Abstract
This surgical technique article describes the anatomic C scapholunate reconstruction technique. It is indicated for complete acute or chronic scapholunate ligament dissociation. The technique addresses severe scapholunate interval gapping, ulnar translocation of the lunate, and rotational/dorsal intercalated segment instability. The C-shaped ligament is cradled from dorsal to volar using a symmetric four anchor/synthetic tape construct through a single dorsal incision and hyperflexion of the wrist. It does not require any volar incision/approach, as previously described techniques, and also avoids vascular disruption of the scaphoid ridge. An athlete patient case with illustration is also presented, who was treated with anatomic C scapholunate reconstruction on one wrist and all-dorsal scapholunate reconstruction on the other wrist. The two wrists are compared, and postoperative management with technique pearls and pitfalls are described.
Key words: Anatomic C, Carpal instability, Dorsal intercalated segment instability, Scapholunate tear, SL dissociation
When presented with the problem of an acute or chronic complete scapholunate dissociation, the concerns are 2-fold. The intrinsic ligament dissociation of the scapholunate (SL) interval leads to gapping and rotational instability.1 There are techniques that repair and address these issues from both volar and dorsal with two or more incisions, such as the Brunelli and its variations, SL 360, and anatomic front and back.2, 3, 4, 5 However, the additional dissection adds greater morbidity, complexity, and surgical time to the procedure. The median nerve is in direct harm and can be catastrophically injured if not protected properly. There is also the interosseous SL reconstruction technique that does not address the problem anatomically since the tunnels are intraosseous. Because of these issues, a new technique was warranted.
With the latest technologies in small anchor/synthetic tape implants, the possibility of placing them along any length/contour of the bony surface to augment and protect ligament healing is attainable. Hence, the thought process veered toward anatomically contouring the actual shape and thus function of the scapholunate ligament in the wrist.
Interestingly, there is a way to achieve a reconstruction for a complete SL tear spanning the C-shaped anatomy entirely from dorsal to volar, with a single dorsal incision and hyperflexion of the wrist (Fig. 1). The blood supply on the scaphoid ridge is not interrupted since the dissection does not need to extend distally.
Figure 1.
The anatomic C scapholunate reconstruction technique makes use of a single dorsal minimally invasive incision.
Indications and Contraindications
The anatomic C scapholunate reconstruction technique is indicated for complete acute or chronic reducible scapholunate ligament dissociation (Garcia-Elias Stage II–IV). It is contraindicated once articular cartilage is damaged/worn, irreducible with arthrosis, and scapholunate advanced collapse wrist is present (Garcia-Elias Stage V–VI).
Surgical Anatomy
The scapholunate ligament is anatomically C-shaped and comprised of three portions: dorsal, membranous, and volar.6 The dorsal portion is the thickest part of the ligament and has traditionally been the portion that is addressed in surgery. Furthermore, we must keep in mind the importance of the extrinsic secondary stabilizing ligaments such as the long radiolunate ligament, the dorsal intercarpal ligament, the dorsal radiocarpal ligament, and dorsocapsular scapholunate septum.7 During closure of the capsule, these secondary stabilizers are repaired back to the bone.
Surgical Technique
Typically, the procedure starts with dry arthroscopy to confirm the diagnosis, assess cartilage, and address any other injuries. However, one can start directly with the open approach to the wrist and assess the pathology through the dorsal incision.
An approximately 2-inch dorsal midline incision is made directly over the fourth extensor compartment. The extensor retinaculum is divided with release of the third compartment radial and fourth compartment ulnar. A ligament-sparing capsulotomy is performed as previously described by Berger et al,8 and the SL interval is identified.
K-wires (0.062” recommended) are placed in the scaphoid and lunate to act as joysticks to correct rotational deformity and maintain reduction. It is essential to place these wires distally on the scaphoid and more ulnar on the lunate to keep adequate space for reconstruction. The k-wires are clamped with a Kocher to hold throughout the procedure. An additional scapholunate pin can be placed away from the planned blind anchor sockets, if the Kocher does not adequately hold. These wires are all removed at the end of the surgery. After the deformity is corrected, a marking pen is used to plan the anchor placement.
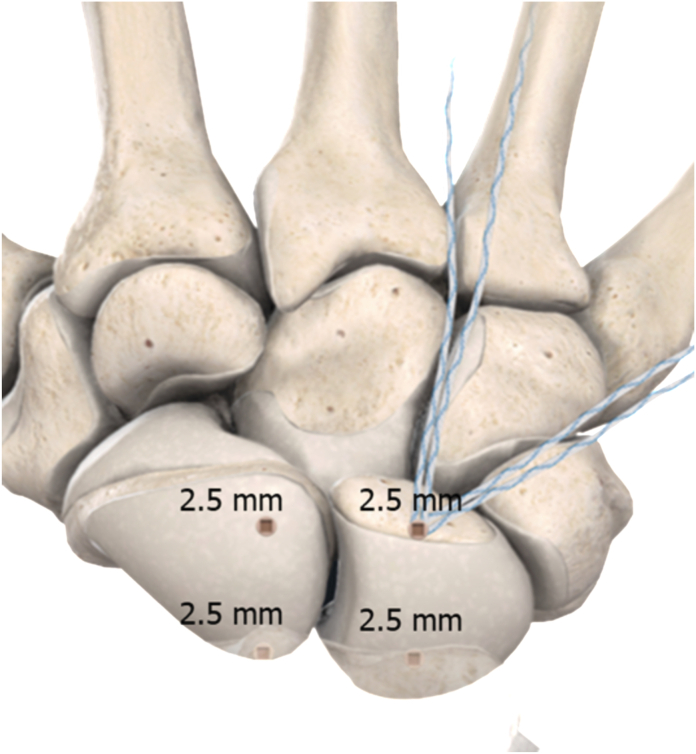
The anatomic C reconstruction technique requires four anchors and a tape construct. In this article, we use 2.5-mm Mini PushLock anchors (Arthrex Inc) with a 2-mm drill, and two 1.3-mm SutureTape (Arthrex Inc). This choice of anchor and consequent drill size is based on patient bone size and real estate present. Two anchors will sit in the scaphoid, and two anchors in the lunate.
Two blind anchor sockets are first drilled into the dorsal portion of the scaphoid and lunate, with no preference of order. These holes are drilled parallel to each other if the SL interval is reduced.
The remaining two blind anchor sockets are now made proximally. The wrist is fully hyperflexed, and the holes are placed on the articular surface of the scaphoid and lunate as volar as possible. This will create a symmetric rectangular configuration of the four anchor sockets. Hyperflexion works on all patients. The patient does not need to be hyperlax or have a connective tissue disorder to hyperflex the wrist. A freer elevator can be used to atraumatically shoehorn the bone to see further volar.
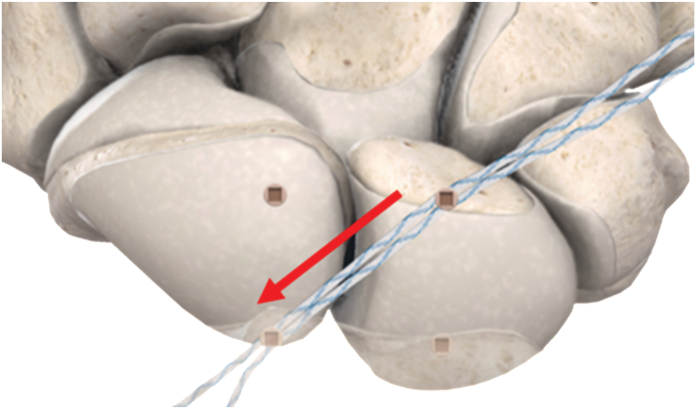
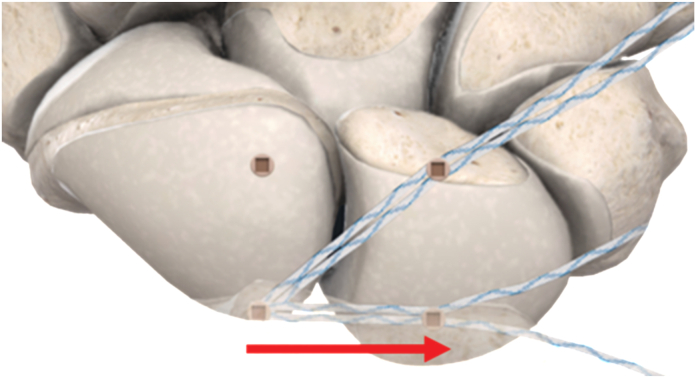
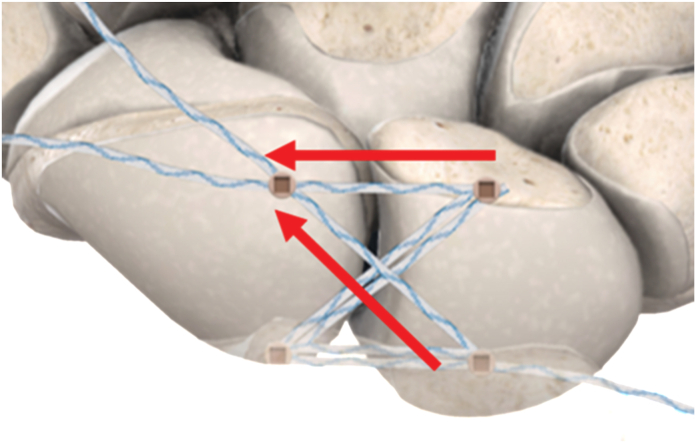
The drill holes are blind sockets that do not connect (Fig. 2) and are drilled with a 2.0-mm drill to a depth of 8 mm. The first anchor in the dorsal/distal lunate is loaded with two 1.3-mm SutureTape; hence, the tapes are doubled over (Fig. 3). Oftentimes, it is necessary to slightly stretch the anchor eyelet to get the sutures in the anchor. Two of the four limbs of tape are then taken to the volar/proximal scaphoid (Fig. 4). They are then brought to the lunate’s volar/proximal socket (Fig. 5). From this volar/proximal lunate socket, only one strand is used along with one strand from the first dorsal/distal lunate anchor socket, and these limbs are brought obliquely and dunked into the dorsal/distal scaphoid socket (Fig. 6).
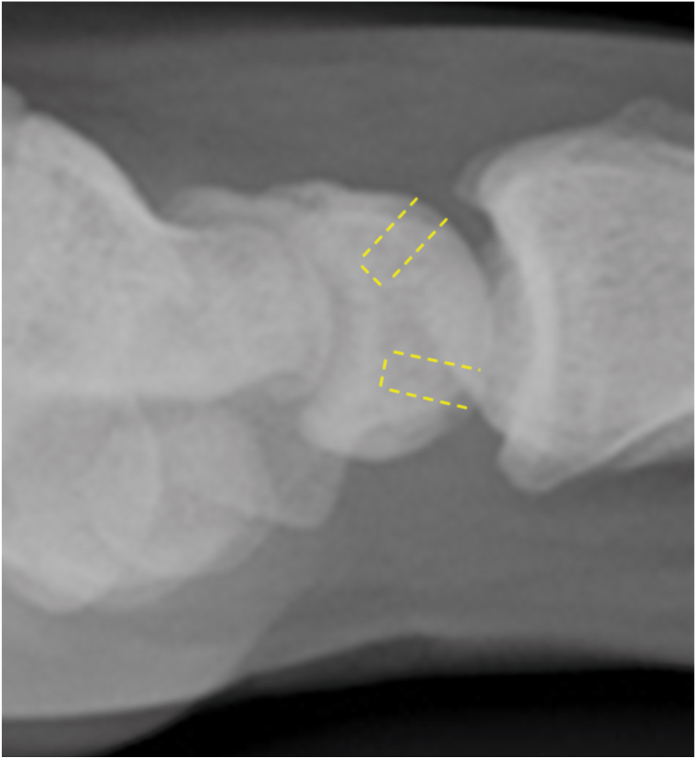
Figure 2.
Lateral radiographic view showing the drill holes are blind sockets that do not overlap.
Figure 3.
The first 2.5-mm anchor in the dorsal/ distal lunate is loaded with two 1.3 mm SutureTape. Hence, the tapes are doubled over.
Figure 4.
Two of the four limbs of tape are taken to the volar/proximal scaphoid with a 2.5-mm anchor.
Figure 5.
Two limbs of tape are brought to the lunate’s volar/ proximal socket with a 2.5-mm anchor.
Figure 6.
From the volar/proximal lunate socket, only one strand of the tape is used along with one strand from the first dorsal/distal lunate anchor socket, and these limbs are brought obliquely and dunked into the dorsal/distal scaphoid.
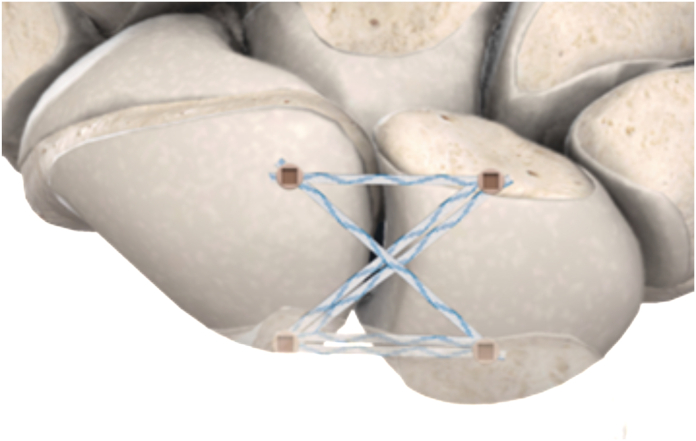
The final construct now has four separate passages of tape across the SL interval, cradling the bones and recreating the C-shaped anatomy of the ligament. There are two parallel limbs of tape formed dorsal and volar to maintain reduction of the gapping, and two crossing limbs of tape that maintain rotational stability (Fig. 7).
Figure 7.
The final construct has four separate passages of suture tape across the SL interval, cradling the bones and recreating the C-shaped anatomy of the ligament. Two parallel limbs of tape are formed dorsal and volar to maintain reduction of the gapping, and two crossing limbs of tape maintain rotational stability.
After all the anchors are placed, the secondary stabilizers are addressed. The remaining limbs of the 1.3-mm suture tape are used to repair the dorsocapsular scapholunate septum back to the dorsal carpus directly to bone with a free needle. The dorsal intercarpal ligament and dorsal radiocarpal ligament should be repaired from the initial capsulotomy.
It is important to note that the option is open for different size tapes and anchors, with or without graft, based on the varying size of the anatomy of the scaphoid and lunate and surgeon preference. The sizes of bony real estate should be under careful consideration intraoperatively, before choosing and committing to the proper size drills and anchor/tape constructs. In the experience of the authors, 2.5-mm anchors are ideal size even with a larger patient (Table 1).
Table 1.
Pearls of the Anatomic C Scapholunate Reconstruction Technique
| Pearls |
|---|
|
Postoperative Management
After surgery, patients return to the office at 10 days followed by hand therapy (HT). At the first visit, an orthosis is fabricated: bivalved, with the wrist in neutral; the patient then begins the range of motion of noninvolved joints. The patient is educated on precautions: no weight-bearing and use of the hand for light activity only with orthosis, observing a 1–2 pound (lb) lift limit. Scar was managed once the incision had healed.
At the 2- to 3-week visit, begin gentle short arc active flexion and extension of the wrist, focusing on a normal movement pattern. Assess digit motion and ensure full extension and flexion. If swelling is an issue and digits do not fully extend, intrinsic strengthening is initiated with memory foam sponges for metacarpophalangeal adduction and rubber band for metacarpophalangeal abduction. Blocking is considered if flexion is limited or intrinsic tightness is present.
The next visit if digit motion was limited is at 4 weeks, but at 6 weeks if digit motion is near normal, with swelling controlled and pain minimal. The patient is encouraged to schedule sooner if orthosis fit is loose because of decreased swelling.
Assess wrist motion around 6 weeks. If progression was observed, then begin a light strengthening program. The patient is instructed to avoid exercises that result in lasting pain. The patient is educated to consider stretching pain that resolves shortly after performing exercises as acceptable, provided it does not exceed a score of three of 10 on the pain scale, and there is no increase in swelling. Prolonged stretching is performed using a 1–2 lb weight. Discuss weaning from orthosis for all activities, except heavy use, with the goal of discontinuing orthosis at 8–10 weeks.
If progress is satisfactory, the patient should call to schedule the next appointment if needed. The patient is instructed to continue the home strengthening/stretching program until 12 weeks and then resume most normal use of the hand including weight-bearing, heavier work tasks, yard work, and exercise. Heavy lifting and competitive sports should not be started until 4 months, depending on the patient’s progress.
If no progress was noted in wrist motion and pain limits its use, the patient should follow-up in 2 weeks.
It is important to monitor whether the patients’ wrists become stiff quickly. Accelerated progression is necessary rather than holding the wrist until complete healing. Joint mobilization and more aggressive passive stretching are considered at 8 weeks if wrist motion is limited.
Pearls and Pitfalls
When drilling the dorsal lunate, it is important to target the drill into the lunate body and not toward the capitolunate joint (Fig. 2). Both dorsal drill tunnels should be parallel to each other, and both proximal tunnels should be parallel to each other. The goal should be to create at least a square, preferably a rectangular tunnel construct, to provide a large footprint over the scapholunate ligament (Fig. 7). When placing the anchor, do not countersink, as this can then penetrate past where is safe and enter the joint. Always lavage bones of any debris.
Complications
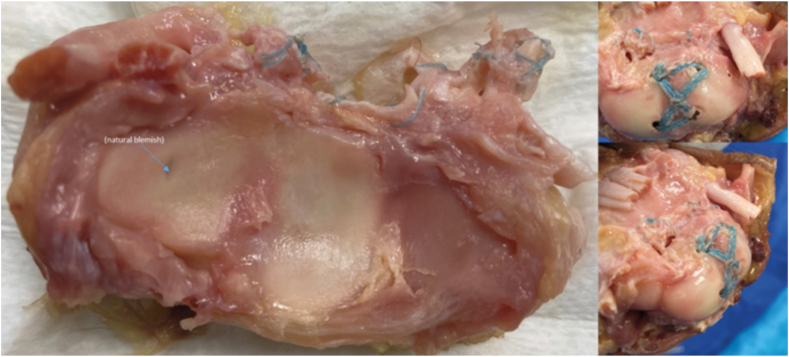
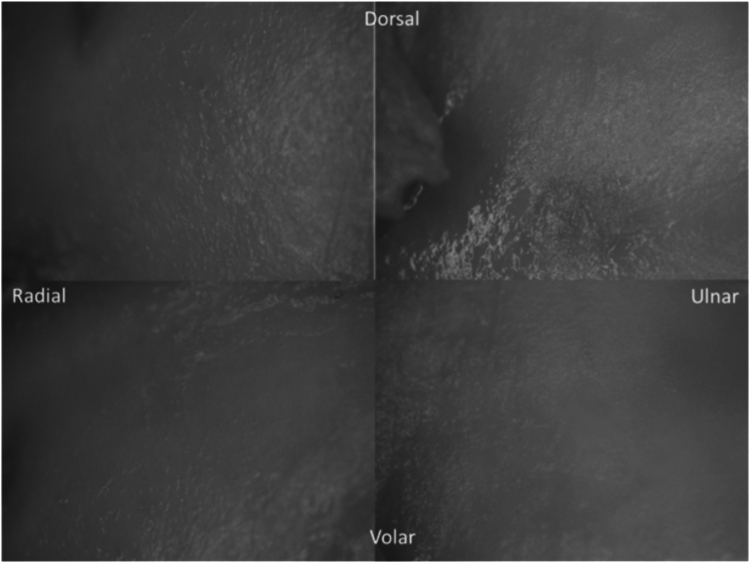
Aside from the benefits, the largest concern is the question of whether the nonabsorbable tape has any wear effects on the radial articular surface. Since the radiocarpal joint is mostly a non–weight-bearing joint, we would not expect any severe effects over time, as the tape itself is a thin and taut construct, tightly contouring against the bone. To be more certain, a cadaver specimen with the anatomic C technique was placed through 124,150 flexion-extension cycles on an 8871 Servohydraulic Instron Mechanical Testing System for three consecutive days (Fig. 8). To make this a more severe test, this specimen was reconstructed with 3.5-mm DX SwiveLock anchors (Arthrex Inc), 3.0-mm drill sockets, and thicker 2-mm FiberTape (Arthrex Inc). The radial articular surface underwent 2× magnification with a dissecting microscope. No visual differences were observed before and after, even with this thicker tape (Fig. 9). It was also of note that the construct itself remained as durable and intact as time zero.
Figure 8.
The anatomic C technique after 124,150 flexion-extension cycles on an 8871 Servohydraulic Instron Mechanical Testing System, for 3 days straight. This specimen was reconstructed with 3.5 mm DX SwiveLock anchors (Arthrex Inc), 3.0-mm drill sockets, and thicker 2-mm FiberTape (Arthrex Inc).
Figure 9.
The radial articular surface under 2× magnification of a dissecting microscope.
Biomechanical testing has also been performed on the strength and rotational stability of the anatomic C technique versus the all-dorsal technique. Maintenance of reduction strength was measured with an 8871 Servohydraulic Instron Mechanical Testing System by pulling apart 20 of 40 density sawbone blocks prepared using the all-dorsal versus the anatomic C techniques, until failure of the constructs was achieved. Student t test showed ultimate load between blocks in the all-dorsal technique with a mean of 311.76 N ± 40.31 N versus blocks in the anatomic C technique with a mean of 520.00 N ± 60.77 N (Table 2). The anatomic C construct showed a much stronger ultimate load (N) until failure—in other words, maintaining reduction—compared with the all-dorsal construct.
Table 2.
Student t test Showed Ultimate Load Between Blocks in the All-Dorsal Technique With a Mean of 311.76 N ± 40.31 N Versus Blocks in the Anatomic C Technique With a Mean of 520.00 N ± 60.77 N∗
 |
The anatomic C construct showed a much stronger ultimate load (N) until failure, in other words maintaining reduction, compared with the all-dorsal construct.
Rotational stability in cadaver specimens was also tested and compared between native/intact, resected, and repaired scapholunate ligament angles in the all-dorsal versus anatomic C techniques with the use of a calibrated goniometer attached to the scaphoid. Rotational stability in the all-dorsal technique in the native/intact SL ligament was 20.54° ± 3.02°, in resected was 30.45° ± 1.61°, and in repaired was 18.07° ± 1.37°, respectively. Rotational stability in the anatomic C technique in the native/intact SL ligament was 20.43° ± 2.12°, in resected was 35.80° ± 3.29°, and in repaired was 14.62° ± 1.73°, respectively (Table 3). Rotational stability within the cadaver specimens with the anatomic C technique showed slightly more stiffness, but notably more stability and retention of natural motions of the scaphoid relative to the lunate, compared with the all-dorsal technique.
Table 3.
Rotational Stability in the All-Dorsal Technique in the Native/Intact SL Ligament Was 20.54° ± 3.02°, Resected Was 30.45° ± 1.61°, and Repaired Was 18.07° ± 1.37°∗
 |
Rotational stability in the anatomic C technique in the native/intact SL ligament was 20.43° ± 2.12°, resected was 35.80° ± 3.29°, and repaired was 14.62° ± 1.73°. Rotational stability within the cadaver specimens with the anatomic C technique showed a bit more stiffness; however, much more stability and retention of natural motions of the scaphoid in relation to the lunate, compared with the all-dorsal technique.
Case Illustration
An active 26-year-old woman presented to the clinic with signs of bilateral wrist pain and scapholunate instability. She was a competitive soccer goalie for years and sustained many injuries to her wrists. She was in a bicycle accident 8 months prior. She went to the emergency department after her accident and was treated conservatively in a cast, as a left wrist sprain with therapy. After 2 months, a magnetic resonance imaging showed a partial scapholunate tear. Pain continued to increase with worsening instability. Despite another month of HT, she failed conservative treatment and wanted surgery. Wrist arthroscopy was performed, which found that the partial tear of the scapholunate interval had escalated into a full-thickness tear. An all-dorsal scapholunate reconstruction was performed as described by Chae and colleagues.9 She then began a typical scapholunate protocol.
During her healing period, while starting graduate school for HT, her opposite right wrist also began to increase in pain. She ended up going through therapy on both wrists simultaneously.
A magnetic resonance imaging of the right wrist demonstrated a partial scapholunate tear, which continued to worsen, and after 6 months of conservative treatment, she wanted surgery on this wrist as well. It was similar in pathology, although with a larger tear at the time of surgery. Diagnostic wrist arthroscopy followed by anatomic C scapholunate reconstruction was performed.
Her therapy protocol was much more aggressive on this right wrist with the anatomic C technique. After 2 weeks, she started dart thrower motion, flexion and extension, and scar massage. She was instructed to remove her orthosis 5–8 times per day to perform range-of-motion exercises. She then started strengthening at 5 weeks. At 3 months, she noted that her recovery went “scary fast” and was amazed at how quickly she progressed. Her grip on the right was 70 lbs with the anatomic C technique, whereas her grip on the left wrist was 65 lbs with the all-dorsal technique. At only 12 weeks, her active motion of the right wrist’s flexion was 65° and extension was 55° (Fig. 10A, B). This trend has been observed with other patients as well.
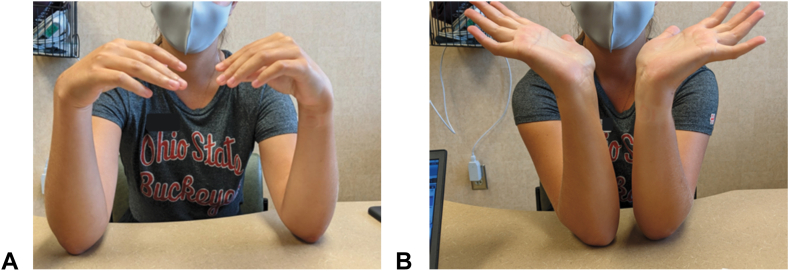
Figure 10.
A At 12 weeks, patient’s active motion of the right wrist’s flexion was 65°. B At 12 weeks, patient’s active motion of the right wrist’s extension was 55°.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
Robert Kalapos, MD, is an employee of Arthrex Inc, and Mollie Manley, MD, is a consultant to Arthrex Inc and has received no financial compensation regarding this manuscript.
Acknowledgments
The authors thank Quintino DeSousa, Illustration Designer.
References
- 1.Kitay A., Wolfe S.W. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2012;37:2175–2196. doi: 10.1016/j.jhsa.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 2.Brunelli G.A., Brunelli G.R. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg Am. 1995;20:S82–S85. doi: 10.1016/s0363-5023(95)80175-8. [DOI] [PubMed] [Google Scholar]
- 3.Thompson R.G., Dustin J.A., Roper D.K., Kane S.M., Lourie G.M. Suture tape augmentation for scapholunate ligament repair: a biomechanical study. J Hand Surg Am. 2021;46:36–42. doi: 10.1016/j.jhsa.2020.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Kakar S., Logli A.L., Ramazanian T., Gaston R.G., Fowler J.R. Scapholunate ligament 360° procedure. Bone Joint J. 2021;103-B(5):939–945. doi: 10.1302/0301-620X.103B5.BJJ-2020-1964.R2. [DOI] [PubMed] [Google Scholar]
- 5.Sandow M., Fisher T. Anatomical anterior and posterior reconstruction for scapholunate dissociation: preliminary outcome in ten patients. J Hand Surg Eur Vol. 2020;45(4):389–395. doi: 10.1177/1753193419886536. [DOI] [PubMed] [Google Scholar]
- 6.Rajan P.V., Day C.S. Scapholunate interosseous ligament anatomy and biomechanics. J Hand Surg. 2015;40:1692–1702. doi: 10.1016/j.jhsa.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 7.Overstraeten L.V., Camus E.J., Wahegaonkar A., et al. Anatomical description of the dorsal capsulo-scapholunate septum (DCSS)-arthroscopic staging of scapholunate instability after DCSS sectioning. J Wrist Surg. 2013;2(2):149–154. doi: 10.1055/s-0033-1338256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berger R.A., Bishop A.T., Bettinger P.C. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35:54–59. doi: 10.1097/00000637-199507000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Chae S., Roh Y.T., Park I.J. Scapholunate dissociation: current concepts of the treatments. Arch Hand Microsurg. 2020;25:77–89. [Google Scholar]