Abstract
We have investigated the use of the protective antigen (PA) and lethal factor (LF) components of anthrax toxin as a system for in vivo delivery of cytotoxic T-lymphocyte (CTL) epitopes. During intoxication, PA directs the translocation of LF into the cytoplasm of mammalian cells. Here we demonstrate that antiviral immunity can be induced in BALB/c mice immunized with PA plus a fusion protein containing the N-terminal 255 amino acids of LF (LFn) and an epitope from the nucleoprotein (NP) of lymphocytic choriomeningitis virus. We also demonstrate that BALB/c mice immunized with a single LFn fusion protein containing NP and listeriolysin O protein epitopes in tandem mount a CTL response against both pathogens. Furthermore, we show that NP-specific CTL are primed in both BALB/c and C57BL/6 mice when the mice are immunized with a single fusion containing two epitopes, one presented by Ld and one presented by Db. The data presented here demonstrate the versatility of the anthrax toxin delivery system and indicate that this system may be used as a general approach to vaccinate outbred populations against a variety of pathogens.
Cytotoxic T lymphocytes (CTL) are essential for immune clearance of many intracellular pathogens, including most viruses and some bacteria (1, 18). CTL recognize infected cells when peptide epitopes (usually 8 to 10 amino acids) derived from these parasites are presented by molecules encoded by the host class I major histocompatibility complex (MHC-I) (17). The epitopes are derived from cytoplasmic proteins cleaved by the proteosome into small peptide fragments. These peptides are then transported into the lumen of the endoplasmic reticulum, where they complex with newly synthesized MHC-I molecules (17). The MHC-I peptide complex is then transported to the cell surface, where recognition by CTL can occur. After recognition of the foreign peptide, CTL lyse the infected cell, depriving the pathogen of its intracellular niche. Cytokines secreted from activated CTL also play a role in the clearance of pathogens (18). After initial exposure to the pathogen, memory CTL are established that are able to respond more rapidly and efficiently upon subsequent exposure. It is these memory CTL that vaccines are designed to elicit, stimulating the effector cells that provide protective immunity to the host.
Because the generation of memory CTL requires intracellular processing of protein antigens and assembly of peptides onto MHC-I molecules, a vaccine system designed to stimulate CTL should deliver protein antigens to the cytosol of host cells. Previous work from this lab has described an epitope delivery system with a modified nontoxic form of anthrax toxin (7, 8). Anthrax toxin consists of three proteins: protective antigen (PA), lethal factor (LF), and edema factor (EF). PA binds to the surface of host cells, where it is cleaved by a furin-like protease into its active form of PA63 (10, 19, 24). LF or EF then bind to PA63, and the protein complex is endocytosed via receptor-mediated endocytosis. After endosomal acidification, PA directs the translocation of either LF or EF into the cytoplasm of host cells where they exert their toxic effects (12, 15). Because anthrax toxin is able to direct the translocation of proteins into the cytoplasm of cells, we have investigated its potential to serve as a vehicle for the priming of specific memory CTL. The strategy involves fusing epitopes to the first 255 amino acids of LF, designated LFn. LFn has the ability to bind PA at the cell surface but completely lacks the LF toxic activity (4, 5). In a previous report, a known epitope of the listeriolysin O protein (LLO) from the intracellularly replicating bacteria, Listeria monocytogenes, was genetically fused to LFn to form the fusion protein LFn-LLO91–99 (7). After immunization with LFn-LLO91–99 mixed with PA, BALB/c mice mounted a protective CTL response against L. monocytogenes (7).
In this report we tested broader applications of the anthrax toxin delivery system. By constructing LFn fusion proteins encoding epitopes from the nucleoprotein (NP) of lymphocytic choriomeningitis virus (LCMV), we demonstrate that vaccination with this delivery system protects mice against subsequent challenge with LCMV. Furthermore, we show that a single fusion protein can be used to prime a CTL response against both LCMV and L. monocytogenes. We also demonstrate that a single toxin fusion can prime a CTL response against LCMV in more than one mouse haplotype. Finally, we conducted experiments designed to test whether the toxin system can be used to deliver a fusion protein containing a substantial portion of the NP protein to the cytoplasm of host cells. The delivery of large protein antigens will be advantageous in outbred populations, where it is not always known which epitope from a given protein will be presented by a particular MHC-I molecule. The data presented here illustrate the versatility of the anthrax toxin delivery system.
MATERIALS AND METHODS
Peptides.
Synthetic peptides LLO91–99 (GYKDGNEYI), NP396–404 (FQPQNGQFI), and NP118–126 (RPQASGVYM) were purchased from Biosynthesis Incorporated (Lewisville, Tex.).
Animals and cell culture.
BALB/c (H-2d) and C57BL/6 (H-2b) mice were purchased from The Jackson Laboratory (Bar Harbor, Maine). All mice were females between 8 and 12 weeks of age. Mouse thymoma EL-4 (H-2b) and mouse mastocytoma P815 (H-2d) cell lines were maintained at 37°C in 7% CO2 in a medium (RP-10) containing RPMI 1640 and 10% fetal bovine serum as previously described (34). The BALB/c clone 7 (H-2d) fibroblast cell line was maintained at 37°C and 7% CO2 in a medium containing Eagle minimal essential medium supplemented with antibiotics and 10% fetal bovine serum.
Construction of LFn fusion proteins.
Five fusion proteins were used in this study: LFn-NP118–126, LFn-NP396–404, LFn-LLO91–99-NP118–126, LFn-NP118–126-NP396–404, and LFn-NP118–404 (Table 1). LFn-NP118–126 was constructed as previously described (7). Briefly, an upstream primer homologous to the 5′ end of LF and containing additional sequence encoding an NdeI site was used in combination with a second primer containing sequence homologous to the 3′ end of LFn that contained additional nonhomologous sequence encoding the nine-amino-acid epitope (NP118–126), two stop codons, and a BamHI site. These primers were used to amplify the fusion sequence by PCR, with the toxin-encoding plasmid from Bacillus anthracis, pXO1, serving as template. The amplified fragment was digested with NdeI and BamHI and ligated into the corresponding sites within the multiple cloning region of the expression vector pET15b (Novagen, Madison, Wis.). The resulting plasmid was used to transform E. coli XL1-Blue (Stratagene, La Jolla, Calif.), and a plasmid from one clone was confirmed by restriction digest and DNA sequence analysis. This plasmid was then used to transform E. coli BL21(DE3) for expression of the fusion protein (35). The construction of LFn-NP396–404 was performed in the same manner by using a downstream primer encoding this epitope. The construction of LFn-LLO91–99-NP118–126 and LFn-NP118–126-NP396–404 was performed essentially as described above. The plasmid encoding the LFn-LLO91–99 fusion protein served as the template for the construction of LFn-LLO91–99-NP118–126. The 5′ primer is as described above. It was used in combination with a 3′ primer that was homologous to the last six amino acids of LLO91–99 and contained additional nonhomologous sequences encoding NP118–126, two stop codons, and a BamHI restriction site. The plasmid encoding the LFn-NP118–126 fusion protein served as the template for the construction of LFn-NP118–126-NP396–404. The 5′ primer is described above. It was used in combination with the 3′ primer that was homologous to the last six amino acids of NP118–126 and which contained additional nonhomologous sequences encoding NP396–404, two stop codons, and a BamHI restriction site. The amplified PCR products were cloned into pET15b as described above.
TABLE 1.
Fusion proteins used in this study
| Fusion protein | Antigen(s) | Epitope(s) | Restricting molecule(s) | Mouse strain tested |
|---|---|---|---|---|
| LFn-NP118–126 | NP from LCMV | NP118–126 | Ld | BALB/c |
| LFn-NP396–404 | NP from LCMV | NP396–404 | Db | C57BL/6 |
| LFn-LLO91–99-NP118–126 | LLO from L. monocytogenes | LLO91–99 | Kd | BALB/c |
| NP from LCMV | NP118–126 | Ld | BALB/c | |
| LFn-NP118–126-NP396–404 | NP from LCMV | NP118–126 | Ld | BALB/c |
| NP from LCMV | NP396–404 | Db | C57BL/6 | |
| LFn-NP118–404 | NP from LCMV | NP118–126 | Ld | BALB/c |
| NP from LCMV | NP396–404 | Db | C57BL/6 |
LFn-NP118–404 was constructed as follows. LFn was amplified by PCR by using the 5′ primer described above in combination with a 3′ primer homologous to the last six amino acids of LFn and encoding a BamHI site. The amplified product was then ligated into pET15b as described above to create plasmid pLFn. NP118–404 was amplified by PCR with 5′ and 3′ primers which encoded sequences homologous to NP. Both primers also contained a nonhomologous sequence encoding a BamHI restriction site, and the 3′ primer encoded two stop codons. Plasmid 2KNP containing the full NP gene served as the template for the PCR reaction (obtained from Peter Southern, University of Minnesota, Minneapolis). The amplified product was restriction digested with BamHI and ligated into the corresponding site of pLFn. The resulting plasmid was then used to transform E. coli XL1-Blue as described above. A clone with an insert in the proper orientation was then used to transform E. coli BL21(DE3).
Expression of LFn fusion proteins.
Recombinant proteins expressed in pET15b contain a His6 tag at the amino terminus of the protein. This tag allows for a single-step purification of the expressed protein by a Ni2+ affinity chromatography column. Cultures of BL21 carrying each of the LFn recombinant plasmids were grown in Luria broth containing ampicillin (50 μg/ml) to an optical density at 600 nm of 0.6 to 0.8, and protein expression was induced by the addition of 1 mM IPTG for 3 h. Cells were pelleted and disrupted by sonication. The sonicate was centrifuged and passed over a Ni2+ column according to the manufacturer’s instructions (Novagen). The bound protein was then eluted with 0.5 M imidazole. Next, the eluted protein was exchanged into 20 mM Tris (pH 8) by gel filtration on a prepared PD-10 column (Pharmacia, Piscataway, N.J.). The purification of LFn-NP118–404 was performed differently in that it required the isolation of inclusion bodies as specified by the manufacturer (Novagen). For inclusion body purification, urea was included in all of the buffers at a concentration of 6 M. After elution of the bound protein (0.5 M imidazole, 6 M urea), the protein was dialyzed against 20 mM Tris (pH 8).
Wild-type PA was isolated from supernatant cultures of an attenuated strain of B. anthracis as previously described (21).
Stimulation of peptide-specific CTL.
Mouse splenocytes were harvested, and CTL cultures were established as described earlier (34). Briefly, spleen cells from experimental mice were isolated and washed once in RP-10. Naive, irradiated (2,000 rads), syngeneic splenocytes were incubated for 1 h with a 10 μM solution of the cognate peptide, washed with RP-10, and used as stimulator cells. Cultures included one-half of the total splenocytes from the experimental animal and an equivalent number of stimulator splenocytes in a total volume of 20 ml of RP-10. Cultures were incubated upright in a T-25 flask at 37°C in 7% CO2.
CTL assay.
EL-4 (H-2b) or P815 (H-2d) target cells were incubated with a 1 μM concentration of the peptide to be tested and 100 μCi of sodium [51Cr]chromate (NEN, Boston, Mass.) for 1 h at 37°C. Control cells without peptide were also incubated in 51Cr. The cells were washed three times to remove unbound peptide and extracellular radionuclide. Ten thousand radiolabeled cells, either treated with peptide or left untreated (negative control), were then added to effector cell dilutions in a 96-well assay plate. The highest dilution represents one-sixth of the stimulated culture or approximately one-twelfth of the total splenocytes from the experimental mouse. The total volume in each well was 200 μl. Spontaneous and maximum lysis of target cells was determined by incubating target cells with either RP-10 or 1% Triton X-100, respectively. After 4 h of incubation at 37°C and 7% CO2, the plates were centrifuged at 1,000 rpm, and 100 μl of the supernatant was counted on a Wallac 1470 gamma counter to determine the release of 51Cr. The percent specific lysis was determined as follows: 100 × (experimental release − spontaneous release)/(maximum release − spontaneous release).
Ex vivo CTL assay.
Ex vivo CTL assays were essentially as described above with the following modifications. BALB/c clone 7 (H-2d) target cells were incubated with a 100 nM solution of NP118–126 peptide and labeled with 51Cr. Dilutions of single-cell suspensions of spleens from experimental and control animals served as the effector cells in this assay. The effector and target cells were incubated together for 6 to 8 h and harvested as described above.
Virus.
LCMV Armstrong (3) and clone 13 (2) strains were propagated in baby hamster kidney cells as previously described (2). LCMV titers were quantitated by plaque assay on Vero cell monolayers as previously described (2).
RESULTS
CTL are primed after immunization with anthrax toxin fusion proteins.
To determine if the anthrax toxin system could be used to stimulate CTL specific for two different pathogens, LCMV and L. monocytogenes, we constructed a series of plasmids encoding fusion proteins between the first 255 amino acids of LF (designated LFn) and the specific CTL epitopes shown in Table 1. The fusions contain either single or multiple CTL epitopes. Groups of mice (three per group) were injected intraperitoneally (i.p.) with 1 μg of the purified fusion proteins mixed with 2.7 μg of PA (except for LFn-NP118–404, which was used at a concentration of 4 μg per mouse plus 2.7 μg of PA). Control groups of mice were injected with the LFn fusion proteins in the absence of PA. Two weeks postimmunization the mice were sacrificed and splenocytes were stimulated on irradiated syngeneic spleen cells which had been previously incubated with the cognate peptide. After 5 days of in vitro stimulation, the cultures were assayed for the ability to lyse peptide-coated P815 (H-2d) or EL-4 (H-2b) cells in a chromium release assay.
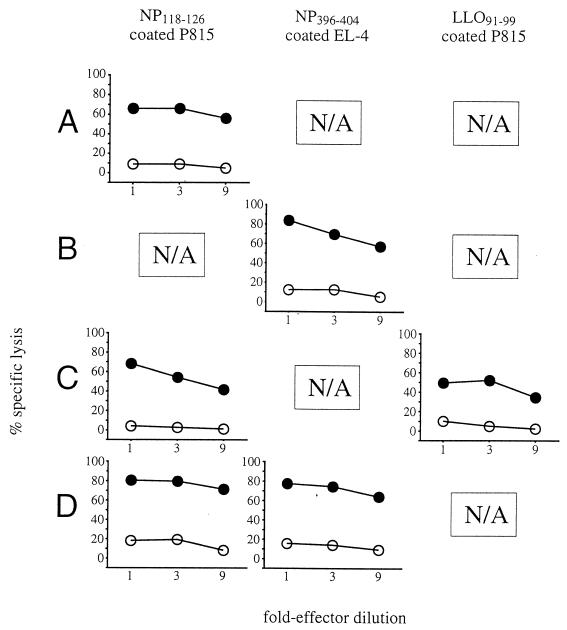
As shown in Fig. 1, cultures from animals immunized with each of the fusion proteins containing either single or double nine-amino-acid epitopes were able to lyse peptide-coated P815 or EL-4 cells to a significantly greater extent than cells not treated with peptide, thus demonstrating that epitope-specific CTL had been primed. No specific lysis was seen in cultures from mice immunized with these fusion proteins in the absence of PA (data not shown). Cultures from animals immunized with LFn-NP118–404 were able to lyse peptide-coated P815 or EL-4 cells to a significantly greater extent than cells not treated with peptide, demonstrating that this longer fusion also was able to prime epitope-specific CTL (Fig. 2). Interestingly, cultures from either BALB/c or C57BL/6 mice immunized with LFn-NP118–404 in the absence of PA demonstrated NP-specific CTL activity (see Discussion).
FIG. 1.
CTL-mediated lysis of peptide coated EL-4 or P815 cells. Mice were injected i.p. with individual LFn fusion proteins plus PA. After in vitro stimulation, samples were assayed for their ability to lyse 51Cr-labeled EL-4 or P815 cells coated with the cognate peptide (closed circles) or not coated (open circles). EL-4 cells (H-2b) were used as targets for cultures from C57BL/6 mice. P815 cells (H-2d) were used as targets for cultures from BALB/c mice. The cultures tested in these assays were splenocytes from individual mice immunized with LFn-NP118–126 (A), LFn-NP396–404 (B), LFn-LLO91–99-NP118–126 (C), or LFn-NP118–126-NP396–404 (D). Targeting was evaluated by 51Cr release. Threefold effector dilutions are shown. Similar levels of lysis were observed for each of three replicates.
FIG. 2.
CTL-mediated lysis of peptide coated EL-4 or P815 cells. Mice were injected i.p. with LFn-NP118–404 plus PA or LFn-NP118–404 alone. After in vitro stimulation, samples were assayed for their ability to lyse 51Cr-labeled EL-4 or P815 cells coated with the cognate peptide (closed circles) or not coated (open circles). The cultures tested in this assay were splenocytes from individual mice immunized with LFn-NP118–404 plus PA (A) or LFn-NP118–404 in the absence of PA (B). Targeting was evaluated by measuring 51Cr release. Threefold effector dilutions are shown. Similar levels of lysis were observed for each of three replicates.
BALB/c mice immunized with LFn-LLO91–99-NP118–126 mounted a CTL response against both LCMV and L. monocytogenes (Fig. 1C), demonstrating that a single fusion protein could prime CTL against two different pathogens. Also shown are data demonstrating that a single fusion protein (LFn-NP118–126-NP396–404 or LFn-NP118–404) could prime an NP-specific response in two different haplotypes of mice (Fig. 1D, Fig. 2). These data suggest that the anthrax toxin system could be used in outbred populations such as humans by fusing peptides which bind to different MHC-I molecules to a single LFn molecule in series.
Immunization with anthrax toxin fusion proteins results in enhanced recall response and protective immunity against LCMV challenge.
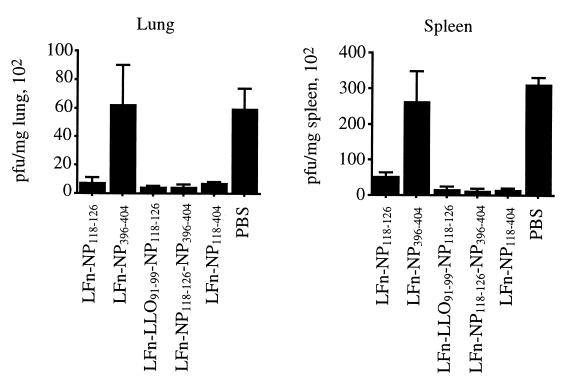
Previous work from this lab has demonstrated that mice immunized with PA plus LFn-LLO91–99 were partially protected against a subsequent challenge with L. monocytogenes (7). Although CTL are important effectors of immunity to L. monocytogenes, they are not the only cell type involved in the resolution of either primary or secondary infections (26). In contrast, CD8+ T cells are the dominant effector population involved in the resolution of infection and subsequent immunity to LCMV (13). There has also been extensive characterization of the immunodominant CTL epitopes presented during LCMV infection (9, 25, 37). We therefore examined the protective capacity of anthrax toxin fusions containing LCMV epitopes. Immunization with an LFn fusion protein encompassing the immunodominant epitope from the nucleoprotein of LCMV, NP118–126, was investigated. This epitope is presented by the Ld MHC-I molecule (30, 37). In order to determine whether protective immunity against LCMV could be generated in mice immunized with LFn fusion proteins containing NP118–126, groups of BALB/c mice (five per group) were immunized with 1 μg of the LFn fusion proteins listed in Table 1 mixed with 2.7 μg of PA. At 8 weeks postimmunization the mice were challenged i.p. with 1.8 × 106 PFU of LCMV Armstrong. At 93 h postchallenge, the mice were sacrificed and the viral titers in the spleens and lungs were determined. As shown in Fig. 3, mice immunized with each of the fusion proteins containing NP118–126 showed protection after challenge with LCMV, as demonstrated by the lower viral titers in the organs of vaccinated animals compared to the control animals. Control BALB/c mice immunized with the haplotype-mismatched LFn-NP396–404 fusion protein were not protected against LCMV challenge. These data demonstrate that NP118–126-specific CTL were primed in vaccinated animals and functioned in a protective capacity.
FIG. 3.
Protection of immunized BALB/c mice after challenge with LCMV Armstrong. Groups of mice were vaccinated with the LFn fusion proteins shown below the graph. Each of the fusion proteins were mixed with PA prior to injection. Control groups were given injections of phosphate-buffered saline. Mice were challenged i.p. with LCMV Armstrong. The number of LCMV PFU per milligram of lung and spleen samples is shown. For all constructs tested, P < 0.05. Significance was calculated by using Wilcoxon’s rank sum analysis.
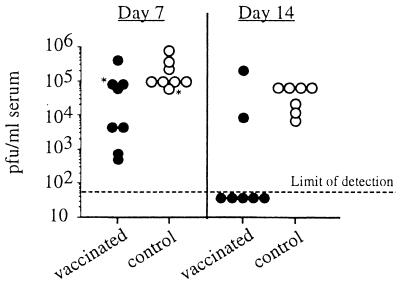
In order to further characterize the protective capacity of CTL primed with the LFn-NP118–126 fusion protein, we challenged immunized BALB/c mice with a variant of LCMV Armstrong, designated clone 13. Clone 13 suppresses the CTL response in immunocompetent naive mice and thereby causes a persistent infection, compared to the acute, rapidly cleared infection caused by LCMV Armstrong (28). Mice immune to LCMV however, are able to mount a vigorous secondary CTL response and control infection of clone 13. The ability to control infection of clone 13 therefore serves as a indicator of memory CTL (32). Groups of BALB/c mice (four per group) were immunized i.p. with 1 μg of LFn-NP118–126 mixed with 2.7 μg of PA. At 7 weeks postimmunization the mice were challenged intravenously (i.v.) with 2 × 106 PFU of clone 13. Control groups of BALB/c mice were immunized with 1 μg of the haplotype-mismatched fusion protein LFn-NP396–404 mixed with 2.7 μg of PA. At days 7 and 14 postchallenge, serum was collected from the mice, and viral titers were measured. As shown in Fig. 4, mice immunized with LFn-NP118–126 had significantly lower viral titers of LCMV compared to control animals. At 14 days after infection five of seven immunized mice had no detectable infectious virus. These data provide further evidence that these LFn fusion protein vaccines elicit LCMV-specific protective immunity.
FIG. 4.
Protection of immunized BALB/c mice against LCMV clone 13. Mice were vaccinated with LFn-NP118–126 plus PA (closed circles). Control groups were injected with the haplotype-mismatched fusion protein LFn-NP396–404 plus PA (open circles). All mice were challenged i.v. with LCMV clone 13. The number of LCMV PFU per milliliter of serum is shown at 7 and 14 days after challenge. The graph contains data pooled from two experiments. The asterisks represent mice that died during the bleeding procedure. P < 0.05 for days 7 and 14. Significance was calculated by using Wilcoxon’s rank sum analysis.
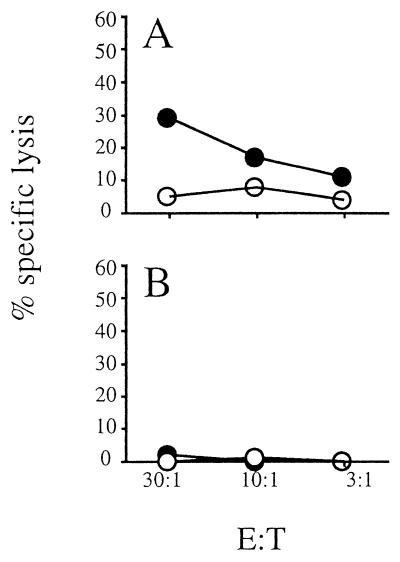
Finally, using an ex vivo CTL assay, we illustrate that vaccinated mice show an enhanced recall response to LFn-NP118–126 upon LCMV challenge. Vaccinated mice with preexisting LCMV-specific memory CTL will mount a rapid and vigorous secondary response upon exposure to LCMV. Since a large number of LCMV-specific CTL will be present in the spleens of vaccinated mice, CTL assays can be performed ex vivo without the need for in vitro stimulation. Groups of BALB/c mice (four per group) were immunized with 1 μg of LFn-NP118–126 mixed with 2.7 μg of PA. Control groups of mice were immunized with 1 μg of LFn-NP396–404 mixed with 2.7 μg of PA. At 16 weeks postimmunization the mice were challenged i.p. with 106 PFU of LCMV Armstrong. Three days after challenge the animals were sacrificed, and spleen cells from a group of four animals were pooled and tested for the ability to lyse NP118–126 peptide-coated BALB/c clone 7 (H-2d) cells. As shown in Fig. 5, mice immunized with LFn-NP118–126 mount an enhanced CTL recall response to NP118–126 after challenge with LCMV, while control groups of mice do not mount a detectable secondary CTL response.
FIG. 5.
Enhanced recall response against LCMV Armstrong challenge in immunized BALB/c mice. Immunized and control mice were challenged with LCMV Armstrong. Three days after challenge the animals were sacrificed, and pooled spleen cells from the groups were directly assayed for their ability to target 51Cr-labeled BALB/c clone 7 cells treated with NP118–126 peptide (closed circles) or not treated (open circles). (A) The immunized group was vaccinated with LFn-NP118–126 mixed with PA. (B) The control group was injected with LFn-NP396–404 mixed with PA.
DISCUSSION
Vaccines designed to stimulate CTL should be able to deliver protein antigens to the cytoplasm of host cells for processing and presentation by MHC-I. Many systems have been exploited to accomplish cytoplasmic delivery, including viral and bacterial vectors and DNA vaccines (7, 8, 14, 22, 27, 33, 36). There have also been reports demonstrating that antiviral immunity can be primed in mice vaccinated with a recombinant Bordetella adenylate cyclase toxin incorporating a CTL epitope from LCMV (11, 29, 31); however, the data demonstrated protection only when the recombinant toxin was injected in the presence of an adjuvant, aluminum hydroxide (29). Therefore, it remains unclear whether the antiviral protection was a result of toxin delivery or adjuvant activity. This report describes the use of a nontoxic, truncated form of anthrax toxin as an epitope delivery system without the use of adjuvant.
We demonstrate that protective immunity against a viral pathogen, LCMV, is generated in BALB/c mice immunized with LFn fusion proteins encoding the immunodominant LFn-NP118–126 epitope. Because the outcome of LCMV infection is determined predominantly by the ability of the host to mount a rapid and effective CTL response, it serves as an excellent model for testing experimental vaccines designed to elicit CTL responses (37). BALB/c mice immunized with various anthrax toxin fusion proteins containing the LFn-NP118–126 epitope showed protection against challenge with LCMV Armstrong as demonstrated by reduced viral titers in the lungs and spleens compared to control animals. In addition, BALB/c mice immunized with PA plus LFn-NP118–126 showed an enhanced recall response to LFn-NP118–126, as demonstrated by an ex vivo CTL assay 3 days after challenge with LCMV Armstrong.
Another LCMV model of infection utilizes an isolate of Armstrong designated clone 13. Clone 13 suppresses the CTL response in naive, immunocompetent mice, and infection with this isolate results in a chronic lifelong LCMV infection (2, 23). In mice where LCMV-specific memory CTL have been primed, there is an effective secondary CTL response which is capable of clearing clone 13 infection and preventing the establishment of a persistent infection. In the experiments presented here, the majority of BALB/c mice immunized with PA plus LFn-NP118–126 were able to clear an LCMV clone 13 infection by day 14 postchallenge, while control mice had established a persistent infection with average serum titers of 105 PFU/ml at the same time point. These data demonstrate that immunization with the anthrax toxin delivery system successfully primes specific memory CTL that are capable of protecting mice against subsequent LCMV challenge.
We also showed that immunization with a single LFn fusion protein can prime a CTL response against two different pathogens, LCMV and L. monocytogenes. BALB/c mice immunized with LFn-LLO91–99-NP118–126 plus PA mounted a specific CTL response against both the LLO and NP epitopes. Cultures of spleen cells from immunized mice were able to lyse peptide-coated cells to a significantly greater extent than untreated cells. Because a number of epitopes can be delivered per vaccination, these data suggest that epitopes from more than one pathogen could be linked in tandem to a single LFn molecule to serve as a polyvalent vaccine.
We also report that different haplotypes of mice can be immunized against LCMV by using a single LFn fusion protein encoding epitopes presented by two different MHC-I molecules. We show here that BALB/c and C57BL/6 mice immunized with LFn-NP118–126-NP396–404 plus PA or LFn-NP118–404 plus PA mounted an NP-specific CTL response. These data suggest that, for a given pathogen, a series of epitopes presented by highly represented MHC-I molecules could be linked in tandem to LFn and used to vaccinate human populations.
The data presented in this study demonstrate that multiple epitopes from the same protein that bind to different MHC-I molecules, or epitopes derived from different pathogens, can be linked in tandem and used to vaccinate mice. Although we have demonstrated the ability to link multiple epitopes to our delivery system, sequential immunizations may be necessary to protect against the wide variety of pathogens encountered. The use of a protein-based vaccine raises the possibility that the host will generate an antibody response against the delivery system itself, preventing the use of the system for subsequent immunizations. In fact, PA is known to generate an antibody response that is capable of preventing the intoxication of animals after exposure to B. anthracis. However, our previous work has demonstrated that immunization with the small amounts of protein used in these experiments does not prevent the use of this system for subsequent vaccination. In the same report we also show that no antibody response against the toxin molecule was detected in mice immunized with this system (6). Taken together, these data suggest that the anthrax delivery system may be versatile enough to induce protective immunity against multiple pathogens in the human population.
Finally, we investigated whether anthrax toxin can deliver larger protein antigens to the cytoplasm of host cells. Since different peptide epitopes from a given protein will be presented on MHC-I from an outbred population, cytoplasmic delivery of larger antigenic proteins is ideal for candidate vaccines designed to prime CTL. Although we report the ability of LFn-NP118–404 to prime a protective CTL response in immunized mice, priming of CTL was not PA dependent. A few explanations exist for this observation. One possibility is that the LFn-NP118–404 fusion protein is capable of entering cells in a PA-independent manner, although this explanation seems unlikely since neither LFn or NP has been reported to enter cells in the absence of PA. Another possibility is that LFn-NP118–404 is being alternatively processed. Although most exogenous antigen taken up by cells is processed and presented by MHC-II molecules, it has been previously reported that peptides from antigens coupled to particulate objects such as latex beads are presented by MHC-I on certain specialized macrophage cells (16, 20). It is possible that these specialized macrophage cells are internalizing particulate LFn-NP118–404 protein and presenting peptides from this protein in the context of MHC-I. In mice vaccinated in the presence of PA it is likely that both intracytoplasmic processing of peptide fragments and alternative processing by certain macrophage cells is resulting in the priming of CTL. Experiments are currently underway to determine the mechanism by which LFn-NP118–404 primes a CTL response in the absence of PA.
ACKNOWLEDGMENTS
We thank Sarah D’Orazio and Christopher Zarozinski for helpful discussions and critical reading of the manuscript. We also thank Ron Bosch for statistical analysis.
This work was supported by grants AI42671, AI41526, AI22021, and AI30048. M.N.S. is the recipient of a Junior Faculty Research Award from the American Cancer Society.
REFERENCES
- 1.Ahmed R, Gray D. Immunological memory and protective immunity: understanding their relation. Science. 1996;272:54–60. doi: 10.1126/science.272.5258.54. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed R, Salmi A, Butler L D, Chiller J M, Oldstone M B. Selection of genetic variants of lymphocytic choriomeningitis virus in spleens of persistently infected mice. J Exp Med. 1984;60:521–540. doi: 10.1084/jem.160.2.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armstrong C, Lillie R D. Experimental lymphocytic choriomeningitis of monkeys and mice produced by a virus encountered in studies of the 1933 St. Louis encephalitis epidemic. Public Health Rep. 1934;49:1019–1027. [Google Scholar]
- 4.Arora N, Kimpel K R, Singh Y, Leppla S H. Fusions of anthrax toxin lethal factor to the ADP-ribosylation domain of Pseudomonas exotoxin A are potent cytotoxins which are translocated to the cytosol of mammalian cells. J Biol Chem. 1992;267:15542–15548. [PubMed] [Google Scholar]
- 5.Arora N, Leppla S H. Residues 1-254 of anthrax toxin lethal factor are sufficient to cause cellular uptake of fused polypeptides. J Biol Chem. 1993;268:3334–3341. [PubMed] [Google Scholar]
- 6.Ballard J D, Collier R J, Starnbach M N. Anthrax toxin as a molecular tool for CTL vaccination: disulfide linked epitopes, multiple injections, and the role of CD4+ cells. Infect Immun. 1998;66:4696–4699. doi: 10.1128/iai.66.10.4696-4699.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ballard J D, Collier R J, Starnbach M N. Anthrax toxin-mediated delivery of a cytotoxic T-cell epitope in vivo. Proc Natl Acad Sci USA. 1996;93:12531–12534. doi: 10.1073/pnas.93.22.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ballard J D, Doling A M, Beauregard K, Collier R J, Starnbach M N. Anthrax toxin mediated delivery in vivo and in vitro of a cytotoxic T-lymphocyte epitope from ovalbumin. Infect Immun. 1998;66:615–619. doi: 10.1128/iai.66.2.615-619.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butz E A, Bevan M J. Massive expansion of antigen-specific CD8+ T cells during acute virus infection. Immunity. 1998;8:167–175. doi: 10.1016/s1074-7613(00)80469-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Escuyer V, Collier R J. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fayolle C, Sebo P, Ladant D, Ullmann A, Leclerc C. In vivo induction of CTL responses by recombinant adenylate cyclase of Bordetella pertussis carrying viral CD8+ T cell epitopes. J Immunol. 1996;156:4697–4706. [PubMed] [Google Scholar]
- 12.Friedlander A M. Macrophages are sensitive to anthrax lethal toxin through an acid-independent process. J Biol Chem. 1986;261:7123–7126. [PubMed] [Google Scholar]
- 13.Fung-Leung W-P, Kundig T M, Zinkernagel R M, Mak T W. Immune response against lymphocytic choriomeningitis virus in mice without CD8 expression. J Exp Med. 1991;174:1425–1429. doi: 10.1084/jem.174.6.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fynan E F, Webster R G, Fuller D H, Haynes J R, Santoro J C, Robinson H L. DNA vaccines: protective immunizations by parenteral, mucosal, and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–11482. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon V M, Leppla S H, Hewlett E L. Inhibitors of receptor-mediated endocytosis block the entry of Bacillus anthracis adenylate cyclase toxin but not that of Bordetella pertussis adenylate cyclase toxin. Infect Immun. 1988;56:1066–1069. doi: 10.1128/iai.56.5.1066-1069.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harding C V, Song R. Phagocytic processing of exogenous particulate antigens by macrophages for presentation by class I MHC molecules. J Immunol. 1994;153:4925–4933. [PubMed] [Google Scholar]
- 17.Heemels M T, Ploegh H. Generation, translocation and presentation of MHC class I-restricted peptides. Annu Rev Biochem. 1995;64:463–491. doi: 10.1146/annurev.bi.64.070195.002335. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann S H. Immunity to intracellular bacteria. Annu Rev Immunol. 1993;11:129–163. doi: 10.1146/annurev.iy.11.040193.001021. [DOI] [PubMed] [Google Scholar]
- 19.Klimpel K R, Molly S S, Thomas G, Leppla S H. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc Natl Acad Sci USA. 1992;89:10277–10281. doi: 10.1073/pnas.89.21.10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kovacsovics-Bankowski M, Clark K, Benacerraf B, Rock K L. Efficient major histocompatibility complex class I presentation of exogenous antigen upon phagocytosis by macrophages. Proc Natl Acad Sci USA. 1993;90:4942–4946. doi: 10.1073/pnas.90.11.4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leppla S H. Bacillus anthracis calmodulin-dependent adenylate cyclase: chemical and enzymatic properties and interactions with eucaryotic cells. Adv Cyclic Nucleotide Protein Phosphorylation Res. 1984;17:189–198. [PubMed] [Google Scholar]
- 22.Martins L P, Lau L L, Asano M S, Ahmed R. DNA vaccination against persistent viral infection. J Virol. 1995;69:2574–2582. doi: 10.1128/jvi.69.4.2574-2582.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matloubian M, Somasundaram T, Kolhekar S R, Selvakumar R, Ahmed R. Genetic basis of viral persistence: single amino acid change in the viral glycoprotein affects the ability of lymphocytic choriomeningitis virus to persist in adult mice. J Exp Med. 1990;172:1043–1048. doi: 10.1084/jem.172.4.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molloy S S, Bresnahan P A, Leppla S H, Klimpel K R, Thomas G. Human furin is a calcium-dependent serine endoprotease that recognizes the sequence Arg-X-X-Arg and efficiently cleaves anthrax toxin protective antigen. J Biol Chem. 1992;267:16396–16402. [PubMed] [Google Scholar]
- 25.Murali-Krishna K, Altman J D, Suresh M, Sourdive D J, Zajac A J, Miller J D, Ahmed R. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity. 1998;8:177–187. doi: 10.1016/s1074-7613(00)80470-7. [DOI] [PubMed] [Google Scholar]
- 26.Portnoy D A. Innate immunity to a facultative intracellular bacterial pathogen. Curr Opin Immunol. 1992;4:20–24. doi: 10.1016/0952-7915(92)90118-x. [DOI] [PubMed] [Google Scholar]
- 27.Russmann H, Shams H, Poblate F, Fu Y, Galan J E, Donis R O. Delivery of epitopes by the Salmonella type III secretion system for vaccine development. Science. 1998;281:565–568. doi: 10.1126/science.281.5376.565. [DOI] [PubMed] [Google Scholar]
- 28.Salvato M, Borrow P, Shimomaye E, Oldstone M B. Molecular basis of viral persistence: a single amino acid change in the glycoprotein of lymphocytic choriomeningitis virus is associated with suppression of the antiviral cytotoxic T-lymphocyte response and establishment of persistence. J Virol. 1991;65:1863–1869. doi: 10.1128/jvi.65.4.1863-1869.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saron M F, Fayolle C, Sebo P, Ladant D, Ullmann A, Leclerc C. Antiviral protection conferred by recombinant adenylate cyclase toxins from Bordetella pertussis carrying a CD8+ T cell epitope from lymphocytic choriomeningitis virus. Proc Natl Acad Sci USA. 1997;94:3314–3319. doi: 10.1073/pnas.94.7.3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schulz M, Aichele P, Vollweider M, Bobe F W, Cardinaux F, Hengartner H, Zinkernagel R. Major histocompatibility complex-dependent T cell epitopes of lymphocytic choriomeningitis virus nucleoprotein and their protective capacity against viral disease. Eur J Immunol. 1989;19:1657–1667. doi: 10.1002/eji.1830190921. [DOI] [PubMed] [Google Scholar]
- 31.Sebo P, Fayolle C, D’Andria O, Ladant D, Leclerc C, Ullmann A. Cell-invasive activity of epitope-tagged adenylate cyclase of Bordetella pertussis allows in vitro presentation of a foreign epitope to CD8+ cytotoxic T cells. Infect Immun. 1995;63:3851–3857. doi: 10.1128/iai.63.10.3851-3857.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shen H, Miller J F, Fan X, Kolwyck D, Ahmed R, Harty J T. Compartmentalization of bacterial antigens: differential effects of priming of CD8 T cells and protective immunity. Cell. 1998;92:535–545. doi: 10.1016/s0092-8674(00)80946-0. [DOI] [PubMed] [Google Scholar]
- 33.Shen H, Slifka M K, Matloubian M, Jensen E R, Ahmed R, Miller J F. Recombinant Listeria monocytogenes as a live vaccine vehicle for the induction of protective anti-viral cell-mediated immunity. Proc Natl Acad Sci USA. 1995;92:3987–3991. doi: 10.1073/pnas.92.9.3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Starnbach M N, Bevan M J. Cells infected with Yersinia present an epitope to class I MHC-restricted CTL. J Immunol. 1994;153:1603–1612. [PMC free article] [PubMed] [Google Scholar]
- 35.Studier F W, Moffatt B A. Use of bacteriophage T7 RNA polymerase to direct selective high-level expression of cloned genes. J Mol Biol. 1986;189:113–130. doi: 10.1016/0022-2836(86)90385-2. [DOI] [PubMed] [Google Scholar]
- 36.Thomson S A, Elliot S L, Sherritt M A, Sproat K W, Coupar B E H, Scalzo A A, Forbes C A, Ladhams A M, Mo X Y, Tripp R A, Doherty P C, Moss D J, Suhrbier A. Recombinant polyepitope vaccines for the delivery of multiple CD8 T cell epitopes. J Immunol. 1996;157:822–826. [PubMed] [Google Scholar]
- 37.Whitton J L, Tishon A, Lewicki H, Gebhard J, Cook T, Salvato M, Joly E, Oldstone M B. Molecular analysis of a five-amino-acid cytotoxic T-lymphocyte (CTL) epitope: an immunodominant region which induces nonreciprocal CTL cross-reactivity. J Virol. 1989;63:4303–4310. doi: 10.1128/jvi.63.10.4303-4310.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]