Abstract
Purpose
The use of a person’s hands is crucial to their ability to succeed at work. Hand pathologies can impact work success by increasing absenteeism (ie, not being able to go to work) and presenteeism (ie, being able to work but in a reduced capacity). In this study, we quantified employed patients’ presenteeism and absenteeism following carpal tunnel release or surgical fixation of a distal radius fracture (DRF).
Methods
In this prospective cohort study, 91 patients (carpal tunnel syndrome [CTS]: n = 62; DRF: n = 29) from June 2022 to December 2023 were included. Baseline patient characteristics and patient-reported outcome measures (PROMs) were collected. Presenteeism and absenteeism were calculated using the World Health Organization’s Health and Work Performance Questionnaire. Questionnaires were sought before surgery and at 3 and 6 months after surgery. Clinical improvement was determined using minimal clinically important difference (MCID) cutoff range estimates. The employee value of lost work was calculated as a percentage of the average patient in each group before surgery and at 6 months after surgery.
Results
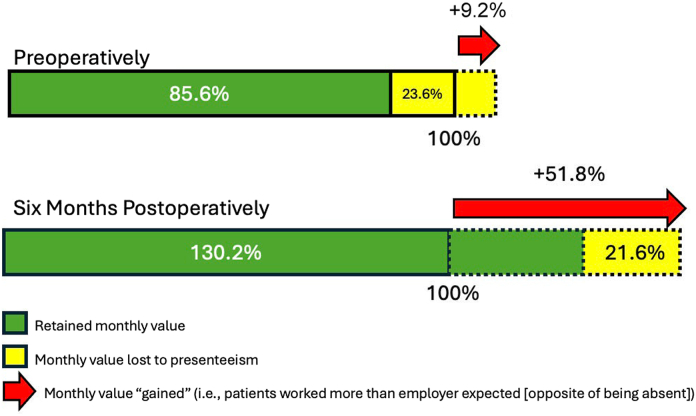
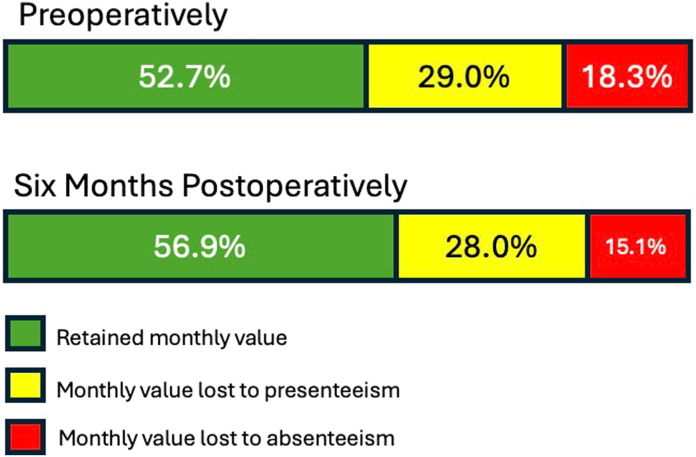
The average change in PROMs scores from before to after surgery at 6 months surpassed the low-end MCID estimates for all functional and pain-related PROMs. For patients undergoing surgery for CTS and DRF, retained employee value rose from 85.6% to 130.2% (ie, worked more than expected) and 52.7% to 56.9%, respectively.
Conclusions
Patients undergoing surgery for CTS or DRF have clinically appreciable improvement in functional and pain symptoms by 6 months after surgery. However, by 6 months after surgery, carpal tunnel release results in greater than complete employee value recovery, compared with surgical fixation of DRFs in which greater than 40% of the employee value remains lost after surgery. These findings can assist with preoperative expectation setting.
Type of study/level of evidence
Prognostic II.
Key words: Absenteeism, Economics, Patient-reported outcome measures, Presenteeism, PROMs, Value
As the leading contributor to disability globally, musculoskeletal injuries can be devastating to individuals, negatively impacting their quality of life, involvement in communities, and work productivity.1 From a societal perspective, musculoskeletal conditions cost the US $213 billion (US Dollars [USD]) in direct and indirect costs in 2011, representing 1.4% of the country’s gross domestic product.2 Within musculoskeletal injuries, the economic impact of hand and upper-extremity (UE) injuries is substantial; in fact, in 2012, hand and UE injuries cost the Netherlands $740 million (USD),3 the most of any musculoskeletal injury type.
Although the economic impact of musculoskeletal conditions, including hand and UE pathologies, is evident, previous studies quantifying the financial effect have focused primarily on missed work (ie, absenteeism). Indeed, the financial impact of hand and wrist surgery often highlights the time to return to work4,5 and, to a lesser extent, the financial burden for patients.6 Although these prior studies inform a great deal of the economic aspects of care for common hand and UE conditions, they fail to consider the impact of these pathologies on people who are at work but perform below their optimal ability, negatively impacting economic productivity and well-being. This concept is known as presenteeism.
A number of studies have found that a variety of musculoskeletal conditions cause increased presenteeism (ie, decreased performance while at work).7, 8, 9 However, there is a paucity of literature examining presenteeism in a hand and UE setting, with one study assessing presenteeism following surgical and nonsurgical treatment for trapeziometacarpal osteoarthritis10 and another considering “work role functioning” (ie, ability to meet work demands) in patients undergoing carpal tunnel release (CTR).11 Using a convenience sample of patients undergoing surgical intervention for carpal tunnel syndrome (CTS) or distal radius fracture (DRF), a common atraumatic and traumatic hand and UE condition, respectively,12,13 this study sought to (1) assess when patients demonstrate clinically appreciable improvement in symptoms through 6 months after surgery using patient-reported outcome measures (PROMs); (2) quantify the level of absenteeism and presenteeism before surgery, 3 months after surgery, and 6 months after surgery; and (3) determine the monthly employee value lost or gained, on average, before surgery and 6 months after surgery.
We hypothesized that patients undergoing surgery for CTS or DRF would experience clinically appreciable improvement in symptoms by 6 months after surgery but that average monthly patient employee value would be less than 100% at 6 months after surgery. We also hypothesized that the lost employee value would be more substantial for patients with a DRF requiring surgery when compared with those with CTS undergoing CTR at the 6 months after surgery.
Materials and Methods
This prospective cohort study was approved by our institutional review board (Protocol #2022P000076) and completed with grant support from the American Foundation for Surgery of the Hand (AFSH) [2021 Resident/Fellow Fast Track Grant; Award 3761].
Between June 2022 and December 2023, patients with isolated, unilateral CTS or DRF that had surgical intervention by one of two hand and UE fellowship-trained surgeons were identified and approached for study inclusion. CTR was performed using a mini-open approach. A standard volar approach was used for all DRFs undergoing open reduction and internal fixation (ORIF). Patients under the age of 18 years who had nonisolated CTS or DRF, who had a diagnosis of inflammatory arthritis, who did not undergo surgical intervention, or who were unemployed were excluded.
A total of 97 patients were consented and enrolled. However, three patients exited the study shortly after enrolling, and three additional patients were identified during the clinic visit as having concurrent injuries. Thus, a total of 91 patients (CTS: n = 62; DRF: n = 29) completed the study.
The following patient characteristics were recorded: age (in years), sex (man or woman), self-reported race (White, Black, Asian, or unknown/declined to answer), self-reported ethnicity (non-Hispanic, Hispanic, or unknown/declined to answer), smoking status (never, former, current, or unknown/declined to answer), employment status (full-time, part-time, or unknown/declined to answer), and insurance type (commercial, Medicare, Medicaid, Workers’ Compensation, or other).
Before surgery, at 3 months after surgery, and at 6 months after surgery, one static hand and UE PROM—the quick disabilities of the arm, shoulder, and hand (QuickDASH)—was collected. The QuickDASH is a validated shortened version of the DASH that is scored from 0 (no disability) to 100 (most severe disability).14 In addition, at the same time points, the patient-reported outcomes measurement information system (PROMIS) UE computerized adaptive test (CAT) v2.0, PROMIS physical function (PF) CAT v1.2, PROMIS pain interference (PI) CAT v1.1, and PROMIS depression CAT v1.0 were collected. The PROMIS questionnaires are general, validated PROMs developed with substantial support from the US National Institutes of Health that are gaining popularity throughout orthopaedic surgery,15 including in hand and UE surgery.16 PROMIS domains were developed and normalized to a general reference population, with a mean T-score of 50 and a SD of 10.17 Higher PROMIS domain score represent “more” of that concept being measured (eg, more PF, more PI, and more depressive symptoms).
The World Health Organization’s Health and Work Performance Questionnaire (WHO-HPQ) was administered before surgery (at the final clinic visit prior to surgery), at 3 months after surgery, and at 6 months after surgery. The WHO-HPQ is a validated, responsive, and sensitive instrument that measures presenteeism and absenteeism across a wide range of job types18 and health conditions.19 Similar to previously published literature in hand surgery,20 we took the score (0 = worst performance to 10 = top performance) on the presenteeism question “Your overall job performance on the days you worked during the past 4 weeks?” and multiplied it by 10 to create an absolute presenteeism score; this represented the percentage of time while at work over the prior 28 days that was productive.21 Thus, a higher absolute presenteeism score is preferred. Absolute absenteeism over the prior 28 days was calculated by taking the answer to the question “How many hours does your employer expect you to work in a typical 7-day week?” and multiplying it by four before subtracting the answer to the question “About how many hours altogether did you work in the past 4 weeks (28 days)?”21 The resulting absolute absenteeism score is in raw hours, with negative scores representing someone working more than an employer expects and positive numbers up to the number of hours an employer expects representing hours missed from work.21 Employee value was then calculated as follows. First, the total number of expected work hours per month was determined. Second, hours lost to absenteeism were then subtracted (or added if patients worked more than was expected of them). Third, the absolute presenteeism score (or percentage of the time while at work over the prior 28 days that was productive) was used on any “remaining hours” to determine the final “employee value.” Ultimately, if an employee worked at full productivity all hours expected by their employee, their employee value would be 100%. If an employee worked fewer hours than expected by their employer or the same number of hours but at a lower level of productivity, their employee value would be 100% minus the percentage not worked and/or amount of work performed at a lower level of productivity; in contrast, if an employee worked more hours than expected by their employer, their employee value would be 100% plus the percentage worked above what was expected minus the percentage lost to work performed at a lower level of productivity.
Statistical analysis
Descriptive statistics were used to summarize patient characteristics collected at presentation. PROMs scores, absolute presenteeism, and absolute absenteeism at each time point were calculated and reported as means and standard deviations (SDs). Patients with missing data at each time point were excluded from the respective analysis.
Assessment of clinical improvement was determined by examining changes in PROMs scores to see if they exceeded minimal clinically important difference (MCID) estimates. Based on the published literature, the QuickDASH MCID estimate range used was 10.4 to 14.22,23 For patients undergoing CTR for CTS, the MCID estimates were as follows: PROMIS UE (4.2–6.3), PF (1.8–2.8), and PI (4.1–8.9).24 For patients undergoing surgical management for a DRF, published MCID estimates for PROMIS PF (5.2) and PROMIS PI (6.8) were used.25 If a published MCID estimate or estimate range was not available for a given PROM and condition, the distribution-based method of one-half of the SD was used.26 A change in PROMs scores greater than MCID estimates suggested appreciable clinical improvement in the symptom being measured.
Using a similar methodology to the one used in prior studies,20,27 the monthly average employee value employers lose to presenteeism and absenteeism was calculated in percentage terms before surgery and at 6 months after surgery using the WHO-HPQ
Results
The average age of included patients was 55 years (SD: 12 years) and a majority were woman (n = 64 [71%]; Table 1). Most patients worked full-time (n = 81 [89%]) and had commercial insurance (n = 73 [80%]; Table 1).
Table 1.
Patient Characteristics (n = 91)
| Characteristic | n (%) or mean (SD) |
|---|---|
| Age, y | 55 (12) |
| Sex | |
| Woman | 64 (71) |
| Man | 26 (29) |
| Self-reported race | |
| White | 71 (78) |
| Black | 9 (9.9) |
| Asian | 4 (4.4) |
| Unknown/declined to answer | 7 (7.7) |
| Self-reported ethnicity | |
| Non-Hispanic | 83 (91) |
| Hispanic | 6 (6.6) |
| Unknown/declined to answer | 2 (2.2) |
| Smoking status | |
| Never | 78 (86) |
| Former | 11 (12) |
| Current | 1 (1.1) |
| Unknown/declined to answer | 1 (1.1) |
| Employment status | |
| Full-time | 81 (89) |
| Part-time | 9 (9.9) |
| Unknown/declined to answer | 1 (1.1) |
| Insurance type | |
| Commercial | 73 (80) |
| Medicare | 11 (12) |
| Medicaid | 1 (1.1) |
| Workers’ compensation | 2 (2.2) |
| Other | 4 (4.4) |
| Surgical intervention | |
| Carpal tunnel release | 62 (68) |
| DRF open reduction and internal fixation | 29 (32) |
Using the low end and distribution-based MCID estimates, patients with both pathologies undergoing surgical intervention demonstrated a change in PROMs scores from the preoperative time point to 6 months after surgery above the MCID threshold for all PROMs except for PROMIS depression (Table 2).
Table 2.
PROMs, Absenteeism, and Presenteeism at Different Time Points
| Carpal Tunnel Syndrome (n = 62) |
DRF (n = 29) |
||
|---|---|---|---|
| PROM | Mean (SD) | PROM | Mean (SD) |
| QuickDASH | QuickDASH | ||
| Before surgery | 41 (23) | Before surgery | 76 (14) |
| After surgery, 3 mo | 20 (20) | After surgery, 3 mo | 20 (18) |
| After surgery, 6 mo | 18 (21) | After surgery, 6 mo | 10 (9.5) |
| PROMIS upper extremity | PROMIS upper extremity | ||
| Before surgery | 41 (12) | Before surgery | 27 (8.3) |
| After surgery, 3 mo | 45 (10) | After surgery, 3 mo | 41 (7.3) |
| After surgery, 6 mo | 46 (11) | After surgery, 6 mo | 47 (8.9) |
| PROMIS PF | PROMIS PF | ||
| Before surgery | 47 (10) | Before surgery | 35 (9.3) |
| After surgery, 3 mo | 50 (11) | After surgery, 3 mo | 51 (5.9) |
| After surgery, 6 mo | 50 (10) | After surgery, 6 mo | 53 (9.1) |
| PROMIS PI | PROMIS PI | ||
| Before surgery | 58 (8.0) | Before surgery | 63 (9.6) |
| After surgery, 3 mo | 52 (11) | After surgery, 3 mo | 49 (7.3) |
| After surgery, 6 mo | 51 (9.9) | After surgery, 6 mo | 47 (7.6) |
| PROMIS depression | PROMIS depression | ||
| Before surgery | 51 (8.2) | Before surgery | 53 (6.4) |
| After surgery, 3 mo | 49 (7.2) | After surgery, 3 mo | 48 (6.0) |
| After surgery, 6 mo | 47 (8.5) | After surgery, 6 mo | 51 (7.4) |
| Absolute presenteeism, % | Absolute presenteeism, % | ||
| Before surgery | 76 (25) | Before surgery | 79 (23) |
| After surgery, 3 mo | 87 (14) | After surgery, 3 mo | 82 (17) |
| After surgery, 6 mo | 84 (15) | After surgery, 6 mo | 79 (12) |
| Absolute absenteeism, hours lost/month∗ | Absolute absenteeism, hours lost/month∗ | ||
| Before surgery | 3.6 (56) | Before surgery | 29 (41) |
| After surgery, 3 mo | 9.2 (48) | After surgery, 3 mo | 12 (72) |
| After surgery, 6 mo | -21 (77) | After surgery, 6 mo | 22 (57) |
Negative numbers represent someone working more than is expected of him/her over a month-long period. Note: patient “n” represents the number of patients enrolled overall and with each pathology requiring surgery.
In the sample of patients undergoing CTR, absolute presenteeism went from 76 (SD: 25) to 87 (SD: 14) to 84 (SD: 15) at preoperative, 3 months postoperative, and 6 months postoperative time points, respectively (Table 2). Across the same sample, absolute absenteeism went from 3.6 hours (SD: 56 hours) to 9.2 hours (SD: 48 hours) to −21 hours (SD: 77 hours) at preoperative, 3 months postoperative, and 6 months postoperative time points, respectively (Table 2). As a reminder, negative absolute absenteeism values represent someone working more than is expected of him or her over a month-long period.
In the sample of patients undergoing ORIF for DRF, absolute presenteeism went from 79 (SD: 23) to 82 (SD: 17) to 79 (SD: 12) at preoperative, 3 months postoperative, and 6 months postoperative time points, respectively (Table 2). Across the same sample, absolute absenteeism went from 29 hours (SD: 41 hours) to 12 hours (SD: 72 hours) to 22 hours (SD: 57 hours) at preoperative, 3 months postoperative, and 6 months postoperative time points, respectively (Table 2).
Among patients undergoing a CTR, an average of 14.4% of monthly employee value was lost before surgery (Fig. 1A). Patients actually worked 9.2% more than their employers expected (ie, the opposite effect of absenteeism), adding monthly employee value (Fig. 1). However, 21.6% of employee value was then lost to presenteeism (Fig. 1). At 6 months after surgery, an average of 30.2% of monthly employee value was gained (Fig. 1). Patients worked 51.8% more than their employees expected; however, 14.2% of the employee value was then lost to presenteeism (Fig. 1).
Figure 1.
An illustration of the average monthly employee value of patients with carpal tunnel syndrome before and 6 months after carpal tunnel release. This is shown in percentage terms. The dashed lines represent employee value above 100% earned by working more hours than expected by employers.
Among patients undergoing an ORIF for DRF, before surgery, 47.3% of monthly employee value was lost (Fig. 2). Overall, 18.3% was attributable to absenteeism, and 29.0% was attributable to presenteeism. At 6 months after surgery, 43.1% of monthly employee value was lost (Fig. 2). Overall, 15.1% was attributable to absenteeism, and 28.0% was attributable to presenteeism.
Figure 2.
An illustration of the average monthly employee value of patients with distal radius fractures before and 6 months after open reduction and internal fixation. This is shown in percentage terms.
Discussion
Across hand and UE surgery, CTR for CTS and ORIF for DRFs are two of the most common pathologies and related interventions.12,13 Although prior research has examined return-to-work timeframes in these patient populations,4,5 there is a paucity of literature examining the economic impact of being present at work but working below optimal performance; this concept is known as presenteeism. This study sought to begin to fill this gap in the literature by considering both absenteeism and presenteeism and calculating employee value. Our work found that all patients appreciated clinically appreciable functional and pain symptom improvement by 6 months after surgery, as measured by a change in PROMs score greater than documented MCID values. The lack of clear mental health improvement may be because of factors outside the specific injuries and surgical interventions performed. However, although patients with CTS undergoing CTR, on average, return to above 100% employee monthly value by 6 months after surgery, patients with a DRF undergoing ORIF, on average, still cost employers 40% of their monthly employee value at 6 months after surgery. Our findings refute our hypothesis regarding patients with CTS undergoing CTR but confirm our hypothesis regarding patients with a DRF undergoing ORIF. These findings can help in preoperative expectation-setting discussions between care teams and patients.
In our study, we found that patients undergoing CTR actually worked longer hours than their employers expected at both presentation and 6 months after surgery; however, at the preoperative time point, patients provided less than 100% employee value because of the negative impact of presenteeism, whereas at 6 months after surgery, the loss of employee value from presenteeism was easily offset by the long hours patients worked. Thus, although patients were not performing at full capacity during the hours they worked at 6 months after surgery, the longer hours above what was expected offset the negative impact of presenteeism from an employee value perspective.
Furthermore, CTS symptoms had clinically improved by 6 months after surgery, which explains our average monthly employee value findings. Initial symptoms of CTS are often nocturnal paresthesias that may worsen to daytime paresthesias and weakness if left untreated. However, we suspect such symptoms rarely would be so severe to force absence from work but may decrease the ability to work at full capacity. Prior research found that baseline work role functioning, improved self-efficacy, and a supportive organization predicted successful work role functioning 6 months following CTR.11 Although our study did not consider these two factors, future work should seek to assess how much employee value each of these characteristics adds.
Among patients with a DRF undergoing an ORIF, we found that despite clinically appreciable improvement in symptoms by 6 months after surgery, substantial employee value (greater than 40%) remained lost. However, there was a 4% improvement in employee value created, on average, between the preoperative and 6-month postoperative time points. Contrary to patients undergoing CTR, this lost employee value was driven by both absenteeism and presenteeism. We suggest that patients with a DRF lose the ability to use one of their hands normally after surgery and postoperative recovery can be painful and impacted by stiffness and weakness for many months. Typically, it may take up to 1 year for full expected postoperative recovery from a DRF requiring an ORIF. These issues may cause patients to miss work and certainly work below their optimal performance. It is interesting to note that despite the employee value improvement at 6 months after surgery compared with the preoperative time point, the results at 6 months were slightly worse than those at 3 months after surgery. We suspect this may be because of patients adapting to their injury and postoperative recovery trajectories but then becoming frustrated as they recognize full recovery may take up to 1 year; however, future research is needed to confirm this hypothesis.
Two previous studies in hand surgery have examined presenteeism and absenteeism and their impact on employee value as it relates to total joint arthroplasty20 and single-level lumbar spine surgery.27 In both studies, patients did not return to full employee value by 1 year after surgery; however, improvements were noted. The difference in these findings and the current study is likely driven by differences in symptoms for CTS (eg, paresthesias are typically more impactful at night and rarely severe enough in day-to-day activities to cause absence from work) and the traumatic nature of sustaining a DRF and its subsequent healing process.
This study has several limitations. First, our study included patients from a single, urban academic hand and UE clinic, which may limit the generalizability of our findings to other settings. Second, recall bias may impact how patients completed the WHO-HPQ, especially related to estimating the total amount of hours worked over a timeframe and performance. Nonetheless, the WHO-HPQ has been shown to be validated, responsive, and sensitive.18,19 Thus, we believe it is an appropriate tool to measure absenteeism and presenteeism. Third, we did not account for a job type in our study (eg, laborer versus primarily computer-based work). Because we use our hands in many day-to-day activities, we did not believe that this was critical to our study; however, we do acknowledge that future work may seek to better understand the impact of presenteeism and absenteeism on employee value within certain employment fields. Fourth, our sample size precluded additional statistical analyses. Fifth, we did not take into account the severity of either condition; however, given our relatively limited sample size, we do not believe additional analyses to this granular of a level would have been able to be appropriately completed. Future research should assess severity of presenteeism and absenteeism over time after surgery. Sixth, our employee value impact may be overestimated, as patients who are doing well (both symptomatically and at work) may not have returned to the office or completed the questionnaires that were part of this study. Sixth, DRF is an acute injury that is often treated days to weeks after it is sustained, whereas CTS is a slow, progressive pathology that occurs over a much longer timeframe. Although one may assume that employees work at full capacity prior to any acute injury like a DRF, this is not necessarily the case. Furthermore, our work still allows readers to assess changes in employee value over time as they recover from undergoing an ORIF for a DRF, which is critical for expectation setting. Overall, we believe that this study provides a preliminary understanding of the employee value gained or lost to employers when their employees have two common hand and UE conditions that require surgical intervention.
In conclusion, this study examined the relationship between appreciable clinical improvement in symptoms and the average monthly employee value lost before surgery compared with 6 months after surgery in patients with CTS undergoing CTR or DRF undergoing an ORIF. We found patients undergoing surgery for CTS or DRF have clinically appreciable improvement in functional and pain symptoms by 6 months after surgery. However, by 6 months after surgery, CTR results in greater than complete employee value recovery, but approximately 40% of the employee value remains lost after surgery for DRF. These insights can help improve preoperative expectation-setting discussions between the care team and patient, as well as alert employers and policymakers to the employee-level impact of patients with these common hand and UE conditions undergoing surgical intervention.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
Acknowledgments
This study was conducted as part of a grant from the American Foundation for Surgery of the Hand (AFSH) [2021 Resident/Fellow Fast Track Grant; Award 3761]. The authors are grateful for the financial support.
References
- 1.Musculoskeletal Health. World Health Organization (WHO); 2022. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions [Google Scholar]
- 2.The Impact of Musculoskeletal Disorders on Americans—Opportunities for Action. Bone and Joint Initiative USA. 2016 https://www.boneandjointburden.org/docs/BMUS%20Executive%20Summary%202016%20%282%29.pdf [Google Scholar]
- 3.de Putter C.E., Selles R.W., Polinder S., Panneman M.J., Hovius S.E., van Beeck E.F. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94(9):e56. doi: 10.2106/JBJS.K.00561. [DOI] [PubMed] [Google Scholar]
- 4.Ratzon N., Schejter-Margalit T., Froom P. Time to return to work and surgeons' recommendations after carpal tunnel release. Occup Med (Lond) 2006;56(1):46–50. doi: 10.1093/occmed/kqi194. [DOI] [PubMed] [Google Scholar]
- 5.MacDermid J.C., Roth J.H., McMurtry R. Predictors of time lost from work following a distal radius fracture. J Occup Rehabil. 2007;17(1):47–62. doi: 10.1007/s10926-007-9069-0. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein D.N., Gruber J.S., Merchan N., Garcia J., Harper C.M., Rozental T.D. What factors are associated with increased financial burden and high financial worry for patients undergoing common hand procedures? Clin Orthop Relat Res. 2021;479(6):1227–1234. doi: 10.1097/CORR.0000000000001616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang W., Gignac M.A.M., Beaton D., Tang K., Anis A.H., Canadian Arthritis Network Work Productivity Group Productivity loss due to presenteeism among patients with arthritis: estimates from 4 instruments. J Rheumatol. 2010;37(9):1805–1814. doi: 10.3899/jrheum.100123. [DOI] [PubMed] [Google Scholar]
- 8.Stewart W.F., Ricci J.A., Chee E., Morganstein D., Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 9.Gignac M.A.M., Cao X., Tang K., Beaton D.E. Examination of arthritis-related work place activity limitations and intermittent disability over four-and-a-half years and its relationship to job modifications and outcomes. Arthritis Care Res (Hoboken) 2011;63(7):953–962. doi: 10.1002/acr.20456. [DOI] [PubMed] [Google Scholar]
- 10.Marks M., Vliet Vlieland T.P., Audigé L., Herren D.B., Nelissen R.G., van den Hout W.B. Healthcare costs and loss of productivity in patients with trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol. 2015;40(9):927–934. doi: 10.1177/1753193414568293. [DOI] [PubMed] [Google Scholar]
- 11.Amick B.C., III, Habeck R.V., Ossmann J., Fossel A.H., Keller R., Katz J.N. Predictors of successful work role functioning after carpal tunnel release surgery. J Occup Environ Med. 2004;46(5):490–500. doi: 10.1097/01.jom.0000126029.07223.a0. [DOI] [PubMed] [Google Scholar]
- 12.Currie K.B., Tadisina K.K., Mackinnon S.E. Common hand conditions: a review. JAMA. 2022;327(24):2434–2445. doi: 10.1001/jama.2022.8481. [DOI] [PubMed] [Google Scholar]
- 13.Corsino C.B., Reeves R.A., Sieg R.N. StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Russell Reeves declares no relevant financial relationships with ineligible companies. StatPearls Publishing; 2024. Distal radius fractures. [PubMed] [Google Scholar]
- 14.Beaton D.E., Wright J.G., Katz J.N., Upper Extremity Collaborative Group Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 15.Brodke D.J., Saltzman C.L., Brodke D.S. PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg. 2016;24(11):744–749. doi: 10.5435/JAAOS-D-15-00404. [DOI] [PubMed] [Google Scholar]
- 16.Hammert W.C., Calfee R.P. Understanding PROMIS. J Hand Surg Am. 2020;45(7):650–654. doi: 10.1016/j.jhsa.2020.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Cella D., Riley W., Stone A., et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kessler R.C., Barber C., Beck A., et al. The World Health Organization health and work performance questionnaire (HPQ) J Occup Environ Med. 2003;45(2):156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- 19.Wang P.S., Beck A., Berglund P., et al. Chronic medical conditions and work performance in the health and work performance questionnaire calibration surveys. J Occup Environ Med. 2003;45(12):1303–1311. doi: 10.1097/01.jom.0000100200.90573.df. [DOI] [PubMed] [Google Scholar]
- 20.Fontana M.A., Islam W., Richardson M.A., Medina C.K., McLawhorn A.S., MacLean C.H. Presenteeism and absenteeism before and after total hip and knee arthroplasty. J Arthroplasty. 2021;36(5):1511–1519.e5. doi: 10.1016/j.arth.2020.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler R., Petukhova M., McInnes K., Üstün T.B. Re: content and scoring rules for the HPQ absenteeism and presenteeism questions. 2007. https://www.hcp.med.harvard.edu/hpq/ftpdir/absenteeism%20presenteeism%20scoring%20050107.pdf
- 22.Sorensen A.A., Howard D., Tan W.H., Ketchersid J., Calfee R.P. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641–649. doi: 10.1016/j.jhsa.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kazmers N.H., Hung M., Bounsanga J., Voss M.W., Howenstein A., Tyser A.R. Minimal clinically important difference after carpal tunnel release using the PROMIS platform. J Hand Surg Am. 2019;44(11):947–953.e1. doi: 10.1016/j.jhsa.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernstein D.N., Houck J.R., Mahmood B., Hammert W.C. Minimal clinically important differences for PROMIS physical function, upper extremity, and pain interference in carpal tunnel release using region- and condition-specific PROM tools. J Hand Surg Am. 2019;44(8):635–640. doi: 10.1016/j.jhsa.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Hollenberg A.M., Hammert W.C. Minimal clinically important difference for PROMIS physical function and pain interference in patients following surgical treatment of distal radius fracture. J Hand Surg Am. 2022;47(2):137–144. doi: 10.1016/j.jhsa.2021.08.025. [DOI] [PubMed] [Google Scholar]
- 26.Norman G.R., Sloan J.A., Wyrwich K.W. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 27.Fontana M.A., Islam W., Richardson M.A., et al. Presenteeism and absenteeism before and after single-level lumbar spine surgery. Spine J. 2022;22(5):776–786. doi: 10.1016/j.spinee.2021.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]