Abstract
We report a case of complicated isolated infrarenal abdominal aortic dissection (IAAD) that was treated with stent graft. A 79-year-old man presented with acute bilateral lower limb pain. A contrast-enhanced CT performed 2 h later revealed sever stenosis of infrarenal abdominal aorta due to IAAD. Angiography identified a primary tear just below the upper end of the IAAD. A smaller stent graft was placed distally to avoid stent graft–induced new entry, and a large stent graft was placed proximally to cover the primary entry. The stenosis improved immediately after the procedure, and pain relief was achieved. Stent graft placement for entry closure appeared to be an effective for IAAD.
Keywords: stent graft, IAAD, stenosis
Introduction
Isolated abdominal aortic dissection (IAAD) is rare, accounting for 1.3% of all aortic dissections. 1 Stenosis due to an IAAD lesion is uncommon complication, with only a small number of cases reported. 2 In such cases, surgery, such as aortic repair or bypass surgery, is typically performed before stent grafting. Recently, endovascular stent grafts have been used to treat thoracic aortic dissection by placing the graft across the primary entry tear. 3 However, the effects of entry closure with a stent graft for IAAD are unclear. We reported a case in which IAAD with stenosis was treated with endovascular stent graft placement for entry closure.
Case
A man in his 70s presented with acute pain in both lower limbs. He had a history of hypertension and bladder cancer. Blood tests revealed a lactic acid level of 44 mg/dL and a creatine kinase level of 326 U/L. Blood pressure in his lower limbs could not be measured. A contrast-enhanced computed tomography (CT) scan performed 2 h later showed severe stenosis of the infrarenal aorta due to abdominal aortic dissection (Figure 1). Neither of the common iliac arteries was enhanced, while the femoral arteries were enhanced due to collateral flow. The diameter of the proximal IAAD lesion was 19 mm, and the terminal aorta measured 15 mm in diameter. He was diagnosed with IAAD as the cause of his lower limb pain and was transferred to the angiography room for endovascular treatment.
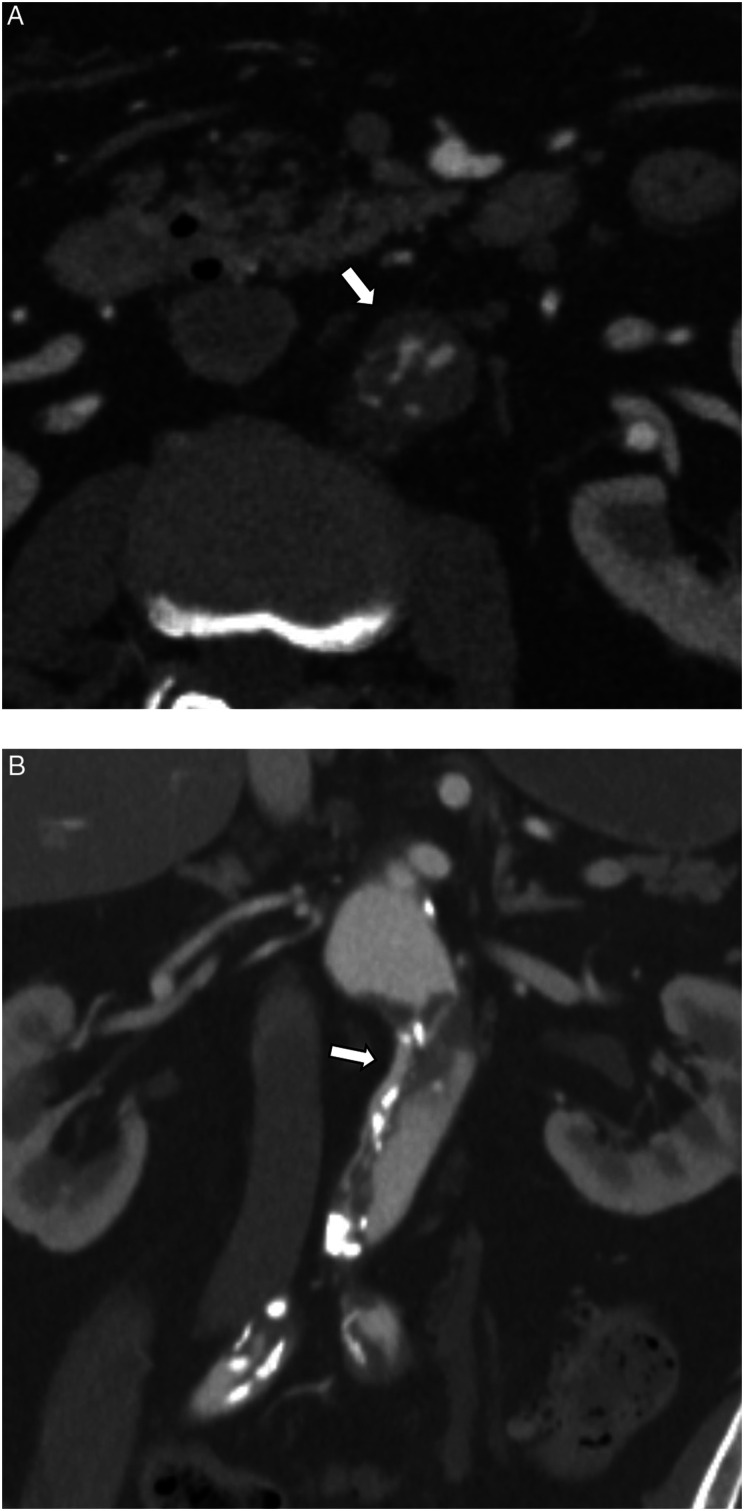
Figure 1.
(a) Axial preoperative contrast-enhanced CT imaging showed severe stenosis of the abdominal aorta due to aortic dissection (arrow). (b) Coronal preoperative contrast-enhanced CT imaging showed dissection extending from the infrarenal abdominal aorta to the bilateral iliac arteries. The true lumen (arrow) was compressed by the false lumen.
General anesthesia was induced. The left femoral artery was surgically exposed. As it was not dissected, it was punctured with an 18-gauge needle. An 8-Fr sheath was inserted, and a 0.035-inch floppy guidewire (Swan excel guidewire®, Alt, Aichi, Japan) was carefully advanced into the true lumen. After guiding the wire up to the suprarenal aorta, intravascular ultrasound (IVUS) was performed to confirm its location in the true lumen. A 4-Fr catheter (Tempo®, Cardinal Health Japan, Tokyo, Japan) was then inserted into the abdominal aorta, and angiography revealed a primary tear just below the upper end of the IAAD (Figure 2). It appeared feasible to cover the primary tear using the abdominal aortic cuff of a stent graft. To avoid distal stent graft–induced new entry (SINE) due to a mismatch between the stent graft and abdominal aorta, a smaller stent graft (diameter: 23 mm, length: 33 mm, Excluder cuff®, Gore Japan, Tokyo, Japan) was initially placed distally using the cuff technique. 4 A large proximal stent graft (diameter: 26 mm, length: 33 mm, Excluder cuff®, Gore Japan, Tokyo, Japan) was then positioned to cover the primary tear. No balloon touch-up was performed as balloon attachments are thought to cause SINE. Angiography from the abdominal aorta showed that the stenosis had been successfully ameliorated, and pain relief was achieved. There were no complications, such as motor paralysis or SINE. 11 days later, he was discharged.
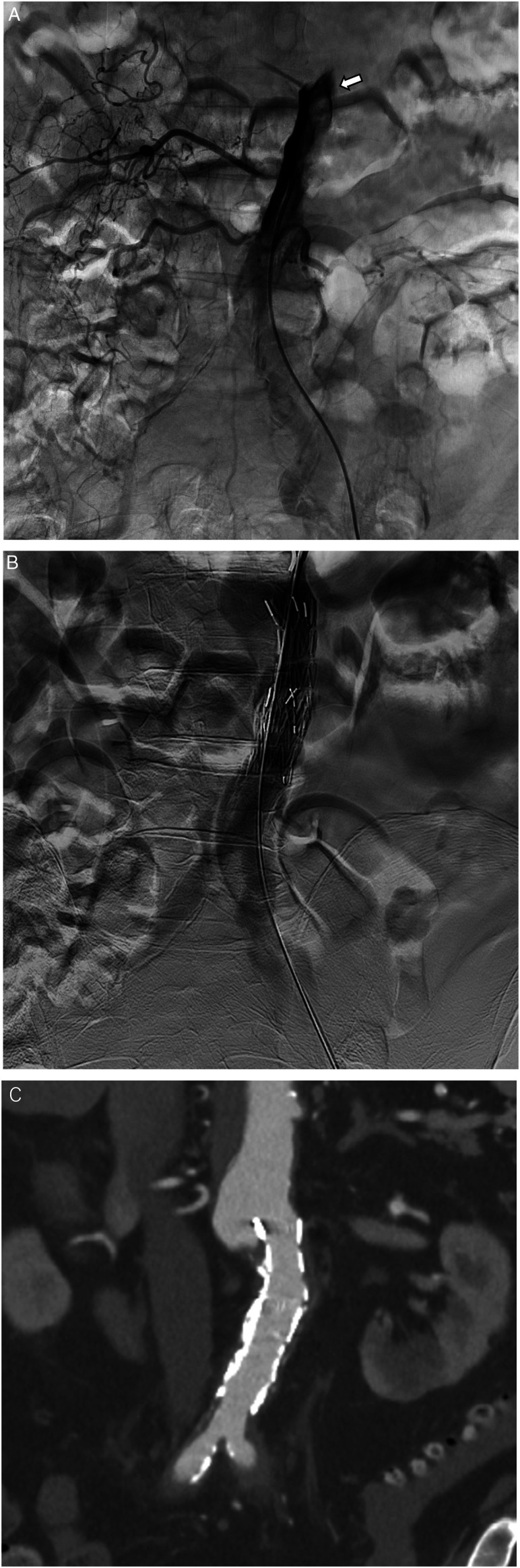
Figure 2.
(a) Angiography performed from the true lumen showed the primary entry tear just below the top of the aortic dissection (arrow). (b) After placement of the stent graft, the angiography showed that the false lumen had disappeared, and the true lumen had dilated. (c) Contrast-enhanced CT performed 2 days after the endovascular treatment showed shrinkage and thrombosis of the false lumen.
Discussion
Stent grafts for aortic disease are typically placed between the sections of normal aorta located proximally and distally to the aortic disease, a method known as healthy-to-healthy placement. In contrast, for entry closure a stent graft is positioned solely around the primary tear to reduce the pressure in the false lumen. Following placement, aortic remodeling, such as the disappearance of the false lumen, occurs, and the stenosis of the distal aorta is improved. Entry closure with a stent graft is commonly performed for thoracic aortic dissection to treat true lumen stenosis. 5 However, there have been no reports about the treatment of IAAD via entry closure with a stent graft. In previously reported IAAD cases, a branching stent graft was placed from the healthy aorta to the healthy iliac artery. This approach carries a risk of arterial injury because complicated manipulation is required in cases of severe stenosis. In the present case, severe stenosis of the terminal aorta was also observed, and making the insertion of a branching stent graft seems difficult. Therefore, we planned to proceed with stent graft placement for entry closure.
There are several key points to note about this case. The first concerns the location of the primary tear. Identifying the primary tear is crucial for performing entry closure. 6 In this case, no clues regarding the tear’s location were apparent on preoperative CT. Therefore, angiography from the true lumen was performed revealing the primary tear just below the upper end of the IAAD. The second point related to the placement of guidewire in the true lumen. Guidewires can easily be advanced into false lumens, particularly in cases of stenosis. Therefore, IVUS was used to confirm guidewire’s placement. The third point pertains to the optimal size of stent graft. If an oversized stent graft had been used, the radial force may have produced a new entry tear. 7 In this case, a smaller stent graft, 23 mm, was placed distally, and a larger stent graft, 26 mm, was placed proximally to match the aorta’s size. The fourth point involves the treatment for residual stenosis. In this case, the stenosis of the aorta and iliac artery was successfully ameliorated with just two stent grafts. The provisional extension to ensure complete attachment has been reported in endovascular treatment of type B aortic dissection with self-expandable bare stents distal to a covered stent graft. 8 If stenosis of the terminal aorta or iliac artery remains, additional stenting with the kissing technique may be required.
In this case, we selected a covered stent graft, whereas bare metal stents had been used in the previous case. 9 Based on the principle of entry closure, a covered stent graft appeared to be the appropriate choice. However, bare metal stent placement has been previously reported for isolated superior mesenteric arterial dissection. 10 A bare metal stent can compress a false lumen if the target artery is small. However, the appropriate aortic size for a bare metal stent remains unclear, and large balloon-expandable bare metal stents are not available in Japan. Thus, a covered stent graft is the preferred choice for IAAD treatment, though a bare metal stent may be considered if the size of aorta is too small.
In this case, aortic stenosis due to IAAD was treated with an abdominal aortic cuff for entry closure without complicated manipulation. Since the most appropriate treatment for IAAD with stenosis remains uncertain, further study of such cases is needed.
Footnotes
Author contributions: Contributions to the submitted work from each author: Junji Horiba, Hitomi Kaneko, and Kurando Kondo contributed to the analysis of the results. Kengo Ohta and Risa Arahata contributed to the writing of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
Informed consent
Informed consent was obtained from the patient to submit this case report.
ORCID iD
Kengo Ohta https://orcid.org/0000-0003-1509-6730
References
- 1.Trimarchi S, Tsai T, Eagle KA, et al. Acute abdominal aortic dissection: insight from the international registry of acute aortic dissection (IRAD). J Vasc Surg 2007; 46: 913–919. [DOI] [PubMed] [Google Scholar]
- 2.Sahsamanis G, Vourliotakis G, Maltezos K, et al. Endovascular treatment of infrarenal isolated abdominal aortic dissection with application of the kissing stents technique: a case report and review of the literature. Ann Vasc Dis 2017; 10: 250–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nienaber CA, Fattori R, Lund G, et al. Nonsurgical reconstruction of thoracic aortic dissection by stent-graft placement. N Engl J Med 1999; 340: 1539–1545. [DOI] [PubMed] [Google Scholar]
- 4.Masada K, Shimamura K, Sakamoto T, et al. A novel method for prevention of stent graft-induced distal re dissection after thoracic endovascular aortic repair for type B aortic dissection. Interact Cardiovasc Thorac Surg 2018; 26: 91–97. [DOI] [PubMed] [Google Scholar]
- 5.Aoki A, Maruta K, Masuda T, et al. Procedure and aortic remodeling effects of entry closure with stentgraft for type B aortic dissection: comparison between the patients with narrow true lumen and those with aneurysmal dilated false lumen. Ann Vasc Dis 2022; 15: 175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiss G, Wolner I, Folkmann S, et al. The location of the primary entry tear in acute type B aortic dissection affects early outcome. Eur J Cardio Thorac Surg 2012; 42: 571–576. [DOI] [PubMed] [Google Scholar]
- 7.Burdess A, D’Oria M, Mani K, et al. Early experience with a novel dissection-specific stent-graft to prevent distal stent-graft-induced new entry tears after thoracic endovascular repair of chronic type B aortic dissections. Ann Vasc Surg 2022; 81: 36–47. [DOI] [PubMed] [Google Scholar]
- 8.Kazimierczak A, Rynio P. Extended petticoat strategy in type B aortic dissection. Eur J Vasc Endovasc Surg 2019; 57: 302. [DOI] [PubMed] [Google Scholar]
- 9.Ono M, Mizuno A, Komiyama N. Successful endovascular therapy for isolated abdominal aortic dissection involving bilateral common iliac arteries. Ann Vasc Dis 2019; 12: 99–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gobble RM, Brill ER, Rockman CB, et al. Endovascular treatment of spontaneous dissections of the superior mesenteric artery. J Vasc Surg 2009; 50: 1326–1332. [DOI] [PubMed] [Google Scholar]