Abstract
In this article, we presented an exceedingly rare clinical case of neurosyphilis, radiological revealed a distinctive “candle guttering appearance.” Posttreatment for syphilis, both clinical symptoms and radiological markers showed complete resolution.
Keywords: syphilis, neurosyphilis, meningomyelitis
Introduction
Early neurosyphilis often shows no significant abnormalities in imaging studies. Syphilitic meningomyelitis is a very rare form of neurosyphilis, with spinal magnetic resonance imaging (MRI) showing the distinctive “candle guttering appearance” being even more uncommon.
Case Description
The patient is a 50-year-old man. On January 31, 2021, he began experiencing progressive numbness and weakness in both lower limbs. Clinical tests conducted on February 7, 2021, revealed a positive syphilis screening (syphilis toluidine red unheated serum test [TRUST]) at 1:32 and positive serum Treponema pallidum hemagglutination assay/ T. pallidum particle agglutination assay (TPPA). By February 9, the symptoms intensified, leading to difficulties in walking, urination, and defecation.
Neurological findings : They are as follows: (1) reduced muscle strength in both lower limbs (grade 4). (2) Increased muscle tone in both lower limbs and attenuated right ankle reflex. (3) Decreased pinprick sensitivity beneath both inguinal areas. (4) Positive bilateral Babinski and Chaddock signs.
Cerebrospinal fluid (CSF) examination : Elevated nucleated cell counts and CSF protein. CSF TRUST was positive at 1:8, and CSF TPPA was also positive. Spinal MRI showed spinal cord swelling at the T2 to T12 vertebral levels. There was an extensive abnormal signal within the cord, manifesting as hyperintensities on both T1 and T2 sequences ( Fig. 1A, B ). Postcontrast images at the levels of T8 and T11 showed nodular enhancement within the spinal cord, exhibiting a “candle dripping sign” ( Fig. 1C, D ).
Fig. 1.
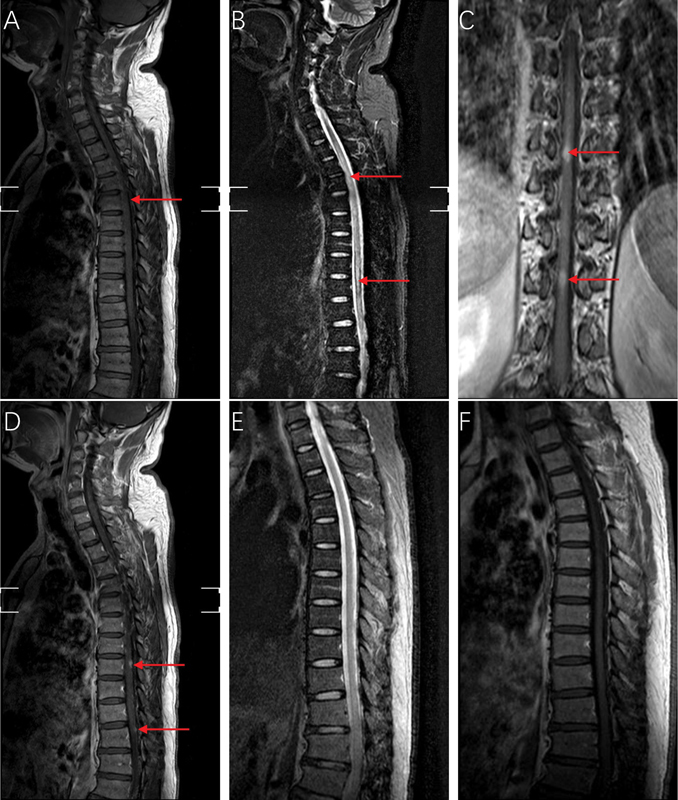
Magnetic resonance imaging of the spinal cord of the patient. ( A ) Sagittal T1-weighted image of the spinal cord showing spinal cord swelling, ( B ) sagittal T2-weighted image of the spinal cord showing long segmental intramedullary hyperintensity, ( C ) coronal T1-weighted enhanced image of the spinal cord showing two enhanced lesions, ( D ) sagittal T1-enhanced image of the spinal cord showing two enhanced lesions (candle guttering appearance), ( E ) sagittal T2-weighted image of the spinal cord after treatment indicating complete resolution of the spinal cord lesions, and ( F ) sagittal T1-weighted image of the spinal cord after treatment indicating complete resolution of the spinal cord swelling.
Treatment and follow-up : Diagnosed with subacute syphilitic meningomyelitis, the patient was administered a 14-day course of penicillin sodium at a dosage of 24 million units per day. Subsequently, the patient received intramuscular injections of benzathine penicillin, at a dosage of 2.4 million units, once a week for a total of 3 weeks. Three months after treatment, the patient's symptoms were alleviated. A follow-up serum TRUST was 1:32, and serum TPPA was positive. Nine months posttreatment, a follow-up serum TRUST test showed a result of 1:2, CSF cell counts and protein levels returned to normal, and the CSF syphilis screening test (TRUST) was negative. Further thoracic spinal MRI revealed complete resolution of the lesion ( Fig. 1E, F ).
Discussion
Syphilitic meningomyelitis was first reported in 1944, 1 clinical manifestations combined with serum and CSF syphilis antibody tests suggest the possible presence of syphilitic meningomyelitis, and spinal MRI plays a crucial role in the diagnosis of syphilitic meningomyelitis. 2 3 4 In 1987, Tashiro et al 5 first reported the MRI manifestations of syphilitic myelitis. In addition to the extensive high signal lesion on the T2-weighted image of the spinal cord, focal nodular enhancement, and spinal cord swelling, the “candle guttering appearance” and “flip-flop sign” are two distinctive radiological presentations of syphilitic meningomyelitis. 6 The “candle guttering appearance” refers to the abnormal peripheral enhancement of the spinal cord, indicating the pial involvement, and is the most common enhancement feature of the lesion. 4 The flip-flop sign, characterized by T1-weighted gadolinium-enhanced images and T2-weighted low signal images, may appear in the phase with pronounced inflammation. 7 Treatment with high doses of penicillin and pulse therapy with prednisolone can reduce spinal cord ischemia and edema.
Conclusion
It is necessary to improve doctors' awareness of syphilitic meningomyelitis and understand its distinctive radiological manifestations.
Funding Statement
Funding None.
Conflict of Interest None declared.
Patient Consent
Informed consent was obtained from the patient for his anonymized information and images to be published in this case report.
Liwen Wang and Jing Fang contributed equally to this work.
References
- 1.Adams R D, Merritt H H. Meningeal and vascular syphilis of the spinal cord. Medicine (Baltimore) 1944;2:181–214. [Google Scholar]
- 2.Berger J R, Dean D. Neurosyphilis. Handb Clin Neurol. 2014;121:1461–1472. doi: 10.1016/B978-0-7020-4088-7.00098-5. [DOI] [PubMed] [Google Scholar]
- 3.Koh P X, Neo S X, Chiew H J, Singh D R, Saini M, Chen Z. Syphilitic spinal disease: an old nemesis revisited. a case series and review of literature. Sex Transm Dis. 2021;48(09):e126–e131. doi: 10.1097/OLQ.0000000000001391. [DOI] [PubMed] [Google Scholar]
- 4.Jiang M J, Zhang H J, Li W R et al. Analysis of EEG Lemple-Ziv complexity and correlative aspects before and after treatment of anti-syphilis therapy for neurosyphilis. Neurol Res. 2019;41(03):199–203. doi: 10.1080/01616412.2018.1520438. [DOI] [PubMed] [Google Scholar]
- 5.Tashiro K, Moriwaka F, Sudo K, Akino M, Abe H. Syphilitic myelitis with its magnetic resonance imaging (MRI) verification and successful treatment. Jpn J Psychiatry Neurol. 1987;41(02):269–271. doi: 10.1111/j.1440-1819.1987.tb00411.x. [DOI] [PubMed] [Google Scholar]
- 6.Wu S, Ye F, Wang Y, Li D. Neurosyphilis: insights into its pathogenesis, susceptibility, diagnosis, treatment, and prevention. Front Neurol. 2024;14:1.340321E6. doi: 10.3389/fneur.2023.1340321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong H, Liu Z, Duan Y et al. Syphilitic meningomyelitis misdiagnosed as spinal cord tumor: case and review. J Spinal Cord Med. 2021;44(05):789–793. doi: 10.1080/10790268.2019.1658283. [DOI] [PMC free article] [PubMed] [Google Scholar]


