Abstract
Purpose
The purpose of this study was to evaluate the biomechanical properties of SutureTape as an alternative technique for arthrodesis of the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joint arthrodesis when compared with surgical steel wire.
Methods
A total of 32 fingers (index, long, ring, and small) from two matched pair cadaveric hands were used. K-wire and surgical steel wire were used for MCP and PIP joint arthrodesis of the control group (group I), whereas K-wire and SutureTape were used for the experimental group (group II). Each sample was potted in high strength resin and secured to a custom fixture mounted to a hydraulic test frame. Each sample underwent cantilever bending in four directions (flexion, extension, ulnar, and radial) at a rate of 0.01 mm/s until a maximum force of 10 N. Thereafter, ramp to failure in extension at a rate of 20 mm/min was performed. Metrics of interest were bending stiffness (N/mm), displacement (mm), and peak load to failure (N), along with failure modes.
Results
For MCP arthrodesis, during cantilever bending in flexion direction, surgical steel construct was found to be stiffer when compared with suture tape (P = .036) and have less displacement (P = .040). No significant differences were detected for stiffness or displacement in extension, ulnar, or radial bending. During the ramp to failure, no significant differences were found for force, stiffness, or displacement. For PIP arthrodesis, the only significant difference detected was for displacement during ulnar bending (P = .035).
Conclusions
For MCP and PIP arthrodesis, the biomechanical performance of the SutureTape arthrodesis was similar to that of the steel wire across all loading conditions except for flexion and ulnar loading.
Clinical relevance
The use of SutureTape for MCP and PIP joint arthrodesis may provide equivalent biomechanical performance to that of steel wire, making it a viable alternative clinically.
Key words: Arthrodesis stability, Biomechanics, Fusion, MCP joint, PIP joint
Osteoarthritis of the hand is a debilitating and common source of hand pain that has been reported to affect up to 67% of women and 55% of men by the age of 55.1 Patients may experience symptoms such as pain, swelling, and loss of motion—all of which can impact quality of life and ability to effectively contribute to the workforce. Nonsurgical treatments include anti-inflammatory medications, both oral and topical, immobilization, and corticosteroids.2,3 Surgical treatments most commonly include arthroplasty and arthrodesis.4
Various surgical techniques for small joint arthrodesis have been reported, including interosseous wiring, K-wire constructs, tension banding, plating, and compression screws.5, 6, 7, 8 Each technique features its own challenges, advantages, and disadvantages. The tension band construct with K-wire and surgical steel wire has been well described but is associated with drawbacks such as skin irritation, pain, and possible seroma formation with subsequent need for implant removal.5,9 Some authors have suggested that these complications are caused by the rigidity and prominence of the implanted hardware.5,10,11 Although advances in tension band techniques have lowered skin irritation and pain compared with the traditional AO method, approximately 30% of patients require a second surgical procedure to address the pain and irritation caused by the implanted hardware.12,13
Some authors have suggested that ultrahigh molecular weight polyethylene suture could be an alternative option, as there would theoretically be minimal risk of symptomatic hardware.12,13 However, it is natural to question if suture would provide similar biomechanical strength as surgical steel. A recent animal study, which analyzed canine olecranon fractures, compared two different tension band techniques, metal wire and ultrahigh molecular weight polyethylene suture, and concluded that the biomechanical stability of these two constructs was similar.14
The purpose of this study was to evaluate the biomechanical performance of two different arthrodesis configurations for metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joint fusion in a matched pair cadaveric model. It was hypothesized that the use of K-wire with SutureTape (Arthrex) technique may offer equivalent biomechanical results when compared with K-wire and surgical steel wire.
Methods
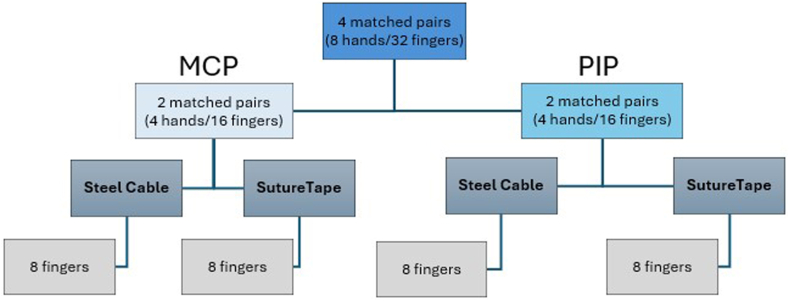
Dissection and instrumentation
A total of four matched pair cadaveric hands (one man and three women; age range: 58–79 years) were procured and randomized into the testing groups, where two sets of hands were used to harvest the PIP joint, and the remaining two sets were used to harvest the MCP joint. All hands were assessed by fluoroscopic radiography to ensure no prior pathology or bony abnormalities were present. Bone mineralization tests were not performed. During dissection, a dorsal incision over the MCP joint and PIP joint for each respective study group was made through the skin, and the extensor tendon was split longitudinally. The joint capsule was also split longitudinally and elevated, and the collateral ligaments were released. The soft tissue was removed except the volar plate for all samples. For the first set of matched pairs, the fingers from each specimen were disarticulated at the carpometacarpal joint and PIP joint to harvest the MCP joint. For the other set of matched pairs, the fingers from each specimen were disarticulated at the MCP joint to harvest the PIP joints. A total of 32 fingers (index, middle, ring, and little) were harvested and divided into two treatment groups where group I (GI) underwent the K-wire and surgical steel as treatment with 22-gauge steel, which served as the control, and the contralateral side was group II (GII), which were treated with K-wire and Arthrex SutureTape (Fig. 1). We did not perform osteotomy in either group as we would clinically because this could have created too much variability in quality of cut cadaver bone.
Figure 1.
Testing group.
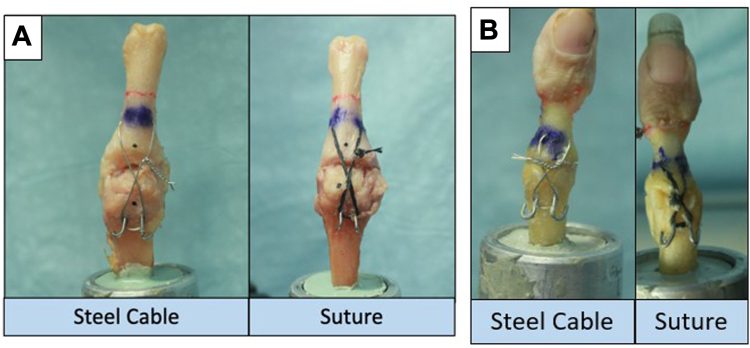
For both groups, two antegrade 0.045 (1.1 mm) K-wires were placed longitudinally from the metacarpal and proximal phalanx head/neck into the proximal phalanx and middle phalanx shaft into subchondral bone distally under fluoroscopic guidance for proper placement. A 1.6 mm K-wire was used to drill a transverse hole in the distal bone, distal to the fusion site in the volar phalanx diaphysis for later passing of wire or SutureTape. For GI (surgical steel group), a 22-gauge wire was passed through the transverse hole of the distal bone and wrapped in a figure-of-eight fashion around proximal K-wires. This size wire is standard at our institution. It is helpful to flatten the curve of the needle for easier passage through the transverse drill holes. The wire was twisted carefully using needle driver for a total of six turns, and this created compression at arthrodesis site. Excess wire was cut and laid flat onto the bone. In a similar fashion, GII (SutureTape group), a 1.3-mm SutureTape was passed through the transverse hole of the distal bone and tightened to create compression at the arthrodesis site and then tied with a surgeon’s knot and three half-hitch ties and laid between the proximal two K-wires. For both groups, the transarticular K-wires were then cut short, bent toward the proximal bony cortex, and tamped antegrade into subchondral bone to avoid excess prominence (Fig. 2A, B). The MCP joints were positioned at 30° of palmar flexion, and the PIP joints were positioned at 45° of palmar flexion.
Figure 2.
Examples of A the metacarpophalangeal and B proximal interphalangeal joint cadaveric subjects with steel (group I) and suture tape (group II) arthrodesis fixation.
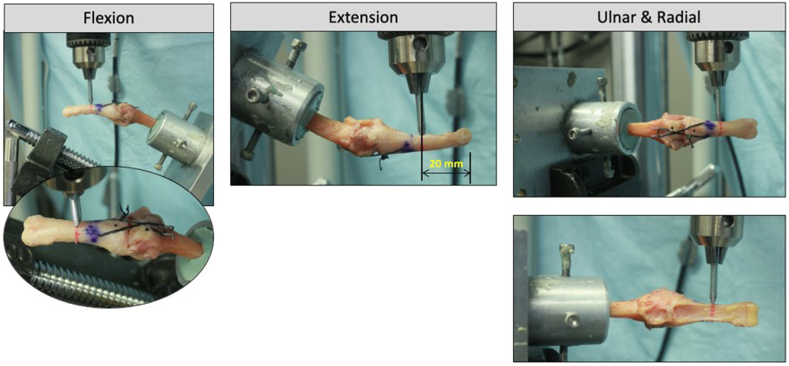
Biomechanical testing
Each sample was potted in high strength resin, such that two-thirds of the distal end was embedded. The potted ends were then secured to a custom fixture mounted to the hydraulic test frame (MTS Bionix; MTS Systems). Each sample underwent cantilever bending in four directions (flexion, extension, ulnar, and radial) at a rate of 0.01 mm/s until a maximum force of 10 N.5,12,15 The load applicator was positioned 20 mm from the joint line, generating a bending moment of 0.2 Nm (Fig. 3). Thereafter, all specimens were loaded in extension at a rate of 20 mm/min until failure. Failure was defined as the first significant decrease in force response. Metrics of interest were collected from test frame data aquisition system, and a load–displacement curve generated was used to calculate bending stiffness (N/mm), displacements (mm), and peak load to failure (N). Additionally, failure modes for each sample were noted.
Figure 3.
For each condition, loading was applied in displacement control at a rate of 0.01 mm/s until 10 N was reached. The distance of load (red line) was 20 mm from the joint, generating a 0.2 Nm bending moment across the MCP joint.
Based on data from literature, an a priori test was used with an effect size (Cohen’s d) of 1.4 to compute the required sample size to detect a difference between the matched paired groups (G∗Power).5,15 Assuming a power of 0.8 and a type I error rate of 0.05, a sample size of 7 per group powers the study to 0.86. The choice of eight samples per group powers the study to 0.92, allowing for any possible tissue rejection or unforeseen failures while retaining proper study power. Commercially available software was used for all comparisons (SPSS) at a significance threshold of 0.05. Mann-Whitney U test was used to compare the stiffness, displacement, and ultimate failure force between the matched pairs. Data are presented as mean ± SD. Research was performed at the Phillip Spiegel Orthopaedic Research Laboratory at the Foundation for Orthopaedic Research and Education, Tampa, FL, 33607.
Results
MCP joint
For MCP arthrodesis evaluation, during cantilever bending in flexion direction, GI construct was found to be stiffer when compared with GII (GI: 11.3 ± 4.0 N/mm vs GII: 7.3 ± 2.6 N/mm; P = .036) and have less displacement (GI: 1.1 ± 0.4 mm vs GII: 1.6 ± 0.4 mm; P = .040). In extension direction, no significant differences were detected for stiffness (P = .294) between GI (4.5 ± 1.6 N/mm) and GII (3.6 ± 1.4 N/mm) or for displacement (P = .208) between GI (2.6 ± 0.8 mm) and GII (3.2 ± 0.8 mm). Similarly, no significant differences were detected in stiffness (GI: 6.4 ± 2.7 N/mm vs GII: 4.9 ± 1.3 N/mm; P = .562) or displacement (GI: 1.8 ± 0.6 mm vs GII: 2.4 ± 0.9 mm; P = .226) during ulnar bending. In the radial direction, no significant differences were detected in stiffness (GI: 6.4 ± 3.0 N/mm vs GII: 4.4 ± 1.2 N/mm; P = .114) or displacement (GI: 2.0 ± 0.8 mm vs GII: 2.6 ± 0.8 mm; P = .084). During the ramp to failure, no significant differences were found for force (GI: 38.3 ± 8.5 N vs GII: 35.4 ± 9.6 N; P = .429), stiffness (GI: 4.0 ± 0.9 N/mm vs GII: 3.2 ± 1.3 N/mm; P = .084), or displacement (GI: 17.4 ± 2.2 mm vs GII: 16.5 ± 0.9 mm; P = .749).
PIP joint
For PIP arthrodesis evaluation, during cantilever bending in flexion direction, no significant differences were detected in stiffness (GI: 7.6 ± 2.4 N/mm vs GII: 6.6 ± 1.5 N/mm, P = .645) or displacement (GI: 1.7 ± 0.5 mm vs GII: 1.9 ± 0.4 mm, P = .521). Similarly, no significant differences were detected in stiffness (GI: 5.2 ± 3.2 N/mm vs GII: 4.8 ± 2.0 N/mm, P = .999) or displacement (GI: 2.8 ± 1.1 mm vs GII: 2.9 ± 1.0 mm, P = .710) during extension bending. For ulnar loading, no significant differences were found for stiffness (GI: 6.4 ± 2.6 N/mm vs GII: 5.3 ± 1.7 N/mm, P = .328); however, the displacement required to reach 10 N was greater in the suture construct compared with the steel construct (GI: 2.1 ± 0.8 mm vs GII: 3.0 ± 0.6 mm, P = .035). No significant differences were found for stiffness (GI: 5.5 ± 1.9 N/mm vs GII: 5.4 ± 2.7 N/mm, P = .674) or displacement (GI: 2.1 ± 0.5 mm vs 2.4 ± 0.6 mm, P = .292) between the steel and suture construct during radial loading. Finally, no significant differences were found for force (GI: 44.0 ± 14 N vs GII: 37.0 ± 11 N, P = .636), stiffness (GI: 5.4 ± 3.4 N/mm vs 5.0 ± 1.9 N/mm, P = .916), or displacement (GI: 12.5 ± 2.5 mm vs 11.4 ± 3.1 mm, P = .246) during ramp to failure.
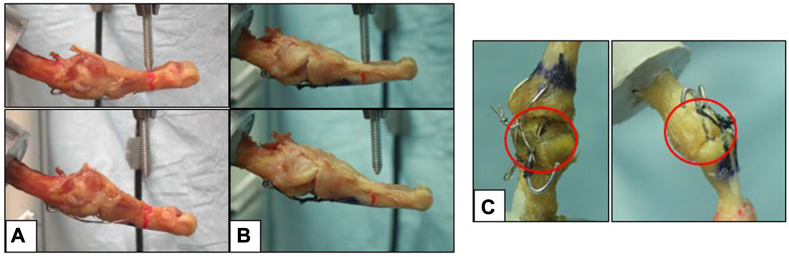
Failure modes
The main failure mode was characterized as plastic deformation, as there was a loss in arthrodesis angulation. After each test, the specimens were examined to further characterize failure mode. For the MCP joints, it was observed that all samples had permanently deformed K-wires, and both the steel and SutureTape were lax compared with the initial taut state. No implant cutout of the bone was observed.
For the PIP joints, it was observed that all samples had failed by bony cutout and had some degree of K-wire bend. The bony cutout can be further described as both K-wires pulling out through the distal end of the phalanx (Fig. 4).
Figure 4.
Illustration of failure modes observed were K-wire deformation in A MCP joints for steel and B MCP joints for suture tape, whereas C both steel and suture tape experience bony cutout.
Discussion
The primary objective of this study was to evaluate the biomechanical strength of two different types of tension band constructs used in MCP and PIP arthrodesis: surgical steel and SutureTape. The findings confirm our hypothesis that the use of SutureTape as a technique offers comparable biomechanical results when compared with surgical steel, as the SutureTape arthrodesis performed similarly across all loading conditions for MCP and PIP arthrodesis other than flexion stiffness and displacement for MCP arthrodesis and ulnar loading for PIP arthrodesis.
Successful arthrodesis of the MCP and PIP joints is dependent on adequate stiffness and stability of a construct. Although the threshold for ideal stiffness for fusion has not been established by prior literature, there is a general notion that increased stiffness is optimal for increasing compression and subsequent union of a fused joint.5,15,16 Several previous studies have investigated MCP and PIP arthrodesis constructs to compare different constructs and their biomechanical properties and have found mixed results. Capo et al5 compared five different types of constructs, oblique K-wire with coronal intraosseous wiring, tension-band-wire, dorsal plate, intramedullary linked screws, and 90/90 wiring, and found intramedullary screws to have the greatest strength in terms of load to failure. Although this notion has been supported by other biomechanical studies, studies have found compression screws to be associated with higher rates of complication, including fracture.12,13,17 An alternative option is the tension band construct, which offers a comparable rate of union, time to fusion, and multidirectional strength with fewer reported complications.11,13,16, 17, 18
The tension band technique offers a reasonable construct to stabilize the arthrodesis while allowing early hand motion. Tension banding across the dorsal aspect of the joint creates compression at the arthrodesis site throughout active motion, which allows for accelerated union. Moreover, the construct uses widely available and affordable materials, such as pins, wires, and durable sutures.10 Tension band construct with suture fixation is a relatively new technique that is growing in popularity compared with traditional methods.14,19,20 Although there remains a paucity of literature investigating the efficacy of sutures in MCP and PIP arthrodesis, several studies have compared sutures with traditional methods of tension banding.14,19,20, Phadnis et al14 compared sutures with wires in the setting of simple olecranon fractures and found sutures to be associated with similar rates of stable union with significantly lower reoperation rate. Similarly, Camarda et al20 used durable sutures to treat transverse patella fractures and found this technique to be associated with satisfactory patient-reported outcomes and low incidences of complications and revision surgery.
Our study is the first to compare the biomechanical strength of surgical steel and SutureTape for arthrodesis of MCP and PIP joints. We found that these two constructs have largely comparable stiffness, displacement, and load to failure. One of the only exceptions was that the steel MCP arthrodesis construct had significantly greater stiffness and less displacement in flexion. However, this was not observed for PIP arthrodesis construct.
Although standard tension band techniques with K-wires and surgical steel have shown reliable arthrodesis, clinically, this method can be irritating to patients. Often, the surgical steel and sometimes the K-wires themselves cause irritation and require removal. Use of suture would likely be less irritating and possibly not require a subsequent procedure. Clinical studies would be required to assess this.
Although these biomechanical results are promising, the study is not without limitations.
One inherent limitation to cadaveric biomechanical studies is that these models do not address important clinical factors such as subcutaneous implant irritation, rates of healing and fusion, or effects of surrounding soft tissue on stabilization.18 A controlled clinical study would be required to address these concerns and establish a basis for functional outcomes and patient success. Another limitation is the amount of tension applied to both groups was not measured and based on the haptic feedback of the surgeon which is subjective. To mitigate possible variance due to tightening, the numbers of wire twists and suture knots were both standardized, and one surgeon performed the instrumentation. Moreover, only two different types of tension band constructs were compared and did not contrast these types of fixations with other commonly used methods for MCP and PIP arthrodesis. Another limitation could be related to specimen (finger) size relative to the K-wire diameter and bone tunnel drilling. As the same diameter K-wire was used for both MCP and PIP, the effect of K-wire is likely contributing to different amounts of stabilization relative to bone size. This may be an explanation as to why a difference in stiffness was detected between the steel and SutureTape only for MCP in flexion and not for PIP. Possible explanations for this outcome may be further understood by the failure modes observed, where for PIP joint, samples failed by bony cutout. Similar failure modes were observed by Kovach et al.18 In the MCP joint samples, both the steel and SutureTape were lax in addition to the K-wires being bent. Although not measured, this laxity may be attributed to knot slipping or unwinding of twisted steel. Our loading protocol was based on previous work; however, the constructs were only tested in cantilever bending, and no rotational moments were tested or cyclical loading. Thumbs were not included due to the cost of multiple cadavers to create adequate group size. Finally, our cadavers were presumably healthy individuals without MCP or PIP osteoarthritis. This brings into question of whether these results would be applicable to a population with pre-existing pathology. Despite these limitations, the study provides a framework for future research as researchers continue to evaluate the clinical efficacy of suture tape tension band construct as a means of fixation for MCP and PIP arthrodesis.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
Acknowledgments
The authors thank Dillon Bates (Coastal Medical Technologies) for providing suture material.
References
- 1.Wan J., Qian X., He Z., Zhu Z., Cheng P., Chen A. Epidemiological trends of hand osteoarthritis from 1990 to 2019: estimates from the 2019 Global Burden of Disease study. Front Med (Lausanne) 2022;9 doi: 10.3389/fmed.2022.922321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valdes K., Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther. 2010;23(4):334–350. doi: 10.1016/j.jht.2010.05.001. quiz 351. [DOI] [PubMed] [Google Scholar]
- 3.Haugen I.K. Hand osteoarthritis: current knowledge and new ideas. Scand J Rheumatol. 2016;45(sup128):58–63. doi: 10.1080/03009742.2016.1203021. [DOI] [PubMed] [Google Scholar]
- 4.Earp B., Cefalu C., Blazar P. Thumb metacarpophalangeal joint arthritis. J Am Acad Orthop Surg. 2019;27(23):e1029–e1039. doi: 10.5435/JAAOS-D-18-00683. [DOI] [PubMed] [Google Scholar]
- 5.Capo J.T., Melamed E., Shamian B., et al. Biomechanical evaluation of 5 fixation devices for proximal interphalangeal joint arthrodesis. J Hand Surg Am. 2014;39(10):1971–1977. doi: 10.1016/j.jhsa.2014.07.035. [DOI] [PubMed] [Google Scholar]
- 6.Nomura Y., Ishikawa H., Abe A., et al. Arthrodesis of the digital joint using intraosseous wiring in patients with rheumatoid arthritis. Mod Rheumatol. 2021;31(1):114–118. doi: 10.1080/14397595.2020.1726607. [DOI] [PubMed] [Google Scholar]
- 7.Brutus J.P., Palmer A.K., Mosher J.F., Harley B.J., Loftus J.B. Use of a headless compressive screw for distal interphalangeal joint arthrodesis in digits: clinical outcome and review of complications. J Hand Surg Am. 2006;31(1):85–89. doi: 10.1016/j.jhsa.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki T., Kawamura D., Matsui Y., Iwasaki N. Arthrodesis of the interphalangeal joints of the hand by two-dimensional intraosseous wiring. BMC Musculoskelet Disord. 2023;24(1):843. doi: 10.1186/s12891-023-06972-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kadic L.I.M., Rademacher N., Liu C.C., Leise B.S., McCauley C.T., Riggs L.M. The influence of a tension band fixation as an adjunct for arthrodesis of the metacarpophalangeal joint in the horse. Vet Surg. 2024;53(1):194–203. doi: 10.1111/vsu.14036. [DOI] [PubMed] [Google Scholar]
- 10.Uhl R.L. Proximal interphalangeal joint arthrodesis using the tension band technique. J Hand Surg Am. 2007;32(6):914–917. doi: 10.1016/j.jhsa.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Breyer J.M., Vergara P., Parra L., Sotelo P., Bifani A., Andrade F. Metacarpophalangeal and interphalangeal joint arthrodesis: a comparative study between tension band and compression screw fixation. J Hand Surg Eur Vol. 2015;40(4):374–378. doi: 10.1177/1753193413514362. [DOI] [PubMed] [Google Scholar]
- 12.Dickson D.R., Mehta S.S., Nuttall D., Ng C.Y. A systematic review of distal interphalangeal joint arthrodesis. J Hand Microsurg. 2014;6(2):74–84. doi: 10.1007/s12593-014-0163-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faulkner H., An V., Lawson R.D., Graham D.J., Sivakumar B.S. Proximal interphalangeal joint arthrodesis techniques: a systematic review. Hand (N Y) 2023;18(1):74–79. doi: 10.1177/1558944721998019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phadnis J.S., Vaughan A., Luokkala T., Peters J., Watson J.J., Watts A. Comparison of all suture fixation with tension band wiring and plate fixation of the olecranon. Shoulder Elbow. 2020;12(6):414–421. doi: 10.1177/1758573219831662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alluri R.K., Hill J.R., Navo P., Ghiassi A., Stevanovic M., Mostofi A. Washer and post augmentation of 90/90 wiring for proximal interphalangeal joint arthrodesis: a biomechanical study. J Hand Surg Am. 2018;43(12):1137.e1–1137.e10. doi: 10.1016/j.jhsa.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Millrose M., Gesslein M., Ittermann T., Kim S., Vonderlind H.C., Ruettermann M. Arthrodesis of the proximal interphalangeal joint of the finger - a systematic review. EFORT Open Rev. 2022;7(1):49–58. doi: 10.1530/EOR-21-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wyrsch B., Dawson J., Aufranc S., Weikert D., Milek M. Distal interphalangeal joint arthrodesis comparing tension-band wire and Herbert screw: a biomechanical and dimensional analysis. J Hand Surg Am. 1996;21(3):438–443. doi: 10.1016/S0363-5023(96)80360-1. [DOI] [PubMed] [Google Scholar]
- 18.Kovach J.C., Werner F.W., Palmer A.K., Greenkey S., Murphy D.J. Biomechanical analysis of internal fixation techniques for proximal interphalangeal joint arthrodesis. J Hand Surg Am. 1986;11(4):562–566. doi: 10.1016/s0363-5023(86)80200-3. [DOI] [PubMed] [Google Scholar]
- 19.Hughes S.C.A., Stott P.M., Hearnden A.J., Ripley L.G. A new and effective tension-band braided polyester suture technique for transverse patellar fracture fixation. Injury. 2007;38(2):212–222. doi: 10.1016/j.injury.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Camarda L., La Gattuta A., Butera M., Siragusa F., D’Arienzo M. FiberWire tension band for patellar fractures. J Orthop Traumatol. 2016;17(1):75–80. doi: 10.1007/s10195-015-0359-6. [DOI] [PMC free article] [PubMed] [Google Scholar]