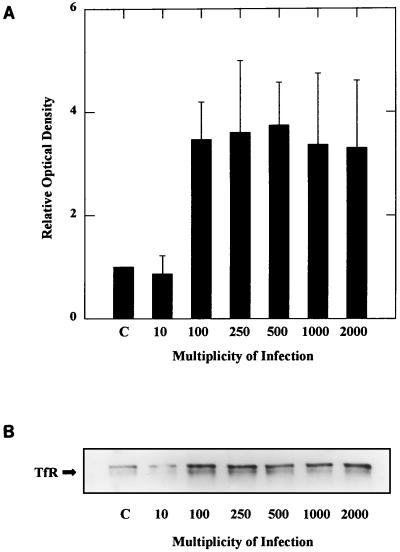
J774A.1 cells were inoculated with viable C. burnetii at MOIs ranging from 10 to 2,000 organisms per cell and then incubated for 12 h prior to sampling. Cells inoculated at an MOI of 100 or greater displayed an increase in TfR receptor expression (Fig. 1). Time course studies revealed that upregulation of TfR expression in infected J774A.1 cells began between 3 and 6 h postinoculation, with the greatest increase evident between 9 and 12 h, and continued to increase at least 24 h postinoculation, at which time the optical density of TfR bands was approximately 4.5-fold greater than that in the uninfected controls (Fig. 2). There was no apparent increase in TfR expression in cells inoculated with inactivated C. burnetii, suggesting that live organisms were required for TfR upregulation.
FIG. 1.
(A) To establish that TfR upregulation was not due to the large numbers of internalized C. burnetii necessary for visualization, J774A.1 cultures were infected with viable C. burnetii at the MOI indicated at the bottom. At 12 h postinfection, TfR expression was examined by immunoblot analysis. The optical density of bands on immunoblots was determined by scanning densitometry; the results shown are the means of three experiments, with error bars indicating standard errors. Student t tests indicate that there is a significant difference in the optical density of TfR bands from cultures infected at an MOI of ≥100 with P ≤ 0.05. (B) Representative immunoblot used to generate the data shown in panel A.
FIG. 2.
(A) The time course of TfR upregulation by C. burnetii infection was determined by immunoblotting. J774A.1 cells were inoculated with viable or inactivated C. burnetii. At designated time points, TfR expression was examined by immunoblot analysis. The optical density of bands was determined by scanning densitometry. TfR expression in cultures inoculated with inactivated C. burnetii show no increase in density, while infection with viable C. burnetii causes densities to increase by 24 h to 4.5 times that seen in uninoculated cells. Results shown are the mean of four experiments, with error bars indicating standard errors. Student t tests indicate that there is a significant difference in the optical density of TfR bands from infected samples taken at 9, 12, and 24 h and that for P < 0.1 (a) for P < 0.05 (b) and for P < 0.001 (c). (B) Representative immunoblots used to generate the data shown in panel A. Lane 12d shows TfR expression at 12 h by uninoculated J774A.1 cells.
TfR distribution and subcellular location.
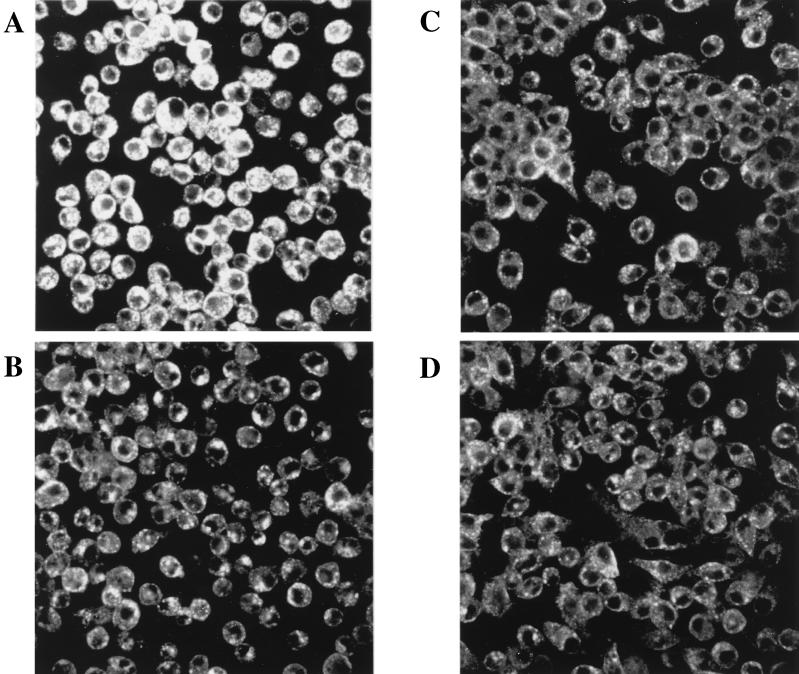
Confocal microscopy was used to visualize the increase in TfR after C. burnetii infection (Fig. 3). The intensity of fluorescence in cells infected with C. burnetii was uniformly distributed and 1.5-fold greater than that seen in either cells treated with inactivated C. burnetii or uninoculated control cells. Both infected cells and cells treated with conditioned medium exhibited a morphological change from spread out to rounded up (Fig. 3A and 3B). However, this morphological change did not correlate with increased TfR expression, as there was no increase in the fluorescence of cells incubated in conditioned medium, demonstrating that soluble factors were not responsible for TfR upregulation. The distribution of fluorescent label on the outside of C. burnetii-infected J774A.1 cells and a subcellular examination by transmission electron microscopy of TfR distribution (not shown) indicate that C. burnetii infection did not disturb the normal TfR trafficking.
FIG. 3.
J774A.1 cells were grown on Thermonox coverslips; TfRs were labeled with an anti-TfR monoclonal antibody and examined by confocal microscopy for TfR expression. (A) J774A.1 cells infected for 16 h with viable C. burnetii show increased TfR expression as well as a rounding up of infected cells. (B) J774A.1 cells incubated in conditioned medium from persistently infected J774A.1 cells. These cells show no upregulation of TfR but do exhibit the rounding up seen in infected cells. (C) J774A.1 cells inoculated with inactivated C. burnetii and (D) uninoculated J774A.1 cells exhibit a basal level of TfR expression and no morphological changes.
Iron concentration in macrophages during infection by C. burnetii.
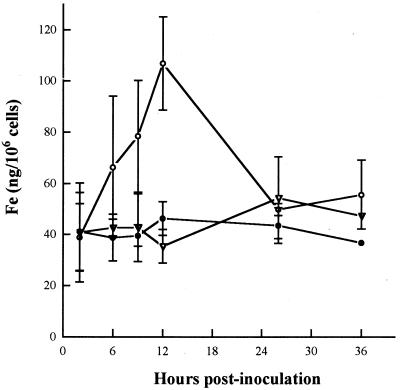
To determine if increased levels of TfR in C. burnetii-infected J774A.1 cells resulted in an increase in intracellular iron, cell lysates were analyzed for iron content by inductively coupled plasma emission (Fig. 4). Inoculation with inactivated C. burnetii did not alter the intracellular iron levels of J774A.1 cells. However, consistent with the observed increase in TfR expression, inoculation with viable C. burnetii resulted in a 2.5-fold increase in intracellular iron during the first 12 h. By 24 h postinfection, intracellular iron concentrations returned to preinfection levels.
FIG. 4.
An increase in intracellular iron would be expected to result from an upregulation of TfRs. The graph shows the intracellular iron content determined by inductively coupled plasma emission of J774A.1 cell cultures inoculated with viable (open circles) and inactivated C. burnetii (filled circles) as well as an uninoculated control (triangles). The results shown are the means for an experiment done in triplicate, and error bars indicate standard deviation. There are no error bars for two points at 36 h, as one data point was available for cells inoculated with inactivated C. burnetii and two were available for uninoculated cells.
Iron requirement for C. burnetii.
The observed increase in TfR expression and total intracellular iron following C. burnetii infection suggests that C. burnetii may acquire iron through accessing the increased pool of intracellular iron. To verify a role for free intracellular iron, the cell-permeant iron chelator DfX was used to reduce the intracellular free iron pool. Cell cultures were treated with 0, 20, and 100 μM DfX were infected and then sampled at 24 and 72 h postinfection (Table 1). J774A.1 cells were scored by microscopic examination as having 0, 1 to 10, 11 to 20, 21 to 50, 51 to 100, or more than 100 C. burnetii organisms per cell. Less than 1% of scored J774A.1 cells had more than 50 intracellular C. burnetii organisms. Averages of each group, 0, 5, 15, 35, 75, or 200, were used to calculate average C. burnetii number per cell. Numbers and viability (above 80% at all time points) of the infected cells were determined for each well. By 72 h after infection, the number of C. burnetii organisms in cells treated with 100 μM DfX had decreased, whereas the number in untreated J774A.1 cells had increased sevenfold. The growth rate and viability of uninfected J774A.1 cells treated with 0, 20, or 100 μM DfX were the same as for similarly treated infected cells. These results suggest that the free intracellular iron pool is a source of iron for C. burnetii. However, as one would expect, removal of iron also slowed (but did not halt) host cell replication; thus, we cannot at this point exclude the possibility that stress on the host cell contributed to the observed depression in the numbers of C. burnetii organisms.
TABLE 1.
Chelation of intracellular free iron with DfX halts C. burnetii proliferationa
| Cells | J774A.1 (106)/well
|
C. b./J774A.1 cell
|
C. b. (106)/well
|
|||
|---|---|---|---|---|---|---|
| 24 h | 72 h | 24 h | 72 h | 24 h | 72 h | |
| Infected | ||||||
| 0 μM DfX | 3.3 ± 1.1 | 14.0 ± 3.0 | 10.4 ± 2.5 | 15.5 ± 2.4 | 3.4 ± 0.9 | 21.6 ± 6.2 |
| 20 μM DfX | 4.9 ± 2.6 | 12.0 ± 1.9 | 9.5 ± 1.7 | 13.4 ± 2.3 | 4.6 ± 0.8 | 16.0 ± 4.4 |
| 100 μM DfX | 4.2 ± 0.2 | 6.9 ± 0.7 | 14.5 ± 0.5 | 5.3 ± 3.4 | 6.0 ± 0.2 | 3.8 ± 2.6 |
| Uninfected | ||||||
| 0 μM DfX | 4.5 ± 0.6 | 15 ± 0.6 | NA | NA | NA | NA |
| 20 μM DfX | 5.5 ± 1.3 | 11 ± 2.2 | NA | NA | NA | NA |
| 100 μM DfX | 4.8 ± 0.9 | 6.3 ± 1.0 | NA | NA | NA | NA |
J774A.1 cells in 24-well plates were infected with C. burnetii (C. b.) and simultaneously incubated in 0, 20, or 100 μM DfX. Three wells for each treatment were harvested at 24 h, and six wells were harvested at 72 h. The number and viability of J774A.1 cells per well were determined by hemocytometer. Infected J774A.1 cells were mounted on slides, and C. burnetii was visualized by Gimenez stain and counted on each slide. C. burnetii per well was calculated by multiplying C. burnetii per J774A.1 cell by J774A.1 cells per well for each well harvested. Viability of J774A.1 cells remained above 80% for all samples. Results are means ± standard deviations. NA, not applicable.
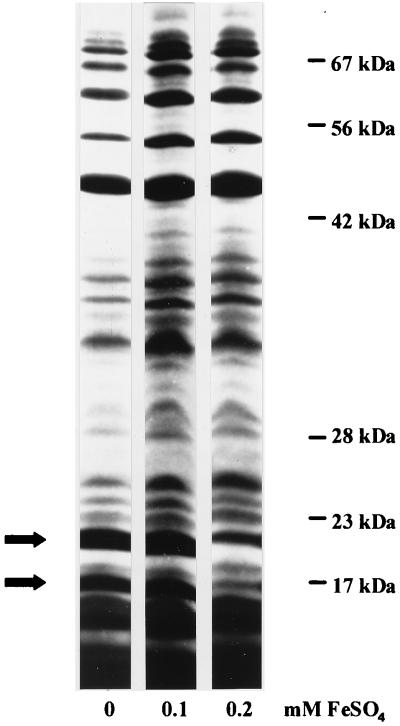
Effect of iron concentration on in vitro translation by C. burnetii.
Experiments with DfX suggested that C. burnetii accesses free intracellular iron. If this is the case, then C. burnetii should be able to access iron in the absence of transferrin or any other host-derived iron carrier. To test this possibility, the effect of free iron on C. burnetii metabolism was assayed in vitro, using purified organisms. C. burnetii was incubated in a citrate buffer containing [35S]methionine-[35S]cysteine at pH 4.5 for 2 h after a 1-h preincubation in unlabeled buffers. We compared results of three independent experiments in which three aliquots of C. burnetii were incubated at 0, 0.1, or 0.2 mM iron. We found that at 0 mM iron, total incorporation of [35S]methionine-[35S]cysteine was 62% ± 9% that seen at 0.2 and 0.1 mM iron and that at 0.2 mM iron, two major proteins, 17 and 20 kDa, showed decreased expression (Fig. 5). These results demonstrated a C. burnetii response to free soluble iron, supporting the hypothesis that C. burnetii is able to obtain iron from the intracellular pool of free iron.
FIG. 5.
To determine the effect of soluble iron on metabolic activity, C. burnetii was labeled with [35S]methionine for 2 h in a citrate buffer (pH 4.5) containing 0, 0.1, or 0.2 mM iron. Proteins expressed during this in vitro incubation were visualized by autoradiography to compare expression. Equal numbers of cells were loaded onto all lanes. Total expression is reduced by 38% in an average of five experiments at 0 mM iron, while expression of a 20-kDa and a 17-kDa protein (indicated by arrows) is reduced at 0.2 mM iron.
DISCUSSION
In living organisms, the intracellular iron concentration must be tightly regulated. Iron is essential for a variety of cellular processes, including electron transport, numerous redox reactions, and DNA biosynthesis. Iron is also toxic, catalyzing the generation of oxygen radicals via the Haber reaction, damaging DNA and cellular membranes (2, 36, 47). Iron uptake in mammalian cells is controlled by the expression of TfRs and the concentration of extracellular iron-loaded transferrin. TfRs are upregulated in response to the depletion of intracellular iron (24, 54). This regulation occurs at the posttranscriptional level by stabilization of TfR mRNA through the interaction of iron-responsive proteins with iron-responsive elements on mRNA (41). There appear to be additional uncharacterized pathways, as exemplified by cytokine-induced control of TfR expression (54). In this study, an increase in TfR expression was observed when J774A.1 cells were infected with viable C. burnetii. Mechanisms that elicit this response are unknown. Soluble factors released by infected cells did not appear to be responsible for TfR upregulation. It is possible that C. burnetii interacts directly with regulation pathways that lead to TfR upregulation. On the other hand, host cells may respond to a decrease in available iron as a result of iron sequestration by C. burnetii.
To move iron into a mammalian cell, TfR binds transferrin, an iron binding serum protein, at the plasma membrane of the cell. The TfR-transferrin complex is internalized via a clathrin-coated pit, which is then incorporated into an early endosome (7, 21). Here vacuolar ATPases lower the internal pH of the endosome to about 5.5 (50), and in response to the lowered pH, the transferrin releases the iron while remaining bound to the TfR (33, 39). The empty transferrin (or apotransferrin)-TfR complex is returned to the plasma membrane; here the neutral pH causes the TfR to lose its affinity for the apotransferrin, and it is released into the serum (12, 28). Thus, TfRs are cycled from the plasma membrane to endosomes (25) and back to the plasma membrane constitutively carrying iron into the cell as long as iron-loaded transferrin is available.
The TfRs upregulated during C. burnetii infection appear to cycle normally, as demonstrated by the fluorescent labeling seen in Fig. 3, and one would expect to see an increase in intracellular iron levels. We found a doubling of intracellular iron by 12 h postinfection, but by 24 h it returned to the preinfection level. Because TfR levels do not return to preinfection levels at this same rate, we speculate that homeostatic mechanisms maintaining intracellular iron balance may achieve this balance (43). Establishment of increased iron traffic may provide an iron source for replicating C. burnetii.
In addition to enhancing the availability of an essential nutrient, the increase in intracellular iron associated with C. burnetii upregulation of TfRs may allow the proliferation of these intracellular pathogens within macrophages. A diet rich in iron enhances infection by intracellular pathogens, while an iron-deficient diet reduces infection (31, 37, 46). In vitro studies have shown that increased intracellular iron levels allow the proliferation of intracellular pathogens (13, 15, 34, 44), some by reversing the gamma interferon stimulation of macrophages that results in the killing of intracellular pathogens (4, 9, 29). The mechanisms of killing by gamma interferon-activated macrophages include an enhancement of the oxidative burst (38), an increase in nitric oxide levels (27), and the downregulation of TfRs accompanied by a reduction in intracellular iron (6, 9, 51). In macrophages infected with C. burnetii, the oxidative burst is reduced (1) and TfR levels are upregulated as reported here, possibly diminishing the ability of macrophages to eliminate these intracellular pathogens.
Certain intracellular pathogens appear to access free iron pools and indeed may require this free iron pool (5, 45). DfX removes intracellular free iron or iron which is not bound by host-chelating proteins. Treatment of infected mammalian cells with DfX halts proliferation of intracellular Plasmodium falciparum (44), E. chaffeensis (4), L. pneumophila (10, 15), and F. tularensis (13), and we found that C. burnetii proliferation was likewise halted by DfX treatment of infected cells. C. burnetii is unique among these pathogens in that it resides within a mature phagolysosome, where the availability of iron is unknown. These studies suggest that C. burnetii is able to exploit the intracellular free iron pool from within the phagolysosome. In vitro experiments support the hypothesis that C. burnetii is able to utilize free iron, as shown by reduced expression of all proteins when iron is limiting and reduced expression of two major proteins when iron concentration is doubled.
This study has shown for the first time that infection of J774A.1 cells with viable but not inactivated C. burnetii is accompanied by an upregulation of TfR expression and that this increase in TfR expression was concurrent with a transient increase in intracellular iron. Microscopy has shown that TfRs cycle normally, carrying iron into the host cells, as supported by an increase in intracellular iron. An increase in intracellular iron may provide an iron source for C. burnetii and/or result in modulation of the immune response to C. burnetii infection; thus, TfR upregulation may be an important virulence factor for C. burnetii.
ACKNOWLEDGMENTS
We thank Michael Konkel for technical advice. We are very grateful to Michael Konkel, Ray Larsen, and Kathleen Postle for assistance in preparation of the manuscript. We thank Robert Hyman from the Salk Institute, San Diego, Calif., for his generous gift of the anti-murine TfR monoclonal antibody. Special thanks go to Christine Davitt, Valerie Lynch-Holm, Vincent Franceschi, and the staff at the Electron Microscopy Center at Washington State University.
This work was supported by grant AI20190 from the National Institutes of Health (NIAID).
Footnotes
This paper is dedicated to the memory of Louis P. Mallavia.
REFERENCES
- 1.Akporiaye E T, Rowatt J D, Aragon A A, Baca O G. Lysosomal response of a murine macrophage-like cell line persistently infected with Coxiella burnetii. Infect Immun. 1983;40:1155–1162. doi: 10.1128/iai.40.3.1155-1162.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babior B M. The respiratory burst of phagocytes. J Clin Investig. 1984;73:599–601. doi: 10.1172/JCI111249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baca O G, Akporiaye E T, Rowatt J D. Possible biochemical adaptations of Coxiella burnetii for survival within phagocytes: effect of antibody. In: Leive L, Schlessinger D, editors. Microbiology—1984. Washington, D.C: American Society for Microbiology; 1984. pp. 269–272. [Google Scholar]
- 4.Barnewall R E, Rikihisa Y. Abrogation of gamma interferon-induced inhibition of Ehrlichia chaffeensis infection in human monocytes with iron transferrin. Infect Immun. 1994;62:4804–4810. doi: 10.1128/iai.62.11.4804-4810.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnewall R E, Rikhisa Y, Lee E H. Erlichia chaffeensis inclusions are early endosomes which selectively accumulate transferrin receptor. Infect Immun. 1997;65:1455–1461. doi: 10.1128/iai.65.4.1455-1461.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhardwaj N, Nash T W, Horwitz M A. Interferon-γ-activated human monocytes inhibit the intracellular multiplication of Legionella pneumophila. J Immunol. 1986;137:2662–2669. [PubMed] [Google Scholar]
- 7.Bleil J D, Bretscher M S. Transferrin receptor and its recycling in HeLa cells. EMBO J. 1982;1:351–355. doi: 10.1002/j.1460-2075.1982.tb01173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burton P R, Kordova N, Paretsky D. Electron microscopic studies of the rickettsia Coxiella burnetii: entry, lysosomal response, and fate of rickettsial DNA in L-cells. Can J Microbiol. 1970;17:143–150. doi: 10.1139/m71-025. [DOI] [PubMed] [Google Scholar]
- 9.Byrd T F, Horwitz M A. Lactoferrin inhibits or promotes Legionella pneumophila intracellular multiplication in nonactivated and interferon gamma-activated human monocytes depending upon its degree of iron saturation. J Clin Investig. 1991;88:1103–1112. doi: 10.1172/JCI115409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byrd T F, Horwitz M A. Interferon gamma-activated human monocytes downregulate transferrin receptors and inhibit the intracellular multiplication of Legionella pneumophila by limiting the availability of iron. J Clin Investig. 1989;83:1457–1465. doi: 10.1172/JCI114038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cornelissen C N, Sparling P F. Iron piracy: acquisition of transferrin-bound iron by bacterial pathogens. Mol Microbiol. 1994;14:843–850. doi: 10.1111/j.1365-2958.1994.tb01320.x. [DOI] [PubMed] [Google Scholar]
- 12.Dautry-Varsat A, Ciechanover A, Lodish H F. pH and the recycling of transferrin during receptor-mediated endocytosis. Proc Natl Acad Sci USA. 1983;80:2258–2262. doi: 10.1073/pnas.80.8.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fortier A H, Leiby D A, Narayanan R B, Asafoadjei E, Crawford R M, Nancy C A, Meltzer M S. Growth of Francisella tularensis LVS in macrophages: the acidic intracellular compartment provides essential iron required for growth. Infect Immun. 1995;63:1478–1483. doi: 10.1128/iai.63.4.1478-1483.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friis R R. Interaction of L cells and Chlamydia psittaci: entry of the parasite and host responses to its development. J Bacteriol. 1972;110:706–721. doi: 10.1128/jb.110.2.706-721.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gebran S J, Newton C, Yamamoto Y, Widen R, Klein T W, Friedman H. Macrophage permissiveness for Legionella pneumophila growth modulated by iron. Infect Immun. 1994;62:564–568. doi: 10.1128/iai.62.2.564-568.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gimenez D F. Staining rickettsiae in yolk-sac cultures. Stain Technol. 1964;39:135–140. doi: 10.3109/10520296409061219. [DOI] [PubMed] [Google Scholar]
- 17.Goren M B, D’Arcy Hart P, Young M R, Armstrong J A. Prevention of phagosome-lysosome fusion in cultured macrophages by sulfatides of Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 1976;73:2510–2514. doi: 10.1073/pnas.73.7.2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guillard J, Berche P, Mounier J, Richard S, Sansonetti P. In vitro model of penetration and intracellular growth Listeria monocytogenes in the human enterocyte-like cell line Caco-2. Infect Immun. 1987;55:2822–2829. doi: 10.1128/iai.55.11.2822-2829.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hackstadt T, Williams J C. Biochemical stratagem for obligate parasitism of eukaryotic cells by Coxiella burnetii. Proc Natl Acad Sci USA. 1981;5:3240–3244. doi: 10.1073/pnas.78.5.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hale T L, Moris R E, Bonventre P F. Shigella infection of Henle intestinal epithelial cells: role of the host cell. Infect Immun. 1979;24:887–894. doi: 10.1128/iai.24.3.887-894.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harding C, Heuser J, Stahl P. Receptor-mediated endocytosis of transferrin and recycling of the transferrin receptor in rat reticulocytes. J Cell Biol. 1983;97:329–339. doi: 10.1083/jcb.97.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hechemy K E, McKee M, Marko M, Samsonoff W A, Roman M, Baca O. Three-dimensional reconstruction of Coxiella burnetii-infected L929 cells by high-voltage electron microscopy. Infect Immun. 1993;61:4485–4488. doi: 10.1128/iai.61.10.4485-4488.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heinzen R A, Scidmore M A, Rockey D D, Hackstadt T. Differential interaction with endocytic and exocytic pathways distinguish parasitophorous vacuoles of Coxiella burnetii and Chlamydia trachomatis. Infect Immun. 1996;64:796–809. doi: 10.1128/iai.64.3.796-809.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hentze M W, Kuhn L C. Molecular control of vertebrate iron metabolism: mRNA-based regulatory circuits operated by iron, nitric oxide, and oxidative stress. Proc Natl Acad Sci USA. 1996;93:8175–8182. doi: 10.1073/pnas.93.16.8175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hopkins C R. Intracellular routing of transferrin and transferrin receptors in epidermoid carcinoma A431 cells. Cell. 1983;35:321–330. doi: 10.1016/0092-8674(83)90235-0. [DOI] [PubMed] [Google Scholar]
- 26.Horwitz M A. The Legionnaires disease bacterium (Legionella pneumophila) inhibits phagosome-lysosome fusion in human monocytes. J Exp Med. 1983;158:2108–2126. doi: 10.1084/jem.158.6.2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iyengar R, Stuehr D J, Marletta M A. Macrophage synthesis of nitrite, nitrate, and N-nitrosamines: precursors and role of the respiratory burst. Proc Natl Acad Sci USA. 1987;84:6369–6373. doi: 10.1073/pnas.84.18.6369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klausner R D, Ashwell G, van Renswoude J, Harford J B, Bridges K R. Binding of apotransferrin to K562 cells: explanation of the transferrin cycle. Proc Natl Acad Sci USA. 1983;80:2263–2266. doi: 10.1073/pnas.80.8.2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kura F, Suzuki K, Watanabe H, Akamatsu Y, Amano F. Difference in Legionella pneumophila growth permissiveness between J774A.1 murine macrophage-like JA-4 cells and lipopolysaccharide (LPS)-resistant mutant cells, LPS1916, after stimulation with LPS. Infect Immun. 1994;62:5419–5423. doi: 10.1128/iai.62.12.5419-5423.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laemmli U K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 31.Lalonde R G, Holbein B E. Role of iron in Trypanosoma cruzi infection in mice. J Clin Investig. 1984;73:470–476. doi: 10.1172/JCI111233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lesley J, Hyman R, Schulte R, Trotter J. Expression of transferrin receptor on murine hematopoietic progenitors. Cell Immunol. 1984;83:14–25. doi: 10.1016/0008-8749(84)90220-x. [DOI] [PubMed] [Google Scholar]
- 33.Lestas A N. The effect of pH upon human transferrin: selective labeling of the two iron-binding sites. Br J Hematol. 1976;32:341–350. doi: 10.1111/j.1365-2141.1976.tb00937.x. [DOI] [PubMed] [Google Scholar]
- 34.Loo V G, Lalonde R G. Role of iron in intracellular growth of Trypanosoma cruzi. Infect Immun. 1984;45:726–730. doi: 10.1128/iai.45.3.726-730.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maurin M, Benoliel A M, Bongrand P, Raoult D. Phagolysosomes of Coxiella burnetii-infected cell lines maintain an acidic pH during persistent infection. Infect Immun. 1992;60:5013–5016. doi: 10.1128/iai.60.12.5013-5016.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCord J M, Day E D. Superoxide-dependent production of hydroxyl radical catalyzed by iron-EDTA complex. FEBS Lett. 1978;86:139–142. doi: 10.1016/0014-5793(78)80116-1. [DOI] [PubMed] [Google Scholar]
- 37.Murray M J, Murray A B, Murray M B, Murray C J. The adverse effect of iron repletion on the course of certain infections. Br Med J. 1978;2:1113–1115. doi: 10.1136/bmj.2.6145.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nathan C F, Murray H W, Wiebe M E, Rubin B Y. Identification of interferon-γ as the lymphokine that activates human macrophage oxidative metabolism and antimicrobial activity. J Exp Med. 1983;158:670–689. doi: 10.1084/jem.158.3.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nunez M T, Gaete V, Watkins J A, Glass J. Mobilization of iron from endocytic vesicles. J Biol Chem. 1989;265:6688–6692. [PubMed] [Google Scholar]
- 40.Ormsbee R A, Peacock M G. Rickettsial plaques assay and cloning procedure. Tissue Cult Assoc. 1976;2:475–478. [Google Scholar]
- 41.Owen D, Kuhn L C. Noncoding 3′ sequences of the transferrin receptor gene are required for mRNA regulation by iron. EMBO J. 1987;6:1287–1293. doi: 10.1002/j.1460-2075.1987.tb02366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rabinovitch M, Veras P S T. Cohabitation of Leishmania amazonensis and Coxiella burnetii. Trends Microbiol. 1996;4:158–161. doi: 10.1016/0966-842x(96)10027-5. [DOI] [PubMed] [Google Scholar]
- 43.Ramm G A, Powell L W, Halliday J W. Pathways of intracellular trafficking and release of ferritin by the liver in vivo: the effect of chloroquine and cytochalasin D. Hepatology. 1994;19:504–513. [PubMed] [Google Scholar]
- 44.Raventos-Suarez C, Pollack S, Nagel R L. Plasmodium falciparum: inhibition of in vitro growth by desferrioxamine. J Trop Med Hyg. 1982;31:919–922. doi: 10.4269/ajtmh.1982.31.919. [DOI] [PubMed] [Google Scholar]
- 45.Reeves M W, Pine L P, Neilands J B, Balows A. Absence of siderophore activity in Legionella species grown in iron-deficient media. J Bacteriol. 1983;154:324–329. doi: 10.1128/jb.154.1.324-329.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reiner N E. Altered cell signaling and mononuclear phagocyte deactivation during intracellular infection. Immun Today. 1994;15:374–381. doi: 10.1016/0167-5699(94)90176-7. [DOI] [PubMed] [Google Scholar]
- 47.Rothman R J, Serroniand A, Faber J L. Cellular pool of transient ferric iron, chelatable by deferoxamine and distinct from ferritin, that is involved in oxidative cell injury. Mol Pharmacol. 1992;42:703–710. [PubMed] [Google Scholar]
- 48.Samuel J E, Frazier M E, Mallavia L P. Correlation of plasmid type and disease caused by Coxiella burnetii. Infect Immun. 1985;49:775–779. doi: 10.1128/iai.49.3.775-779.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sansonetti P J, Ryan A, Clerc P, Maurelli A T, Mourier J. Multiplication of Shigella flexneri within HeLa cells: lysis of the phagocytic vacuole and plasmid-mediated contact hemolysis. Infect Immun. 1986;51:461–469. doi: 10.1128/iai.51.2.461-469.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sutherland R, Delia D, Schneider C, Newman R, Kemshead J, Greaves M. Ubiquitous cell-surface glycoprotein on tumor cells is proliferation-associated receptor for transferrin. Proc Natl Acad Sci USA. 1981;78:4515–4519. doi: 10.1073/pnas.78.7.4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taetle R, Honeysett J M. γ-Interferon modulates human monocyte/macrophage transferrin receptor expression. Blood. 1988;71:1590–1595. [PubMed] [Google Scholar]
- 52.Veras P S T, de Chastellier C, Moreau M, Villiers V, Thibon M, Mattei D, Rabinovitch M. Fusion between large phagocytic vesicles: targeting of yeast and other particulates to phagolysosomes that shelter the bacterium Coxiella burnetii or the protozoan Leishmania amazonensis in Chinese hamster ovary cells. J Cell Sci. 1994;107:3065–3076. doi: 10.1242/jcs.107.11.3065. [DOI] [PubMed] [Google Scholar]
- 53.Veras P S T, Moulia C, Dauguet C, Tunis C T, Thibon M, Rabinovitch M. Entry and survival of Leishmania amazonensis amastigotes within phagolysosome-like vacuoles that shelter Coxiella burnetii in Chinese hamster ovary cells. Infect Immun. 1995;63:3502–3506. doi: 10.1128/iai.63.9.3502-3506.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weiss G, Wachter H, Fuchs D. Linkage of cell mediated immunity to iron metabolism. Immunol Today. 1995;16:495–500. doi: 10.1016/0167-5699(95)80034-4. [DOI] [PubMed] [Google Scholar]
- 55.Wyrick P B, Brownridge E A. Growth of Chlamydia psittaci in macrophages. Infect Immun. 1978;19:1054–1060. doi: 10.1128/iai.19.3.1054-1060.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]