Abstract
Background:
The U.S. drug overdose epidemic is increasingly severe and steep increases have been seen among women.
Objective:
To explore trends in drug overdose deaths among women in the United States by race, ethnicity, and age group.
Design:
This study is a retrospective observational study of drug overdose deaths among U.S. women from 1999 to 2021.
Methods:
We use CDC WONDER Multiple Causes of Death files data using International Classification of Diseases, 10th Revision (ICD-10) codes X40–X44, X60–X64, X85, and Y10–Y14 to identify overall drug overdose deaths, T40.5 for cocaine-related deaths, T40.0–T40.4, T40.6 for opioid-related deaths, T42.4 for benzodiazepines, and T43.6 to identify psychostimulants. Race and ethnicity were defined as non-Hispanic Black, White, American Indian/Alaska Native (AI/AN), Asian, and Hispanic. We calculated overdose death rates per 100,000 women for all overdose deaths and for specific drugs by year, stratified by race and ethnicity.
Results:
From 1999 to 2021, overdose deaths among all women in the United States increased by 480%. Overdose deaths rose 750% for non-Hispanic AI/AN women, 490% for non-Hispanic Black women, 450% for non-Hispanic White women, 325% for Hispanic women, and 150% for non-Hispanic Asian or Pacific Islander women. Women ages 35–44 and 45–54 saw the largest increases in overall overdose deaths. Cocaine-related deaths were more prevalent among non-Hispanic Black women, opioid and methamphetamine-related deaths were more prevalent among non-Hispanic AI/AN women, and benzodiazepine-related deaths were more prevalent among non-Hispanic White women.
Conclusion:
Increases in overdose deaths were noted in all races, ethnicities, and age groups, with deaths continuing to accelerate in 2021. Our study highlights a need for interventions expanding access to medications for opioid use disorder, naloxone, fentanyl test strips, and contingency management while accounting for gendered roles and vulnerabilities.
Keywords: drug overdose deaths, women, race and ethnicity, substance use, age
Plain language summary
Drug overdose deaths among women 1999–2021 in the United States: Differences by race/ethnicity and age
Background:
The U.S. drug overdose epidemic is increasingly severe and steep increases have been seen among women. The study aimed to explore trends in drug overdose deaths among women in the U.S. by race, ethnicity, and age group. From examining these differences, the researchers sought to offer insights to inform overdose prevention strategies for women who use drugs and face different treatment needs.
Methods:
We used CDC WONDER Multiple Causes of Death files data to identify drug overdose deaths overall and by type (cocaine-related, opioid-related, benzodiazepine-related, and psychostimulant-related) among U.S. women from 1999–2021. Race and ethnicity were defined as Non-Hispanic Black, White, American Indian/Alaska Native (AI/AN), Asian, and Hispanic. We calculated overdose death rates per 100,000 women for all overdose deaths and for specific drugs by year, grouped by race and ethnicity.
Results:
Increases in overdose deaths were noted in all races, ethnicities, and age groups, with deaths continuing to accelerate in 2021. Our findings were: Overdose deaths among all women in the United States increased by 480%. Specifically, overdose deaths rose by: 750% for Non-Hispanic AI/AN women 490% for Non-Hispanic Black women 450% for Non-Hispanic White women 325% for Hispanic women 150% for Non-Hispanic Asian or Pacific Islander women. Women ages 35–44 and 45–54 saw the largest increases in overall overdose deaths. Cocaine-related deaths were more prevalent among Non-Hispanic Black women. Opioid and methamphetamine-related deaths were more prevalent among Non-Hispanic AI/AN women. Benzodiazepine-related deaths were more prevalent among Non-Hispanic White women.
Conclusions:
Our study highlighted a need for interventions expanding access to medications for opioid use disorder (MOUD), naloxone, fentanyl test strips, and contingency management while taking roles and vulnerabilities specific to women into account.
Introduction
Drug overdose deaths overall and among women
Drug overdose deaths in the United States continue to be of concern, rising from around 17,000 in 1999 to over 100,000 in 2021. 1 The national rise in overdose deaths has occurred in waves characterized by increases due to prescription opioid-related deaths beginning in the 1990s, then increases in heroin-related deaths around 2010, soaring increases in synthetic opioids such as fentanyl in 2013, and a current fourth wave characterized by increases in opioid, namely fentanyl, and stimulant-related deaths.2,3 While drug overdose deaths are increasing on a national level, sex differences in these deaths are evident. Overall, more men die from drug overdose yearly, accounting for 70% of overdose deaths in 2022, 1 yet growing evidence suggests increasing overdose deaths among women.4,5
Drug overdose deaths among women jumped from 5591 in 1999 to 32,398 in 2021. 1 Substance use outcomes and deaths warrant the exploration of sex differences as several biological differences in males and females exist to influence the short-term and long-term effects of substance use by sex. 6 In addition, some evidence, though mixed, suggests the subjective effects of drugs being influenced by ovarian hormones. 6 Specifically, certain stages in menstrual cycles have been associated with greater drug liking and reporting pleasant effects, and progesterone is associated with acute decreases in cocaine craving and reoccurrence of substance use disorders (SUD) among women.6,7 Other evidence suggests women use smaller amounts of drugs and for a shorter duration before they develop a SUD, may have more drug cravings in general, and are more likely to have a reoccurrence of SUD after treatment than men. 7
Racial and ethnic differences in overdose deaths overall
Along with sex differences, disparities in drug overdose by race and ethnicity are also evident.8,9 While drug overdose deaths increased significantly for all racial and ethnic groups by 2020, the drug overdose mortality rate for Black individuals surpassed the rate for non-Hispanic White individuals for the first time in over 20 years.1,10 While several studies have demonstrated overall racial and ethnic differences in drug overdose deaths, literature on racial/ethnic disparities in drug overdose deaths among women is sparse.
Age-related differences in overdose deaths overall and among women
In addition to racial and ethnic disparities in drug overdose deaths overall, age-specific differences exist. 11 Between 1999 and 2021, the 35–44 age group had the most drug overdose deaths, with the rate rising from 14.0 to 62.0 deaths per 100,000 individuals.12,13 Yet, few studies examine age-related trends in drug overdose deaths, specifically among female decedents. An investigation of overdose mortality rates among women aged 30–64 revealed a 260% increase from 1999 to 2017; however, this only offered insights for a subset of women. 14 Further, research on drug overdoses among women between 2020 and 2021, when the COVID-19 pandemic exacerbated overdose deaths, is needed. 15
Current study
The present study assesses differences in drug overdose deaths among U.S. women from 1999 to 2021 by race and ethnicity, age group, and drug type. Regarding race and ethnicity, we provide trends for non-Hispanic Black, White, American Indian/Alaska Native (AI/AN), Asian, and Hispanic women, providing comprehensive side-by-side data. We examine differences within an understudied population and offer insights that can optimize drug overdose prevention strategies for women who use drugs and face different treatment needs.
Methods
Drug overdose death codes
This retrospective observational study uses data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) Multiple Causes of Death files to assess drug overdose trends among women. 16 Specifically, we use the International Classification of Diseases, 10th Revision (ICD-10) codes X40–X44, X60–X64, X85, and Y10–Y14 to identify overall drug overdose deaths. To identify specific substances implicated in a drug overdose death, we used code T40.5 for cocaine-related deaths, T40.0–T40.4, T40.6 for opioid-related deaths, T42.4 for benzodiazepines, and T43.6 to identify psychostimulants with abuse potential (mainly methamphetamine). 15 We report our findings consistent with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. 17
Sex, age, race, and ethnicity
CDC WONDER includes the decedent’s gender based on the death certificate, and we use this data to extract overdose deaths, specifically among women. Age groups were defined as 15–24 years of age, 25–34 years of age, 35–44 years of age, 45–54 years of age, 55–64 years of age, and 65+; these classifications allowed enough data to compare over time. Race and ethnicity data in CDC WONDER are reported by the decedent’s family members or determined by the coroner and were categorized into mutually exclusive categories: Hispanic, non-Hispanic White, non-Hispanic Asian or Pacific Islander,
Non-Hispanic Black, and non-Hispanic AI/AN. In 2021, CDC WONDER modified its race and ethnicity categories, separating individuals who are Asian or Pacific Islander and allowing reports of “more than one race.” We show drug overdose death rates using both the combined non-Hispanic Asian or Pacific Islander when assessing trends over time for consistency. Because CDC WONDER also includes the new racial/ethnic categories from 2018 to 2021, we can assess how using each set of definitions in 2018–2020 impacts our estimates. In sensitivity analyses, we use the new racial/ethnic definitions for 2018–2020 (effectively removing decedents with more than one race from the other racial/ethnic categories) but find little impact on our overall results (Supplemental Materials).
Statistical analysis
We calculated overdose death rates per 100,000 women for all drug overdose deaths and for specific substances (opioids, cocaine, benzodiazepines, methamphetamine) attributed deaths each year, stratified by race and ethnicity. We use CDC WONDER’s Census population estimates for women by race and ethnicity and plot trends in mortality rates between 1999 and 2021. We note that the figures contain varying y-axis scales due to large variations in the magnitude of different substances’ implications in overdose deaths.
Results
General trends in drug overdose deaths among women
From 1999 to 2021, drug overdose deaths among all women in the United States increased by 480%, from 5591 in 1999 to 32,398 in 2021. In this period, there were 4644 overdose deaths among non-Hispanic AI/AN women, 3243 overdose deaths among non-Hispanic Asian/Pacific Islander women, 39,902 overdose deaths among non-Hispanic Black women, 22,389 overdose deaths among Hispanic women, and 294,178 overdose deaths among Non-Hispanic White women. There was an overall pattern of increased death rates from 2015 to 2017, followed by a steep decrease until 2019. From 2019 to 2021, there was an additional sharp increase in death rates. These patterns were exhibited for all age groups, although the pattern was much less strong among older women.
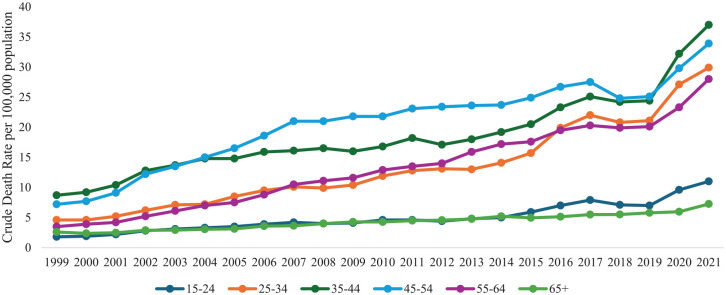
Trends in drug overdose deaths by age
Age-stratified trends in drug overdose deaths are illustrated in Figure 1. All specified age groups experienced increased rates of drug overdose deaths with varying magnitudes during the study period. The greatest increase in rates of drug overdose deaths during the study period occurred among women in midlife. In 1999, there were 1983 overdose deaths among women aged 35–44, and 1344 among women aged 45–54 died from an overdose. By 2021, there were 7967 overdose deaths among women aged 35–44 (a 300% increase) and 6912 overdose deaths among women aged 45–54 (a nearly 415% increase). We found that, generally, older women (ages 65 or older) had the lowest drug overdose death rate, followed by young adult women aged 15–24, then women aged 55–64, and women aged 25–34. While overdose deaths increased for women of all age groups throughout the years, between 1999 and 2003, women aged 35–44 had the highest overdose death rates, with women aged 45–54 second. From 2004 to 2019, overdose fatalities were greatest among women aged 45–54; however, in 2020–2021, women aged 35–44 had the highest overdose rates once again.
Figure 1.
Drug overdose deaths among women by age group in the United States, 1999–2021.
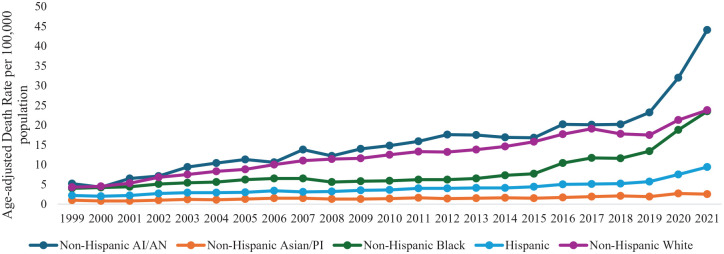
Trends in drug overdose deaths by race and ethnicity
Race and ethnicity-stratified, age-adjusted drug overdose deaths reported by CDC WONDER are illustrated in Figure 2. Overall, Non-Hispanic Asian or Pacific Islander women had the lowest rate of drug overdose deaths per 100,000 persons, followed by Hispanic women, then Non-Hispanic Black women, Non-Hispanic White women, and then Non-Hispanic AI/AN women generally had the highest rates of drug overdose deaths across the study period.
Figure 2.
Drug overdose deaths among women by race/ethnicity in the United States, 1999–2021.
All five racial and ethnic groups experienced large percentage increases in rates of drug overdose deaths between 1999 and 2021, although with varying magnitudes. In 1999, the age-adjusted overdose death rate was 5.2 per 100,000 persons for non-Hispanic AI/AN women, which rose by nearly 750% to 44.0 in 2021. For non-Hispanic Asian or Pacific Islander women, the age-adjusted rate rose from 1.0 in 1999 to 2.5 in 2021 (~ 150% increase); for non-Hispanic Black women, the age-adjusted rate rose from 4.0 in 1999 to 23.5 in 2021 (nearly 490% increase); for Hispanic women, the age-adjusted rate rose from 2.2 in 1999 to 9.4 in 2021 (nearly 325% increase); and for non-Hispanic White women the age-adjusted rate rose from 4.3 in 1999 to 23.8 in 2021 (~ 450% increase).
Similar to the age-stratified groups, there was a relatively steep increase in death rates from 2019 to 2021. This pattern was especially true of non-Hispanic Black women (an increase of 10.1 overdose deaths per 100,000) and non-Hispanic AI/AN women (an increase of 20.9 overdose deaths per 100,000).
Trends in drug overdose deaths by race and ethnicity and specific drug type
Rates of drug overdose deaths among women were measured separately for opioids, cocaine, benzodiazepines, and methamphetamine (Figure 3(a)–(d)). Importantly, the prevalence of individual substances in overdose deaths varies too greatly to have consistent y-axes for each graph; as such, each graph should be interpreted as a standalone graph and not in comparison with the other graphs. Opioid overdose death rates began to rise steadily for non-Hispanic AI/AN women and non-Hispanic White women beginning in the mid-2000s. Opioid overdose death rates began to rise for non-Hispanic Black and Hispanic women later, around 2015 or so. At this time, the overdose rate also ticked up for non-Hispanic Asian/Pacific Islander women but at a much lower level. All groups except non-Hispanic Asian/Pacific Islander women also saw large increases between 2019 and 2021.
Figure 3.
Overdose deaths among women by race/ethnicity and specific substance in the United States, 1999–2021. (a) Opioid overdose deaths. (b) Cocaine overdose deaths. (c) Benzodiazepine overdose deaths. (d) Methamphetamine overdose deaths.
Rates of overdose deaths for cocaine rose later, around 2015, but then rose. From 2016 to the peak in 2021, the crude death rate/100,000 among Non-Hispanic AI/AN women rose more than 215% from 1.7 to 5.5 per 100,000 population; more than 100% (1.8–3.6 per 100,000 population) for Non-Hispanic White women, and nearly 220% (3.6–11.4 per 100,000 population) among Black women. In contrast, overdose death rates attributed to benzodiazepines tended to rise steadily for all groups from 1999 onward. However, the rate of benzodiazepine overdose deaths is much lower than for other substances. This may also explain the unexpected dips in some years for some racial/ethnic groups, where low rates are more likely to fluctuate.
All racial/ethnic groups had relatively low methamphetamine death rates until 2009; then, the rate began to soar for non-Hispanic AI/AN women. Non-Hispanic White women experienced large increases in methamphetamine overdose deaths beginning around 2012, and increases for non-Hispanic Black and Hispanic women began in 2019, albeit at a lower overall level than for non-Hispanic AI/AN and White women.
Discussion
Study findings
This study examined trends in drug overdose death among women from 1999 to 2021 by age group, race, ethnicity, and specific substances commonly implicated in overdose deaths. We found overdose deaths were most common among women aged 35–44 and 45–54, increasing by 300% and 415%, respectively, for those age groups from 1999 to 2021. The overall age pattern is consistent with earlier work assessing these overdose trends among women earlier in the drug overdose epidemic. 12 Findings suggest a need for interventions for substance use treatment and overdose response training tailored to women in this age demographic. Effective substance use treatment components for women include safe social support and positive self-identity, coping skills, and emotional regulation. 18
In addition to age-related distinctions, large increases in drug overdose deaths were seen among non-Hispanic Black (nearly 500% increase), White (450% increase), and AI/AN women (750%). The acceleration in these shifts in drug overdose deaths was most seen between 2019 and 2021 for most racial/ethnic groups. Moreover, when assessing substance-specific overdose deaths by race and ethnicity, opioid-related overdose rates increased for all groups. Yet, these increases occurred earlier for non-Hispanic White and AI/AN women, suggesting prescription opioid-induced deaths. For Black and Hispanic women, these deaths began to rise in 2015, suggesting deaths related to synthetic opioids. Nationwide, we see a proliferation of fentanyl-related deaths soaring these most recent years of this drug overdose epidemic, with fentanyl and its analogs comprising much of opioid-related deaths.3,19 The increased potency of drugs through adulteration with fentanyl and its analogs often requires multiple doses of naloxone, an opioid reversal drug. 20 Yet, the racial differences in access to naloxone, particularly the decreased access seen among Black people who use drugs, have been documented. 21 Another study assessed evidence of naloxone administration among opioid overdose deaths in 2019 and documented that non-Hispanic Asian and Pacific Islanders had the lowest proportion of naloxone administration, while non-Hispanic AI/AN individuals had the highest. 22 These findings suggest that (1) updated research is needed to assess disparities in naloxone access for racial minorities and (2) interventions are needed to expand access to naloxone in minority communities, along with fentanyl testing strips. 20
Overall, the increases in overdose deaths among underrepresented racial groups, particularly Black and AI/AN individuals, should be contextualized within the broader social inequalities faced by these groups, including discriminatory laws and disparate enforcement of drug laws, access to healthcare, and stigma faced when accessing care, all factors that impede harm-reduction efforts and engagement in substance use treatment. 8 Pro et al. found that a lower level of community distress was the strongest correlate of treatment success for individuals seeking substance use treatment, yet Black and Native American individuals in treatment were overrepresented among those in treatment from areas with high community distress. 23 These findings underscore the importance of contextualizing substance use treatment outcomes and overdose deaths within the broader structure of social determinants of health. Further, ensuring access to culturally tailored treatment is critical to ensure different demographic groups have access to appropriate treatment, particularly interventions to increase access to medications for opioid use disorder (MOUD). Specifically, being treated with buprenorphine has been especially associated with positive treatment outcomes for Black individuals with opioid use disorder. 23
Our findings also illustrate the rise of cocaine use around 2015, which was highest among non-Hispanic Black women. However, the percent increase was similar among non-Hispanic Black, White, and AI/AN women. In addition, the rise of methamphetamines, particularly among AI/AN women, is concerning. While no Food and Drug Administration-approved medications for stimulant use disorders exist, behavioral treatments such as contingency management and cognitive behavioral therapy are used to help individuals reduce or abstain from illicit stimulant use. 24 Contingency management, which provides increasing incentives for abstaining from drugs, is the most effective behavioral therapy for reducing or abstaining from cocaine and methamphetamine use, with strong effect sizes.24,25 However, contingency management is severely underutilized, yet such efficacy of contingency management suggests that incorporating this approach into women-specific drug treatment may improve treatment outcomes.24 –26
While more men die from a drug overdose than women, women who use drugs have been shown to have greater excess mortality than men.27,28 Women who use drugs face numerous challenges that increase their likelihood of other co-occurring adverse health and social effects due to increasing rates of incarceration, HIV, gender-based violence, and stigma.29 –34 Specifically, the interconnectedness between drug use, sex work, and the criminal justice system warrants especially targeted outreach to women who use drugs and engage in sex work and women reentering society after incarceration as the period leaves individuals at the highest risk of fatal drug overdoses.32,33,35 Globally, most women involved in the criminal justice system are there due to drug-related offenses. 30 As such, interventions partnering with jails and prisons to provide overdose response training and naloxone to individuals immediately before release are needed.36,37
Moreover, women who use drugs are known to have unique needs, and gender roles in drug cultures may leave women with less autonomy than men who use drugs.29,38 Intimate partner violence and violence in general toward women who use drugs by men and law enforcement are common, particularly among women who engage in sex work.29,30,35 Yet, women who use drugs may be denied access to domestic violence shelters and associated services.29,30 Available harm-reduction programs and substance use treatment pose barriers to access and retention, including fear of harassment and logistical barriers such as childcare and transportation.29,30,32
In addition to criminal justice-based interventions, strengthening women-focused community-based drug treatment systems to incorporate childcare, transportation services, and can help ease the logistical barriers to SUD treatment.32,39 Many women who use drugs have children, and the stress and responsibilities of having children may trigger substance use, yet losing custody of children may also trigger substance use and reduce the likelihood of treatment success.29,35 As such, SUD treatment incorporating parenting skills may be especially beneficial to improve treatment outcomes and reduce intergenerational transmission of substance use. 35 Moreover, using female-certified recovery specialists, individuals in long-term recovery as peer support and case management, and outreach services to recruit women who use drugs may bolster treatment engagement and retention. 40
Limitations and strengths
Our study should be contextualized within several limitations. First, our study assesses trends in overdose deaths by age, race, and ethnicity among women. However, we do not have individual-level data on decedents to contextualize their deaths. Second, race and ethnicity are often reported by next of kin; however, when the data is unavailable, it is determined by the medical examiner, who may not accurately assess the decadent’s racial/ethnic background. In addition, death certificate data do not include information on decedents’ drug use or addiction history. We also note that overdose deaths are based on the given substance being involved; however, it is also possible that multiple substances were involved. Unfortunately, CDC WONDER does not provide data on a single substance (e.g., cocaine but not opioids). Despite these limitations, this study examines current trends in overdose deaths among U.S. women and provides epidemiological data needed for surveillance and intervention development.
Conclusion
We assessed trends in drug overdose deaths among U.S. women from 1999 to 2021 for non-Hispanic Black, White, AI/AN, Asian, and Hispanic women. We found that from 1999 to 2021, total drug overdose deaths among all women in the United States increased by approximately 480%, from 5591 in 1999 to 32,398 in 2021. Non-Hispanic Black, AI/AN, and White women saw the largest increase in overdose deaths, which continued to increase in 2021. Regarding age group, the greatest increase in rates of drug overdose deaths during the study period occurred among women in midlife, though all age groups saw increases. These findings call for interventions expanding access to MOUD, naloxone, fentanyl test strips, and contingency management while accounting for gendered roles and vulnerabilities that impact women who use drugs.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057241307088 for Drug overdose deaths among women 1999–2021 in the United States: Differences by race, ethnicity, and age by Abenaa A Jones, Joel E Segel, Emma M Skogseth, Hannah B Apsley and Alexis R Santos-Lozada in Women’s Health
Acknowledgments
We acknowledge the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research, from which our data is derived.
Footnotes
ORCID iDs: Emma M Skogseth  https://orcid.org/0009-0006-8815-5307
https://orcid.org/0009-0006-8815-5307
Hannah B Apsley  https://orcid.org/0000-0002-0829-5603
https://orcid.org/0000-0002-0829-5603
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: The data used for this study is deidentified, publicly available data and did not require Institutional Review Board approval.
Consent for Publication: Not required as this is a secondary data analysis.
Author contribution(s): Abenaa A Jones: Writing – review & editing; Writing – original draft; Funding acquisition; Conceptualization.
Joel E Segel: Writing – review & editing; Formal analysis.
Emma M Skogseth: Writing – review & editing; Writing – original draft.
Hannah B Apsley: Writing – review & editing.
Alexis R Santos-Lozada: Writing – review & editing.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the National Institute on Drug Abuse (North Bethesda, Maryland) (K01DA051715: P.I., Abenaa A Jones).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Data used in this study can be found online at CDC WONDER.
References
- 1. National Institute on Drug Abuse. Drug Overdose Death Rates | National Institute on Drug Abuse (NIDA), 2024. [cited 26 July 2024], https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
- 2. CDC. Understanding the opioid overdose epidemic, https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html (2024, accessed June 8, 2024).
- 3. Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy 2019; 71: 183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carmichael AE, Schier JG, Mack KA. Drugs and drug classes involved in overdose deaths among females, United States: 1999–2017. J Womens Health (Larchmt) 2022; 31(3): 425–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Motyka MA, Al-Imam A, Haligowska A, et al. Helping women suffering from drug addiction: needs, barriers, and challenges. Int J Environ Res Public Health 2022; 19(21): 14039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McHugh RK, Votaw VR, Sugarman DE, et al. Sex and gender differences in substance use disorders. Clin Psychol Rev 2018; 66: 12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute on Drug Abuse. Sex and Gender Differences in Substance Use | National Institute on Drug Abuse (NIDA), 2020. [cited 26 July 2024], https://nida.nih.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use
- 8. Friedman J, Beletsky L, Jordan A. Surging racial disparities in the US overdose crisis. Am J Psychiatry 2022; 179(2): 166–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kariisa M, Scholl L, Wilson N, et al. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. Morb Mortal Wkly Rep 2019; 68(17): 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Friedman JR, Hansen H. Evaluation of increases in drug overdose mortality rates in the US by race and ethnicity before and during the COVID-19 pandemic. JAMA Psychiatry 2022; 79(4): 379–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jalal H, Buchanich JM, Sinclair DR, et al. Age and generational patterns of overdose death risk from opioids and other drugs. Nat Med 2020; 26(5): 699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Products—Data Briefs—Number 81—December 2011 [cited August 2 2024], https://www.cdc.gov/nchs/products/databriefs/db81.htm (2019).
- 13. Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001–2021. NCHS Data Brief 2022; 457: 1–8. [PubMed] [Google Scholar]
- 14. VanHouten JP. Drug overdose deaths among women aged 30–64 years—United States, 1999–2017. MMWR Morb Mortal Wkly Rep 2019; 68: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Han B, Einstein EB, Jones CM, et al. Racial and ethnic disparities in drug overdose deaths in the US during the COVID-19 pandemic. JAMA Netw Open 2022; 5(9): e2232314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Multiple Cause of Death Data on CDC WONDER [cited 18 August 2023], https://wonder.cdc.gov/mcd.html
- 17. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147(8): 573–577. [DOI] [PubMed] [Google Scholar]
- 18. Bailey K, Trevillion K, Gilchrist G. What works for whom and why: a narrative systematic review of interventions for reducing post-traumatic stress disorder and problematic substance use among women with experiences of interpersonal violence. J Subst Abuse Treat 2019; 99: 88–103. [DOI] [PubMed] [Google Scholar]
- 19. Park JN, Weir BW, Allen ST, et al. Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct J 2018; 15(1): 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rhodes B, Costenbader B, Wilson L, et al. Urban, individuals of color are impacted by fentanyl-contaminated heroin. Int J Drug Policy 2019; 73: 1–6. [DOI] [PubMed] [Google Scholar]
- 21. Dayton L, Gicquelais RE, Tobin K, et al. More than just availability: who has access and who administers take-home naloxone in Baltimore, MD. PLoS One 2019; 14(11): e0224686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Quinn K, Kumar S, Hunter CT, et al. Naloxone administration among opioid-involved overdose deaths in 38 United States jurisdictions in the State Unintentional Drug Overdose Reporting System, 2019. Drug Alcohol Depend 2022; 235: 109467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pro G, Hayes C, Brown CC, et al. Individual and health policy factors associated with positive heroin and opioid treatment response: United States, 2018. Am J Public Health 2022; 112(Suppl 1): S66–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bolívar HA, Klemperer EM, Coleman SRM, et al. Contingency management for patients receiving medication for opioid use disorder: a systematic review and meta-analysis. JAMA Psychiatry 2021; 78(10): 1092–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Benishek LA, Dugosh KL, Kirby KC, et al. Prize-based contingency management for the treatment of substance abusers: a meta-analysis. Addict Abingdon Engl 2014; 109(9): 1426–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Institute on Drug Abuse. What treatments are effective for people who misuse methamphetamine? | National Institute on Drug Abuse (NIDA), 2024. [cited July 26 2024], https://nida.nih.gov/publications/research-reports/methamphetamine/what-treatments-are-effective-people-who-misuse-methamphetamine
- 27. Larney S, Mathers BM, Poteat T, et al. Global epidemiology of HIV among women and girls who use or inject drugs: current knowledge and limitations of existing data. J Acquir Immune Defic Syndr 2015; 69(Suppl 2): S100–S109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA 2019; 322(20): 1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blankenship KM, Reinhard E, Sherman SG, et al. Structural interventions for HIV prevention among women who use drugs: a global perspective. J Acquir Immune Defic Syndr 2015; 69(Suppl 2): S140–S145. [DOI] [PubMed] [Google Scholar]
- 30. El-Bassel N, Strathdee SA. Women who use or inject drugs: an action agenda for women-specific, multilevel and combination HIV prevention and research. J Acquir Immune Defic Syndr 2015; 69(Suppl 2): S182–S190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gilbert L, Raj A, Hien D, et al. Targeting the SAVA (Substance Abuse, Violence, and AIDS) syndemic among women and girls: a global review of epidemiology and integrated interventions. J Acquir Immune Defic Syndr 2015; 69(Suppl 22): S118–S127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jones AA, O’Leary CC, Striley CW, et al. Substance use, victimization, HIV/AIDS risk, and recidivism among females in a therapeutic justice program. J Subst Use 2018; 23(4): 415–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jones AA, Dyer TV, Das A, et al. Risky sexual behaviors, substance use, and perceptions of risky behaviors among criminal justice involved women who trade sex. J Drug Issues 2019; 49(1): 15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Page K, Tsui J, Maher L, et al. Biomedical HIV prevention including pre-exposure prophylaxis and opiate agonist therapy for women who inject drugs: state of research and future directions. J Acquir Immune Defic Syndr 2015; 69: S169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Strathdee SA, West BS, Reed E, et al. Substance use and HIV among female sex workers and female prisoners: risk environments and implications for prevention, treatment, and policies. J Acquir Immune Defic Syndr 2015; 69(1): S110–S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Showalter D, Wenger LD, Lambdin BH, et al. Bridging institutional logics: implementing naloxone distribution for people exiting jail in three California counties. Soc Sci Med 2021; 285: 114293. [DOI] [PubMed] [Google Scholar]
- 37. Wenger LD, Showalter D, Lambdin B, et al. Overdose education and naloxone distribution in the San Francisco County Jail. J Correct Health Care 2019; 25(4): 394–404. [DOI] [PubMed] [Google Scholar]
- 38. McNeil R, Shannon K, Shaver L, et al. Negotiating place and gendered violence in Canada’s largest open drug scene. Int J Drug Policy 2014; 25(3): 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Apsley HB, Vest N, Knapp KS, et al. Non-engagement in substance use treatment among women with an unmet need for treatment: a latent class analysis on multidimensional barriers. Drug Alcohol Depend 2023; 242: 109715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jones AA, Strong-Jones S, Bishop RE, et al. The impact of family systems and social networks on substance use initiation and recovery among women with substance use disorders. Psychol Addict Behav 2024; 38(8): 850–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057241307088 for Drug overdose deaths among women 1999–2021 in the United States: Differences by race, ethnicity, and age by Abenaa A Jones, Joel E Segel, Emma M Skogseth, Hannah B Apsley and Alexis R Santos-Lozada in Women’s Health