Abstract
Many patients with underlying medical conditions are treated with local anesthetics in dental clinics. Dental local anesthetic cartridges contain the vasoconstrictor adrenaline, which can affect the cardiovascular system. For this reason, the adrenaline in the cartridge (2% lidocaine + 1:80,000 adrenaline) is sometimes diluted in order to avoid hemodynamic changes in these patients. However, at the same time, considerations have to be made for coring. Coring is a process in which a piece of rubber is scraped off when a needle is inserted into a rubber stopper, and the rubber is mixed with the drug solution. Particles generated during the coring process contaminate local anesthetic solutions. In this study, we closely observed the puncture site of a 33G dental needle inside a cartridge to investigate a safe dilution method that considers coring. The puncture site was located within 1.50 ± 0.08 mm (mean ± SD) of the diameter from the center of the rubber stopper of the cartridge head. Punctures were made with a 0.75-mm outer diameter metal needle outside the 1.50-mm diameter range from the center of the rubber stopper to reduce the overlap between puncture sites and minimize the risk of coring. After discarding half of the cartridge, 2% lidocaine without adrenaline was injected by piercing the end of the rubber stopper at the cartridge head with a 22–27G metal needle (outer diameter approximately 0.4–0.7 mm). This method minimizes the risk of rubber displacement and coring while ensuring a safe and effective dilution process. Providing a safer method for adrenaline dilution reduces the risk of coring and contamination in dental anesthetic cartridges.
Keywords: Adrenaline, Cartridge, Coring, Dental Anesthesia, Dilution Technique, Local Anesthesia
INTRODUCTION
Many patients with underlying medical conditions are administered local dental anesthetics when visiting dental clinics [1]. However, these anesthetics tend to contain adrenaline, a vasoconstrictor, whose exposure should be minimized in patients with cardiovascular diseases, including hypertension, ischemic heart disease, and obstructive hypertrophic cardiomyopathy [2,3]. This highlights the need to establish a consensus on safe dental care using local dental anesthetics in patients with underlying diseases [1,4,5,6].
Because adrenaline in dental local anesthetic cartridges may affect circulatory dynamics in patients with cardiovascular disease owing to its systemic effects, methods aimed at diluting the adrenaline concentration of these cartridges have been reported [7]. In Japan, local dental anesthetics include lidocaine plus adrenaline, propylocaine (prilocaine), felypressin, and mepivacaine without vasoconstrictors [8]. Adrenaline acts primarily on the pulpal arteries, whereas felypressin acts on the pulpal veins. Therefore, adrenaline is a stronger vasoconstrictor and has a longer duration of action than felypressin [8]. It has been reported that 3% propitocaine (prilocaine) with 0.03 IU/mL felypressin may be appropriate for patients who cannot tolerate tachycardia [4]. The use of 3% mepivacaine without vasoconstrictors is safer than 2% lidocaine with 1:100,000 adrenaline in controlling elevated heart rate but has a poorer anesthetic success rate [9]. However, lidocaine plus adrenaline is primarily used in Japanese dental clinics.
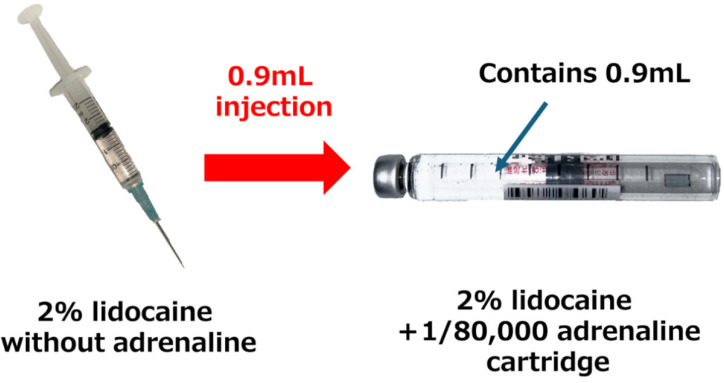
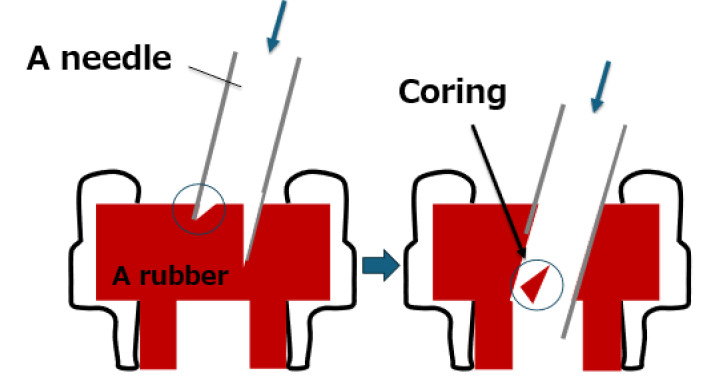
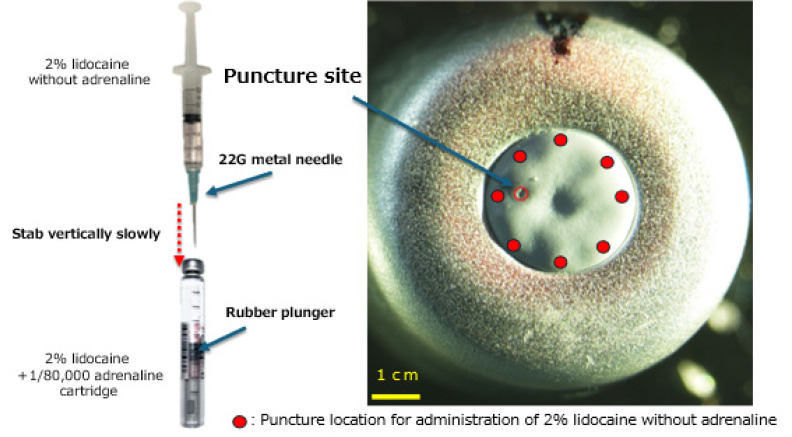
In Japan, local anesthesia for dental treatment is often administered using special glass cartridges [7]. The total adrenaline in the cartridge can be diluted by discarding half of the cartridge (2% lidocaine + 1:80,000 adrenaline; A80) and filling the cartridge with 2% lidocaine without adrenaline (Fig. 1) [7]. Although selecting anesthesia cartridges that already have the appropriate adrenaline dilution (1:100,000 and 1:200,000) would be ideal for safety and waste reduction, these are not available in Japan. However, this process increases the likelihood of coring, a phenomenon in which rubber from the cartridge is scraped off and mixed with an anesthetic solution (Fig. 2) [7].
Fig. 1. Adrenaline dilution for dental local anesthetic cartridges. The adrenaline in the cartridge was diluted by injecting 0.9 mL of 2% lidocaine without adrenaline into 0.9 mL of a dental local anesthetic cartridge (2% lidocaine + 1/80,000 adrenaline).
Fig. 2. Coring. Coring is a phenomenon in which when an injection needle is inserted into the rubber stopper of an infusion or vial, a portion of the rubber stopper (a piece of rubber) is scraped off and mixed into the drug solution.
In this study, we closely observed the puncture site of a 33G dental needle inside a cartridge and determined the optimal technique to reduce the risk of coring during adrenaline dilution to establish a safe dilution method that prevents coring.
METHODS
1. Materials
We used 100 cartridges (five registration numbers, 20 cartridges each) of dental local anesthetics (ORA Injection Dental Cartridge 1.8 mL; GC Showa Yakuhin Co., Ltd, Tokyo, Japan) injected with a 33G dental injection needle (NIProject Dental Needle; NIPRO CORPORATION, Osaka, Japan). The rubber stopper in the cartridge was made of gray butyl rubber, and the 33G needle, commonly used in dental anesthetic procedures, had an outer diameter of approximately 0.21 mm.
2. Methods
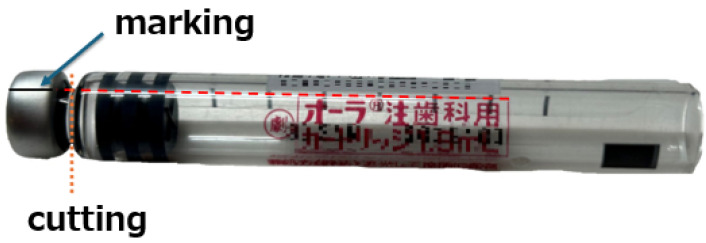
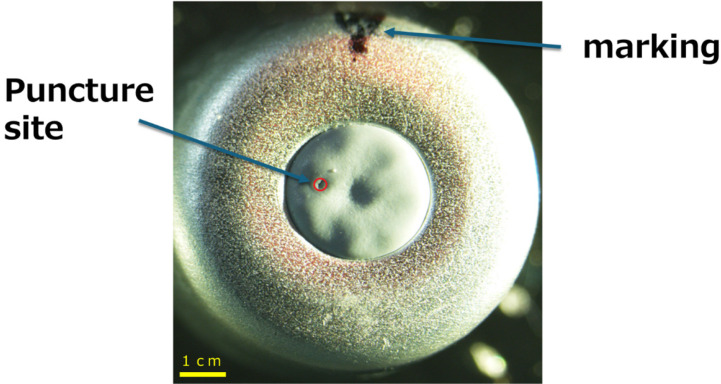
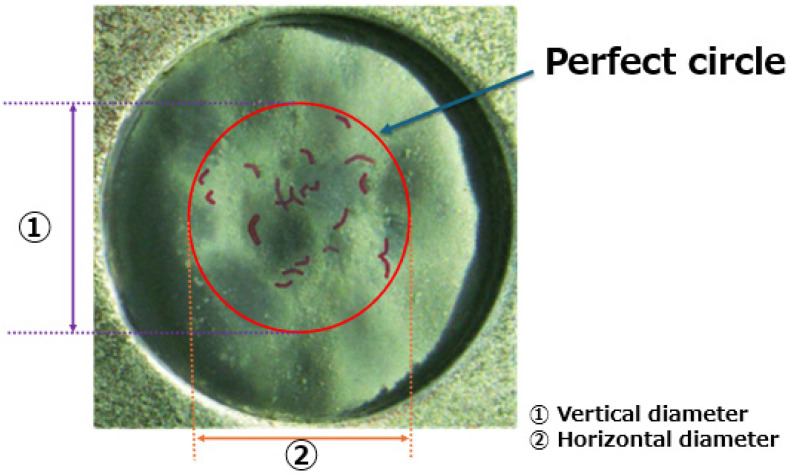
The head of the dental local anesthetic cartridge was marked to determine its location and the cartridge head was cut with a laboratory bar (Fig. 3). Subsequently, images were obtained using a stereomicroscope (SZX16; Olympus, Tokyo, Japan) to observe the puncture site of the rubber plug with reference to the marked position (Fig. 4). After marking the puncture site on each image, 20 images for each registration number were superimposed using Adobe Photoshop Elements 14. Based on the 20 puncture sites, a regular circle was drawn on the superimposed images, and the vertical and horizontal diameters (mm) of the regular circle were measured (Fig. 5). Twenty images per registration number were selected based on a preliminary analysis, which indicated that this sample size provided an optimal balance between statistical power and image clarity.
Fig. 3. Marking and cutting positions in cartridges. The marking positions were set by referring to the cartridge labels to capture photographs that overlapped the 20 cartridges. After the marking, the neck of the cartridge was removed.
Fig. 4. Puncture site of the cartridge rubber stopper. Images were taken so that the markings were positioned on top of the image, and the puncture site could be clearly observed.
Fig. 5. An example of 20 image superimpositions and measurement items. After coloring the puncture sites in each of the 20 images, the images were superimposed. A perfect circle was drawn on the superimposed image and its vertical and horizontal diameters were measured.
3. Statistical analysis
All values are expressed as the mean ± standard deviation (SD). We used Microsoft 365® Excel for statistical analyses. Unpaired t-tests were used to determine whether there were differences between the average vertical and horizontal diameters obtained from the five images (20 superimposed images). The significance level was set at P < 0.05.
RESULTS
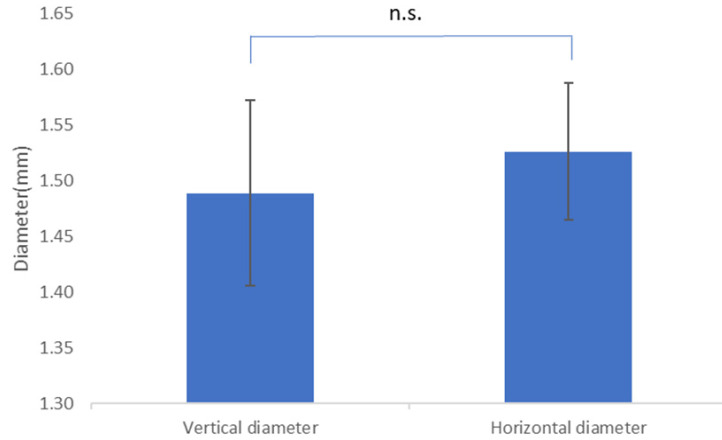
The diameters of the regular circles were 1.49 ± 0.08 mm (n = 5) and 1.53 ± 0.06 mm (n = 5) for vertical and horizontal diameters, respectively. No significant differences were observed between the vertical and horizontal diameters (P > 0.05, unpaired t-test) (Fig. 6). The average diameter of the circle (vertical + horizontal) was 1.50 ± 0.08 mm (n = 10).
Fig. 6. Comparison of vertical and horizontal diameters (mm) of puncture circles. The vertical and horizontal diameters were measured from five overlapping images, and the mean and standard deviations were calculated. The results were 1.49 ± 0.08 mm (mean ± SD, n = 5) for the vertical and 1.53 ± 0.06 mm (mean ± SD, n = 5) for the horizontal, with no significant statistical difference (P > 0.05). N, number; n.s., no significant; SD, standard deviation.
DISCUSSION
1. Coring
Coring, whereby rubber strips enter the body through a vein, can cause pulmonary infarction, cerebral infarction, regional tissue infarction, pulmonary granuloma, and even death in some cases [10,11]. In this study, the diameter of the circle (vertical and horizontal) was 1.50 ± 0.08 mm. Thus, a second needle puncture of 1.42–1.58 mm in diameter from the center of the rubber stopper would increase the likelihood of coring due to overlapping puncture sites. Therefore, to minimize coring, a ≤ 22G metal needle was used for refilling and puncturing. Puncturing was performed at least 0.75 mm away from the initial puncture site to avoid overlapping.
The factors that cause coring are: (1) the use of an obtuse needle; (2) an oblique puncture; (3) repeated punctures at the same site, although the puncture angle (45° or 90°) does not affect the occurrence of coring [11,12]. Although coring has not been reported with local anesthetics for dental use, it occurs in vials of propofol and rocuronium, which are frequently used in dental anesthesia, using various needle sizes (18G, 20G, and 21G) [11]. In particular, larger gauge needles have been reported to be a factor influencing coring after puncturing rubber vial stoppers multiple times, regardless of the puncture angle [11]. In Japan, coring became a major issue in 2021 when microscopic black material was detected in COVID-19 vaccine vials [13]. Additionally, coring is an important issue with dental local anesthetic cartridges because of their small size and the masking effect of the label, which makes visualization difficult [14].
Our study provides concrete measurements for the optimal puncture diameter (1.50 ± 0.08 mm), highlighting the increased likelihood of coring with repeated punctures in close proximity. However, while our findings suggest that puncture overlap within the range of 1.42–1.58 mm increases the risk of coring, the variability in rubber stopper materials across different manufacturers may influence the generalizability of these results.
2. Safe puncture position during adrenaline dilution
The vertical and horizontal diameters were measured correctly. The diameter of the regular circle is 1.50 ± 0.08 mm (n = 10), indicating that the length from the rubber plug (approximately 3 mm in diameter) at the cartridge head to the regular circle is approximately 0.75 mm (Fig. 7).
Fig. 7. Safe needle positions for adrenaline dilution. Slowly and vertically pierce the end of the cartridge rubber stopper. with a 22–27G metal needle (outer diameter approximately 0.4–0.7 mm).
The smaller the needle thickness, the smaller the percentage of coring; however, when coring occurs, the foreign body (rubber piece) becomes smaller and more difficult to detect [14]. However, because the rubber stopper on the head of the dental local anesthetic cartridge is smaller and thinner than the infusion or vial formulation, puncturing should be performed slowly and vertically using a ≤22G metal needle to avoid coring. Another method involves puncturing using a rubber plunger (Fig. 7), which is thicker than the rubber plugs on the head side, thereby increasing the incidence of coring [11]. Even if a long and thin metal needle is used for injection, the rubber plunger is likely to be displaced when the needle is withdrawn from the rubber stopper, rendering the cartridge inoperable.
In this study, a safe dilution method that takes into consideration coring was established. After discarding half of the cartridge, 2% lidocaine without adrenaline should be injected by piercing the end of the rubber stopper at the cartridge head with a 22–27G metal needle (outer diameter approximately 0.4–0.7 mm). Particles generated during the coring process contaminate local anesthetic solutions, the analysis of which is also important.
Footnotes
- Takutoshi Inoue: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing.
- Toru Yamamoto: Writing – review & editing.
DECLARATIONS OF INTEREST: The authors declare no conflicts of interest regarding the publication of this letter.
References
- 1.Katakura A. Necessity of providing dental care to medically compromised patients in Japan’s super-aged society and the way forward. Jpn Dent Sci Rev. 2022;58:279–285. doi: 10.1016/j.jdsr.2022.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Declouxa D, Ouanounoub A. Local anaesthesia in dentistry: a review. Int Dent J. 2020;71:87–95. doi: 10.1111/idj.12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karm MH, Kim M, Park FD, Seo KS, Kim HJ. Comparative evaluation of the efficacy, safety, and hemostatic effect of 2% lidocaine with various concentrations of epinephrine. J Dent Anesth Pain Med. 2018;18:143–149. doi: 10.17245/jdapm.2018.18.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kyosaka Y, Owatari T, Inokoshi M, Kubota K, Inoue M, Minakuchi S. Cardiovascular comparison of 2 types of local anesthesia with vasoconstrictor in older adults: a crossover study. Anesth Prog. 2019;66:133–140. doi: 10.2344/anpr-66-02-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho JTF, van Riet TCT, Afrian Y, Sem KTHCJ, Spijker R, de Lange J, et al. Adverse effects following dental local anesthesia: a literature review. J Dent Anesth Pain Med. 2021;21:507–525. doi: 10.17245/jdapm.2021.21.6.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seminario-Amez M, González-Navarro B, Ayuso-Montero R, Jané-Salas E, López-López J. Use of local anesthetics with a vasoconstrictor agent during dental treatment in hypertensive and coronary disease patientspatients. a systematic review. J Evid Based Dent Pract. 2021;21:101569. doi: 10.1016/j.jebdp.2021.101569. [DOI] [PubMed] [Google Scholar]
- 7.Inoue T, Yamamoto T. Adrenaline dilution in dental local anesthesia for patients with underlying disease. J Dent Anesth Pain Med. 2024;24:297–299. doi: 10.17245/jdapm.2024.24.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tachibana K, Kasahara M, Matsuura N, Ichinohe T. Effects of local anesthetics with vasoconstrictors on dental pulp blood flow and oxygen tension. Anesth Prog. 2021;68:214–219. doi: 10.2344/anpr-68-02-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su N, Liu Y, Yang X, Shi Z, Huang Y. Efficacy and safety of mepivacaine compared with lidocaine in local anaesthesia in dentistry: a meta-analysis of randomised controlled trials. Int Dent J. 2014;64:96–107. doi: 10.1111/idj.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campagna R, Pessis E, Guerini H, Feydy A, Drapé JL. Occurrence of coring after needle insertion through a rubber stopper: study with prednisolone acetate. Eur Radiol. 2013;23:424–427. doi: 10.1007/s00330-012-2602-3. [DOI] [PubMed] [Google Scholar]
- 11.Chotikawanich T, Kammee T, Khantee S. The impact of needle size and angle on rubber coring after multiple puncturing of multi-dose propofol vial rubber stoppers. Heliyon. 2022;8:e09389. doi: 10.1016/j.heliyon.2022.e09389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mateen MA, Dwivedi D, De A, Haldar A. Fragmentation and coring of a vial – an avoidable threat. Indian J Anaesth. 2023;67:945–947. doi: 10.4103/ija.ija_941_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chooi WH, Ng PW, Hussain Z, Ming LC, Ibrahim B, Koh D. Vaccine contamination: Causes and control. Vaccine. 2022;40:1699–1701. doi: 10.1016/j.vaccine.2022.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hruska JL, Saasouh W, Alhamda MS. Coring revisited: a case report and literature review. Cureus. 2022;14:e29750. doi: 10.7759/cureus.29750. [DOI] [PMC free article] [PubMed] [Google Scholar]