Dear Editor:
Medical emergencies, such as vasovagal syncope (VVS), anaphylaxis, and choking, can occur suddenly during dental treatment, regardless of whether the patient has an underlying disease. Dental providers are required to manage these emergencies promptly and appropriately. Simulation training has been the only effective means whereby dental providers can learn to deal with medical emergencies without risking their lives of the patient [1]. Although the utility of simulations based on humanoid simulators, such as high-fidelity mannequins or robot patients, has been reported, the purchasing or developing these simulators is expensive [1]. As an alternative approach, Sanuki et al. have provided dental students with a screen-based simulator using a smartphone-/tablet-compatible vital sign simulation app. (SimMon; Castle+Andersen ApS, Hillerød, Denmark) and reported an improvement in the confidence of students in managing medical emergencies [2]. Compared with humanoid simulators, SimMon is inexpensive, costing approximately 23 USD at the Apple App Store (price as of October 2024), and enables users to freely set vital signs such as heart rate (HR), blood pressure (BP), and arterial oxygen saturation (SpO2) on a screen that mimics a patient monitor. These simulations can be stored anywhere on a device with the app and downloaded. We conducted an online screen-based simulation (screen-based telesimulation) using SimMon, and in this letter, we provide an overview of this approach and report on its utility.
Twelve dental providers from two dental clinics in Japan (three dentists, two dental hygienists, and seven dental assistants) participated in the simulation. One month before the simulation, the participants were provided with a video produced by the authors and were instructed to study it thoroughly until the day of the simulation. In the video, a board-certified dental anesthesiology specialist (BCDAS) explained the pathology, symptoms, diagnosis, and treatment of VVS, anaphylaxis, and choking during dental treatment.
On the simulation day, the learners and a BCDAS educator participated in an online meeting using Zoom (Zoom Video Communications, Inc., San Jose, CA, USA). Using the recording functions in Zoom, the entire simulation was recorded on video, and provided to all learners at a later date as review materials. The learners were initially provided with a link to an online questionnaire created using Google Forms, which was designed to assess their understanding of the management of VVS, anaphylaxis, and choking (pre-questionnaire) based on a 10-point numerical rating scale (NRS), in which scores of 0 and 10 indicated no understanding and complete understanding, respectively. Informed consent to participate in the survey was obtained from all learners using the same form. After the pre-questionnaire, using the screen-sharing function of Zoom, the learners were presented with a scenario of a simulated patient whose condition suddenly changed during dental treatment. The following is an example of a scenario of a simulated patient who developed VVS. A 32-year-old woman reported cold sweats and feeling sick immediately after receiving local anesthesia for a pulpectomy, and her vital signs (HR, BP, SpO2, and respiratory rates) were subsequently displayed on the screen using SimMon installed on an iPad (Fig. 1). Learners were instructed by the educator to correctly diagnose the medical condition of the patient based on the scenario and vital signs and to select an appropriate treatment. When the learners selected to administer drugs or change the position of the patient, the educator changed the vital signs of the simulated patient using SimMon. For example, if the learners selected to administer oxygen, the SpO2 value was increased. Learners could consult with one another, and when unsure of a decision, the educator gave hints regarding diagnosis and treatment, which enabled the learners to play a central role in determining the management methods. The simulation ended when the simulated symptoms of the patient and vital signs improved. The educator then provided feedback to the learners to review their knowledge of diagnosis and treatment during medical emergencies. Learners participated in three screen-based simulations (approximately 90 min) based on VVS, anaphylaxis, and choking scenarios. After completing all simulations, the learners’ understanding of the management of each medical emergency was evaluated. Their satisfaction with the screen-based simulation was measured using an NRS (0 = completely unsatisfied, 10 = completely satisfied) (post-questionnaire). The pre- and post-questionnaire NRS scores were compared using the Wilcoxon t-test, with significant differences at the P < 0.05.
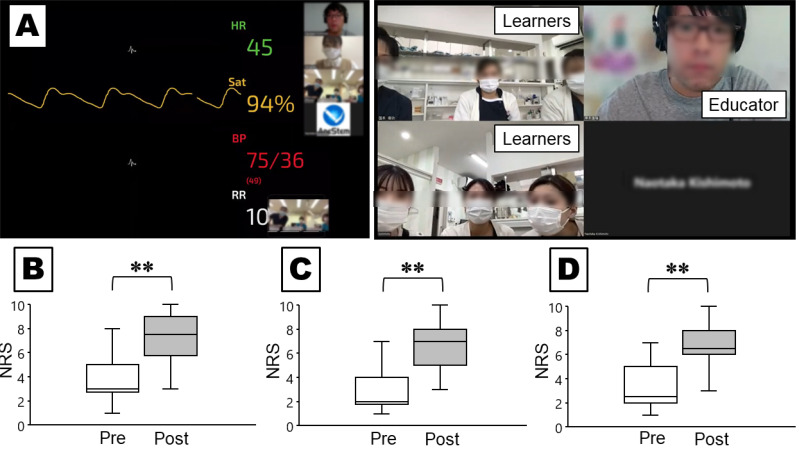
Fig. 1. (A) Screen-based telesimulation in a dental clinic using Zoom (Zoom Video Communications, Inc., San Jose, CA, USA). Vital signs were generated using SimMon (Castle+Andersen ApS, Hillerød, Denmark) for a simulated patient experiencing a medical emergency (Left). Video feedback after the simulation training between the educator and learners (Right). Comparison of the scores for understanding the management of vasovagal syncope (B), anaphylaxis (C), and choking (D) before and after the simulation. **P < 0.01. Pre = pre-questionnaire; Post = post-questionnaire.
Figure 1 shows a comparison of the pre- and post-questionnaire results. The post-questionnaire scores for understanding the management of VVS (median, 7.5; interquartile range [IQR], 5.75–9) were significantly higher than the pre-questionnaire scores (median, 3; IQR, 2.75–5) (P < 0.01). Similarly, the post-questionnaire scores for understanding the management of anaphylaxis (median, 7; IQR, 5–8) were significantly higher than the pre-questionnaire scores (median, 2; IQR, 1.75–4) (P < 0.01), and the post-questionnaire scores for understanding the management of choking (median, 6.5; IQR, 6–8) were significantly higher than the pre-questionnaire scores (median, 2.5; IQR, 2–5) (P < 0.01). Moreover, the median score for satisfaction with the screen-based simulation was 9 (IQR, 7.5–10).
Screen-based simulation has certain advantages, its low cost, as it does not require a humanoid simulator and its accessories. Additionally, it does not necessitate a specific venue for the simulation or storage of the simulator, and it can be performed with almost no time or location restrictions as long as a computer or mobile device is available [3]. Consequently, it has been applied in various medical education situations; for example, for medical students to learn the management of anaphylaxis and heart failure [4] and for critical care fellows to understand electroencephalography [5]. To the best of our knowledge, our screen-based telesimulation for dental providers that enables these individuals to learn the management of medical emergencies is the first of its kind, and it was demonstrated to enhance dental providers’ understanding of the management of VVS, anaphylaxis, and choking, with the learners’ reporting a high level of satisfaction with this method of learning, thereby indicating its utility as a tool that can contribute to improving the clinical management of medical emergencies.
ACKNOWLEDGMENT
The authors would like to thank Dr. Masanori Sakurai and Dr. Toshinori Kunimoto for their cooperation in holding the screen-based simulation training.
Footnotes
- Naotaka Kishimoto: Conceptualization, Data curation, Writing – original draft.
- Toru Yamamoto: Writing – review & editing.
- Simon D Tran: Supervision.
- Takuro Sanuki: Writing – review & editing.
- Kenji Seo: Supervision.
DECLARATIONS OF INTEREST: None.
References
- 1.Kishimoto N, Sanuki T, Liu Y, Tran SD, Seo K. Simulation training for medical emergencies of dental patients: A review of the dental literature. Jpn Dent Sci Rev. 2023;59:104–113. doi: 10.1016/j.jdsr.2023.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanuki T, Komasawa N, Kurata S, Ayuse T. Efficacy of simulation application SimMon for emergency response training. Am J Emerg Med. 2016;34:927–928. doi: 10.1016/j.ajem.2016.02.044. [DOI] [PubMed] [Google Scholar]
- 3.Nelson CK, Schwid HA. Screen-based simulation for anesthesiology. Int Anesthesiol Clin. 2015;53:81–97. doi: 10.1097/AIA.0000000000000076. [DOI] [PubMed] [Google Scholar]
- 4.Tan GM, Ti LK, Tan K, Lee T. A comparison of screen-based simulation and conventional lectures for undergraduate teaching of crisis management. Anaesth Intensive Care. 2008;36:565–569. doi: 10.1177/0310057X0803600411. [DOI] [PubMed] [Google Scholar]
- 5.Fahy BG, Vasilopoulos T, Chau DF. Use of flipped classroom and screen-based simulation for interdisciplinary critical care fellow teaching of electroencephalogram interpretation. Neurocrit Care. 2020;33:298–302. doi: 10.1007/s12028-020-00985-5. [DOI] [PubMed] [Google Scholar]