Abstract
Introduction The Pittsburg Sleep Quality Index (PSQI) is widely used in different population groups to assess self-reported sleep quality over the previous month. As the Arabic language is spoken by more than 400 million people, the PSQI has been translated into Arabic for its optimal application to Arabic-speaking individuals. However, the test-retest reliability of the Arabic version of the PSQI has not been reported yet.
Objective To examine the reliability and agreement of a bilingual Arabic-English version of the PSQI (AE-PSQI) among bilingual Arabic-English-speaking adolescents and young adults of the United Arab Emirates (UAE) with good or poor sleep quality.
Materials and Methods We included 50 bilingual Arabic-English-speaking adolescents and young adults (mean age of 20.82 ± 2.7 years; 30/50 subjects classified as poor sleepers [PSQI > 5] at baseline) who filled put the AE-PSQI twice, 7 days apart. The internal consistency of the AE-PSQI was assessed through the Cronbach's alpha. The intraclass correlation coefficient (ICC[3,1]) was used to assess the test-retest reliability. The standard error of measurement (SEM), the smallest real difference (SRD), and the Bland-Altman plots were used to report agreement measures.
Results The global score on the AE-PQSI showed an acceptable level of internal consistency with a Cronbach's alpha value of 0.65, and no floor and ceiling effects were observed. The 95% confidence intervals (95%CI: 0.63-0.87) of the ICC(3,1) revealed moderate to strong reliability estimates for overall AE-PSQI scores. The SEM and SRD were of 1.6 and 4.5 respectively, and the Bland-Altman plots revealed a moderate agreement between the baseline and retest global AE-PQSI scores.
Conclusion The AE-PSQI is a reliable instrument to assess sleep quality in bilingual Arabic-English-speaking adolescents and young adults with good or poor sleep quality. Further studies on the validity and responsiveness of the AE-PSQI are warranted in individuals with and without sleep disorders.
Keywords: PSQI, reliability, sleep quality, young adults, psychometric property
Introduction
Good sleep quality in all age groups is essential for physical, mental, and cognitive functioning, which could impact quality of life 1 . Poor sleep quality has become a public health concern that has been associated with several serious medical conditions. 1 This problem is becoming increasingly recognized for adolescents and young adults, 2 3 and it is linked to obesity, 4 depression, musculoskeletal pain, 5 6 7 8 cognitive impairments and increased risk-taking medications. 1 9 10 11 Consequently, a reduction in physical functioning, psychological well-being, self-care, activities of daily living, ability to work, and interpersonal relationships has been reported to be associated with reduced sleep quality in adolescents and young adults. 3 4 5 6 7 10 12 13 14 15 16 17 Emphasizing the importance of sleep quality and including sleep assessment as a major part of the routine clinical practice are necessary. Therefore, a better understanding of sleep quality assessment tools can help in the identification and management of sleep problems before the patients suffer the long-term consequences associated with poor sleep.
Sleep quality can be assessed objectively and subjectively. Self-reported questionnaires were found to be one of the most used methods to assess subjective sleep quality among different populations, including adolescents and young adults. They are also known to be the most cost-effective measurement method. 18 The Pittsburgh Sleep Quality Index (PSQI), the Epworth Sleepiness Scale (ESS), and the Functional Outcomes of Sleep Questionnaire (FOSQ) are often used to assess an individual's subjective sleep quality. 19 20 The PSQI contains 19 self-reported items and 5 questions covering 7 domains of subjective sleep quality (including sleep duration, disturbances, latency, daytime dysfunction, habitual sleep efficiency, sleep quality, and use of sleeping medications) during the previous month. This tool has been designed to identify and differentiate good and poor sleepers. 21 The global PSQI score ranges from 0 to 21, and higher scores are indicative of worse quality of sleep (scores > 5 indicate poorer sleep quality). The PSQI has been widely used and found to have adequate psychometric properties and sensitivity of 89.6% and specificity of 86.5% (kappa = 0.75; p < 0.001) in differentiating good from poor sleepers. 22
The PSQI has been translated into 51 languages. 23 A systematic review revealed an acceptable internal consistency and construct validity 24 for the English, 25 Chinese, 11 Korean, 26 and Portuguese 27 versions of the PSQI. The original PSQI has been validated among different populations, such as healthy individuals, 28 29 30 and patients with sleep disorders, 31 psychiatric disorders, 32 neurological diseases, and chronic conditions. 33 34 The internal consistency of the original PSQI has been found to be fair to good, with a Cronbach alpha coefficient ranging from 0.64 to 0.83. 22 24 The original PSQI total score test-retest reliability estimates have been found to be moderate (r = 0.56) in pregnant women, 35 and strong (r = 0.87) in individuals with primary insomnia. 36
In 2010, the PSQI was translated into Arabic, and was tested by Suleiman et al. 37 (2010) on 35 healthy bilingual Arabic-English-speaking individuals. It has correlated strongly with the Insomnia Severity Index (ISI; r = 0.76), and moderately with the vitality subscale of the Medical Outcome Study Short Form-36 (r = -0.33). 37 However, the Arabic translation of the PSQI has demonstrated borderline/minimal acceptability (Cronbach alpha = 0.65). 37 Another study 38 examined the internal consistency of the Arabic PSQI in cancer patients and found a Cronbach alpha coefficient of 0.77, demonstrating very good acceptability. According to a systematic review by Al Maqbali et al. 23 (2020), the Arabic PSQI meets the quality assessment criteria for content, construct validity and internal consistency; however, criterion validity agreement, reliability, responsiveness, floor and ceiling effects, and interpretation have not been reported. No study has specifically investigated the test-retest reliability of the Arabic version of the PSQI yet. 39 Moreover, (self-administered) bilingual versions of questionnaires/tests may be more useful and applicable than the monolingual one for bilingual individuals. 40 41 42 Therefore, in the present study we have examined the test-retest reliability of a bilingual Arabic-English PSQI (AE-PSQI) among healthy bilingual Arabic-English-speaking adolescents and young adults of the United Arab Emirates (UAE).
Materials and Methods
Participants
In the present cross-sectional study, 50 participants of both sexes, aged between 14 and 26 years, with either poor or good sleep quality at the baseline assessment, were recruited from schools and universities in the UAE. Participants were excluded if they had a medical condition or had recently undergone surgeries that affected their sleep. The ethical approval for this study was approved by the Research Ethics Committee of the University of Sharjah (REC-22-02-23-01-S).
Procedure
Body weight was measured to the nearest 100 g using a standard portable digital weighing scale. Height was measured to the nearest 1 cm using a portable stadiometer. The Body Mass Index (BMI) was calculated for each participant as body weight (kg) divided by height in meters squared.
Pittsburgh Sleep Quality Index (PSQI)
The overall sleep quality over the preceding month 22 in adolescents and young adults was assessed using the PSQI, 33 considering that this questionnaire is used among adolescents and young adults as a reliable and valid tool. 43 44 It consists of 19 items divided into 7 sleep-related variables: 1) sleep quality; 2) sleep latency; 3) sleep duration; 4) sleep efficiency; 5) sleep disturbance; 6) medication use; and 7) daytime dysfunction. Every item is rated on a 4-point Likert scale in terms of frequency or severity. The sum of the component scores yields a global PSQI score ranging from 0 to 21, with higher scores indicating poor sleep quality. Scores > 5 indicate poor sleep quality, while those ≤ 5 indicate good sleep quality. 45
Sample Size Estimation
Considering a minimum acceptable reliability (intraclass correlation coefficient, ICC) of 0.60, an expected reliability (ICC) of 0.80, a significance level of 0.05, and a power of 0.80, the number of participants required is 49 for 2 measurements (test [baseline] versus retest [after 7 days]). 46 Therefore, 50 participants were recruited for the present study.
Procedure
The subjects were invited to participate in the study through social media adverts, university/school notice boards, and word of mouth. The study procedures were explained to the interested participants. Prior to being enrolled in the study, participants and/or their parents read the information sheet and informed consent was provided by them (in the case of adults) or by their parents/guardians (in the case of adolescents). We provided both English and the corresponding Arabic translations of each item of the PSQI together to all participants. The participants were asked to fill the AE-PSQI twice, seven days apart.
Statistical Analysis
Descriptive characteristics of the participants were presented as mean and standard deviation (SD) values. Data were tested for normal distribution using the Shapiro-Wilk test and histograms. As the data were not normally distributed, log and square-root transformation were applied, but the transformed data did not meet the required assumption of normality. The distribution of means from any skewed distribution was considered nearly normal if the number of participants is considered large enough (∼ > 30). 47 Therefore, we used parametric tests for the statistical analysis. The McNemar test was used to compare the proportion of participants with good and poor sleep quality regarding the baseline and retest global scores on the AE-PSQI. The IBM SPSS Statistics for Windows (IBM Corp., Armonk, NY, United States) software, version 28.0, was used for the statistical analysis, and values of p < 0.05 were set as the threshold for statistical significance.
Floor and Ceiling Effects
The floor and ceiling effects were assessed with the percentage of participants who scored the lowest (0) and highest (21) respectively. If more than 15% participants scored lowest or highest scores, then floor or ceiling effects were considered to exist. 48
Internal Consistency
Internal consistency refers to the degree of consistency among all internal items of the questionnaire. The internal consistency of the AE-PSQI was assessed using the Cronbach alpha; in addition, the item-to-total correlation was assessed using the Pearson correlation coefficient and the alpha values for the tool, if each item was deleted, were reported. The item-to-total correlation refers to the correlation between each item/component and the global score on the PSQI. The alpha score was interpreted according to the following criteria: lower than 0.60: “unacceptable”; 0.60 to 0.65: “undesirable”; 0.65 to 0.70: “minimally acceptable”; 0.70 to 0.80 “respectable”; 0.80 to 0.90 “very good”; and much higher than 0.90: “consider shortening the scale”. 49
Test-Retest Reliability
We compared the Pearson correlation coefficient, the Spearman correlation coefficient, and the ICC ([3,1]; two-way mixed effects, consistency, single measurements, agreement) for the test-rest reliability analysis of the baseline PSQI global and component scores and seven-day retest scores. As the reliability estimates were almost the same for all three analyses for all comparisons, and there were 50 participants, the ICC(3,1) was used for further interpretation; ICC values > 0.75 are considered strong, those from 0.40 to 0.75 are moderate, and those < 0.40 are considered poor to estimate reliability. 50 The standard error of measurement (SEM), as a measure of agreement, was calculated using the following equation: Sp √(1- r ), in which Sp is the pooled standard deviation of test-retest measures and r is the reliability coefficient (ICC). 51 52 Additionally, the smallest real difference (SRD), the threshold to detect a “real” change beyond the measurement error, was analyzed using the formula 1.96 * SEM * √2. 52
Bland-Altman Plots
To further explore the agreement of test-retest AE-PSQI scores, the Bland-Altman plot was used. The plots with mean values against differences of global PSQI scores between baseline (1) and retest (2) with 95% limits of agreement (mean bias ± [1.96 * SD]) were used. Here, mean bias and SD are the mean ± SD values of differences respectively. A significance level < 0.050 was set for all analyses. While assessing the test-retest agreement in the plot, the differences between the tests were arbitrarily considered high if they were ≥ 1.5 SDs, moderate if the differences ranged from 1.0 to 1.49 SDs, and low if the differences were < 1.0 SD. 53
Results
Participant Characteristics
This study included 50 participants. The mean age of the sample was of 20.82 ± 2.7 years, and it included 34 female (68%) and 16 male (32%) subjects. Participants characteristics are shown in Table 1 . The proportion of poor sleepers (PSQI > 5) at baseline was of 60% (n = 30/50), which was significantly different ( p = 0.039) from that of the retest (46%; n = 23/50).
Table 1. Characteristics of the study participants (n = 50).
| Characteristics | Mean ± SD |
|---|---|
| Age (in years) | 20.82 ± 2.7 |
| Sex: n (female/male) | 50 (34/16) |
| Body mass (in kg) | 59.28 ± 15.9 |
| Height (in cm) | 164.58 ± 7.7 |
| BMI (in kg/m 2 ) | 21.80 ± 5.3 |
Abbreviations: BMI , Body Mass Index; SD, standard deviation.
Floor and Ceiling Effects
None of the included participants showed floor or ceiling effects based on the AE-PSQI global score calculated with test-retest responses.
Internal Consistency
A Cronbach alpha score of 0.65 was obtained, which met “the minimally acceptable” criterion for the internal consistency of the AE-PSQI. The alpha scores were nearly the same for both the baseline and retest scores. The item-to-total correlation coefficients ranged from 0.31 to 0.74, and the smallest component-total correlation coefficient was found for the use of sleep medications, while the largest was found for sleep latency ( Tables 2 ).
Table 2. Item-to-total correlation.
| Items | Item-to-total correlation* | Alpha if item was deleted |
|---|---|---|
| Subjective sleep quality | 0.71 | 0.56 |
| Sleep latency | 0.74 | 0.54 |
| Sleep duration | 0.70 | 0.58 |
| Sleep efficiency | 0.46 | 0.68 |
| Sleep disturbances | 0.44 | 0.64 |
| Use of sleeping medicine | 0.31 | 0.66 |
| Daytime dysfunction | 0.55 | 0.63 |
Note:* Pearson correlation coefficient.
Test-retest Reliability
The ICC(3,1) values revealed strong relative reliability for the global PSQI score. Except for the sleep efficiency component (ICC = 0.26), all other subcomponents showed moderate to strong reliability estimates. There were no statistically significant differences in paired t -tests comparing the test-retest scores ( p > 0.05), and there was no statistically significant systematic bias in the data ( 3 ). The SEM for the global AE-PSQI score was of 1.6 and the SRD was found to be of 4.5.
Table 3. PSQI item characteristics, paired t -test (test 1 versus test 2) p -values, and intraclass correlation coefficients (ICC[3,1]) with 95% confidence intervals and p -values.
| PSQI Items | Test 1: mean |
Test 1: standard deviation | Test 2: mean |
Test 2: standard deviation |
Paired
t
-test:
p -value |
ICC(3,1) | 95%CI | p -value | |
|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||||
| Subjective sleep quality | 1.16 | ± 0.91 | 1.16 | ± 0.79 | 1.000 | 0.66 | 0.48 | 0.79 | < 0.001 |
|
Sleep
latency |
0.78 | ± 0.86 | 0.80 | ± 0.86 | 0.785 | 0.82 | 0.70 | 0.89 | < 0.001 |
| Sleep duration | 1.28 | ± 1.03 | 1.36 | ± 1.05 | 0.552 | 0.59 | 0.37 | 0.74 | < 0.001 |
| Sleep efficiency | 0.56 | ± 0.97 | 0.52 | ± 0.84 | 0.799 | 0.26 | 0 | 0.50 | 0.034 |
| Sleep disturbance | 1.04 | ± 0.53 | 0.94 | ± 0.62 | 0.168 | 0.62 | 0.41 | 0.76 | < 0.001 |
| Use of sleep medication | 0.12 | ± 0.39 | 0.08 | ± 0.34 | 0.322 | 0.70 | 0.52 | 0.82 | < 0.001 |
| Daytime dysfunction | 1.22 | ± 0.84 | 1.10 | ± 0.79 | 0.182 | 0.70 | 0.53 | 0.82 | < 0.001 |
|
Global PSQI
score |
6.16 | ± 3.27 | 5.96 | ± 3.11 | 0.510 | 0.77 | 0.63 | 0.87 | < 0.001 |
Abbreviations: 95%CI, 95% confidence interval; ICC, intraclass correlation coefficient; PSQI, Pittsburg Sleep Quality Index.
Bland-Altman Plot
The Bland-Altman plot depicting the test (1) versus retest (2) mean global AE-PSQI scores is shown in Figure 1 . An analysis of the plot revealed a moderate agreement between both tests because nearly all differences were falling within 1.0 to 1.49 SDs. Only one outlier was present in the plot. Nevertheless, this interpretation is based on arbitrary thresholds suggested by Jensen et al. 53 (2016).
Fig. 1.
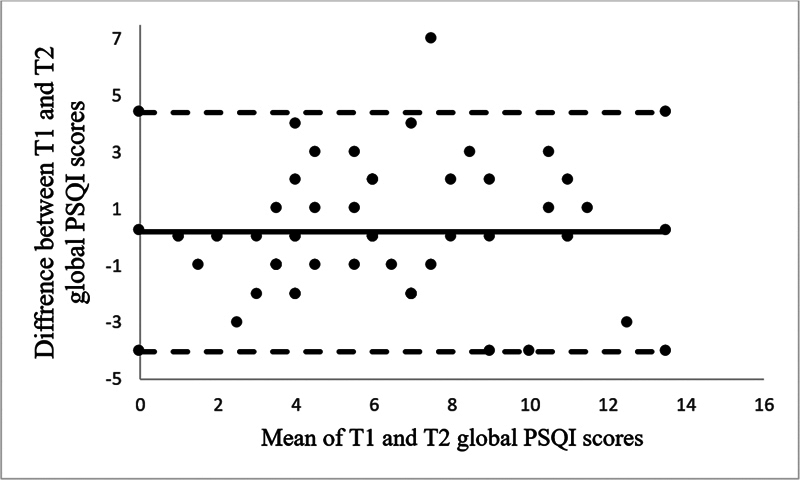
Bland-Altman plot showing agreement between baseline (T1) and retest (T2) global PSQI scores.
Discussion
In the present study, healthy bilingual Arabic-English-speaking adolescents and young adults were recruited to assess the test-retest reliability of AE-PSQI. Even though previous studies 54 55 have used the Arabic version of the PSQI for data collection in young healthy individuals, none of them have assessed the test-retest reliability of the Arabic version or of the AE-PSQI.
The global AE-PSQI score did not show either floor or ceiling effects, which indicates that the item analysis supported the quality of the content validity of the AE-PSQI. In the present study, < 15% of the participants scored lowest or highest scores. The internal consistency of the AE-PQSI was minimally acceptable (Cronbach alpha = 0.65) among our healthy adolescent and young adult participants. Our results are comparable with those of previous studies validating the Italian PSQI in healthy children 56 and the Arabic PSQI in healthy Arab Americans. 37 The Italian and Brazilian version of the PSQI presented good internal consistency values, of 0.72 and 0.71 respectively; however, both versions were focused on one age group: either children or adolescents. 56 57 The Arabic PSQI has been reported to meet the quality assessment criteria for internal consistency. 23 The internal consistency of the original PSQI was found to be fair to good, with a Cronbach alpha value ranging from 0.64 to 0.83. 22 24
Overall, the test-retest reliability estimate for the AE-PSQI global score was strong (ICC = 0.77), while the reliability estimates of other subcomponents, except the sleep efficiency, ranged from moderate to strong. Previous studies have found test-retest reliability estimates to be moderate (r = 0.65) for the Brazilian PSQI version in healthy adolescents 57 and strong (r = 0.83) for the Italian PSQI version in healthy children. 56 Furthermore, two other studies including both healthy and symptomatic participants (with sleep problems) revealed a high internal consistency (Cronbach α = 0.84) and moderate reliability (r = 0.65) for the Korean PSQI, 26 and good internal consistency (Cronbach α = 0.70) and strong reliability (r = 0.83) for the Kurdish PSQI. 58 Therefore, the PSQI has been found to have acceptable internal consistency and reliability, irrespective of the language used.
The SEM of the AE-PSQI global score was of 1.6. Moreover, the SEM of the Brazilian PSQI has been reported to be of 1.1 for healthy adolescents. 57 As the previous study 37 investigating the psychometric properties of the Arabic PSQI in healthy adults has not reported agreement measures, comparisons of SEM/SRD values of the AE-PSQI with that of the Arabic PSQI were not possible.
Strengths and Limitations of the Study
To our knowledge, the present study is the first of its kind investigating the floor and ceiling effects, internal consistency, and test-retest reliability of the AE-PSQI, and positive findings were observed for the AE-PQSI using multiple reliability and agreement estimates. As only healthy adolescents and young adults with good or poor sleep quality were included, the results cannot be generalized to individuals with clinical conditions affecting sleep.
Future Recommendation
Future research is essential to explore various population groups, as a valid and reliable AE-PSQI is needed to support clinical decision-making for interventions that can improve sleep quality. This is particularly relevant for bilingual individuals who speak both Arabic and English and present issues such as insomnia, sleep disorders, chronic pain, fibromyalgia, multiple sclerosis etc. Moreover, other psychometric properties (such as validity and responsiveness) of the AE-PSQI should be investigated further.
Conclusion
The AE-PSQI was found to be a reliable instrument to assess sleep quality in bilingual Arabic-English-speaking adolescents and young adults with good or poor sleep quality. The AE-PSQI demonstrated no floor or ceiling effects, minimally acceptable internal consistency, and moderate to strong test-retest reliability estimates.
Funding Statement
Funding Source The authors declare that they have received no specific grants from funding agencies in the public, private, or not-for-profit sectors for the conduction of the present study.
Conflict of Interests The authors have no conflict of interests to declare.
Authors Contributions
AA: conceptualization, design, supervision, data curation, data analysis, interpretation, drafting, and revision; SAM, HYA, ZAZ, TMEH, HIA, and FSJ: data collection, data curation, interpretation, drafting, and revision; SAM: data analysis; AAS: interpretation, drafting, and critical revision; AA led the writing of the paper; all authors read and approved the final manuscript.
References
- 1.Filip I, Tidman M, Saheba N et al. Public health burden of sleep disorders: underreported problem. Journal of Public Health. 2017;25(03):243–248. doi: 10.1007/s10389-016-0781-0. [DOI] [Google Scholar]
- 2.Colrain I M, Baker F C. Changes in sleep as a function of adolescent development. Neuropsychol Rev. 2011;21(01):5–21. doi: 10.1007/s11065-010-9155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahl R E, Lewin D S. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(06):175–184. doi: 10.1016/S1054-139X(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 4.Fatima Y, Doi S AR, Mamun A A. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17(11):1154–1166. doi: 10.1111/obr.12444. [DOI] [PubMed] [Google Scholar]
- 5.Alkhatatbeh M J, Abdul-Razzak K K, Khwaileh H N. Poor sleep quality among young adults: The role of anxiety, depression, musculoskeletal pain, and low dietary calcium intake. Perspect Psychiatr Care. 2021;57(01):117–128. doi: 10.1111/ppc.12533. [DOI] [PubMed] [Google Scholar]
- 6.Gregory A M, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16(02):129–136. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 7.McKnight-Eily L R, Eaton D K, Lowry R, Croft J B, Presley-Cantrell L, Perry G S.Relationships between hours of sleep and health-risk behaviors in US adolescent students Prev Med 201153(4-5):271–273. 10.1016/j.ypmed.2011.06.020 [DOI] [PubMed] [Google Scholar]
- 8.Palermo T M, Wilson A C, Lewandowski A S, Toliver-Sokol M, Murray C B. Behavioral and psychosocial factors associated with insomnia in adolescents with chronic pain. Pain. 2011;152(01):89–94. doi: 10.1016/j.pain.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Telzer E H, Fuligni A J, Lieberman M D, Galván A. The effects of poor quality sleep on brain function and risk taking in adolescence. Neuroimage. 2013;71:275–283. doi: 10.1016/j.neuroimage.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruce E S, Lunt L, McDonagh J E. Sleep in adolescents and young adults. Clin Med (Lond) 2017;17(05):424–428. doi: 10.7861/clinmedicine.17-5-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai P-S, Wang S Y, Wang M Y et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(08):1943–1952. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 12.Goldman S E, Stone K L, Ancoli-Israel S et al. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007;30(10):1317–1324. doi: 10.1093/sleep/30.10.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhai K, Gao X, Wang G. The role of sleep quality in the psychological well-being of final year undergraduatestudents in China. Int J Environ Res Public Health. 2018;15(12):2881. doi: 10.3390/ijerph15122881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riegel B, Weaver T E. Poor sleep and impaired self-care: towards a comprehensive model linking sleep, cognition, and heart failure outcomes. Eur J Cardiovasc Nurs. 2009;8(05):337–344. doi: 10.1016/j.ejcnurse.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park J. A study on the sleep quality, pain, and instrumental activities of daily living of outpatients with chronic stroke. J Phys Ther Sci. 2019;31(02):149–152. doi: 10.1589/jpts.31.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hui S KA, Grandner M A. Trouble sleeping associated with lower work performance and greater health care costs: Longitudinal data from Kansas state employee wellness program. J Occup Environ Med. 2015;57(10):1031–1038. doi: 10.1097/JOM.0000000000000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kent R G, Uchino B N, Cribbet M R, Bowen K, Smith T W. Social Relationships and Sleep Quality. Ann Behav Med. 2015;49(06):912–917. doi: 10.1007/s12160-015-9711-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skender S, Ose J, Chang-Claude J et al. Accelerometry and physical activity questionnaires - a systematic review. BMC Public Health. 2016;16(01):515. doi: 10.1186/s12889-016-3172-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Axelsson J, Kecklund G, Åkerstedt T. Day-to-day determinants of sleep quality - a longitudinal diary study. Sleep. 2003;26:A300. [Google Scholar]
- 20.Yi H, Shin K, Shin C. Development of the sleep quality scale. J Sleep Res. 2006;15(03):309–316. doi: 10.1111/j.1365-2869.2006.00544.x. [DOI] [PubMed] [Google Scholar]
- 21.Popević M B, Milovanović A PS, Milovanović S, Nagorni-Obradović L, Nešić D, Velaga M. Reliability and Validity of the Pittsburgh Sleep Quality Index-Serbian Translation. Eval Health Prof. 2018;41(01):67–81. doi: 10.1177/0163278716678906. [DOI] [PubMed] [Google Scholar]
- 22.Buysse D J, Reynolds C F, III, Monk T H, Berman S R, Kupfer D J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(02):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 23.Al Maqbali M, Dunwoody L, Rankin J, Hacker E, Hughes C, Gracey J. Psychometric properties and cultural adaptation of sleep disturbance measures in Arabic-speaking populations: A systematic review. J Sleep Res. 2020;29(01):e12877. doi: 10.1111/jsr.12877. [DOI] [PubMed] [Google Scholar]
- 24.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro C M, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 25.Raniti M B, Waloszek J M, Schwartz O, Allen N B, Trinder J. Factor structure and psychometric properties of the Pittsburgh Sleep Quality Index in community-based adolescents. Sleep. 2018;41(06) doi: 10.1093/sleep/zsy066. [DOI] [PubMed] [Google Scholar]
- 26.Sohn S I, Kim D H, Lee M Y, Cho Y W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16(03):803–812. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 27.Del Rio João K A, Becker N B, de Neves Jesus S, Isabel Santos Martins R. Validation of the Portuguese version of the Pittsburgh Sleep Quality Index (PSQI-PT) Psychiatry Res. 2017;247:225–229. doi: 10.1016/j.psychres.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 28.Study of Osteoporotic Fractures . Beaudreau S A, Spira A P, Stewart A et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med. 2012;13(01):36–42. doi: 10.1016/j.sleep.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuksel H, Sogut A, Yilmaz O, Demet M, Ergin D, Kirmaz C. Evaluation of sleep quality and anxiety-depression parameters in asthmatic children and their mothers. Respir Med. 2007;101(12):2550–2554. doi: 10.1016/j.rmed.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 30.Buysse D J, Hall M L, Strollo P J et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(06):563–571. doi: 10.5664/jcsm.27351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mondal P, Gjevre J A, Taylor-Gjevre R M, Lim H J. Relationship between the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in a sleep laboratory referral population. Nat Sci Sleep. 2013;5:15–21. doi: 10.2147/NSS.S40608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doi Y, Minowa M, Uchiyama Met al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects Psychiatry Res 200097(2-3):165–172. 10.1016/S0165-1781(00)00232-8 [DOI] [PubMed] [Google Scholar]
- 33.Kotronoulas G C, Papadopoulou C N, Papapetrou A, Patiraki E. Psychometric evaluation and feasibility of the Greek Pittsburgh Sleep Quality Index (GR-PSQI) in patients with cancer receiving chemotherapy. Support Care Cancer. 2011;19(11):1831–1840. doi: 10.1007/s00520-010-1025-4. [DOI] [PubMed] [Google Scholar]
- 34.Mariman A, Vogelaers D, Hanoulle I, Delesie L, Tobback E, Pevernagie D. Validation of the three-factor model of the PSQI in a large sample of chronic fatigue syndrome (CFS) patients. J Psychosom Res. 2012;72(02):111–113. doi: 10.1016/j.jpsychores.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Skouteris H, Wertheim E H, Germano C, Paxton S J, Milgrom J. Assessing sleep during pregnancy: a study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Womens Health Issues. 2009;19(01):45–51. doi: 10.1016/j.whi.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(03):737–740. doi: 10.1016/S0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 37.Suleiman K H, Yates B C, Berger A M, Pozehl B, Meza J. Translating the pittsburgh sleep quality index into arabic. West J Nurs Res. 2010;32(02):250–268. doi: 10.1177/0193945909348230. [DOI] [PubMed] [Google Scholar]
- 38.Suleiman K, Hadid L A, Duhni A. Psychometric Testing of the Arabic version of the Pittsburgh Sleep Quality Index (A-PSQI) among Coronary Artery Disease Patients in Jordan. Journal of Natural Sciences Research. 2012;2(08):15–19. [Google Scholar]
- 39.Al Maqbali M, Hughes C, Gracey J, Rankin J, Dunwoody L, Hacker E. Validation of the Pittsburgh Sleep Quality Index (PSQI) with Arabic cancer patients. Sleep Biol Rhythms. 2020;18(03):217–223. doi: 10.1007/s41105-020-00258-w. [DOI] [Google Scholar]
- 40.Lee A, Lambert K, Byrne P, Lonergan M. PREVALENCE OF CONSTIPATION IN PATIENTS WITH ADVANCED KIDNEY DISEASE. J Ren Care. 2016;42(03):144–149. doi: 10.1111/jorc.12157. [DOI] [PubMed] [Google Scholar]
- 41.Anati N M, Ain A. Including Students with Disabilities in UAE Schools: A Descriptive Study. Int J Spec Educ. 2012;27(02):75–85. [Google Scholar]
- 42.Karami H. The Development and Validation of a Bilingual Version of the Vocabulary Size Test. RELC J. 2012;43(01):53–67. doi: 10.1177/0033688212439359. [DOI] [Google Scholar]
- 43.Larche C L, Plante I, Roy M, Ingelmo P M, Ferland C E. The Pittsburgh Sleep Quality Index: Reliability, Factor Structure, and Related Clinical Factors among Children, Adolescents, and Young Adults with Chronic Pain. Sleep Disord. 2021;2021:5.546484E6. doi: 10.1155/2021/5546484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Farah N M, Saw Yee T, Mohd Rasdi H F. Self-Reported Sleep Quality Using the Malay Version of the Pittsburgh Sleep Quality Index (PSQI-M) In Malaysian Adults. Int J Environ Res Public Health. 2019;16(23):4750. doi: 10.3390/ijerph16234750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.On Behalf Of The Eclb-Covid Consortium . Trabelsi K, Ammar A, Masmoudi L et al. Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during covid-19 lockdown: Eclb covid-19 international online survey. Int J Environ Res Public Health. 2021;18(08):4329. doi: 10.3390/ijerph18084329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.“wnarifin.github.ioSample size calculator,”[Cited 19 January 2023]. Available from:https://wnarifin.github.io/ssc/ssicc.html
- 47.Norman G R, Streiner D L. Hamilton:: B.C. Decker; 2008. “Biostatistics: The Bare Essentials,”; p. 32. [Google Scholar]
- 48.McHorney C A, Tarlov A R. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4(04):293–307. doi: 10.1007/BF01593882. [DOI] [PubMed] [Google Scholar]
- 49.DeVellis R F. Fourth Edition. Sage publications; 2017. Scale development: Theory and applications. [Google Scholar]
- 50.Xiong P, Spira A P, Hall B J. Psychometric and structural validity of the pittsburgh sleep quality index among filipino domestic workers. Int J Environ Res Public Health. 2020;17(14):1–17. doi: 10.3390/ijerph17145219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Atkinson G, Nevill A M. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26(04):217–238. doi: 10.2165/00007256-199826040-00002. [DOI] [PubMed] [Google Scholar]
- 52.Schuck P, Zwingmann C.The 'smallest real difference' as a measure of sensitivity to change: a critical analysis Int J Rehabil Res 2003260285–91. 10.1097/01.mrr.0000070759.63544.65PubMed [DOI] [PubMed] [Google Scholar]
- 53.Jensen N SO, Camargo Tde FB, Bergamschi D P. Body mass index and waist circumference are good indicators for classifying children's nutritional status. Cien Saude Colet. 2016;21(04):1175–1180. doi: 10.1590/1413-81232015214.138712015. [DOI] [PubMed] [Google Scholar]
- 54.ElHafeez S A, Meira E Cruz M, Gouda S et al. Sleep quality and anxiety among Egyptian population during covid-19 pandemic. Sleep Sci. 2022;15(01):8–16. doi: 10.5935/1984-0063.20210020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Albqoor M A, Shaheen A M. Prevalence and differences in habitual sleep efficiency, sleep disturbances, and using sleep medication: a national study of university students in Jordan. Sleep Breath. 2021;25(02):1127–1134. doi: 10.1007/s11325-020-02174-2. [DOI] [PubMed] [Google Scholar]
- 56.Scialpi A, Mignolli E, De Vito C et al. Italian Validation of the Pittsburgh Sleep Quality Index (PSQI) in a Population of Healthy Children: A Cross Sectional Study. Int J Environ Res Public Health. 2022;19(15):9132. doi: 10.3390/ijerph19159132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Passos M HP, Silva H A, Pitangui A CR, Oliveira V MA, Lima A S, Araújo R C. Reliability and validity of the Brazilian version of the Pittsburgh Sleep Quality Index in adolescents. J Pediatr (Rio J) 2017;93(02):200–206. doi: 10.1016/j.jped.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 58.Seidi P AM, Mohammadi H, Khazaie H, Abas N Q, Jaff D. Psychometric properties of the Kurdish version of Pittsburgh Sleep Quality Index. Sleep Med. 2019;63:75–81. doi: 10.1016/J.SLEEP.2019.04.022. [DOI] [PubMed] [Google Scholar]


