Abstract
Purpose of Review
Non-arthritic hip pain is a common presentation among the general population, with many possible contributing etiologies. While radiographs, computed tomography, and magnetic resonance imaging are all within the standard diagnostic workup, ultrasonography has emerged as a facile tool given its low cost, lack of radiation, and dynamic application. This article reviews the utility of ultrasound (US) in evaluation of non-arthritic hip pain and its ability to detect pathology both statically and dynamically in comparison and as an adjunct to standard imaging modalities.
Recent Findings
Current research highlights applications of US to commonly treated hip pathologies including femoroacetabular impingement, labral tears, hip microinstability, and various other extra-articular phenomena. While static evaluation seems to add similar value to that of radiography, several novel protocols have been developed that allow for dynamic evaluation of joint biomechanics, including extent and onset of impingement and femoral head translation, that cannot be assessed with more standard imaging modalities.
Keywords: Ultrasound, Femoroacetabular impingement, Microinstability, Non-arthritic hip pain, Femoroacetabular joint biomechanics, Femoral head translation, Dynamic hip evaluation
In evaluation of patients with non-arthritic hip pain, US is a low cost, easy-to-use, dynamic bedside tool that can aid in the diagnostic workup of patients with a broad number of pain generators. While literature demonstrates that its static evaluation often does not quite reach the accuracy of more advanced modalities, dynamic assessment of the hip joint has the potential to be quite useful in routine evaluation.
Introduction
Non-arthritic hip pain is common among the general population and affects patients across a wide range of ages [1]. Appropriate evaluation and workup are essential for diagnosing hip pain and determining the best treatment options, as the etiology of potential pain generators both within and surrounding the hip joint is extensive. As with many orthopaedic conditions, radiographs, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are commonly utilized in diagnostic workup. However, many conditions that affect the hip are dynamic in nature, ranging from those resulting in restricted range of motion (i.e., femoroacetabular impingement [FAI]) to excessive motion within the joint (i.e., dysplasia, instability). While the mentioned imaging modalities are excellent in assessing a patient’s static patho-anatomy, evaluation of many conditions may benefit from dynamic investigation. Ultrasonography presents an opportunity to evaluate the hip dynamically [2], with a lack of radiation, lower cost compared to other forms of advanced imaging, and minimal invasiveness [3]. While initially challenging with a notable learning curve requiring proper training [4], there are many benefits to this modality. This review will present the use of ultrasound (US) in evaluation of static hip anatomy and pathology as well as in dynamic evaluation to aid in diagnostic workup of non-arthritic hip pain.
Ultrasound Techniques
While US has become a widely used tool within medicine and specifically within the musculoskeletal system, technical set up is crucial to optimally evaluate appropriate anatomy. Transducer type, frequency, the use of Doppler, patient positioning and probe orientation should all be selected carefully. In general, higher-frequency linear transducers (10–20 MHz) are useful for the evaluation of superficial structures given improved spatial resolution with decreased penetration and depth, while lower-frequency linear transducers and occasionally, curvilinear transducers, have decreased resolution but can be valuable at evaluating deeper structures such as deeper joint recesses, or when evaluating larger patients [3, 5]. Transducer compression can be used to help differentiate a simple, compressible joint effusion from a less compressible complex joint effusion and synovial hypertrophy. Furthermore, real-time Doppler imaging can be used to assess for associated hyperemia, which may be beneficial in the setting of a suspected septic joint or an inflammatory arthropathy with active synovitis [3]. Like all imaging in orthopaedic surgery, it is important to note that all US findings should be imaged in perpendicular planes, i.e. short-axis/transverse and long-axis/longitudinal [5, 6]. Choosing patient and probe positioning is dependent on the focus of evaluation and will be discussed later in the review.
Static Hip Evaluation
US can be used to assess anterior, medial, lateral, and posterior hip structures and pathology. The anterior quadrant and associated structures can be easily visualized with the patient positioned supine, hip neutral rotation and slightly abducted with the probe placed anteriorly in the inguinal region in the long- and short-axes [2, 5, 7, 8], (Fig. 1). Both bone and soft tissue structures can be evaluated. Bony structures that can be evaluated include proximal femoral anatomy, such including cam morphology (Fig. 2), and basic acetabular anatomy, including the evaluation of FAI and subspine impingement. Evaluable soft tissue structures include the acetabular labrum (Fig. 3), the hip capsule, the surrounding musculotendinous structures, and the surrounding neurovascular structures (Figs. 1 and 2).
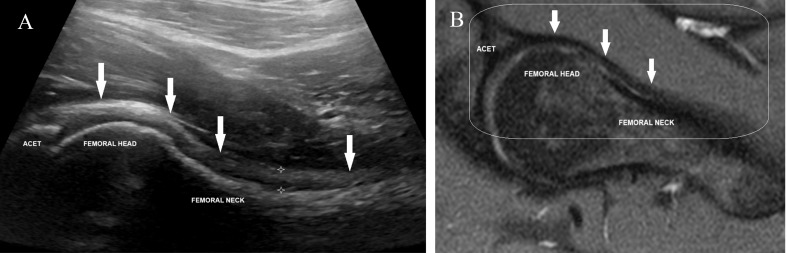
Fig. 1.
(A) Long-axis sonographic image of the normal hip obtained with the transducer placed obliquely along the femoral neck. The image demonstrates the acetabulum (ACET) and the proximal femur. The arrows point to the hip joint capsule extending inferiorly to near the greater trochanter and the stars measure the capsular thickness. (B) A sagittal proton density fat-suppressed MR image rotated counter-clockwise. The rectangle shows the field-of-view on US with the same corresponding structures
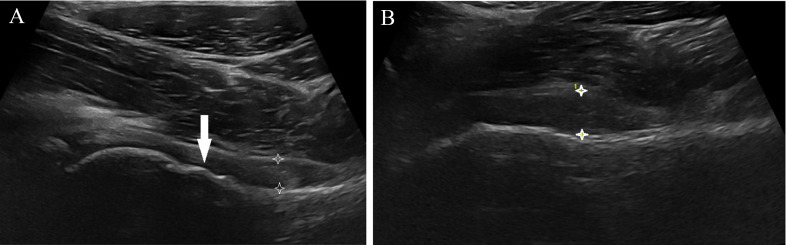
Fig. 2.
Long-axis US images of the hip at (A) neutral and (B) internal rotation. The arrow in A points to a cam deformity at the femoral head-neck junction. The stars show a thickened joint capsule measuring greater than 7 mm and further increasing in thickness during (B) internal rotation
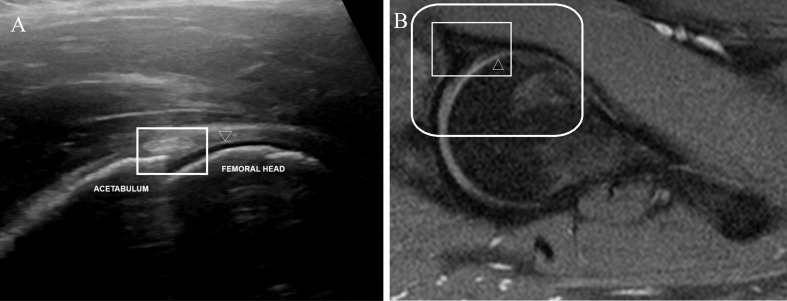
Fig. 3.
(A) Long-axis US image of the hip demonstrating the normal hyperechoic triangular-shaped anterior acetabular labrum (rectangle) with the anechoic articular cartilage (open arrowhead) along the femoral head. (B) A sagittal proton density fat-suppressed MR image rotated counter-clockwise. The outside, larger rectangle shows the field-of-view on US and the smaller inner rectangle surrounds the hypointense anterior acetabular labrum. The open arrowhead again depicts the hyperintense articular cartilage along the femoral head
Proximal Femur
In assessment of non-arthritic hip conditions, the use of US has been particularly valuable in the evaluation of proximal femur morphology and its contribution to underlying femoroacetabular impingement (FAI) (Fig. 2). While radiographs, CT, and MRI have previously been the mainstay of evaluation of proximal femur morphology, several metrics have been proposed in the sonographic evaluation of the proximal femur, including alpha angle, anterior femoral distance (AFD), and offset ratio. Buck et al. were the first to propose assessment of cam morphology with US in 2011, proposing a protocol for assessment of cam morphology and alpha angles in anterior and anterosuperior views [9]. In comparison to MRI, it was observed that neither alpha angle, presence of an osseous protuberance, nor the contour of the femoral neck were sensitive or specific for detection of cam-type morphology on US, and notably only found moderate inter-reader agreement of US evaluation [9]. On the contrary, Lerch et al. later measured alpha angle with the hip in 20 degrees of external rotation, neutral rotation, and 20 degrees of internal rotation and found measurements at internal rotation and neutral to have significant correlation to alpha angle measured on MRI (0.77 p < 0.0001 at 20 degrees of internal rotation), as well as noting correlation of US and MRI in regard to AFD and offset ratio (the quotient of the head-neck offset divided by the head diameter), with good overall interobserver reliability [10]. Lerch further expanded on these results in 2016 in comparison to standard radiographs (AP, frog-leg lateral views) and found US was as reliable at diagnosing FAI when using MRI as the gold standard [11]. In contrast, when comparing to a CT scan, Robinson et al. found US evaluation of alpha angle to have a high sensitivity (91.3%), but a low specificity (43.8% and > 10 degrees of absolute value difference between the two modalities [12]. Hsu et al. focused on anterior femoral distance, a measurement that per author takes 10 s to record, and found that it was reliable at diagnosing FAI in the anterior but not anterosuperior contour (gold standard MRI measurements of alpha angle > 55 degrees), with sensitivity and specificity of 80.9 and 87.5%, respectively [13]. In regards to clinical outcomes, Biernacki et al. utilized the methodology of Buck and found that an alpha angle greater than 60 degrees was correlated with worse iHOT scores compared to those with lower alpha angles [14]. Overall, while some data appears promising, given the mixed data on accuracy of using US in assessment of proximal femur morphology when compared to CT or MRI, use may be most optimal as a screening tool that helps guide the physician towards further advanced imaging and assessment, and not as the sole imaging modality in diagnostic workup.
Acetabulum
Although difficult to evaluate pincer lesions on US [9], the acetabulum can also be visualized to assess for the presence of subspine impingent. Anterior inferior iliac spine (AIIS) morphology has been found to frequently play a role in patients with FAI, with inferior and distal extension of the subspine found to occur in just over 20% of patients with FAI [15, 16]. While most frequently evaluated on CT scan, two studies have investigated the utility of US in assessment of AIIS morphology [17, 18]. In particular, Amar et al. found high accuracy (92.3%) in the classification of subspine morphology when compared to false profile radiographs [18]. Of note, this evaluation was performed with the patient supine and the probe placed in the long-axis at the inguinal region at the level of the hip joint (Fig. 4).
Fig. 4.
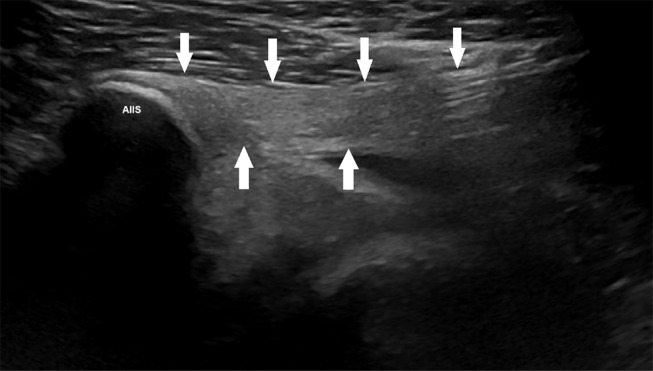
Long-axis sonographic image along the anterior aspect of the hip reveals the anterior inferior iliac spine (AIIS) and a normal direct head rectus femoris tendon (arrows)
Sun et al. applied US in combination with CT to determine what findings may suggest clinical subspine impingement. They found that US identification of type III bone morphology, as well as heterogenous hypoechoic signal in the anterosuperior joint capsule and the direct rectus femoris tendon origin were associated with arthroscopically confirmed subspine impingement. When combined with evidence of a low-lying AIIS on CT scan, US had a sensitivity of 75.0% and specificity of 77.4% for clinical subspine impingement [17]. These results suggest that US may be a useful adjunct to assess when a patient may have clinical subspine impingement contributing to their overall symptomology.
Acetabular Labrum
Evaluation of the labrum is important in the diagnostic workup of non-arthritic hip pain, with a number of different etiologies (trauma, FAI, capsular laxity, hip hypermobility, dysplasia, degeneration) potentially contributing to labral pathology [19]. While arthroscopic evaluation is the gold standard assessment, MR arthrography is generally considered the optimal non-operative imaging modality, as the intraarticular administration of a gadolinium contrast mixture facilitates improved visualization of the labrum [19]. Use of US for evaluation of the labrum was first reported by Mitchell et al. in 2003, during which poor utility was noted with only 13% sensitivity of detection of labral tears on US in a study of 25 hip arthroscopies [20]. Sofka et al. further documented the US exam of the labrum, noting best assessment with standard anterior viewing with the transducer placed along the long-axis of the hip joint with the patient supine (of note, only the anterosuperior labrum can be viewed in this plane). They described the normal labrum to appear as a hyperechoic, compact, triangular structure (Fig. 3A), with tears visualized as irregular or linear hypoechoic fissures or clefts [21], (Fig. 5). Additionally, ultrasonography after intraarticular injection, referred to as the “sonographic effect,” may improve visualization [21, 22].
Fig. 5.
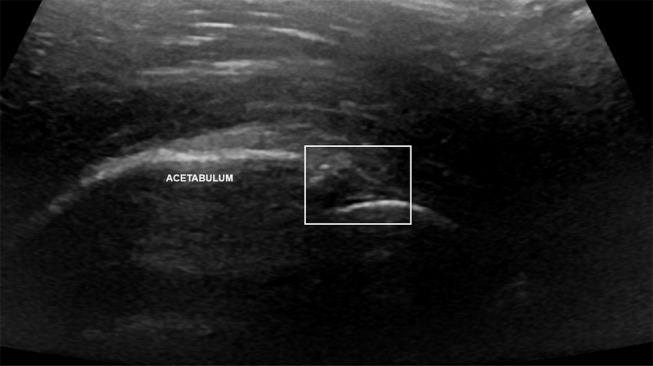
Long-axis US image of the anterior hip showing an ill-defined, irregular hypoechoic appearance of the anterior acetabular labrum consistent with a complex tear (rectangle)
As compared to MRI, Troelsen et al. reported a sensitivity of 44% and a specificity of 75% for diagnosing labral tears via ultrasound; however the authors found improved results in a subsequent study, including a sensitivity of 95% and only one false negative (no true negatives reported in a study of 17 hips). This was felt to be secondary to improved experience of the same examiner across both studies [23, 24]. A number of other studies have investigated the accuracy of US compared to MR since then [22, 25, 26], with the largest cohort reported of 195 patients, noting that when using arthroscopic evaluation as the gold standard, US had a lower sensitivity (68.5%) but a higher specificity (81.8%) when compared to 3T MRI [27]. A recent article by Fu et al. proposed several criteria for US evaluation of the acetabular labrum, and found that labral heterogenous echogenicity was the most indicative of a labral tear, but the combination of this alongside a labral cleft, plump morphology, paralabral cysts, and a focal hyperechoic area portrays a diagnosis of labral tear, with a sensitivity of 90%, specificity of 71%, and accuracy of 85%. They also suggested using the cross-sectional area of the labrum as a diagnostic criteria, with a cutoff of 0.215 cm2 contributing to the best diagnostic efficacy (sensitivity and specificity 74%) [28]. Overall, utilization of US for evaluation of the acetabular labrum is a quick, inexpensive, and dynamic option which provides direct visualization of the anterosuperior labrum and underlying pathology.
Femoroacetabular Joint Capsule
The hip capsule is an easily evaluated structure on US at it lies superficial to the joint (Figs. 1A and 2). A distance of 7 mm or more between the capsule and femur is indicative of a joint effusion and/or synovial hypertrophy with good reproducibility and interobserver reliability [29] (Fig. 2). In addition to using the capsule as a proxy for joint effusion and synovial hypertrophy, capsular evaluation may be particularly important in evaluation of patients with instability and ligamentous laxity, as the hip capsule is crucial to joint biomechanics and stability [30, 31], and these patients may have altered capsular anatomy and biomechanics (Fig. 2). A recent study by Gao et al. found US to be effective in evaluation of capsular thickness, finding mean hip joint capsule thickness in 307 patients to be 5.0 ± 1.5 mm and 5.0 ± 1.2 mm when measured by US and MRI, respectively, spending only 5–10 min on examination [32].
Other Structures
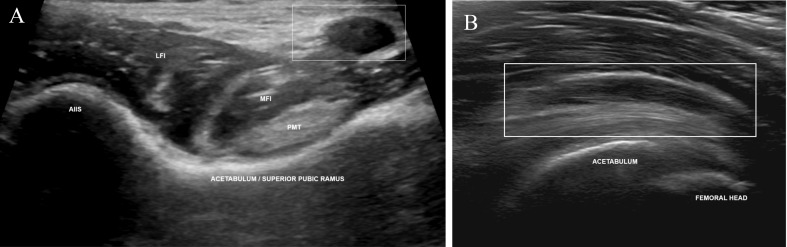
Extra-articular musculature can be easily visualized with ultrasound. From the supine position, the rectus femoris origin and musculotendinous junction can be evaluated (Fig. 4), as well as the iliopsoas insertion and musculotendinous junction (Fig. 6). Placing the leg and hip in a frog-leg position can allow for direct visualization of the hip adductors, originating from the pubis and ischium of the pelvis. In the lateral position, the gluteal musculature as well as the iliotibial band and underlying greater trochanteric bursa can be viewed with patient’s hip in slight flexion. The proximal musculature is best viewed in the longitudinal plane at or below the level of the iliac tubercle, while the trochanteric bursa, gluteus medius insertion, and bony architecture of the greater trochanter are best viewed directly over the greater trochanter in either the transverse or longitudinal plane. Turning attention posteriorly, the hamstring musculature can be identified most easily at their origins at the ischial tuberosity. This is best done with the patient in prone positioning and the probe in the transverse plane, during which the conjoint tendon (semitendinosus, long head of the biceps femoris), semimembranosus, and additionally the sciatic nerve can be evaluated as they travel distally, along with the short head of the biceps originating from the linea aspera of the femur. Posteriorly, the piriformis muscle can also be identified at the level of the greater sciatic notch, at the lateral border of the sacrum passing cephalomedial to caudolateral just beneath the gluteus maximus [2, 5, 8].
Fig. 6.
Sonographic images of the normal iliopsoas complex at the level of the acetabulum. (A) Short-axis image demonstrates the anterior inferior iliac spine (AIIS) laterally and the psoas major tendon medially. The rectangle surrounds the neurovascular bundle. (B) Long-axis image showing the normal iliopsoas myotendinous structures overlying the acetabulum with the tendon appearing hyperechoic and fibrillar and the surrounding muscle more hypoechoic. Abbreviations: LFI, lateral fibers of the iliacus muscle; MFI, medial fibers of the iliacus muscle
Dynamic Hip Evaluation
The hip is a dynamic joint and many of the conditions that contribute to non-arthritic pathologies can be related to either restricted motion (i.e., FAI, subspine impingement) or too much motion (i.e., dysplasia, microinstability). While standard imaging modalities are nearly always used to evaluate the static anatomy of the hip, US offers the ability to dynamically evaluate the anatomic structures around the hip and evaluate for pathological states as the hip is exposed to various positions, stresses, and ranges of motion. Several publications have defined protocols for dynamic evaluation of the hip and associated conditions [7, 33], as will be discussed in subsequent sections.
Hip Range of Motion and Femoroacetabular Impingement
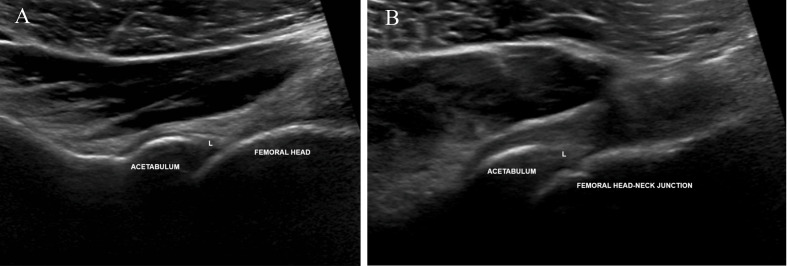
The use of US to evaluate the hip joint during motion has identified that much of the prior normative data regarding the degree of motion within the femoroacetabular joint is largely inaccurate due to the difficulty with evaluation of the relationship of soft tissues, bony anatomy and contributions of lumbosacral movement to hip joint mobility. In a study of 40 asymptomatic young males, Larkin et al. found the mean impingement-free hip range of motion is 65 degrees of flexion (the point at which labral morphology began to change) and bony abutment between the femur and acetabulum occurs at approximately 95 degrees, which is approximately 25% less than values that have been previously described [34]. In asymptomatic young women, values were found to be slightly higher, with mean impingement-free flexion and maximum flexion observed at 72 and 101 degrees, respectively [35]. In patients experiencing symptoms of FAI, Sahr et al. proposed that dynamic evaluation of hip ROM and impingement may be useful in determining the clinical significance of FAI. With the probe at the anterolateral aspect of the hip and oriented in the long-axis/longitudinal plane, the joint can be flexed from neutral to 90 degrees. Identification of femoral morphology through ROM, the point at which the labrum becomes impinged, and reproduction of symptoms are useful indicators of clinically relevant FAI [33], (Fig. 7).
Fig. 7.
Long-axis US images during dynamic imaging for FAI with the transducer placed along the anterolateral aspect of the hip. (A) Image obtained at neutral and showing the anterolateral aspect of the normal, triangular-shaped acetabular labrum (L). (B) Representative, long-axis dynamic image obtained while flexing the hip to 90 degrees showing no evidence of FAI with no deformation of the labrum and no osseous/cam impingement
Understanding of the point of impingement as well as normative hip ROM is critical in surgical decision-making, both preoperatively and intraoperatively, for patients with abnormal hip kinematics and hip pain.
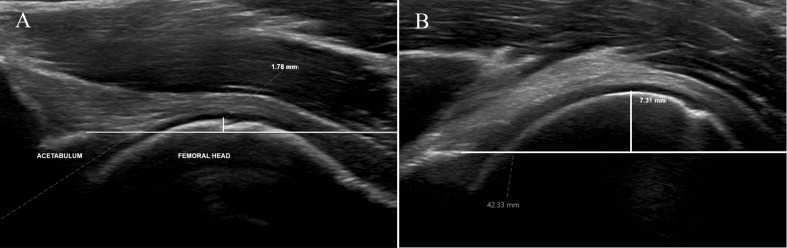
Microinstability
US has also been found to be useful for patients suspected of having hip microinstability when used to dynamically evaluate the hip during range of motion. Microinstability is when supraphysiologic motion of the femoral head occurs within the acetabulum, which can be associated with hip pain and patients who report a subjective sensation of hip instability [36]. Anterior translation of the femoral head with respect to the adjacent acetabulum can be evaluated with the patient in a supine or prone position. An anterior-directed force can be applied by either placing the hip in abduction, external rotation, and extension off the exam table while using it as a fulcrum, or with the patient prone and allowing gravity to apply an anterior force to the head [33]. Building on this, as proposed by D’Hemecourt et al. in 2019, femoral head translation can be quantified sonographically by measuring anterior femoral head translation as the hip goes from a neutral to a position that maximizes anterior femoral head translation, a position akin to an anterior apprehension test (hip extended, externally rotated off the side of the bed, and contralateral hip hyper-flexed), yielding excellent intra- and interrater reliability between three physicians [37], (Fig. 8).
Fig. 8.
Long-axis sonographic images of the anterior hip during dynamic imaging for microinstability. (A) Image obtained at neutral revealing the anterior aspect of the femoral head to be only minimally (1.78 mm) anterior to the acetabulum. (B) Image obtained with the ipsilateral hip extended and externally rotated and the contralateral hip hyperflexed. This resulted in significant (7.31 mm) anterior translation of the femoral head, anterior to the acetabulum, during stress maneuvers with bowing of the overlying joint capsule and corresponding symptoms, consistent with microinstability
In a cohort of young females, the same group found that in positions of extension with external rotation, dancers with hip pain experienced larger anterior femoroacetabular translation compared to non-dancers with hip pain (mean 6.3 mm vs. 5.2 mm; p = 0.01), and that dancers with hip pain also had higher anterior translation than dancers without hip pain (6.3 mm vs. 4.2 mm; p < 0.001) [38]. Jackson et al. similarly evaluated hip anterior translation in a group of asymptomatic dancers in the neutral and extension/external rotation positions of the hip joint and found anterior translation in extension, external rotation to be a mean of 3.8 mm and 4.1 mm in females and males, respectively, with a mean difference of 1.2 mm and 1.3 mm anterior to anterior translation in the neutral position [39].
In contrast to anterior translation of the femoral head, Le et al. proposed a protocol for evaluation of posterior femoroacetabular translation with the patient in either a lateral decubitus or standing position, with the probe at the lateral aspect of the hip, parallel to the femur. Posterior directed forces were obtained by either passively flexing 110°, adducting, and internally rotating the hip (PFADIR) while in a lateral decubitus position, or by having the patient stand with feet hip-distance apart and flexing their spine over to reach their contralateral toes (PStand). In this cohort, they found mean values of translation to be 3.6 mm, 10.5 mm, and 8.2 mm for neutral, PFADIR, and PStand respectively, with fair to good intra-rater reliability and good to excellent inter-rater reliability [40]. Given its ability to observe joint biomechanics while simultaneously assessing a patient’s symptomatology throughout motions placing both anterior and posterior stress on the joint, US is a useful tool at determining the role hip microinstability plays in a patient’s pathology. It remains to be seen how these sonographic findings of instability correlate with symptom relief after various surgical treatments.
Ischiofemoral Impingement
Ischiofemoral impingement is a less common etiology of hip pain compared to other sources and involves mechanical conflict between the lesser trochanter and ischium of the pelvis. This condition is best evaluated with the patient in a prone position and with the probe transversely oriented around the level of the gluteal crease to visualize the ischiofemoral space, which is bound medially by the ischium and laterally by the lesser trochanter, with the quadratus femoris muscle and sciatic nerve visualized within this space. The knee can then be flexed at 90 degrees to allow for control of femoral rotation– the ischiofemoral space is observed while externally rotating the hip, noting impingement with marked compression of the quadratus femoris as well as possibly the sciatic nerve, along with reproduction of patient symptoms [33]. While evaluation of the ischiofemoral space has most commonly been performed with MRI, measurements attained by US have been found to be correlated to those of MRI in both asymptomatic patients and those with symptoms of ischiofemoral impingement, although with variable accuracy compared to MRI [41, 42]. Further reports have noted that using an US-guided anesthetic injection of the fascial plane between the quadratus femoris and the obturator muscles can help in diagnosis and treatment of ischiofemoral syndrome [43–45].
Snapping Hip Syndrome
Snapping hip syndrome is a condition in which an audible or palpable “snap” or pop can be felt or heard by the patient during motion of the hip. It is often associated with pain, locking, or a stabbing sensation and has been reported to occur in as high as 5–10% of the general population [46]. While intra-articular pathology can cause similar symptoms in what is described as intra-articular snapping hip syndrome, extra-articular snapping hip syndrome can be further delineated as internal and external. Internal snapping is caused by the iliopsoas tendon snapping over the iliopectineal eminence, whereas external snapping is caused by movement of the gluteus maximus or the iliotibial band over the greater trochanter [46, 47]. Extra-articular snapping hip syndrome can often be diagnosed with clinical exam, however, dynamic US can be useful for confirmation and identification of involved structures [5]. In evaluation of external snapping hip, the patient is best positioned in the lateral decubitus position with the probe evaluating the peri-trochanteric region, with evaluation of relative movement of structures while the patient flexes and extends their hip. In early flexion, transient restraint of the iliotibial band and gluteus maximus tendon against the posterolateral aspect of the greater trochanter will be seen, followed by a sudden release with increased flexion. Care should be taken to observe the state of the iliotibial band and greater trochanteric bursa, as these can be thickened and inflamed [48]. Internal snapping hip is best observed with the patient supine, with the transducer held in an oblique transverse plane between the anteroinferior iliac spine and the superior pubic ramus (Fig. 6A). The patient then performs hip flexion-abduction-external rotation, followed by extension and adduction; the sonographer then evaluates for snapping of the psoas major tendon on the superior pubic ramus with extension and adduction [46, 48]. Alternatively, for both external and internal snapping hip evaluation, the patient can also be asked to produce any movements that they know will reproduce their symptoms.
Intra-Operative Use during Hip Arthroscopy
Several investigations have applied the use of US intra-operatively alongside hip arthroscopy and the surgical treatment of FAI. Intra-operative use was first described by Hua et al. in attempt to limit radiation and provide a better assessment of 3-dimensional space and soft tissue structures than fluoroscopy. An intra-operative radiologist assisted with the procedure, and while the group found US to be successful with limited complications, they did note drawbacks including a crowded surgical field, the potential for poor visualization with hemorrhage as well as increased difficulty with larger patient habitus [49]. Weinrauch et al. published methodology with a similar technique, however, without the assistance of a radiologist and with the use of longitudinal traction, and although finding a similar low iatrogenic complication rate and eventual ease of use, noted the importance of undergoing formal musculoskeletal US training as well as using fluoroscopy for assistance in their first 30 cases [50]. Keough et al. demonstrated the use of US-assistance in lateral positioning, and while also noted success, expressed similar limitations to prior as well as possibly losing the ability to judge the extent of resection during osteoplasty [51]. Results of comparative studies between US and fluoroscopy have been mixed, with advantages of US notable for being less cumbersome and able to image from anterior to posterior [52], however, with potentially higher operative time and higher rate of iatrogenic injury, at least early in training [53]. In addition to its use for portal placement intraoperatively, Kaplan et al. proposed a protocol for assessing cam lesions intraoperatively, although given the steep learning curve and prior heterogenous results of measuring alpha angles with US, suggested US may best be used pre- and post-operatively, not intra-operatively, to avoid radiation at less “critical” timepoints [54]. However, a study by Clapp et al. investigated US measurement of pre- and post-osteoplasty alpha angles in 20 cadaveric hips and found no significant difference between measurements on US and fluoroscopy in six hip positions pre- and post-osteoplasty, aside from flexion with neutral rotation post-osteoplasty [55], suggesting US may be a feasible alternative to intraoperative fluoroscopy. Overall, while intraoperative use of US does present advantages such as limiting radiation and allowing for dynamic assessment of bone and soft tissue in multiple planes, the intraoperative utility is debatable and may come with a steep learning curve.
Conclusion
Several imaging modalities have become useful in diagnostic workup of patients presenting with non-arthritic hip pain. Current literature demonstrates inconclusive accuracy of US to detect hip pathology in static evaluation when compared to MRI, suggesting US may be more useful as an adjunct or screening tool in this regard. However, in dynamic application, US allows for evaluation of joint biomechanics (i.e., pathologic range of motion, femoral head translation) as well as the dynamic interplay of extra-articular anatomy (i.e., ischiofemoral impingement, snapping hip syndrome) which can be difficult to assess with more traditional, static modalities. Further investigations remain necessary to standardize methodology and normative values, as well as investigate ways in which US can be better optimized for intraoperative use.
Key References
Papers of particular interest, published recently (within past 3 years), have been highlighted as:
• Of importance.
•• Of major importance.
-
17.
• Sun Y, Liu R, Tian Y, Fu Q, Zhao Y, Xu Y, et al. Ultrasound Assessment of Hip Subspine Bone Morphology Soft-tissue Correlates with Clinical Diagnosis of Impingement. Arthroscopy. 2023;39(10):2144-53. 10.1016/j.arthro.2023.03.024. A retrospective study demonstrating the utility of US in evaluation of subspine impingement, finding it may be a useful adjunct to CT and an alternative to plain radiographs.
-
18.
• Amar E, Rosenthal R, Guanche CA, Palmanovich E, Ankory R, Levy O, et al. Sonographic evaluation of anterior inferior iliac spine morphology demonstrates excellent accuracy when compared to false profile view. Knee Surg Sports Traumatol Arthrosc. 2021;29(5):1413-9. 10.1007/s00167-020-06304-x. A comparative study suggesting US evaluation of subspine morphology is reliable and comparable to that of standard radiographic evaluation.
-
28.
• Fu Q, Jiang L, Cui L, Gao G, Xu Y, Tian C, et al. Quantitative and Qualitative Ultrasound Evaluation for the Diagnosis of an Anterosuperior Acetabular Labral Tear. Ultrasound Med Biol. 2022;48(5):924 − 32. 10.1016/j.ultrasmedbio.2022.01.016. An investigation of US evaluation of acetabular labral tears, identifying several characteristics to help in identification of clinically relevant pathology.
-
32.
• Gao G, Fang H, Zhou K, Mo Z, Liu J, Meng L, et al. Ultrasound had high accuracy in measuring hip joint capsule thickness. BMC Musculoskelet Disord. 2024;25(1):101. 10.1186/s12891-024-07228-0. A retrospective review suggesting that US is a low-cost, reliable alternative to MRI in evaluation of hip joint capsule thickness.
-
33.
•• Sahr ME, Endo Y, Sink EL, Miller TT. Dynamic ultrasound assessment of hip instability and anterior and posterior hip impingement. Skeletal Radiol. 2023;52(7):1385-93. 10.1007/s00256-022-04264-6. A technical report describing methods of dynamic US evaluation of hip instability as well as femoroacetabular and ischiofemoral impingement alongside relevant physical exam maneuvers.
-
38.
•• Scott CP, d’Hemecourt PA, Miller PE, Sugimoto D, Jackson SS, Kobelski GP, et al. Femoroacetabular translation in female athletes and dancers assessed by dynamic hip ultrasonography. BMJ Open Sport Exerc Med. 2021;7(4):e001169. 10.1136/bmjsem-2021-001169. A comparative study demonstrating larger femoroacetabular translation in female dancers with hip pain when compared to female non-dancers with hip pain as well as asymptomatic female dances via US evaluation.
-
40.
•• Le HM, d’Hemecourt PA, Jackson SS, Whitney KE, Miller PE, Millis MB, et al. Protocol and validity testing of femoroacetabular posterior translation with dynamic hip ultrasonography. Skeletal Radiol. 2024;53(7):1287-93. 10.1007/s00256-024-04560-3. A feasibility study presenting a protocol for dynamic evaluation of femoroacetabular posterior translation using US, demonstrating reliability across raters with variable levels of US experience.
-
53.
•• Trasolini NA, Sivasundaram L, Rice MW, Gursoy S, Clapp IM, Alter TD, et al. Ultrasound Can Determine Joint Distraction During Hip Arthroscopy but Fluoroscopic-Guided Portal Placement Is Superior. Arthrosc Sports Med Rehabil. 2022;4(3):e1083-e9. 10.1016/j.asmr.2022.03.005. A cadaveric study demonstrating US is useful in evaluation adequate joint distraction during hip arthroscopy, however with higher frequency of iatrogenic injury and longer procedure time when compared to standard fluoroscopic guidance.
-
55.
•• Clapp IM, Alter TD, Sivasundaram L, Gursoy S, Perry AK, Nho SJ. Ultrasound Demonstrates Potential in Identifying Proximal Femoral Morphology Before and After Cam Resection: A Cadaveric Study. Arthroscopy. 2023;39(3):751-7.e2. 10.1016/j.arthro.2022.10.015. A cadaveric study suggesting US may be a feasible alternative to intraoperative fluoroscopy at evaluated pre- and post-osteoplasty alpha angles intraoperatively.
Author Contributions
S.R., S.S., and M.H. drafted the main manuscript. S.S. provided Figures for the manuscript. A.G. and I.Z. provided important guidance with content and detailed editing and proofing of the final manuscript.
Funding
No funding was received.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Enseki KR, Bloom NJ, Harris-Hayes M, Cibulka MT, Disantis A, Di Stasi S, et al. Hip Pain and Movement Dysfunction Associated with Nonarthritic Hip Joint Pain: a revision. J Orthop Sports Phys Ther. 2023;53(7):Cpg1–70. 10.2519/jospt.2023.0302. [DOI] [PubMed] [Google Scholar]
- 2.Tyng-Guey W. Ultrasonographic Examination of the adult hip. J Med Ultrasound. 2012;20(4):201–9. 10.1016/j.jmu.2012.10.009. [Google Scholar]
- 3.Nestorova R, Vlad V, Petranova T, Porta F, Radunovic G, Micu MC, et al. Ultrasonography of the hip. Med Ultrason. 2012;14(3):217–24. [PubMed] [Google Scholar]
- 4.Mullaney PJ. Qualitative ultrasound training: defining the learning curve. Clin Radiol. 2019;74(4):327..e7-.e19. [DOI] [PubMed] [Google Scholar]
- 5.Lungu E, Michaud J, Bureau NJ. US Assessment of sports-related hip injuries. Radiographics. 2018;38(3):867–89. 10.1148/rg.2018170104. [DOI] [PubMed] [Google Scholar]
- 6.Backhaus M, Burmester GR, Gerber T, Grassi W, Machold KP, Swen WA, et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60(7):641–9. 10.1136/ard.60.7.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mezian K, Ricci V, Güvener O, Jačisko J, Novotný T, Kara M, et al. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for (adult) hip. Am J Phys Med Rehabil. 2022;101(11):e162–8. 10.1097/phm.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 8.Probyn L, Flores D, Rowbotham E, Cresswell M, Atinga A. High-resolution ultrasound in the evaluation of the adult hip. J Ultrason. 2023;23(95):e223–38. 10.15557/jou.2023.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buck FM, Hodler J, Zanetti M, Dora C, Pfirrmann CW. Ultrasound for the evaluation of femoroacetabular impingement of the cam type. Diagnostic performance of qualitative criteria and alpha angle measurements. Eur Radiol. 2011;21(1):167–75. 10.1007/s00330-010-1900-x. [DOI] [PubMed] [Google Scholar]
- 10.Lerch S, Kasperczyk A, Warnecke J, Berndt T, Rühmann O. Evaluation of Cam-type femoroacetabular impingement by ultrasound. Int Orthop. 2013;37(5):783–8. 10.1007/s00264-013-1844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lerch S, Kasperczyk A, Berndt T, Rühmann O. Ultrasound is as reliable as plain radiographs in the diagnosis of cam-type femoroacetabular impingement. Arch Orthop Trauma Surg. 2016;136(10):1437–43. 10.1007/s00402-016-2509-6. [DOI] [PubMed] [Google Scholar]
- 12.Robinson DJ, Lee S, Marks P, Schneider ME. Ultrasound determination of the femoral Head-Neck Alpha Angle. Ultrasound Med Biol. 2018;44(2):495–501. 10.1016/j.ultrasmedbio.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Hsu YC, Wu YC, Wang HH, Lee MS, Huang GS. Assessment of cam-type femoroacetabular impingement by ultrasonography: value of anterior femoral distance measurements. Ultraschall Med. 2012;33(7):E158–65. 10.1055/s-0032-1330325. [DOI] [PubMed] [Google Scholar]
- 14.Biernacki JL, d’Hemecourt PA, Stracciolini A, Owen M, Sugimoto D. Ultrasound alpha angles and Hip Pain and function in female Elite Adolescent Ballet dancers. J Dance Med Sci. 2020;24(3):99–104. 10.12678/1089-313x.24.3.99. [DOI] [PubMed] [Google Scholar]
- 15.Amar E, Warschawski Y, Sharfman ZT, Martin HD, Safran MR, Rath E. Pathological findings in patients with low anterior inferior iliac spine impingement. Surg Radiol Anat. 2016;38(5):569–75. 10.1007/s00276-015-1591-8. [DOI] [PubMed] [Google Scholar]
- 16.Aguilera-Bohorquez B, Brugiatti M, Coaquira R, Cantor E. Frequency of Subspine Impingement in patients with femoroacetabular impingement evaluated with a 3-Dimensional dynamic study. Arthroscopy. 2019;35(1):91–6. 10.1016/j.arthro.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 17.Sun Y, Liu R, Tian Y, Fu Q, Zhao Y, Xu Y, et al. Ultrasound Assessment of Hip Subspine bone morphology soft-tissue correlates with clinical diagnosis of impingement. Arthroscopy. 2023;39(10):2144–53. 10.1016/j.arthro.2023.03.024. [DOI] [PubMed] [Google Scholar]
- 18.Amar E, Rosenthal R, Guanche CA, Palmanovich E, Ankory R, Levy O, et al. Sonographic evaluation of anterior inferior iliac spine morphology demonstrates excellent accuracy when compared to false profile view. Knee Surg Sports Traumatol Arthrosc. 2021;29(5):1413–9. 10.1007/s00167-020-06304-x. [DOI] [PubMed] [Google Scholar]
- 19.Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105–17. 10.1007/s12178-009-9052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell B, McCrory P, Brukner P, O’Donnell J, Colson E, Howells R. Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sport Med. 2003;13(3):152–6. 10.1097/00042752-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Sofka CM, Adler RS, Danon MA. Sonography of the acetabular labrum: visualization of labral injuries during intra-articular injections. J Ultrasound Med. 2006;25(10):1321–6. 10.7863/jum.2006.25.10.1321. [DOI] [PubMed] [Google Scholar]
- 22.Jung JY, Kim GU, Lee HJ, Jang EC, Song IS, Ha YC. Diagnostic value of ultrasound and computed tomographic arthrography in diagnosing anterosuperior acetabular labral tears. Arthroscopy. 2013;29(11):1769–76. 10.1016/j.arthro.2013.07.274. [DOI] [PubMed] [Google Scholar]
- 23.Troelsen A, Jacobsen S, Bolvig L, Gelineck J, Rømer L, Søballe K. Ultrasound versus magnetic resonance arthrography in acetabular labral tear diagnostics: a prospective comparison in 20 dysplastic hips. Acta Radiol. 2007;48(9):1004–10. 10.1080/02841850701545839. [DOI] [PubMed] [Google Scholar]
- 24.Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop. 2009;80(3):314–8. 10.3109/17453670902988402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jin W, Kim KI, Rhyu KH, Park SY, Kim HC, Yang DM, et al. Sonographic evaluation of anterosuperior hip labral tears with magnetic resonance arthrographic and surgical correlation. J Ultrasound Med. 2012;31(3):439–47. 10.7863/jum.2012.31.3.439. [DOI] [PubMed] [Google Scholar]
- 26.Liu XD, Cui LG, Xu Y, Sun Y, Hao YX, Song L. [Application of ultrasound for evaluation of anterosuperior acetabular labral tear]. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49(6):1014–8. [PubMed] [Google Scholar]
- 27.Gao G, Fu Q, Cui L, Xu Y. The diagnostic value of Ultrasound in Anterosuperior Acetabular Labral tear. Arthroscopy. 2019;35(9):2591–7. 10.1016/j.arthro.2019.02.052. [DOI] [PubMed] [Google Scholar]
- 28.Fu Q, Jiang L, Cui L, Gao G, Xu Y, Tian C, et al. Quantitative and qualitative Ultrasound evaluation for the diagnosis of an Anterosuperior Acetabular Labral tear. Ultrasound Med Biol. 2022;48(5):924–32. 10.1016/j.ultrasmedbio.2022.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Koski JM, Anttila PJ, Isomäki HA. Ultrasonography of the adult hip joint. Scand J Rheumatol. 1989;18(2):113–7. 10.3109/03009748909099926. [DOI] [PubMed] [Google Scholar]
- 30.Nepple JJ, Smith MV. Biomechanics of the Hip Capsule and Capsule Management Strategies in Hip Arthroscopy. Sports Med Arthrosc Rev. 2015;23(4):164–8. 10.1097/jsa.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 31.Kay J, Memon M, Rubin S, Simunovic N, Nho SJ, Belzile EL, et al. The dimensions of the hip capsule can be measured using magnetic resonance imaging and may have a role in arthroscopic planning. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1246–61. 10.1007/s00167-018-5162-5. [DOI] [PubMed] [Google Scholar]
- 32.Gao G, Fang H, Zhou K, Mo Z, Liu J, Meng L, et al. Ultrasound had high accuracy in measuring hip joint capsule thickness. BMC Musculoskelet Disord. 2024;25(1):101. 10.1186/s12891-024-07228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sahr ME, Endo Y, Sink EL, Miller TT. Dynamic ultrasound assessment of hip instability and anterior and posterior hip impingement. Skeletal Radiol. 2023;52(7):1385–93. 10.1007/s00256-022-04264-6. [DOI] [PubMed] [Google Scholar]
- 34.Larkin B, van Holsbeeck M, Koueiter D, Zaltz I. What is the impingement-free range of motion of the asymptomatic hip in young adult males? Clin Orthop Relat Res. 2015;473(4):1284–8. 10.1007/s11999-014-4072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahan MC, Yu CC, Shields R, van Holsbeeck M, Zaltz I. Impingement-free hip flexion in asymptomatic young adult women. J Bone Joint Surg Am. 2020;102(Suppl 2):22–6. 10.2106/jbjs.19.01088. [DOI] [PubMed] [Google Scholar]
- 36.Safran MR. Microinstability of the hip-gaining Acceptance. J Am Acad Orthop Surg. 2019;27(1):12–22. 10.5435/jaaos-d-17-00664. [DOI] [PubMed] [Google Scholar]
- 37.d’Hemecourt PA, Sugimoto D, McKee-Proctor M, Zwicker RL, Jackson SS, Novais EN, et al. Can dynamic Ultrasonography of the hip reliably assess anterior femoral head translation? Clin Orthop Relat Res. 2019;477(5):1086–98. 10.1097/corr.0000000000000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott CP, d’Hemecourt PA, Miller PE, Sugimoto D, Jackson SS, Kobelski GP, et al. Femoroacetabular translation in female athletes and dancers assessed by dynamic hip ultrasonography. BMJ Open Sport Exerc Med. 2021;7(4):e001169. 10.1136/bmjsem-2021-001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson S, Whitney KE, Lanois CJ, Yen YM, Owen M, d’Hemecourt P. Ultrasound Observation of Hip Translational Motion in adolescent dancers. J Dance Med Sci. 2021;25(2):105–9. 10.12678/1089-313X.061521e. [DOI] [PubMed] [Google Scholar]
- 40.Le HM, d’Hemecourt PA, Jackson SS, Whitney KE, Miller PE, Millis MB, et al. Protocol and validity testing of femoroacetabular posterior translation with dynamic hip ultrasonography. Skeletal Radiol. 2024;53(7):1287–93. 10.1007/s00256-024-04560-3. [DOI] [PubMed] [Google Scholar]
- 41.Finnoff JT, Johnson AC, Hollman JH. Can Ultrasound accurately assess Ischiofemoral Space dimensions? A validation study. Pm r. 2017;9(4):392–7. 10.1016/j.pmrj.2016.06.024. [DOI] [PubMed] [Google Scholar]
- 42.Lu B, Deng H, Chen B, Zhao J. The accuracy assessment of ultrasound for the diagnosis of ischiofemoral space - A validation study. J Xray Sci Technol. 2019;27(4):605–14. 10.3233/xst-180482. [DOI] [PubMed] [Google Scholar]
- 43.Wu WT, Chang KV, Mezian K, Naňka O, Ricci V, Chang HC, et al. Ischiofemoral Impingement Syndrome: Clinical and Imaging/Guidance issues with Special Focus on Ultrasonography. Diagnostics (Basel). 2022;13(1). 10.3390/diagnostics13010139. [DOI] [PMC free article] [PubMed]
- 44.Kim DH, Yoon DM, Yoon KB. Ultrasound-guided Quadratus Femoris muscle injection in patients with Lower Buttock Pain: Novel Ultrasound-guided Approach and Clinical Effectiveness. Pain Physician. 2016;19(6):E863–70. [PubMed] [Google Scholar]
- 45.Backer MW, Lee KS, Blankenbaker DG, Kijowski R, Keene JS. Correlation of ultrasound-guided corticosteroid injection of the quadratus femoris with MRI findings of ischiofemoral impingement. AJR Am J Roentgenol. 2014;203(3):589–93. 10.2214/ajr.13.12304. [DOI] [PubMed] [Google Scholar]
- 46.Piechota M, Maczuch J, Skupiński J, Kukawska-Sysio K, Wawrzynek W. Internal snapping hip syndrome in dynamic ultrasonography. J Ultrason. 2016;16(66):296–303. 10.15557/JoU.2016.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewis CL. Extra-articular snapping hip: a Literature Review. Sports Health. 2010;2(3):186–90. 10.1177/1941738109357298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bureau NJ. Sonographic evaluation of snapping hip syndrome. J Ultrasound Med. 2013;32(6):895–900. 10.7863/ultra.32.6.895. [DOI] [PubMed] [Google Scholar]
- 49.Hua Y, Yang Y, Chen S, Wang Y, Li Y, Chen J, et al. Ultrasound-guided establishment of hip arthroscopy portals. Arthroscopy. 2009;25(12):1491–5. 10.1016/j.arthro.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 50.Weinrauch P, Kermeci S. Ultrasound-assisted hip arthroscopy. Arthrosc Tech. 2014;3(2):e255–9. 10.1016/j.eats.2013.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keough T, Wilson D, Wong I. Ultrasound-guided Portal Placement for Hip Arthroscopy. Arthrosc Tech. 2016;5(4):e851–6. 10.1016/j.eats.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gordey E, Wong I. Comparison of complications in X-Ray Versus Ultrasound-guided hip arthroscopy. Arthroscopy. 2022;38(3):802–7. 10.1016/j.arthro.2021.06.029. [DOI] [PubMed] [Google Scholar]
- 53.Trasolini NA, Sivasundaram L, Rice MW, Gursoy S, Clapp IM, Alter TD, et al. Ultrasound can determine joint distraction during hip arthroscopy but fluoroscopic-guided Portal Placement is Superior. Arthrosc Sports Med Rehabil. 2022;4(3):e1083–9. 10.1016/j.asmr.2022.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaplan DJ, Fenn TW, Larson JH, Nho SJ. Intraoperative use of Ultrasound for assessing Cam Deformity and Cam Resection. Arthrosc Tech. 2023;12(5):e729–35. 10.1016/j.eats.2023.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Clapp IM, Alter TD, Sivasundaram L, Gursoy S, Perry AK, Nho SJ. Ultrasound demonstrates potential in identifying proximal femoral morphology before and after Cam Resection: a cadaveric study. Arthroscopy. 2023;39(3):751–e72. 10.1016/j.arthro.2022.10.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.