Abstract
Purpose of Review
As the field of hip preservation evolves, the diagnosis of borderline dysplasia (defined as a lateral center edge angle between 18°-25°) has shown itself to be one of the more challenging diagnoses to treat. As the nuances of acetabular coverage have come to light, the question of whether borderline hip dysplasia is best treated with isolated hip arthroscopy, periacetabular osteotomy, or whether a combined procedure is best, is now top of mind. The goal of these procedures is to not only improve patient symptoms, but to correct underlying pathology and ideally slow the development of hip osteoarthritis. The purpose of this review is to summarize the recent literature and clinical findings regarding both isolated hip arthroscopy and periacetabular osteotomy in the surgical management of borderline hip dysplasia.
Recent Findings
Current research demonstrates improved postoperative clinical outcome scores for both patients who had isolated hip arthroscopy in the setting of borderline hip dysplasia and for those patients who underwent periacetabular osteotomy. Mid-term outcomes for patients in both groups have showed low rates of conversion to total hip arthroplasty.
Summary
No gold standard in the surgical management of borderline hip arthroscopy exists. Improved clinical outcomes have been seen postoperatively in patients who undergo hip arthroscopy and in patients who undergo periacetabular osteotomy. Successful clinical outcomes seem to rely on treatment of the underlying clinical pathology and are largely based on the appropriate surgical indications and appropriate surgical techniques. Surgical decision making in this patient population should be individualized based on a comprehensive evaluation of the patient.
Keywords: Borderline hip dysplasia, Hip arthroscopy, Periacetabular osteotomy, Hip preservation
Introduction
Hip dysplasia remains a growing interest in orthopedics and is now recognized as a common cause of hip pain and dysfunction as well as precursor to the development of osteoarthritis [1–3]. Hip dysplasia is defined by an acetabulum that is deficient in shape and orientation with decreased depth. This deficiency leads to poor coverage of the femoral head, relative lateralization of the hip center of rotation and a smaller contact area between the femoral head and dysplastic acetabulum. In the setting of acetabular hip dysplasia, an asymmetric concentration of force is distributed across the hip joint and can lead to secondary articular cartilage and labral damage [3]. Among patients with only mild degenerative changes, those with hip dysplasia have a higher risk of progression of degeneration and higher rates of total hip arthroplasty at both 10 and 20 years when compared to patients with isolated femoroacetabular impingement or normal hip morphology [4]. The prevalence of hip dysplasia in asymptomatic patients has been reported in the literature anywhere from 3.6 to 12.8% depending on the radiographic indexes used [5, 6]. The prevalence of hip dysplasia in those presenting with hip pain has been reported as 8.4% and the overall age- and sex-adjusted annual incidence of hip dysplasia diagnosis has been reported as high as 12.7 per 100,000 person-years [5]. Because hip dysplasia is a common source of hip pain and is present in 20–40% of patients with hip osteoarthritis [1–3, 5], diagnosing and intervening on these patients early to prevent the development of osteoarthritis is an emerging area of research. As a growing body of evidence supports that intervention may result in hip preservation, the expansion of the field of hip preservation has mirrored our increased understanding, interest and ability to treat this patient population.
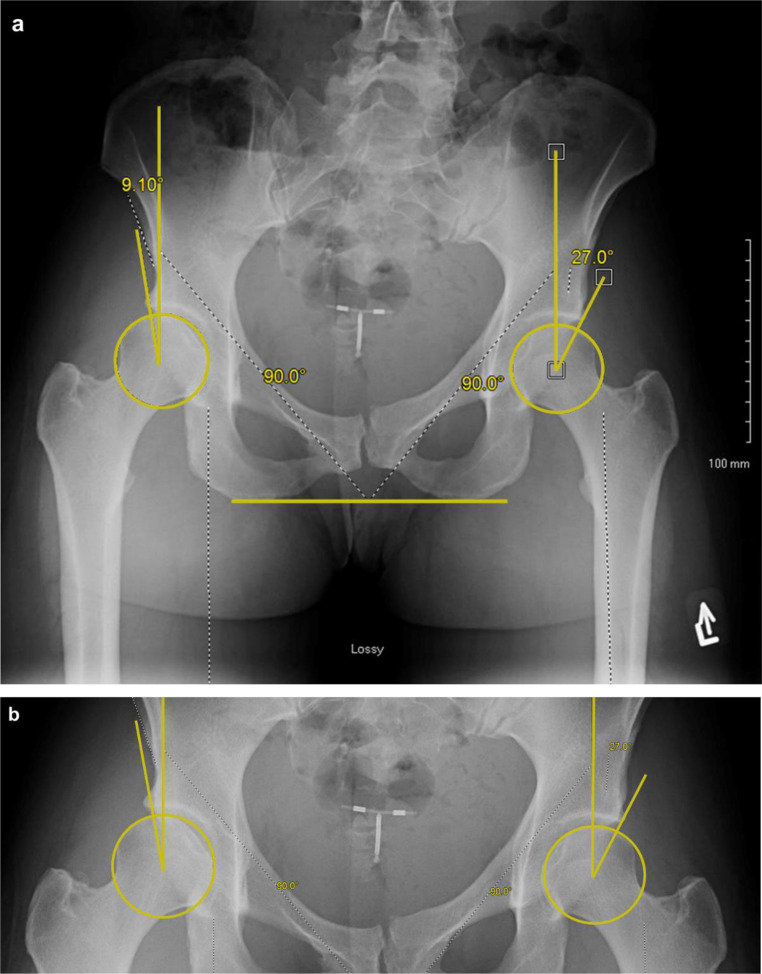
The current standard definition of hip dysplasia is based on the radiographic lateral center edge angle (LCEA). Those with a LCEA < 25° are defined as abnormal and those with an LCEA > 25° are defined as normal (Fig 1) [7, 8]. The term “borderline hip dysplasia” was first described by Wiberg in 1939, and typically refers to a LCEA that is between 18°-25°, though some publications describe it as an LCEA between 20°-25° [9]. For the purpose of this review, we will define borderline hip dysplasia as an LCEA of 18°-25° [10]. The LCEA has been shown to be a reliable radiographic parameter and is the most commonly used measurement within orthopedics [11]. The surgical management for those hips defined as dysplastic (LCEA < 18°) is a periacetabular osteotomy. In this population, arthroscopy alone in the setting of frank hip dysplasia is not recommended, as the chondral and labral pathology in this setting is a sequelae of the underlying abnormal bony morphology [12, 13]. Additionally, isolated arthroscopy with acetabular rim resection for pincer-type impingement in the setting of hip dysplasia can result in iatrogenic instability of the hip and further chondral and labral degeneration [14]. Violation of the hip capsule during hip arthroscopy can further destabilize the dysplastic hip. Periacetabular osteotomy in the setting of hip dysplasia (LCEA < 18°) has been shown to have high survival rates and patient satisfaction outcomes and therefore is the surgical treatment of choice in this patient population [12–14]. In hips with adequate acetabular coverage (LCEA > 25°) that have been identified as having intra-articular pathology or femoroacetabular impingement (FAI), the surgical treatment often consists of isolated hip arthroscopy to address any intra-articular pathology (chondral damage, labral pathology) with concomitant osteoplasty if indicated. In this setting, isolated hip arthroscopy has been shown to have excellent clinical outcomes [15–17]. However, a surgical indications “gray area” exists when acetabular coverage is not “normal” (LCEA < 25°) but is not “bad enough” to be called frank hip dysplasia (LCEA < 18°). Currently, no standard protocol exists for treatment of borderline hip dysplasia (LCEA between 18°-25°) and the surgical management of these patients remains quite varied.
Fig. 1.
Preoperative Lateral Center-Edge Angle of Wiberg Measurements. Legend: The Lateral Center-Edge Angle (LCEA) measured on the right and left hip on a standing anteroposterior pelvis radiograph. A perfect circle is drawn around the femoral head, and a Cobb angle is drawn creating a 90° angle between a line drawn across the ischium and a line drawn into the center of the femoral head (a). Then an angle is created between the vertical line in the center of the femoral head the lateral edge of the sourcil. Care must be taken to draw the line to the lateral most aspect of the sourcil to not include any upturn of the sourcil (b)
The primary objective of this paper is to review and summarize current literature regarding the surgical treatment options of borderline hip dysplasia and their respective postoperative outcomes. Understanding these options can help orthopedic surgeons make informed decisions best tailored to the individual patient in the management of borderline hip dysplasia.
Isolated Hip Arthroscopy in Borderline Dysplasia
Hip arthroscopy is a growing area of interest in orthopedic sports medicine. The number of hip arthroscopies performed each year has exponentially increased over the past 20 years [5]. The incidence of hip arthroscopy in patients with FAI and labral pathology has been noted to increase as much as 85% between 2011 and 2018 [18]. In the absence of hip dysplasia, hip arthroscopy has been shown to have excellent outcomes in the setting of FAI or intra-articular pathology [16, 17, 19]. However, the role of hip arthroscopy alone in the setting of borderline hip dysplasia, as defined by the LCEA between 18°-25°, is still being evaluated. Multiple prior studies have attempted to clarify the outcomes of this patient population and more recent studies have begun to show favorable results.
Recent case series have shown improved short term and midterm clinical and patient reported outcomes measures (PROMs) when comparing preoperative and postoperative scores for those patients undergoing hip arthroscopy in the setting of borderline hip dysplasia. Yang et al. reviewed the general outcomes of hip arthroscopy in the borderline hip dysplasia (LCEA 20°-25°) population with 83.1% of patients meeting the calculated minimal clinical important difference (MCID) threshold for all patient reported outcomes and 57.1% meeting the threshold for Patient Acceptable Symptomatic State (PASS) at a minimum of 2 years follow up [20]. Additionally they found that higher preoperative alpha angle was strongly associated with improved patient reported outcomes [20], suggesting that CAM-type impingement may have been the predominant generator of the pathomechanics in this population. Patients with a preoperative Tönnis angle of > 15° were not included in an attempt to exclude concomitant hip instability. Important to note in this study, all hip arthroscopies were performed by a single senior author utilizing an interportal capsulotomy through which labral and chondrolabral pathology was addressed including labral repair via suture anchors or labral reconstruction. All patients also underwent femoroplasty and any additional extraarticular pathologies were addressed, including ischiofemoral impingement and subspine impingement if applicable. Lastly, it is important to note that the capsulotomy in this study was closed with interrupted sutures in all patients [19]. A case series by Domb et al. included patients with borderline hip dysplasia (LCEA 18°-25°), intra-articular hip pathology and minimum 5 year follow up who underwent hip arthroscopy with labral preservation (repair vs. debridement) and capsular plication [21]. In this study all patients underwent capsulotomy, labral repair vs. debridement, and any additional necessary procedures in the central compartment including femoroplasty if CAM deformity was present. All patients then underwent capsular plication and closure. Importantly, all surgeries were performed by a single, high-volume hip arthroscopy surgeon. They found that the mean Modified Harris Hip Score (mHHS), Non-Arthritic Hip Score (NAHS), Hip Outcome Score Sport-Specific Subscale (HOS-SSS) and the visual analog scale (VAS) score for pain all significantly improved postoperatively when compared to preoperatively. They did however note that 19% of their patients (n = 4) underwent a secondary arthroscopic procedure [21]. Notably, the limitations of this study design include the lack of control group to which these results can be compared.
When comparing the outcomes between the borderline hip dysplasia population and those with normal hip morphology, favorable results of hip arthroscopy alone have also been shown in recent studies. A study by Cvetanovich et al. published in 2017 retrospectively reviewed PROMs in the femoroacetabular impingement (FAI) population in those with borderline dysplastic hips (LCEA 18°-25°) and normal hip morphology (LCEA 25.1°-40°) who underwent isolated hip arthroscopy [22]. All patients had negative instability tests on clinical exam. These patients underwent hip arthroscopy, capsule closure, labral repair (> 90% of both groups), as well as bony work including femoroplasty and acetabuloplasty as indicated [22]. They found no significant difference in groups in final PROM scores, score improvements (postoperative-preoperative scores), or percentage of patients experiencing clinically significant improvements at minimum 2 year follow-up (mean 2.6 ± 0.6 years). There was no difference in the percentage of patients in each group meeting the MCID and PASS criteria. Additionally, both groups demonstrated significant improvements in all PROM scores (minimum 2 year follow up, at an average of 2.6 ± 0.6 years follow-up). They did not find differences in the rates of subsequent surgery between the normal coverage and borderline dysplastic groups as only one patient in the borderline dysplastic group underwent a second surgery in their follow up window (revision hip arthroscopy) [22]. Furthermore, Matsuda et al. compared the preoperative and postoperative International Hip Outcome Tool (iHOT-12) scores between patients who underwent hip arthroscopy in the setting of low (borderline dysplasia), normal and high (global pincer FAI) lateral acetabular coverage [23]. These patients were classified into three groups postoperative based on preoperative LCEA (borderline < 25°, normal 25.1°-38.9° and pincer > 39°). They found a significant improvement in preoperative and postoperative iHOT-12 scores in all three groups. The only statistical difference between groups was lower prevalence of acetabuloplasty in the borderline dysplasia group. They did not find a significant effect on acetabular coverage on the incidence of revision arthroscopy or conversion to total hip arthroplasty [23]. Lastly, Beck et al. described midterm outcomes (minimum 5 year follow up) of hip arthroscopy for FAI between patients with borderline hip dysplasia (LCEA 20°-25°) and normal acetabular coverage (LCEA 25°-40°) [24]. Both groups had statistically significant increases in PROM scores over the 5 year period; although, there was no significant difference between groups. There was no statistical difference in the frequency in which patients in either group achieved PASS or MCID. All patients in this cohort underwent capsular closure as part of their arthroscopic surgery. In the borderline hip dysplasia group, female sex, higher LCEA, being physically active and running for exercise were preoperative predictors of achieving clinical success at 5 years [24].
In all recent studies noted above, capsular closure in the form of repair or plication was performed. Given the above studies have found positive clinical results following hip arthroscopy in the borderline dysplastic patient, the importance of capsular closure can be inferred and should not be overlooked. In addition, only two of the above studies accounted for additional preoperative clinical or radiographic signs of hip instability, including the Tönnis angle, femoro-epiphyseal acetabular roof (FEAR) index, Beighton score, or clinical exam findings of instability. Hip instability in the setting of borderline hip dysplasia is a potential confounding factor which cannot be addressed with hip arthroscopy alone, therefore this is an important factor to keep in mind when critically evaluating these studies. Further evaluation of hip instability will be addressed later on in this review. Additionally, it should be emphasized that the hip arthroscopy surgeries in the above studies were performed by high volume, experienced hip arthroscopists. This should be considered by readers when evaluating the outcomes data, as hip arthroscopy is known to be a technically challenging procedure with a steep learning curve so the published results may not be generalizable to the general orthopedic population. Despite the recent favorable outcomes regarding the role of isolated hip arthroscopy in the borderline dysplastic hip population, there is limited data regarding long term outcomes.
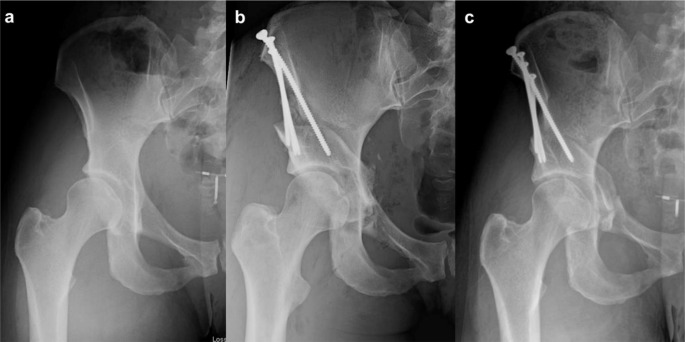
Periacetabular Osteotomy in Borderline Dysplasia
Periacetabular osteotomy (PAO) can be performed with or without hip arthroscopy for the treatment of symptomatic hip dysplasia in skeletally mature patients with intact articular cartilage [25–28]. The current widely utilized PAO was first described by Dr. Reinhold Ganz in 1988. Since then, PAO has evolved and has demonstrated durable outcomes in patients with hip dysplasia (Fig. 2). Clinical outcomes following PAO have been increasingly reported, particularly within the United States and Europe [29]. Long-term data survivorship has been reported as high as 92% at 15 years and there is optimism for further improvement in outcomes as advancements in surgical techniques are developed and indications for PAO are refined [14, 30]. Early studies with long-term follow-up have been reported on patients with LCEA angles typically below 20°-25° degrees, leaving a paucity of data for those who have borderline hip dysplasia (with LCEA angles between 18°-25° degrees) and are at-risk for future arthritis or who have failed hip arthroscopy [31–37]. Therefore, there has been increased examination of the role for PAO within borderline hip dysplasia populations.
Fig. 2.
Preoperative and Postoperative Radiographs Following Periacetabular Osteotomy. Legend: Anteroposterior radiographs of the right hip in a patient who underwent Periacetabular Osteotomy (PAO) in the setting of acetabular dysplasia (lateral center edge angle measured 9.1° preoperatively). Preoperative (a), two weeks postoperative (b) and one-year postoperative radiographs demonstrating healed PAO (c)
Preoperative Assessment
The indication for PAO involves a thorough clinical and radiographic assessment to assess whether the patient’s symptoms are driven by structural instability or FAI and microinstability as pinpointing the driving etiology of a patient’s symptoms is of utmost importance when determining the appropriate surgical management. Additionally, paramount to any surgical decision making involves the patient’s goals of care and an appropriate trial of conservative management including physical therapy, activity modification, and others. On clinical exam, instability can be assessed by several maneuvers including hip abduction-hyperextension-external rotation (AB-HEER), hyperextension-external rotation (HEER), the prone apprehension relocation test (PART), and the prone instability test [38–41]. Of these tests, the AB-HEER has been shown in one study to have the highest sensitivity for diagnosing hip instability (80.6%), while the prone instability test has been shown to have a specificity as high as 98% [41]. It should be noted however that there is no one gold standard clinical exam for diagnosing hip instability, and multiple provocative tests have been described, and should be used in combination (Table 1) [39]. In concert with physical examination, many radiographic parameters exist to assess the borderline dysplastic hip in addition to LCEA. Symptoms driven by instability may be suggested by hip internal rotation in flexion > 20°, radiographic femoro-epiphyseal acetabular roof (FEAR) index of >5, anterior center-edge angle of < 20°, and an acetabular inclination of > 10° [42–44]. However, cutoffs suggestive of instability, such as with FEAR, continue to change and radiographic markers have recently been shown to poorly correlate with anterior acetabular coverage seen on low-dose CT [43, 45, 46]. In addition to a comprehensive clinical exam, our institution’s hip-preservation protocols include preoperative radiographs (standing anteroposterior, false profile, 45° Dunn lateral, and in patients considered for PAO, a Von Rosen view), non-contrast hip magnetic resonance imaging in the setting of a native hip (MR arthrogram if the patient has had prior surgery) and low-dose 3-dimensional computed tomography in all patients as part of the standard preoperative work-up [28].
Table 1.
Physical Examination Maneuvers to Assess Hip Instability
| Summary of Tests to Evaluate Hip Instability | Acronym | Patient Position | Description |
|---|---|---|---|
| Abduction-extension-external rotation test | AB-HEER | Lateral |
Abduct the hip to 30 and externally rotate. Place pressure on posterior aspect of greater trochanter. Extend the leg from 10 of flexion to full extension while placing anterior force through greater trochanter. Positive test reproduces the patient’s symptoms |
| Anterior apprehension test (also known as hyperextension-external rotation test) | HEER | Supine |
Place the buttock of side being examined on the edge of table. Extend and externally rotate the affected lower extremity while keeping the contralateral limb in flexion. Positive test reproduces anterior hip pain |
| Axial distraction test | Supine |
Place patient’s hip and knee in 30o of flexion. While examining patient, keep your knee beneath affected thigh, against the patient’s ischium. Axial distraction of hip results in positive test if patient’s pain or apprehension is replicated, or whether hip toggles. |
|
| Log roll test (also known as the dial test) | Supine |
Examiner internally rotates foot past neutral and releases foot. Foot will fall into ER; if ER is greater than contralateral side, this is suggestive of anterior capsular laxity (especially if foot table angle is < 20) and is a positive test. |
|
| Posterior apprehension test | Supine |
Place the affected hip in 90° flexion. Provide additional adduction and internal rotation of affected hip. Lastly, apply posterior force. Test is positive if pain or apprehension is reproduced. |
|
| Prone Apprehension Relocation Test | PART | Prone |
Place the patient prone on the examination table with the affected hip held in extension approximately 10° to 15° and abducted approximately 10° from midline. Support the patient’s bent knee and pushes downward on the femur while supporting the knee. A positive test replicates the patient’s anterior hip pain. |
| Prone external rotation test | Prone ER test | Prone |
Place the affected hip in maximal external rotation. Place anterior pressure on the posterior greater trochanter in an attempt to translate the femoral head anteriorly. Positive test replicates patient’s symptoms. |
Clinical Outcomes Following Periacetabular Osteotomy
Current data regarding PAO outcomes in those with borderline hip dysplasia show promising short and mid-term clinical benefit. McClincy et al., in 2019, reported on 39 patients who underwent PAO for patients with a LCEA between 18°-25° degrees with symptoms associated with instability [47]. The cohort was primarily female patients (n = 37, 95%) with a mean LCEA of 20°, preoperative Tönnis grade 0, and osteoplasty of the anteroinferior iliac spine was performed concomitantly in eight (20%) of patients. At a mean follow-up of 2.2 years, no patients underwent subsequent arthroplasty or revision surgery, while four patients (10%) had a postoperative mHHS score < 70 and were considered clinical failures. There was a mean improvement seen in all patient reported outcomes examined (mHHS, HOOS, UCLA activity score, SF-12), although clinically significant outcomes were not reported [47]. Similarly, Livermore et al., studied 20 patients who underwent PAO for symptomatic instability in the setting of borderline hip dysplasia (LCEA 18°-25°). At a mean 5-year follow-up, no patients met criteria for failure which was defined as conversion to total hip arthroplasty [48]. Additionally, no patients met criteria for clinical failure, as defined by Patient Reported Outcomes Measurement Information System (PROMIS) outcome measures physical function computerized adaptive test score less than 40. Achievement of clinically significant outcomes were not reported in this study, however, which limits comparisons to aforementioned hip arthroscopy studies [48].
In the largest study to date of patients undergoing PAO in patients with borderline hip dysplasia (LCEA 18°-25°), Nepple and colleagues reported on 186 hips with a mean LCEA of 20.7° at a mean 3.3 years follow-up [44]. Thirty hips had undergone a previous hip arthroscopy most commonly for labral repair (73.1%) or femoral osteoplasty (38.5%). A concurrent procedure was performed in 88.7% of those undergoing PAO with 69.9% of these hips undergoing an arthroscopy immediately prior to their PAO. Three patients underwent subsequent hip arthroscopy following PAO (1.6%) for persistent symptoms. An additional twelve hips failed to achieve either MCID or PASS for the Modified Harris Hip Score (mHHS), thus for an overall clinical failure rate of 8% (n = 15, including both reoperations and failure to achieve MCID/PASS). However, those who had undergone a prior hip arthroscopy demonstrated inferior postoperative PROM scores and more-commonly met criteria for clinical failure (23% and 5% in those with and without prior arthroscopy, respectively). While this represents a large cohort with promising clinical outcomes, no control group was utilized and this study lacked long-term follow-up [44].
While there are limited studies on the use of PAO in the borderline dysplastic hip population, recent studies have shown promising clinical results. Additional mid-term and long-term studies are warranted to further examine clinically significant outcomes, reoperations, and conversion to arthroplasty following this procedure.
PAO in the Setting of Prior Hip Arthroscopy
As the debate between the appropriate first line treatment for borderline hip dysplasia continues, it is worthwhile to examine the characteristics and outcomes of those who fail initial hip arthroscopy and subsequently undergo PAO. Understanding this data may provide insight into selection of first line management in future patients and implications of each. When examining the patient characteristics of hip arthroscopy failures in the setting of hip dysplasia, Ross et al. reported on 30 patients in the Academic Network for Conservational Hip Outcomes Research (ANCHOR) Study Group who failed hip arthroscopy and underwent subsequent PAO an average of 22 months after their index arthroscopy [49]. A preoperative diagnosis of borderline hip dysplasia (LCEA 20°-25°) and hip dysplasia (LCEA < 20°) was present in 27% and 67% of patients, respectively [49]. Importantly, they also noted that 93% of these patients had increased acetabular inclination (> 10°) and 70% had anterior center edge angle of < 20°. All 30 patients (100%) had at least one radiographic measurement indicative of acetabular dysplasia reinforcing the need for a comprehensive preoperative assessment of this patient population as LCEA alone may not be adequate when assessing dysplasia. Additionally, in the patient population who have failed a hip arthroscopy and subsequently undergo a PAO for definitive treatment of hip dysplasia, the outcomes may not be as good as in those patients who have a PAO as the index surgery [10, 50, 51]. Ricciardi and colleagues compared PROMs, reoperations, and complications between patients undergoing symptomatic hip dysplasia with (N = 25 hips) or without (N = 85 hips) prior hip arthroscopy [51]. The indications for primary hip arthroscopy were heterogeneous given the research institution is a tertiary referral center, but importantly no patients had known iatrogenic dysplasia secondary to over resection of the acetabular rim during their index arthroscopy. Patients underwent PAO if they had acetabular dysplasia (LCEA < 25°), minimal radiographic osteoarthritis, and failed nonoperative management. The LCEA of those with a prior arthroscopy (median 22°; range 17°-32°) was not different when compared to patients without prior surgery (median 18°; range 9°-21°) [51]. While there were no differences in reoperations or complications, those who underwent a prior hip arthroscopy had inferior 6-month and 1-year PROMs (HOS-activities of daily living, HOS-sport, iHOT-33, and mHHS). Novais et al. similarly performed a retrospective cohort using the ANCHOR database comparing postoperative PROMs and radiographic outcomes in patients who underwent PAO with (N = 52) or without (N = 104) having undergone a prior hip arthroscopy [50]. Patients were included if they underwent PAO for hip dysplasia (LCEA < 25° or acetabular index of Tonnis greater than 10°), while indications for hip arthroscopy were heterogeneous. Baseline and 1-year postoperative PROMs were decreased in patients who had previously failed hip arthroscopy when compared to those without a prior surgery [50]. However, the magnitude of change in PROMs as well as LCEA, ACEA, and acetabular index were not significantly different between cohorts.
The above studies highlight the importance of a thorough discussion and evaluation in this patient population as although an index isolated hip arthroscopy procedure may be a smaller procedure with quicker recovery as compared to PAO, those patients undergoing a subsequent PAO following hip arthroscopy may have inferior outcomes.
Periacetabular Osteotomy vs. Hip Arthroscopy: A Direct Comparison
While there are no current randomized control trials comparing PAO with hip arthroscopy, several retrospective cohort studies exist [52, 53]. Grammatopoulos et al. compared clinical outcomes at short-term follow-up in patients with borderline hip dysplasia (defined as LCEA 20°-25° and acetabular index 10°-15°) who underwent either PAO-only (n = 42), isolated hip arthroscopy (n = 127), or combined PAO and an intra-articular treatment (open or arthroscopic, n = 122) [53]. It should be noted that several demographic and radiographic differences were found between groups. Those undergoing isolated hip arthroscopy tended to be older (p < .001), male (p < .001), had not had a previous procedure (p = .02), had a higher Tonnis grade (p < .001), and had higher baseline HOOS scores (p = .02). Complications, reoperations, and final postoperative patient-reported outcomes were not statistically different between groups. Changes in SF-12 scores tended to be smaller in those undergoing isolated PAO (4 ± 19) when compared to isolated hip arthroscopy (10 ± 16) or combined PAO and an intra-articular procedure (12 ± 15; p = .02). It should also be noted that indications for PAO versus hip arthroscopy were not discussed within this abstract and thus is a significant limitation to the study which is in addition to its short-term follow-up of 1-year [53].
More recently, Andronic and colleagues compared clinical outcomes in those undergoing PAO and isolated hip arthroscopy in a propensity-matched retrospective cohort with 5-year minimum follow-up [52]. Defining borderline hip dysplasia as an LCEA of 18°-25°, Andronic et al. successful matched 28 and 49 patients undergoing PAO or hip arthroscopy, respectively, by age, sex, body mass index, and Tonnis grade (all p ≥ .241). Labral debridement and repair were performed in 8 and 41 hips, with all patients undergoing capsular plication. Those undergoing PAO tended to have smaller LCEA (21.1° vs. 22.6°, p = .002) and alpha angle (47.1 vs. 58.0, p < .001), and an increased FEAR index (0.0 vs. -3.6, p = .003) when compared to the isolated hip arthroscopy cohort. Postoperative mHHS scores as well as achievement of MCID, PASS and maximum outcome improvement satisfaction threshold did not significantly differ between groups. Including seven patients who underwent hardware removal in the PAO cohort, those undergoing isolated hip arthroscopy had fewer reoperations (4 vs. 8, p = .024). One patient in the hip arthroscopy cohort underwent subsequent THA, while no patients undergoing PAO underwent THA (p > .999). While this study had mid-term follow-up, was adequately powered, and matched for important preoperative variables, it had limited discussion regarding clinical indications for patients who underwent PAO when compared to hip arthroscopy [52]. Larger studies, with long-term follow-up are warranted to further evaluate the differences in clinically significant outcomes, reoperations and conversion to THA in those undergoing isolated hip arthroscopy versus PAO.
Conclusion
As hip preservation is commonly seen as a “final frontier” within orthopedics, so is its respective pathology. Borderline hip dysplasia, or “transitional acetabular coverage,” remains a controversial pathology without a clear, gold-standard treatment. Symptomatic patients who have failed conservative management in the setting of borderline hip dysplasia may have successful short and mid-term outcomes following hip arthroscopy, periacetabular osteotomy or both. However, successful and durable outcomes are obtained by treating the etiology underlying individual patient’s pain – whether due to dysplasia, femoroacetabular impingement, intra-articular pathology, instability, or a combination. Thus, a comprehensive assessment of a patient’s history, physical examination, and imaging are warranted to determine whether an individual patient with borderline hip dysplasia is best treated with isolated hip arthroscopy or periacetabular osteotomy. Additional studies directly comparing these procedures with long-term follow-up are warranted.
Author Contributions
EW and KW wrote the main manuscript text and prepared figures. AS was involved in manuscript and figure conception, reviewe and editing.
Funding
No funding was received for the development of this manuscript.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing Interests
Andrea Spiker, MD is unpaid for: American Orthopaedic Association: Board or committee memberAmerican Orthopaedic Society for Sports Medicine: Board or committee member Arthroscopy: Editorial or governing board. Arthroscopy Association of North America: Board or committee member Video Journal of Sports Medicine/American Journal of Sports Medicine: Editorial or governing board Andrea Spiker is paid consultant for Stryker.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gala L, Clohisy JC, Beauĺe PE. Hip dysplasia in the Young Adult. J Bone Joint Surg Am. 2016;98:63–73. [DOI] [PubMed] [Google Scholar]
- 2.Rankin AT, Bleakley CM, Cullen M. Hip Joint Pathology as a leading cause of Groin Pain in the Sporting Population: a 6-Year review of 894 cases. Am J Sports Med. 2015;43:1698–703. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Dobson MA, Robison JF, Warth LC, Zheng J, Liu SS, Yehyawi TM, Callaghan JJ. Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Joint Surg Am. 2011;93(Suppl 2):3–9. [DOI] [PubMed] [Google Scholar]
- 4.Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. The John Charnley Award: redefining the natural history of Osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaPrade MD, Melugin HP, Hale RF, Leland DP, Bernard CD, Sierra RJ, Trousdale RT, Levy BA, Krych AJ. (2021) Incidence of Hip Dysplasia Diagnosis in Young Patients With Hip Pain: A Geographic Population Cohort Analysis. Orthop J Sport Med. 2021; Mar 5;9(3). [DOI] [PMC free article] [PubMed]
- 6.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–9. [DOI] [PubMed] [Google Scholar]
- 7.Wilkin GP, Ibrahim MM, Smit KM, Beaulé PE. A contemporary definition of hip dysplasia and structural instability: toward a Comprehensive classification for Acetabular Dysplasia. J Arthroplasty. 2017;32:S20–7. [DOI] [PubMed] [Google Scholar]
- 8.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the Hip Joint with Special references to the complication of Osteoarthritis. Acta Chir Scand. 1939.
- 10.Nepple JJ. Editorial Commentary: at the intersection of Borderline Dysplasia and Femoroacetabular Impingement-which Way should we turn? Arthroscopy. 2020;36:1185–8. Commentary that discusses operative management in those with borderline hip dysplasia. [DOI] [PubMed]
- 11.Carreira DS, Emmons BR. (2019) The Reliability of Commonly Used Radiographic Parameters in the Evaluation of the Pre-Arthritic Hip: A Systematic Review. JBJS Rev. 2019; Feb;7(2):e3. [DOI] [PubMed]
- 12.Parvizi J, Bican O, Bender B, Mortazavi SMJ, Purtill JJ, Erickson J, Peters C. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24:110–3. [DOI] [PubMed] [Google Scholar]
- 13.Kain MSH, Novais EN, Vallim C, Millis MB, Kim YJ. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg Am. 2011;93(Suppl 2):57–61. [DOI] [PubMed] [Google Scholar]
- 14.Wells J, Schoenecker P, Duncan S, Goss CW, Thomason K, Clohisy JC. Intermediate-term hip survivorship and patient-reported outcomes of Periacetabular Osteotomy: the Washington University experience. J Bone Joint Surg Am. 2018;100:218–25. [DOI] [PubMed] [Google Scholar]
- 15.Clohisy JC, Ackerman J, Baca G, et al. Patient-reported outcomes of Periacetabular Osteotomy from the prospective ANCHOR Cohort Study. J Bone Joint Surg Am. 2017;99:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murata Y, Uchida S, Utsunomiya H, Hatakeyama A, Nakamura E, Sakai A. A comparison of clinical outcome between athletes and nonathletes undergoing hip arthroscopy for Femoroacetabular Impingement. Clin J Sport Med. 2017;27:349–56. [DOI] [PubMed] [Google Scholar]
- 17.Kyin C, Maldonado DR, Go CC, Shapira J, Lall AC, Domb BG. Mid- to Long-Term outcomes of Hip Arthroscopy: a systematic review. Arthroscopy. 2021;37:1011–25. [DOI] [PubMed] [Google Scholar]
- 18.Zusmanovich M, Haselman W, Serrano B, Banffy M. The incidence of hip arthroscopy in patients with Femoroacetabular Impingement Syndrome and Labral Pathology increased by 85% between 2011 and 2018 in the United States. Arthroscopy. 2022;38:82–7. [DOI] [PubMed] [Google Scholar]
- 19.Malviya A, Stafford GH, Villar RN. Is hip arthroscopy for femoroacetabular impingement only for athletes? Br J Sports Med. 2012;46:1016–8. [DOI] [PubMed] [Google Scholar]
- 20.Yang F, Zhou Z, Zhang X, Huang H, Ju X, Wang J. Arthroscopy confers favorable clinical outcomes in Asian patients with Borderline Developmental Dysplasia of the hip. Orthop Surg. 2023;15:2393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with Labral Preservation and Capsular Plication in patients with Borderline Hip Dysplasia: Minimum 5-Year patient-reported outcomes. Am J Sports Med. 2018;46:305–13. [DOI] [PubMed] [Google Scholar]
- 22.Cvetanovich GL, Levy DM, Weber AE, Kuhns BD, Mather RC, Salata MJ, Nho SJ. Do patients with Borderline Dysplasia have inferior outcomes after hip arthroscopic surgery for Femoroacetabular Impingement compared with patients with normal Acetabular Coverage? Am J Sports Med. 2017;45:2116–24. [DOI] [PubMed] [Google Scholar]
- 23.Matsuda DK, Kivlan BR, Nho SJ, Wolff AB, Salvo JP, Christoforetti JJ, Ellis TJ, Carreira DS. Arthroscopic outcomes as a function of Acetabular Coverage from a large hip arthroscopy Study Group. Arthroscopy. 2019;35:2338–45. [DOI] [PubMed] [Google Scholar]
- 24.Beck EC, Drager J, Nwachukwu BU, Rasio J, Jan K, Chahla J, Nho SJ. Patients with Borderline Hip Dysplasia achieve clinically significant improvement after arthroscopic femoroacetabular impingement surgery: a Case-Control Study with a minimum 5-Year follow-up. Am J Sports Med. 2020;48:1616–24. [DOI] [PubMed] [Google Scholar]
- 25.Leopold VJ, Hipfl C, Perka C, Hardt S, Becker L. (2023) Periacetabular osteotomy for symptomatic hip dysplasia in middle aged patients: does age alone matter? Arch Orthop Trauma Surg. 2024; Mar;144(3). [DOI] [PMC free article] [PubMed]
- 26.Kamath AF. Bernese periacetabular osteotomy for hip dysplasia: Surgical technique and indications. World J Orthop. 2016;7:280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wyles CC, Vargas JS, Heidenreich MJ, Mara KC, Peters CL, Clohisy JC, Trousdale RT, Sierra RJ. Natural history of the dysplastic hip following modern Periacetabular Osteotomy. J Bone Joint Surg Am. 2019;101:932–8. [DOI] [PubMed] [Google Scholar]
- 28.Spiker AM, Turner EHG, Gans I, Sisel HI, Wiseley BR, Goodspeed DC. Combined hip arthroscopy and Periacetabular Osteotomy (PAO): Technical Focus on Arthroscopically elevating the iliocapsularis and performing the Open PAO. Arthrosc Tech. 2021;10:e2293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wei T, Xiao F, He X, Peng P, He W, He M, Wei Q. A bibliometric analysis and visualization of research trends on periacetabular osteotomy. J hip Preserv Surg. 2023;10:181–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Büchler L, Beck M. Periacetabular osteotomy: a review of Swiss experience. Curr Rev Musculoskelet Med. 2014;7:330–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after Periacetabular Osteotomy survive 30 years with good clinical results, no progression of arthritis, or Conversion to THA. Clin Orthop Relat Res. 2017;475:1154–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–23. [DOI] [PubMed] [Google Scholar]
- 33.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–79. [DOI] [PubMed] [Google Scholar]
- 35.Thomas GER, Palmer AJR, Batra RN, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthr Cartil. 2014;22:1504–10. [DOI] [PubMed] [Google Scholar]
- 36.Hatakeyama A, Utsunomiya H, Nishikino S, Kanezaki S, Matsuda DK, Sakai A, Uchida S. Predictors of poor clinical Outcome after Arthroscopic Labral Preservation, Capsular Plication, and Cam Osteoplasty in the setting of Borderline Hip Dysplasia. Am J Sports Med. 2018;46:135–43. [DOI] [PubMed] [Google Scholar]
- 37.Clohisy JC, Nepple JJ, Larson CM, Zaltz I, Millis M. Persistent structural disease is the most common cause of repeat hip preservation surgery. Clin Orthop Relat Res. 2013;471:3788–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spiker AM, Fabricant PD, Wong AC, Suryavanshi JR, Sink EL. Radiographic and clinical characteristics associated with a positive PART (Prone Apprehension Relocation Test): a new provocative exam to elicit hip instability. J hip Preserv Surg. 2020;7:288–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watchmaker LE, Hetzel SJ, Sink EL, Spiker AM. (2021) Interrater Reliability of the Prone Apprehension Relocation Test. Orthop J Sport Med. 2021; Sep 20;9(9). [DOI] [PMC free article] [PubMed]
- 40.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–8. [DOI] [PubMed] [Google Scholar]
- 41.Hoppe DJ, Truntzer JN, Shapiro LM, Abrams GD, Safran MR. Diagnostic accuracy of 3 physical examination tests in the Assessment of Hip Microinstability. Orthop J Sport Med. 2017; Nov 27;5(11). [DOI] [PMC free article] [PubMed]
- 42.Wyatt M, Weidner J, Pfluger D, Beck M. The Femoro-Epiphyseal Acetabular roof (FEAR) index: a New Measurement Associated with instability in Borderline Hip Dysplasia? Clin Orthop Relat Res. 2017;475:861–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen K, Wu J, Zhang X, Han X, Li T, Xia J, Shen C, Chen X. A Modified Approach to Measuring Femoro-Epiphyseal Acetabular roof (FEAR) index has better intraobserver and interobserver reliability compared with the original FEAR Index. Arthroscopy. 2023. Available online 10.1016/j.arthro.2023.11.024. [DOI] [PubMed] [Google Scholar]
- 44.*Nepple JJ, Parilla FW, Pashos GE, Clohisy JC. Outcomes of Periacetabular Osteotomy for Borderline Acetabular Dysplasia. J Bone Joint Surg Am. 2023;105:137–44. Large retrospective review that presents outcomes following osteotomy in those with borderline hip dysplasia. [DOI] [PubMed]
- 45.Truntzer JN, Hoppe DJ, Shapiro LM, Safran MR. Can the FEAR Index be used to Predict Microinstability in patients undergoing hip arthroscopic surgery? Am J Sports Med. 2019;47:3158–65. [DOI] [PubMed] [Google Scholar]
- 46.Graesser EA, Schwabe MT, Clohisy JC, Nepple JJ. Defining the Borderline dysplastic hip: high variability in Acetabular Coverage and femoral morphology on low-dose computed Tomography. Am J Sports Med. 2023;51:2551–8. [DOI] [PubMed] [Google Scholar]
- 47.McClincy MP, Wylie JD, Kim YJ, Millis MB, Novais EN. Periacetabular Osteotomy improves Pain and function in patients with lateral center-edge Angle between 18° and 25°, but are these hips really Borderline Dysplastic? Clin Orthop Relat Res. 2019;477:1145–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Livermore AT, Anderson LA, Anderson MB, Erickson JA, Peters CL. Correction of mildly dysplastic hips with periacetabular osteotomy demonstrates promising outcomes, achievement of correction goals, and excellent five-year survivorship. Bone Joint J. 2019;101–B:16–22. [DOI] [PubMed] [Google Scholar]
- 49.JR R, JC C. Patient and disease characteristics associated with hip arthroscopy failure in acetabular dysplasia. J Arthroplasty. 2014;29:160–3. [DOI] [PubMed] [Google Scholar]
- 50.Novais EN, Coobs BR, Nepple JJ, et al. Previous failed hip arthroscopy negatively impacts early patient-reported outcomes of the periacetabular osteotomy: an ANCHOR matched Cohort Study. J Hip Preserv Surg. 2018;5:370–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ricciardi BF, Fields KG, Wentzel C, Kelly BT, Sink EL. Early functional outcomes of Periacetabular Osteotomy after failed hip arthroscopic surgery for symptomatic Acetabular Dysplasia. Am J Sports Med. 2017;45(11):2460–7. [DOI] [PubMed] [Google Scholar]
- 52.*Andronic O, Chaharbakhshi EO, Zingg PO, Germann C, Rahm S, Lall AC, Domb BG. No difference in patient-reported outcomes for Periacetabular Osteotomy and Hip Arthroscopy with Capsular Plication in the setting of Borderline Hip Dysplasia: a propensity-matched Multicenter Study with Minimum 5-Year follow-up. Arthrosc J Arthrosc Relat Surg. Mar; 2024;40(3):754–62. Large retrospective review in those who underwent osteotomy in the setting of borderline hip dysplasia. [DOI] [PubMed]
- 53.Grammatopoulos G, Pascual-Garrido C, Nepple J, Larson CM, Bedi A, Beaule P, Clohisy JC, Group A. The Borderline dysplastic hip: arthroscopy or PAO? Orthop J Sports Med. 2018;6(7 suppl4):Jul27. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.