Abstract
Purpose
Historically, infraclavicular brachial plexus injuries (IBPIs) were considered neuropraxic injuries that would improve with nonsurgical intervention. However, more recent studies suggest that these injuries may benefit from surgical intervention. The aims of this retrospective study were to (1) describe injury patterns and associated injuries of isolated, traumatic IBPIs, (2) evaluate the concordance of preoperative ultrasound and magnetic resonance neurography with surgical findings of patients who underwent surgical intervention for IBPIs, and (3) describe outcomes of surgical intervention for these injuries.
Methods
A total of 148 patients who underwent surgical intervention for traumatic injury to the IBP by one of three hand/upper-extremity fellowship-trained surgeons from 1995 to 2021 were included. Patients with supraclavicular brachial plexus injuries, stretch injuries, nonsurgical IBPIs, and brachial plexus dysfunction without traumatic injury were excluded.
Results
The most common cause of injury was motor vehicle accident (74%). Scapular fractures were associated with IBPI in 22% of patients. Isolated branch injuries were the most common (58.8%), of which isolated musculocutaneous nerve injury was the most frequent (40.6%). Preoperative ultrasound and magnetic resonance neurography were concordant with surgical findings in eight of nine and seven of nine patients, respectively. Nerve transfers were the most common intervention (46%). Muscle strength improved after surgery, with an increase from 1 to 5 points on the Medical Research Council scale at 14–50 months after surgery.
Conclusions
Infraclavicular brachial plexus injuries are associated with high-energy trauma and concomitant upper-extremity fractures. Ultrasound and magnetic resonance neurography are mostly concordant with surgical findings in patients undergoing surgical intervention for IBPIs. Prognosis for muscle recovery after surgery is good in patients with IBPIs.
Clinical relevance
Infraclavicular brachial plexus injuries can improve with surgical intervention.
Key words: Infraclavicular brachial plexus injury
Brachial plexus injuries (BPIs) are rare but potentially devastating. Brachial plexus injuries may result in social and functional impairment for individuals, and on a societal level, these injuries are associated with substantial health care costs.1 Brachial plexus injuries can be divided into two categories based on their relationship to the clavicle: proximal (supraclavicular) and distal (infraclavicular brachial plexus injury [IBPI]). Isolated supraclavicular and complete BPIs account for 90% of BPI in adults, whereas isolated IBPIs account for the remaining 10%.2,3
Today, motor vehicle accidents remain the most common cause of traumatic BPIs.2,4,5 Given the high-energy mechanism of injury in BPI, concomitant injuries to nearby vascular and osseous structures are common. Previous studies have shown that traumatic supraclavicular and complete BPIs are frequently associated with upper limb fractures, spine injuries, and head trauma.4,5 Isolated IBPIs can occur following shoulder dislocations and proximal humerus fractures.6, 7, 8, 9 Injuries to the axillary nerve, ulnar nerve, and medial cord are most common following anterior shoulder dislocations; axillary and radial nerve injuries are associated with proximal humerus fractures; and musculocutaneous and radial nerve injuries are seen most frequently with arm hyperextension injuries.8, 9, 10
Imaging modalities, such as ultrasound (US) and magnetic resonance neurography (MRN), or peripheral nerve magnetic resonance imaging (MRI), serve as an important adjunct to clinical examination and electrodiagnostic findings in patients with BPIs and may aid in preoperative planning in cases of surgical BPIs. Ultrasound and MRN are especially useful for evaluating nerve continuity and changes in nerve caliber.11, 12, 13, 14 However, the reported accuracy of US and MRI findings compared with intraoperative findings in the setting of traumatic peripheral nerve lesions varies. Some studies have shown high accuracy of US and MRI in detecting traumatic peripheral nerve pathology, such as nerve discontinuity and neuroma formation, relative to intraoperative findings.15, 16, 17 Other studies have found that preoperative US and MRI may be less accurate in the setting of trauma compared with other nontraumatic etiologies of peripheral nerve pathology.18 To our knowledge, no studies to date have examined the accuracy of US and MRN in identifying isolated, traumatic IBPI.
Historically, IBPI were considered neuropraxic injuries that completely recovered without surgical intervention in most patients.19 However, given the increasing number of motor vehicle accidents, improved survival among patients with severe injuries, and global participation in higher velocity sports, in combination with improved imaging and electrodiagnostic modalities to evaluate these injuries, there has been a paradigm shift in the understanding and treatment of these injuries. More recently, authors have advocated for surgical intervention, as the rate of axonotmetic or neurotmetic IBPI is higher than previously reported.20,21 However, outcomes of surgical intervention for IBPI are underreported.
This study’s primary aim was to describe injury patterns and associated injuries of isolated, traumatic surgical infraclavicular BPIs. The secondary aim was to evaluate the concordance of preoperative US and MRN with surgical findings in patients undergoing surgical intervention for IBPIs. The tertiary aim was to describe outcomes of surgical intervention for these injuries.
Materials and Methods
This institutional review board-approved retrospective case series included 1,626 patients who sustained acute, traumatic IBPIs between 1995 and 2021 and underwent surgical intervention by one of three hand and upper-extremity fellowship-trained surgeons at one of two institutions (one in the United States and one in India). Surgical indications were based on the following: physical examination, time course of expected spontaneous recovery, EMG findings, and imaging findings. Patients were identified by review of surgical records for patients who underwent surgery for isolated IBPIs. Patients were included in the study if they underwent surgical intervention for an injury to the divisions, cords, or branches (n = 148). Patients were excluded if they sustained supraclavicular BPIs, stretch injuries to the entire brachial plexus, atraumatic brachial plexus dysfunction (eg, Parsonage Turner Syndrome), or nonsurgical IPBI (n = 1,456). Polytrauma patients were included if they had an isolated IBPI (the remainder of the plexus was intact). Patients with injuries proximal to the IBP (cervical spine and traumatic brain injury) were excluded. The mechanism of injury-associated injuries, injury location, US/MRN findings, surgical findings, surgical interventions, and preoperative or postoperative muscle strength testing (by Medical Research Council Scale) were documented. Magnetic resonance neurography and US were evaluated by musculoskeletal fellowship-trained radiologists (D.B.S. and O.K.N., respectively), and MRN/US reports were reviewed for the present study. The data were reported as percentages. No additional statistical analysis was performed.
Results
Of the 1,626 patients who underwent surgical intervention for IBPIs in our original cohort, 148 met inclusion criteria. Of these 148 patients, 93% were men. Mean age was 30.1 years (range, 10–65 years). Mean time between injury and surgery was 17.6 months (range, 3.2–106.3 months), and mean follow-up time was 33 months from surgery (range, 3–164 months). Most patients were right-hand-dominant (75%), and the right upper extremity was injured in 60% of patients. Thirty-six percent of patients injured their dominant arm (Table 1).
Table 1.
Demographic Information for Patients Included in the Study
| Patient Characteristic | No. (%) |
|---|---|
| Male (n = 148) | 138 (93) |
| Hand dominance: right (n = 16) | 12 (75) |
| Injured side: right (n = 144) | 86 (60) |
| Dominant arm injured (n = 14) | 5 (36) |
| Fracture present (n = 20) | 12 (60) |
| Vascular injury present (n = 20) | 9 (45) |
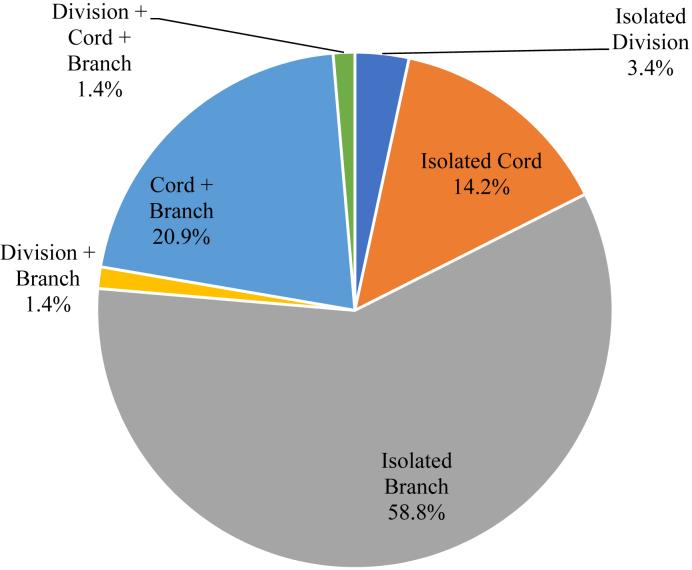
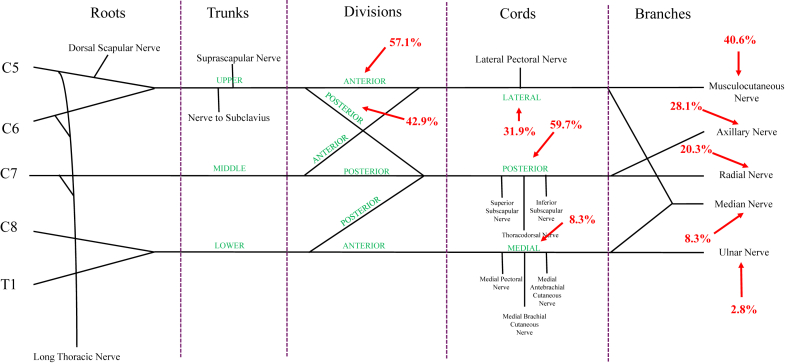
Isolated branch injuries were the most common (58.8%), followed by combined injuries to a cord and a branch (20.9%), and isolated cord injuries (14.2%, Fig. 1). The upper trunk anterior division (57.1%) was involved more frequently than its posterior division (42.9%). For the cords, the posterior cord had the highest injury rate (59.7%), followed by the lateral cord (31.9%) and medial cord (8.3%). For the branches, the musculocutaneous nerve was most frequently involved (40.6%), followed by the axillary (28.1%), radial (20.3%), median (8.3%), and ulnar (2.8%) nerves (Fig. 2).
Figure 1.
Location of infraclavicular brachial plexus injuries. Isolated branch injuries were the most common location of injury.
Figure 2.
Brachial plexus demonstrating frequency of injury to the divisions, cords, and branches.
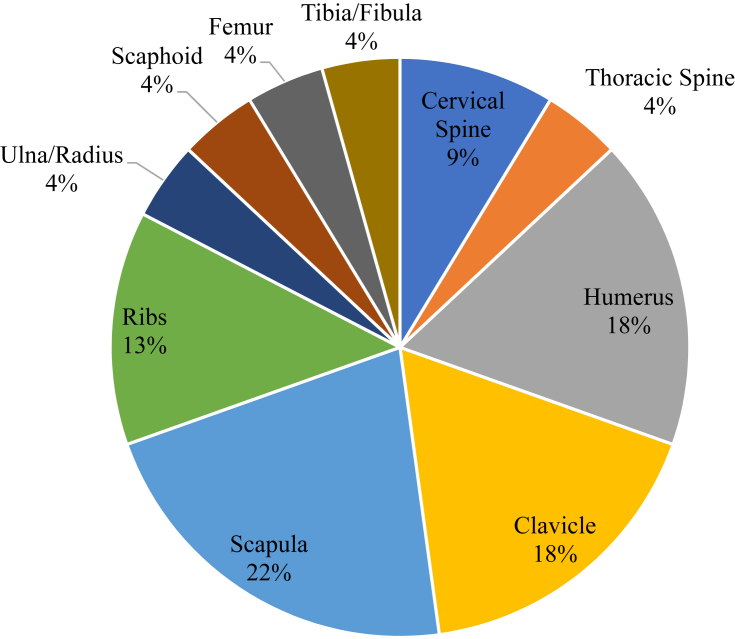
Motor vehicle accidents accounted for the majority of IBPIs (74%), followed by industrial injuries (8%), falls (6%), other injuries (6%), iatrogenic injuries (3%), sports injuries (2%), and gunshot wounds (2%). Fractures of the scapula were the most common in patients with IBPI (22%), followed by fractures of the humerus (18%), clavicle (18%), and ribs (13%, Fig. 3).
Figure 3.
Fractures associated with infraclavicular brachial plexus injuries.
Diagnostic ultrasound (DUS) and intraoperative findings were concordant in eight of nine patients with DUS and detailed surgical reports were available. Magnetic resonance neurography and intraoperative findings were concordant in seven of nine patients with MRN and detailed surgical reports were available (Table 2).
Table 2.
Concordance of US and MRN Findings in Patients With IBPI
| Intraoperative Location of Injury | MRN Location of Injury | US Location of Injury | MRN Concordant With Surgical Findings? (Yes/No) | US Concordant With Surgical Findings? (Yes/No) |
|---|---|---|---|---|
| Medial cord, lateral cord, and musculocutaneous nerve | Injury not specified within plexus—likely roots through branches | No∗ | ||
| Medial cord, median nerve, ulnar nerve, and radial nerve | Lateral cord, median nerve, ulnar nerve, and radial nerve | Yes, mostly | ||
| Axillary nerve | Axillary nerve | Yes | ||
| Posterior cord, musculocutaneous nerve, radial nerve, and axillary nerve | Musculocutaneous nerve, radial nerve, and axillary nerve | Posterior cord | Yes, mostly† | Yes, mostly |
| Lateral cord, posterior cord, and musculocutaneous nerve | All divisions and cords | Lateral cord, posterior cord, musculocutaneous nerve | No‡ | Yes |
| Median nerve and radial nerve | Median nerve and radial nerve | Median nerve and radial nerve | Yes | Yes |
| Musculocutaneous nerve, median nerve, and radial nerve | Musculocutaneous fascicular bundle of lateral cord, posterior cord (radial and axillary fascicular bundles), radial nerve, median nerve, and ulnar nerve | Radial nerve, median nerve, and ulnar nerve | Yes | Yes |
| Axillary nerve | Axillary nerve | Yes | ||
| Medial cord, musculocutaneous nerve, median nerve, ulnar nerve, and axillary nerve | Medial cord, musculocutaneous nerve, and axillary nerve | Posterior cord, axillary nerve∗ | Yes, mostly§ | No§ |
| Posterior cord, medial cord, and ulnar nerve | Posterior cord and ulnar nerve | Posterior cord, medial cord, and ulnar nerve | Yes, mostly¶ | Yes |
| Lateral cord | Lateral cord | Yes | ||
| Lateral cord, medial cord, median nerve, and ulnar nerve | Lateral cord, medial cord, median nerve, and ulnar nerve | Yes |
Metal artifact from previous hardware.
Cords were normal on MRN.
MRN does not specify which divisions/cords.
Infraclavicular brachial plexus evaluation limited by postsurgical scar tissue from clavicle distal to axilla.
Medial cord well-maintained on MRN.
The most common surgical intervention performed was an isolated nerve transfer (46%), followed by nerve graft + nerve transfer (28%), isolated nerve graft (22%), nerve graft + tendon transfer (2%), isolated tendon transfer (1%), combined nerve graft + nerve transfer + tendon transfer (1%), and isolated neurolysis (1%). The most common nerve transfers included the following ulnar nerve to biceps (29.2%), Somsak transfer (19.8%), median nerve to brachioradialis (18.9%), intercostal nerve to triceps (17.9%), thoracodorsal nerve to triceps (15.1%), and intercostal nerve to musculocutaneous nerve (14.2%). The most common tendon transfers included latissimus to biceps (71%), flexor carpi radialis to extensor digitorum communis (14.5%), and palmaris longus to extensor pollicus longus (14.5%).
Preoperative and postoperative muscle strength data were available for 10 patients. All patients had strength improvement of at least 1 point on the Medical Research Council scale in each muscle group tested (Table 3).
Table 3.
MRC Strength Before and After Surgery for the Patients With Both Preoperative and Postoperative Strength Information Available
|
Procedure Category |
Procedures | Time Between Injury and Surgery (Mo) | Latest Follow-Up (Mo) | Before Surgery |
After Surgery |
Delta |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Biceps | Triceps | Deltoid | FCR | FDS | FPL | Biceps | Triceps | Deltoid | FCR | FDS | FPL | Biceps | Triceps | Deltoid | FCR | FDS | FPL | ||||
| Tendon transfer | FDP LF to IF/LF/RF/SF | 18.7 | 18 | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 5 | 4 | 1 | 5 | 5 | 4 | |||||
| Neurolysis | Neurolysis only | 3.2 | 14.2 | 4 | 0 | 0 | 5 | 4 | 1 | 4 | |||||||||||
| Nerve transfer + neurolysis | TD nerve to radial nerve, median nerve to biceps, ulnar nerve to brachialis muscle, and neurolysis | 5.6 | 18.9 | 0 | 1 | 3 | 4 | 4 | 4 | 4 | 3 | 1 | |||||||||
| Nerve transfer + nerve graft + neurolysis | NT: spinal accessory nerve to suprascapular nerve (contains NG), NT: medial head of triceps to teres minor, and NT: long head of triceps to axillary nerve, neurolysis | 9.7 | 49.9 | 5 | 5 | 0 | 5 | 4 | 4 | ||||||||||||
| Tendon transfer + nerve graft + nerve transfer + neurolysis | NG: median nerve, ulnar nerve, radial nerve, NT: brachialis to AIN, and TT: FDP (side-to-side), neurolysis | 4.9 | 23.7 | 5 | 0 | 5 | 5 | 4 | 5 | 4 | 4 | ||||||||||
| Nerve transfer + neurolysis | Radial nerve to axillary nerve, neurolysis | 5.9 | 12.9 | 5 | 5 | 3 | 5 | 5 | 4 | 1 | |||||||||||
| Nerve transfer + nerve graft + neurolysis | NG: axillary nerve, radial nerve, NT: ulnar nerve to biceps, median nerve to brachioradialis, neurolysis | 5.6 | 25.1 | 0 | 0 | 0 | 4 | 3 | 4 | 4 | 3 | 4 | |||||||||
| Nerve graft + neurolysis | Axillary nerve, neurolysis | 5.4 | 47.7 | 5 | 3 | 0 | 5 | 5 | 4 | 2 | 4 | ||||||||||
| Nerve transfer | Medial pectoral nerve to musculocutaneous nerve | 4.7 | 22.4 | 0 | 0 | 2 | 0 | 4 | 4 | 4 | 4 | 4 | 4 | 2 | 4 | ||||||
| Neurolysis | Neurolysis only | 5.5 | 35.8 | 4 | 4 | 3 | 3 | 0 | 0 | 5 | 5 | 5 | 4 | 4 | 1 | 1 | 2 | 1 | 4 | ||
AIN, anterior interosseous nerve; FCR, flexor carpi radialis; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus; IF, index finger; LF, long finger; MRC, Medical Research Council; NG, nerve graft; NT, nerve transfer; RF, ring finger; SF, small finger; TD, thoracodorsal.
Discussion
We found that isolated branch injuries were the most common injury pattern, with the musculocutaneous and axillary nerves most frequently involved in patients undergoing surgery for IBPIs. Most patients were young men who sustained a motor vehicle accident with associated fractures of the humerus, scapula, and/or ribs. Preoperative US correctly identified the location of IBPI in 8/9 patients and MRN correctly identified the location of IBPI in 7/9 patients, with detailed imaging and surgical data available. Postsurgical scarring and metal artifacts accounted for two of the three discordant cases. Nearly half of all patients underwent nerve transfers, and the most common transfer was ulnar nerve to biceps. Among patients who had muscle strength data available, muscle recovery was excellent following plexus surgery.
Similar to previous studies, we found that the majority of traumatic surgical BPI in our cohort occurred in young men following motor vehicle accidents and were frequently associated with fractures of the shoulder girdle.4,5 Given the close proximity to the surgical neck of the proximal humerus, the axillary and musculocutaneous nerves may be particularly susceptible to injury in patients with proximal humerus fractures.
In the present study, DUS was concordant with surgical findings in eight of nine patients who had detailed imaging and surgical information available. The one patient for whom DUS was not concordant with surgical findings had a subtantial amount of postsurgical scarring extending from the clavicular to axillary regions, which limited full evaluation of the infraclavicular brachial plexus on US. Magnetic resonance neurography was concordant with surgical findings in seven of nine patients. In one of these patients, there was metal artifact that obscured the brachial plexus distal to the clavicle. Our results follow those of Gruber et al,22 who found that high-resolution US had high positive predictive and negative predictive values (1.0 and 0.92, respectively) for diagnosing supraclavicular brachial plexus injuries compared with intraoperative findings.
Rates of muscle strength recovery following different surgical interventions for IBPIs, including nerve grafting, nerve transfers, and nerve repair, are mixed in the literature.9,23,24 Wu et al10 found good prognosis for muscle recovery in lateral (11/11) and posterior cord injuries (20/24) and isolated axillary nerve injuries (22/28), following anterior shoulder dislocation. Those with medial cord injuries had the poorest prognosis for recovery (14/27) at a minimum 8-month follow-up. Our results suggest that prognosis for muscle recovery after surgery is good following surgical intervention for IBPIs.
We acknowledge several limitations in the present study. First, this is a retrospective study; therefore, surgical interventions were not randomized. In addition, the present study was an interinstitutional and intercontinental collaboration, and complete chart information, including associated injuries, muscle strength, and imaging data, was not available for 83% of the included patients. However, the location of injury information (based on surgical findings) was available for all patients included in the study, and all patients included in the study had isolated surgical IBPI.
Notably, at the senior author’s institution, imaging is performed on all patients with IBPI, and given the interinstitutional nature of the present study, detailed imaging information was only available for a subset of patients included in the final cohort. Additionally, as the cases spanned a wide time range, imaging protocols and quality varied with implementation of more recent improvements, particularly in MRN, over the past 3 years at the senior author’s institution. EMGs were performed on a small subset of patients and, therefore, were not included in the present study. Finally, this study is susceptible to sample bias as only included patients who underwent surgical intervention for IBPIs, and the prognosis for muscle recovery for patients undergoing surgical intervention could not be compared with those who were managed nonoperatively. The recovery rate of nonsurgical IBPI can be explored in future investigations.
In conclusion, the prognosis for muscle recovery is good in patients who undergo surgical intervention with IBPI. Ultrasound and MRN are valuable imaging modalities that can accurately identify the location of injury in patients with IBPIs.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
References
- 1.Hong T.S., Tian A., Sachar R., Ray W.Z., Brogan D.M., Dy C.J. Indirect cost of traumatic brachial plexus injuries in the United States. J Bone Joint Surg Am. 2019;101(16) doi: 10.2106/JBJS.18.00658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaiser R., Waldauf P., Ullas G., Krajcová A. Epidemiology, etiology, and types of severe adult brachial plexus injuries requiring surgical repair: systematic review and meta-analysis. Neurosurg Rev. 2020;43(2):443–452. doi: 10.1007/s10143-018-1009-2. [DOI] [PubMed] [Google Scholar]
- 3.Bertelli J.A., Ghizoni M.F., Soldado F. Patterns of brachial plexus stretch palsy in a prospective series of 565 surgically treated patients. J Hand Surg Am. 2017;42(6):443–446.e2. doi: 10.1016/j.jhsa.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 4.Kaiser R., Mencl L., Haninec P. Injuries associated with serious brachial plexus involvement in polytrauma among patients requiring surgical repair. Injury. 2014;45(1):223–226. doi: 10.1016/j.injury.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Faglioni W., Jr., Siqueira M.G., Martins R.S., Heise C.O., Foroni L. The epidemiology of adult traumatic brachial plexus lesions in a large metropolis. Acta Neurochir (Wien) 2014;156(5):1025–1028. doi: 10.1007/s00701-013-1948-x. [DOI] [PubMed] [Google Scholar]
- 6.Le Hanneur M., Colas M., Serane-Fresnel J., et al. Endoscopic brachial plexus neurolysis in the management of infraclavicular nerve injuries due to glenohumeral dislocation. Injury. 2020;51(11):2592–2600. doi: 10.1016/j.injury.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Kim D.H., Murovic J.A., Tiel R.L., Kline D.G. Infraclavicular brachial plexus stretch injury. Neurosurg Focus. 2004;16(5) [PubMed] [Google Scholar]
- 8.Hems T.E., Mahmood F. Injuries of the terminal branches of the infraclavicular brachial plexus: patterns of injury, management and outcome. J Bone Joint Surg Br. 2012;94(6):799–804. doi: 10.1302/0301-620X.94B6.28286. [DOI] [PubMed] [Google Scholar]
- 9.Lam W.L., Fufa D., Chang N.J., Chuang D.C. Management of infraclavicular (Chuang Level IV) brachial plexus injuries: a single surgeon experience with 75 cases. J Hand Surg Eur Vol. 2015;40(6):573–582. doi: 10.1177/1753193414553753. [DOI] [PubMed] [Google Scholar]
- 10.Wu F., Dhir R., Ng C.Y. Patterns of nerve injury and recovery rates of infraclavicular brachial plexus lesions following anterior shoulder dislocation. J Hand Surg Am. 2022;47(12):1227.e1–1227.e7. doi: 10.1016/j.jhsa.2021.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Nischal N., Gupta S., Lal K., Singh J.P. Performance evaluation of high-resolution ultrasound versus magnetic resonance imaging in diagnosing peripheral nerve pathologies. Indian J Radiol Imaging. 2021;31(1):43–48. doi: 10.1055/s-0041-1729130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aggarwal A., Srivastava D.N., Jana M., et al. Comparison of different sequences of magnetic resonance imaging and ultrasonography with nerve conduction studies in peripheral neuropathies. World Neurosurg. 2017;108:185–200. doi: 10.1016/j.wneu.2017.08.054. [DOI] [PubMed] [Google Scholar]
- 13.Szaro P., Geijer M., Ciszek B., McGrath A. Magnetic resonance imaging of the brachial plexus. Part 2: traumatic injuries. Eur J Radiol Open. 2022;9 doi: 10.1016/j.ejro.2021.100392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toia F., Gagliardo A., D’Arpa S., Gagliardo C., Gagliardo G., Cordova A. Preoperative evaluation of peripheral nerve injuries: what is the place for ultrasound? J Neurosurg. 2016;125(3):603–614. doi: 10.3171/2015.6.JNS151001. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal A., Chandra A., Jaipal U., et al. Can imaging be the new yardstick for diagnosing peripheral neuropathy?-a comparison between high resolution ultrasound and MR neurography with an approach to diagnosis. Insights Imaging. 2019;10(1):104. doi: 10.1186/s13244-019-0787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen D.Z., Cong R., Zheng M.J., et al. Differential diagnosis between pre- and postganglionic adult traumatic brachial plexus lesions by ultrasonography. Ultrasound Med Biol. 2011;37(8):1196–1203. doi: 10.1016/j.ultrasmedbio.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 17.Umans H., Kessler J., de la Lama M., Magge K., Liebling R., Negron J. Sonographic assessment of volar digital nerve injury in the context of penetrating trauma. AJR Am J Roentgenol. 2010;194(5):1310–1313. doi: 10.2214/AJR.09.3884. [DOI] [PubMed] [Google Scholar]
- 18.Zaidman C.M., Seelig M.J., Baker J.C., Mackinnon S.E., Pestronk A. Detection of peripheral nerve pathology: comparison of ultrasound and MRI. Neurology. 2013;80(18):1634–1640. doi: 10.1212/WNL.0b013e3182904f3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leffert R.D., Seddon H. Infraclavicular brachial plexus injuries. J Bone Joint Surg Br. 1965;47:9–22. [PubMed] [Google Scholar]
- 20.Burge P., Rushworth G., Watson N. Patterns of injury to the terminal branches of the brachial plexus. The place for early exploration. J Bone Joint Surg Br. 1985;67(4):630–634. doi: 10.1302/0301-620X.67B4.4030864. [DOI] [PubMed] [Google Scholar]
- 21.Guy I., Guerero D., Shirley C., Edwards C., Miller C., Power D. Patterns of injury to the infraclavicular brachial plexus following dislocation of the glenohumeral joint. J Musculoskelet Surg Res. 2019;3:90–97. [Google Scholar]
- 22.Gruber H., Glodny B., Galiano K., et al. High-resolution ultrasound of the supraclavicular brachial plexus–can it improve therapeutic decisions in patients with plexus trauma? Eur Radiol. 2007;17(6):1611–1620. doi: 10.1007/s00330-006-0464-2. [DOI] [PubMed] [Google Scholar]
- 23.Alnot J.Y. Traumatic brachial plexus palsy in the adult. Retro- and infraclavicular lesions. Clin Orthop Relat Res. 1988;237:9–16. [PubMed] [Google Scholar]
- 24.Sulaiman O.A., Kim D.D., Burkett C., Kline D.G. Nerve transfer surgery for adult brachial plexus injury: a 10-year experience at Louisiana State University. Neurosurgery. 2009;65(4 suppl):A55–A62. doi: 10.1227/01.NEU.0000341165.83218.AC. [DOI] [PubMed] [Google Scholar]