ABSTRACT
Background and Aims
In Africa, telemedicine holds great potential to revolutionize surgical care delivery, especially in areas where access to quality treatment is scarce. Data about the use of these services in African countries is, however, limited. To outline the present issues in surgical care delivery, as well as the significant role of telemedicine in advancing surgical care delivery in Africa. This review will also discuss the challenges behind telemedicine utilization in Africa, and recommend targeted measures to address those barriers while promoting the enhanced integration of telemedicine into surgical care delivery.
Methods
A comprehensive online literature search was conducted using several search engines, including PubMed, ScienceDirect, and Google Scholar to assess the potential advantages of telemedicine over traditional surgical practices in Africa, as well as to identify the challenges hindering its implementation. The literature review examined the role of nongovernmental organizations in promoting telemedicine adoption across various African countries. Literature search terms include “countries of Africa,” “impact of telesurgery and telemedicine in Africa,” and “current situation of telemedicine in intervention.” Only articles written in English were considered, and inclusion criteria included relevance to our research objectives and countries in Africa.
Results
The potential for telesurgery in Saharan and sub‐Saharan countries is still a milestone to be unlocked, but already telemedicine implementation has shown great results. Although hindrances like trust, lack of infrastructure, and lack of trained personnel in the field of telecommunication have been issues. There is a rise in the use of telemedicine in areas of interest like postsurgical care, doctor‐patient consultation, and tele‐monitoring. Various schemes and plans implemented by public organizations have also peaked since the pandemic. A telemedicine establishment requires multifactorial development occurring in a step‐by‐step manner. Although complexity in development and barriers faced in countries in Africa are concerns, the outcomes of using telemedicine are considerably better. The rising population and lack of medical specialists have led to a gap in access to approachable surgical care, and telemedicine has shown promising potential to overcome it.
Conclusion
Telemedicine implementation has changed the method of intervention in clinics all over the world. Implementation of parts of telemedicine like telesurgery and tele‐monitoring has the potential to overcome the concern of a rising population, but there is still a long way to go.
Keywords: challenges to telemedicine, inaccessibility, initiatives in Africa, recommendations, telemedicine, telemedicine and its applications
1. Introduction
According to the Health Professions Council of South Africa (HPCSA), telemedicine is defined as the application of electronic telecommunications, information technology (IT), or other electronic means to deliver healthcare services in two geographically distinct locations to facilitate, improve, and strengthen clinical, educational and research, especially to the under‐serviced areas in the Republic of South Africa. Telemedicine is an umbrella term, covering all healthcare components and activities as well as the healthcare system that they operate on. It may also be regarded as the use of electronic information and communication technologies for the administration or support of healthcare when distance separates participants [1]. Millions of people residing in various Low‐ and Middle‐Income Countries (LMICs) lack access to surgical care because of its extreme scarcity. According to a World Health Organization (WHO) investigation of the nation's major health centers, only suturing—1 of the 35 basic operations listed—was consistently given at all facilities. These institutions serve a catchment area of 23 million people and employ 64 surgeons in a variety of subspecialties; yet, it appears that they are unable to deliver a complete range of surgical services [2]. Despite the high volume of surgeries, the system has several nonphysical inefficiencies that can be addressed to minimize cancellations and boost capacity. Improving just the physical resources alone will not likely be sufficient to expand access to care in many environments. To truly enhance access to surgical treatment, patients' finances and processing will be essential factors to consider [3].
Telemedicine, therefore, is a revolutionary dimension to healthcare that moves beyond the clinical management of electronic medical record and electronic health record (EHR) simply because the electronic platforms efficiently collect, retrieve, and share patient information. More importantly, telemedicine empowers healthcare providers to manage patients optimally through real‐time consultation, case transfer, and virtual follow‐ups. It can be stated that the possibility of effective transfer of complex cases into specialized care centers in the surgical care setting is also supported by telemedicine solutions that ensure timely and proper care. The integration of telemedicine with EHR systems enables remote access to patient information, allows surgeons to make informed decisions, and coordinates care through distances. Telemedicine allows scheduling and consultation in rural areas; the surgeons can also make virtual consultations or visits, thus reducing traveling time and making optimal use of resources. Such are what help improve the surgical workflow while enhancing the quality and access to care by the patients in the remote regions [4].
One such study on the use of telemedicine in Africa has shown to be very beneficial in delivering patient care by greatly reducing the time taken in patient care delivery by creating a proper channel and a system for keeping track of the tests and investigations required pre‐and postoperatively. It has also been documented to reduce postoperative complications and infections in the patient by making regular follow‐ups feasible through different mediums of telecommunication which otherwise would have been difficult to achieve [4].
This review article aims to include a comprehensive analysis of the both effectiveness, and the shortcomings of telemedicine in the delivery of surgical care in the African continent, and the scope of this article is to focus on the recommended targeted measures to address the barriers to telemedicine, while also promoting the enhanced integration of telemedicine into surgical care delivery.
1.1. The Current State of Surgical Care Delivery in Africa
The necessary surgical care is inaccessible to many individuals who reside in low‐to‐middle‐income countries. Within this context, the call to improve access to safe surgery has recently escalated, as evidenced by the attention to inadequate surgical access outlined in the report of the Lancet Commission on Global Surgery [5]. Surgical conditions contribute to a loss of about thirty‐eight disability‐adjusted life years per 1000 population, either due to premature mortality or living with a disability secondary to surgical conditions, with the majority of surgical care provided by district hospitals in the continent [6]. Rural residents of Africa are unable to gain access to specialist referral hospitals easily, due to difficulties in traveling long distances, either because they are hesitant to undertake such journeys or they lack the means to do so. Surgical care in most of the rural hospitals in Sub‐Saharan Africa, where most of its population resides, is delivered by medical officers who have not received any formal training in surgery [7, 8].
Africa faces many obstacles in administering surgical services to its population, mainly because of the growing burden of non‐communicable diseases, lack of surgical workforce, and limited resources and infrastructure in the country [8, 9, 10]. These challenges are mostly encountered in resource‐limited countries such as Uganda [8]. According to a study, African children aged 5 years and above tend to die from injuries rather than from HIV, tuberculosis, and malaria altogether [11]. A significant portion of injured patients fail to make it to a healthcare facility, with only about one‐third managing to present to the hospital, and many presenting at a later, more critical stage [12]. In remote areas, there is limited access to surgical services as a result of inadequate transportation, poor road infrastructure, and a shortage of equipment and skilled surgical professionals [13]. The lack of infrastructure and resources profoundly impacts the ability to provide surgical care effectively, control infection, store medication, dispose of hazardous waste, and provide necessary training and supervision [14]. The limited infrastructure in nations with low‐to‐middle income has increased the rate of mortality and morbidity in patients requiring surgery, which subsequently led to an increase in case fatality rates for surgical conditions that are easily treated [5]. This affects the functionality of facilities, compromises the quality of care of surgical patients, and leads to demoralization of healthcare workers [8]. The disparities in surgical care between rural and urban areas in Africa persist because the necessary infrastructure and skilled personnel required for surgical services are mostly concentrated in urban areas, which highlights the restricted access faced by individuals living in rural regions of Africa. It is also evident that trained personnel are reluctant to work in rural areas due to theirpoor infrastructure and the lack of incentives [15].
1.2. Telemedicine and Its Application in Surgical Care Delivery in Africa
Telemedicine has showcased its efficacy in facilitating swift access to healthcare providers for diagnosis, treatment, and prevention measures of various health conditions. The adoption of telemedicine in Sub‐Saharan Africa originated in 1980 when Ethiopia, Ghana, Nigeria, and Gambia initiated the HealthNet telemedicine project. Various countries have followed and sustained this progress, with Rwanda serving as a notable example, improving healthcare and promoting health‐related education and surveillance for both professionals and patients [16] (Figure 1).
Figure 1.
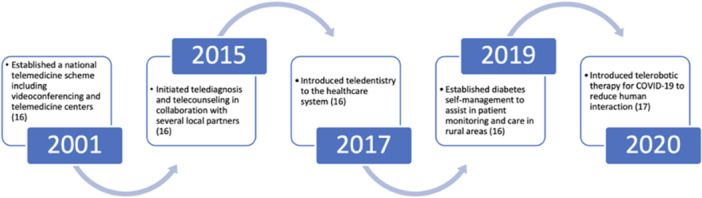
Utilization of Telemedicine in Rwanda from 2001 to 2020 [16, 17].
Historically, surgery was viewed as a specialty that required in‐person care. Nonetheless, telemedicine is now being used for patient and provider education, as well as other parts of surgical treatment [18]. Telemedicine approaches are employed for precise diagnosis, management decision‐making, preoperative anesthesia meetings, and consultation with other surgical departments. Additionally, digital photos, live video, or SMS are utilized to inspect postoperative wounds or medical equipment, like nasogastric tubes, aiding physicians in assessing local complications effectively—the third approach substitutes follow‐up in‐person visits for telemonitoring [4]. Tele‐education, the ongoing instructions tailored to the needs of the patients, also facilitates a deeper comprehension of the patient's circumstances, supports therapy individualization, and enhances results [19]. Therefore, to guarantee efficient communication, a variety of modalities are used, such as text messaging, digital photographs, health applications, mobile phones, and teleconferencing [4].
Significant progress has been made in post‐discharge surgical care through telemedicine, like replacing follow‐up clinic visits with calls or videocalls and ongoing monitoring and collection of clinical data through text messages or images, which showed excellent therapeutic results, increased patient satisfaction through improved accessibility, shortened wait periods, and lower expenditure for both patients and healthcare systems [20]. When compared to traditional in‐person follow‐ups, telemedicine offers comparable complication rates and outstanding clinical outcomes for both nonelective high‐risk procedures and elective low‐risk procedures [21]. Acknowledging the importance of patient satisfaction as a cornerstone of quality surgical care, individuals who have benefited from postoperative telemedicine services have expressed high patient satisfaction levels, highlighting the simplicity of use as a notable advantage [21]. Moreover, it expands access to clinical treatment for individuals from urban and rural locations with limited transportation options [22]. Telemedicine services not only make surgical care more accessible and reduce the need for in‐person visits but also create additional in‐clinic slots for the evaluation of new surgical patients, which can lead to a potential rise in several elective surgeries [21]. Patients also perceive telemedicine services as cost‐effective as compared to the traditional in‐clinic follow‐up visits, which typically incur higher financial costs, encompassing missed work and travel expenses, in addition to appointment fees [23].
While telemedicine services offer promising solutions in addressing several surgical challenges, including transportation hurdles to healthcare facilities and limited access to physicians, a few formidable obstacles remain. These include the substantial burden of surgical disease, barriers to receiving proper treatment, insufficient infrastructure and resources within the healthcare system, as well as the lack of technical advancements, which collectively suggest that telemedicine protocols for surgical care will be more difficult to implement in low‐income nations [24]. The workload that currently exists for healthcare professionals presents another possible obstacle, as telemedicine requires additional time and effort [16]. Network instability and coverage issues, higher setup costs for technology, poor image quality, the inability to confirm information delivery by SMS recipients, time zone differences for international collaborations and mentoring, and the unequal distribution of services within and across geographic regions are possible restrictions [24]. The lack of a framework for balancing the interests of major and diverse stakeholders in the installation of telemedicine programs in some African regions resulted in a hold‐up in the field's advancement and a rise in sustainability‐related problems [16]. In addition, the use of telemedicine services presents serious concerns about patient security and privacy because private information is shared and certain modalities lack encryption, which increases the risk of data breaches [21].
1.3. The Role of Telemedicine in Enhancing Surgical Care Delivery in Africa
1.3.1. Telemedicine Initiatives in Africa–Insights and Lessons Learned
Dodoo and colleagues (2022) discussed that since the completion of the original projects, little progress has been made in terms of service growth due to the progress and challenges of telemedicine programs in Sub‐Saharan Africa and the installation of telemedicine systems in the Saharan States [16]. The study also indicates that in particular during the COVID‐19 period, appropriate progress has been made in the deployment, extension, and sustainability of telemedicine systems and services. Given these factors, to improve the current healthcare provision for enhanced user acceptance and satisfaction, an urgent stakeholder focus should be given to the imbalanced deployment of telemedicine systems [16]. The lessons learned from a project on telemedicine in Western Africa have been documented by Geissbuhler et al. [25]. It was seen that there was the instability of basic infrastructure, the electricity supply in particular, as well as the limitation of international bandwidth, which is often abused, especially by e‐mail accounts hosted outside of the country, along with the lack of reliable connectivity beyond major cities. Nevertheless, as the national infrastructure develops, these issues are continuing to improve [25]. The significance of telemedicine during the COVID‐19 pandemic in Africa has been emphasized in a study conducted by David and colleagues (2020) [25]. The telemedical medical network, which was created to bridge the gap in patient access to medical treatment, had its own set of issues. Poor internet connectivity, a lack of telemedicine knowledge, and basic infrastructure instability, with a focus on power supply, are among the obstacles that African nations encounter when establishing a robust telemedical network. One of the reasons telemedicine remains unpopular in many African nations is that African populations have insufficient awareness of it. In addition, physical interaction between patients and healthcare providers is still required in some instances, since remote doctors can only treat ailments to a certain extent.
Telemedicine can be useful in eliminating the shortage of doctors in a certain area by helping connect the locals to a wide number of doctors outside the particular area [26]. A tele‐mentoring program designed for gynecologic oncologists in Mozambique has enhanced the understanding of surgical technique, and staging, along with the preoperative and postoperative management for patients [27]. It also can offer rural African regions access to previously inaccessible information and technologies. Surgical teams are often very restricted and need the support of experts who have substantial experience with certain surgical procedures and patients. Telesurgery enables surgeons with lesser training and those practicing in rural places with low socioeconomic conditions of healthcare, to achieve better health outcomes [28]. Telemedicine also allows the scope to observe, monitor, and provide real‐time inputs to inexperienced surgeons in rural areas through video calling which can help to greatly reduce any complications that may otherwise arise during the surgery [29].
The advantages and limitations of telemedicine are summarized (Table 1). General Ethical Guidelines are regulated by the HPSCA, and were revised in December 2021 [33] (Table 2).
Table 1.
| Advantages of telemedicine | Limitations of telemedicine |
|---|---|
| Telemedicine improves access to healthcare services, especially in rural locations with inadequate facilities | Africa faces a variety of challenges, including funding limitations, ethical concerns about patient privacy, and individual and governmental policies. Technological challenges include issues like the absence of infrastructure for such projects |
| Telemedicine has the potential to address medical challenges, particularly in areas where distance is a substantial barrier to healthcare access | Limited adaption of telemedicine in African countries due to obstacles which include low computer literacy among medical professionals, insufficient funding, and reluctance due on the perception of high costs [30] |
| Collaborations for Healthcare Solutions with big healthcare companies can help deliver healthcare solutions to remote areas | Financial limitations due to national financial budgetary limits |
| Improved Health Infrastructure: Telemedicine has helped countries like certain African countries improve training, service delivery, and collaboration among healthcare facilities [32] | Inadequate ICT infrastructure‐ For the efficient installation and operation of a telemedicine program, many poor nations lack the information and communication technology (ICT) necessary, including as computers, Internet networks, printers, and energy. Further problems associated with the telemedicine network's downtime in rural and isolated areas include power supply and internet connectivity [31] |
| Enables distance education, teleconsultations, and knowledge sharing of data and knowledge between healthcare professionals in African countries [30] | A large amount of start‐up Cost is needed to set up the initial process [31] |
| Improved access to specialist medical services by enabling remote diagnosis and consultations | Absence of any Brand‐ambassadors or leaders in the field of telemedicine to guide the way for setting up telemedicine in these countries [31] |
| Cost Savings – reduced the burden of transportation costs needed to reach the healthcare hospitals [32] | Policy Barriers ‐ Lack of a consistent and standardized telemedicine policy causes uncertainty when developing telemedicine‐related services, programs, and ensuring their seamless execution [31] |
| Increases patient engagement through patient counseling and ensuring there is proper adherence to treatment regimes through regular teleconsultations which would otherwise not be possible [32] |
Table 2.
Government policies and regulations ‐ general ethical guidelines are regulated by the HPSCA, and were revised in December 2021 [33].
| Governing body | Regulated by the Health Professions Council of South Africa (HPCSA) |
| Authorization | During the COVID‐19 pandemic, telemedicine was authorized by the HPCSA, allowing remote consultations via telephonic or virtual platforms, with fees permitted for services rendered [33]. |
| Types of telemedicine | Routine, Specialist and Emergency consultations |
| Users | Doctor‐doctor‐, doctor‐user interface |
| Monetary Regulation | Routine consultation fees of the doctor |
| Insurance | Professional Insurance Cover |
| Eligibility | Only doctors registered with the HPCSA |
| Platform | Various internet consultation platforms but not social media |
| Records | To be maintained ensuring patient confidentiality |
| Consent | Prior informed consent is needed from the patient |
| Privacy | Patient confidentiality must be maintained, adhering to the Protection of Personal Information Act (POPIA) and the National Health Act [33]. |
| Transfer of Information | Regulated by the POPIA |
| Liabilities | Noncompliance to the guidelines can lead to disciplinary action |
1.3.2. Impact of Telemedicine on Surgical Outcomes in Africa
Over the past 2 decades, telemedicine has become significant in various fields of medicine by overcoming barriers like remoteness, space, and time. Growth in the communication field has led to significant growth in physician‐patient interaction [34]. In low‐income countries lacking access to life‐saving interventions due to a lack of surgeons, with as few as 0.5 surgeons per 100,000 people, telesurgery plays a significant role. The first‐ever use of telesurgery in Africa was done in Somalia by army personnel [16]. As much as it is significant and urgently needed in low‐income countries, it also faces a lack of trust from patients [16, 24].
Sierra Leone is a political conflict area where trauma led to 325,000 deaths, sharing 7% of the disease burden with just two specialist surgeons [35]. Here, telesurgery has a greater role where a surgeon in training or not trained in a specific procedure or a healthcare worker can perform a life‐saving or emergency intervention [35, 36]. However, in recent years, data shows us that people mostly use telemedicine in cases of postoperative care and preoperative care, as it overcomes the barrier of transport and also reduces doctor‐patient consultant time [36]. Telemedicine has a great deal of interest in LMICs because of its feasibility and usability. Furthermore, it helps hospitals and clinics keep track of and update patients about surgery cancellations and referrals, mainly those living in remote areas of Africa [37].
Efforts are being made in different parts of Africa to improve surgical management and intervention, such as a network led by Africans known as AfroSurg collaborative (AfroSurg) that is setup to provide essential knowledge in training new surgeons; surgical services were established in 2020 by the government as the National Department of Health Technical Working Group; and also, the National Surgical Obstetric and Anesthesia Plan [38]. All these setups and plans are made to provide affordable management. The process has been shown to speed up by introducing telelearning to doctors and trainees to have a seamless process [39]. Though telesurgery processes requiring high specialties are only seen in high‐income countries, rescue intervention and connecting to mass populations in remote areas have shown improvement. Mainly in cases like when healthcare workers manage burn patients, in cases of obstruction in ventilation, releasing of intracranial pressure, or stopping bleeding from deep arteries, in all these cases, health workers can benefit from advice [34]. Telemedicine usage has spiked during the COVID‐19 pandemic, mainly in areas of postsurgical care and patient consultation. In the Republic of Mozambique, oncologists and gynecologists have increased the use of tele‐monitoring in training, improving knowledge and staging of cancers [40].
With growing populations and increasing demand for consulting services in African countries, telemedicine emerges as the only viable solution. However, with internet connectivity still lacking at just 15% and surgical and medical supplies behind, telesurgery still faces difficulty [39, 41]. Hence, to bolster the field of telemedicine, a gradual, step‐by‐step development should take place before the widespread implementation of telemedicine in various surgical domains. This includes expanding surgical tool manufacturing and investing more in telecommunication [36, 41]. Such efforts mark a pivotal milestone in the advancement of surgical care in Africa, ultimately improving the affordability and accessibility of surgical services [16].
1.4. Challenges to Telemedicine Adoption in Surgical Care Delivery in Africa
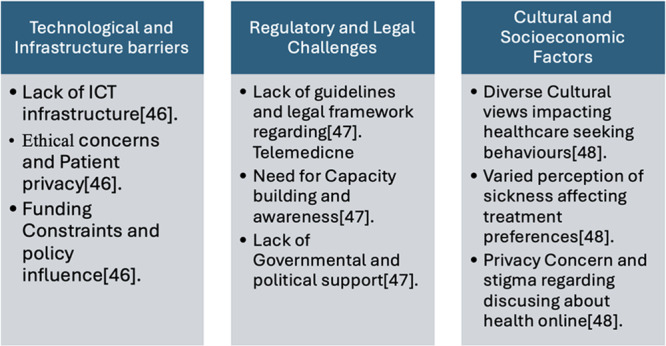
The technological and infrastructure barriers to adopting telemedicine to provide surgical care in sub‐Saharan Africa include inadequate Information communication and technological infrastructure which leads to substandard implementation of tools like telemedicine. The ethical concerns of patient privacy, lack of funding, and individual and government policies are some of the nontechnological barriers to adopting telemedicine [42]. The Regulatory and Legal challenges related to telemedicine in Africa include the lack of guidelines, legal frameworks, and legislation, as well as the absence of direction from key health organizations like African Union Health Ministers and the New Partnership for Africa's Development on e‐health. In the past 5 years, e‐health telemedicine or telehealth h has not been included in any of the policies [43]. To address this, there is a need for capacity development within governments and increased awareness and training in telemedicine. African communities have different views on diseases. Providing conventional healthcare in Africa is not easy because of the different cultural understandings of what causes sickness and diseases, which may affect the way people seek healthcare. Many patients perceive their illnesses as instances of certain social, natural, or spiritual conditions in their lives. Therefore, seeking medical help from doctors may be mandatory in Africa. Although many patients tend to like one‐to‐one consultations with their physicians, others prefer consulting with religious personnel before undergoing modern treatment. People are afraid of letting others tell them about their diseases through internet linkage mainly within stigmatizing environments though some other individuals are just unwilling to discuss them online for various reasons as such [44]. The important challenges to adoption of telemedicine in Africa are highlighted (Figure 2).
Figure 2.
2. Future Directions and Recommendations
Telemedicine modalities in surgical care enhance efficiency and quality of care by reaching a larger population and reducing hospital readmissions [4]. It is therefore imperative that policymakers prioritize telemedicine initiatives since they possess the ability to improve health outcomes of the populations living in rural regions with restricted access, shortage of doctors, and inadequate infrastructure [44]. By doing so, policymakers can effectively bridge the gap between patients and high‐quality medical services, ensuring equitable access and benefits for everyone, regardless of their geographical location [45]. Although more research is being conducted on telemedicine in LMICs, the employment of telemedicine modalities in surgery is becoming more commonplace. However, only a limited number of these studies have involved well‐conducted randomized controlled trials and evaluated their clinical efficacy. Therefore, there is a pressing need for additional research to strengthen evidence‐based practice and to guide appropriate actions to be taken by the healthcare systems [24].
Telemedicine is an economical way to provide medical care that can genuinely enhance patient outcomes with limited resources [46]. Therefore, policymakers and healthcare professionals in Sub‐Saharan Africa must create telemedicine implementation plans that are unique to each nation. Developers must consider creating a telemedicine system that is easy to use, affordable, and beneficial to both patients and healthcare providers [47]. However, to fully embrace and utilize any digital health solution, it is imperative to have supervisory structures, clear roles and accountability for decision‐making, and effective training programs for frontline health workers and community‐based clinicians [46]. It is also recommended that telemedicine technology training be included in the curriculum for medical students [47]. Systems design must also take patient data security and appropriate data management and storage into account. An important feature to be implemented in LMICs is the provision of offline capacity and backup systems, which enable users to input data and utilize the system even in the event of a poor or unavailable network connection [46].
To ensure that telemedicine is used in healthcare in a way that fosters quality partnerships, balances stakeholder interests, expands the use of affordable telemedicine services, and provides technical support and ongoing funding, governments and policymakers should establish stringent protocols, legislation, and ethical standards. Maintaining excellent partnerships with foreign partners is also advantageous since it contributes to the stakeholders' acceptance [47]. The infrastructure—human, technological, and systemic—that allows the digital health program to operate at scale is just as crucial as steady financial support. It permits long‐term sustainable operations and ensures adherence to national health policies and guidelines through regulatory standards and frameworks [46]. Therefore, investments set aside for creating and executing telemedicine will rise along with partnerships between the public and private health sectors toexpand the funding sources for telemedicine initiatives [47].
3. Conclusion
In recent years, the use of telemedicine has shown tremendous potential for the future as a solution to the crisis of an increasing population and a shortage of specialists in African countries [16]. After the pandemic, telemedicine uses in different fields such as patient consultancy and telemonitoring of healthcare personnel have risen, as it was mostly the only way to provide consultancy to most parts of Africa [37, 40]. Telesurgery still requires more development than other fields of telemedicine, as evidence shows that even a latency of 300 ns can change outcomes. Nonetheless, telemonitoring and tele‐education are becoming more familiar in several parts of Africa. It also made different parts of the world provide consulting and training for young surgeons in Africa [24, 37].
As the cornerstone of telemedicine development hinges on the improvement of telecommunication and connectivity infrastructure, these are two prime target areas for investment before the integration of regular bases of telesurgery in clinical practices [37]. Thus, a gradual strategy is required for improvement, alongside expanding the manufacturing of surgical supplies [35]. Though barriers to telemedicine adoption in different parts of Africa persist, from unstable connectivity to a lack of healthcare investment, coupled with resistance and trust issues regarding these services, the potential of telemedicine far exceeds these challenges [24].
Author Contributions
Olivier Uwishema: conceptualization, project administration, writing‐review and designing. All authors: data collection and assembly. Olivier Uwishema: reviewed and edited the first draft. Manuscript writing: all authors. Alicia Kwan Su Huey: reviewed and edited the second draft. Magda Wojtara: reviewed and edited the third draft. Olivier Uwishema: reviewed and edited the final draft. Final approval of manuscript: all authors. Figure 1 was created by Zeinab Kazan [1, 3]. Figure 2 was created by Raj Pravin Patel [1, 6]. Table 1 was created by Karan Choudhary [1, 5]. Table 2 was created by Karan Choudhary [1, 5].
Ethics Statement
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
We would like to thank Oli Health Magazine Organization's members for their contributions and support for this manuscript. The authors declare that there were no funding sources for this manuscript. Furthermore, no external organizations had any role in the study design; collection, analysis or interpretation of data; writing of the report; or the decision to submit the report for publication.
Data Availability Statement
This review paper does not contain original data. The findings and conclusions presented are based on a synthesis of existing literature. All data and information referenced in this review are derived from previously published studies, which are cited throughout the manuscript. Readers can access the original research data and findings from the sources mentioned in the references. For any queries regarding specific data or to access certain studies, please refer to the respective journals or databases where the original research is published.
References
- 1. Institute of Medicine (US) ., Committee on Evaluating Clinical Applications of Telemedicine, eds. Field M. J. (Washington (DC): National Academies Press (US), 1996). [Google Scholar]
- 2. Penoyar T., Cohen H., Kibatala P., et al., “Emergency and Surgery Services of Primary Hospitals in the United Republic of Tanzania,” BMJ Open 2, no. 1 (2012): e000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rajaguru P. P., Jusabani M. A., Massawe H., Temu R., and Sheth N. P., “Understanding Surgical Care Delivery in Sub‐Saharan Africa: A Cross‐Sectional Analysis of Surgical Volume, Operations, and Financing at a Tertiary Referral Hospital in Rural Tanzania,” Global Health Research and Policy 4 (2019): 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Asiri A., AlBishi S., AlMadani W., ElMetwally A., and Househ M., “The Use of Telemedicine in Surgical Care: A Systematic Review,” Acta Informatica Medica 26, no. 3 (2018): 201–206, 10.5455/aim.2018.26.201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meara J. G., Leather A. J. M., Hagander L., et al., “Global Surgery 2030: Evidence and Solutions for Achieving Health, Welfare, and Economic Development,” The Lancet 386, no. 9993 (2015): 569–624. [DOI] [PubMed] [Google Scholar]
- 6. Luboga S., Macfarlane S. B., von Schreeb J., et al., “Increasing Access to Surgical Services in Sub‐Saharan Africa: Priorities for National and International Agencies Recommended by the Bellagio Essential Surgery Group,” PLoS Medicine 6, no. 12 (2009. Dec 22): e1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Galukande M., von Schreeb J., Wladis A., et al., “Essential Surgery at the District Hospital: A Retrospective Descriptive Analysis in Three African Countries,” PLoS Medicine 7, no. 3 (2010): e1000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ozgediz D., Galukande M., Mabweijano J., et al., “The Neglect of the Global Surgical Workforce: Experience and Evidence from Uganda,” World Journal of Surgery 32, no. 6 (2008): 1208–1215. [DOI] [PubMed] [Google Scholar]
- 9. Archampong E. Q., “Surgery in Developing Nations,” British Journal of Surgery 93, no. 5 (2006): 516–517. [DOI] [PubMed] [Google Scholar]
- 10. Kelly C. M., Starr N., Raykar N. P., Yorlets R. R., Liu C., and Derbew M., “Provision of Surgical Care in Ethiopia: Challenges and Solutions,” Global Public Health 13, no. 11 (2018): 1691–1701. [DOI] [PubMed] [Google Scholar]
- 11. Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T., and Murray C. J., “Global and Regional Burden of Disease and Risk Factors, 2001: Systematic Analysis of Population Health Data,” The Lancet 367, no. 9524 (2006): 1747–1757. [DOI] [PubMed] [Google Scholar]
- 12. Mock C., Ofosu A., and Gish O., “Utilization of District Health Services By Injured Persons in a Rural Area of Ghana,” The International Journal of Health Planning and Management 16, no. 1 (2001): 19–32. [DOI] [PubMed] [Google Scholar]
- 13. Grimes C. E., Bowman K. G., Dodgion C. M., and Lavy C. B. D., “Systematic Review of Barriers to Surgical Care in Low‐Income and Middle‐Income Countries,” World Journal of Surgery 35, no. 5 (2011): 941–950. [DOI] [PubMed] [Google Scholar]
- 14. Hsia R. Y., Mbembati N. A., Macfarlane S., and Kruk M. E., “Access to Emergency and Surgical Care in Sub‐Saharan Africa: The Infrastructure Gap,” Health Policy and Planning 27, no. 3 (2012. May): 234–244. [DOI] [PubMed] [Google Scholar]
- 15. Mungadi I. A., “Quality Surgical Care for Rural Dwellers: The Visiting Option,” Tropical Doctor 35, no. 3 (2005): 151–153. [DOI] [PubMed] [Google Scholar]
- 16. Dodoo J. E., Al‐Samarraie H., and Alsswey A., “The Development of Telemedicine Programs in Sub‐Saharan Africa: Progress and Associated Challenges,” Health and Technology 12, no. 1 (2022): 33–46, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8613515/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mugabo A. Rwanda Deploys Robots in Treating COVID‐19 Patients. The East African [Internet]. 2020 May 14, https://allafrica.com/stories/202005140352.html.
- 18.Telemedicine in pediatric surgery ‐ PubMed [Internet]. [cited 2024 Mar 8], https://pubmed.ncbi.nlm.nih.gov/29801660/.
- 19. Farias F. A. C., Dagostini C. M., Bicca Y. A., Falavigna V. F., and Falavigna A., “Remote Patient Monitoring: A Systematic Review,” Telemedicine and E‐Health 26, no. 5 (2020): 576–583. [DOI] [PubMed] [Google Scholar]
- 20. Gunter R. L., Chouinard S., Fernandes‐Taylor S., et al., “Current Use of Telemedicine for Post‐Discharge Surgical Care: A Systematic Review,” Journal of the American College of Surgeons 222, no. 5 (May 2016): 915–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Williams A. M., Bhatti U. F., Alam H. B., and Nikolian V. C., “The Role of Telemedicine in Postoperative Care,” mHealth 4 (2018): 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ellimoottil C. and Boxer R. J., “Bringing Surgical Care to the Home Through Video Visits,” JAMA Surgery 153, no. 2 (2018): 177–178. [DOI] [PubMed] [Google Scholar]
- 23. Demaerschalk B. M., Cassivi S. D., Blegen R. N., et al., “Health Economic Analysis of Postoperative Video Telemedicine Visits to Patients’ Homes,” Telemedicine and e‐Health 27, no. 6 (2021): 635–640. [DOI] [PubMed] [Google Scholar]
- 24. Owolabi E. O., Mac Quene T., Louw J., Davies J. I., and Chu K. M., “Telemedicine in Surgical Care in Low‐ and Middle‐Income Countries: A Scoping Review,” World Journal of Surgery 46, no. 8 (2022): 1855–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Geissbuhler A., Ly O., Lovis C., and L'haire J. F., “Telemedicine in Western Africa: Lessons Learned From a Pilot Project in Mali, Perspectives and Recommendations,” AMIA… Annual Symposium Proceedings. AMIA Symposium 2003 (2003): 249–253. [PMC free article] [PubMed] [Google Scholar]
- 26. David K. B., Solomon J. K., Yunusa I., et al., “Telemedicine: An Imperative Concept During COVID‐19 Pandemic in Africa,” Pan African Medical Journal 35, no. Suppl 2 (2020): 129, 10.11604/pamj.supp.2020.35.25281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Holmer H., Lantz A., Kunjumen T., et al., “Global Distribution of Surgeons, Anaesthesiologists, and Obstetricians,” The Lancet Global Health 3, no. Suppl (2015): S9–S11, 10.1016/S2214-109X(14)70349-3. [DOI] [PubMed] [Google Scholar]
- 28. Heyes R., Haram N. H., Luck J. E., Billingsley M. L., and Greenfield M. J., “The Role of Augmented Reality Telesurgery in Promoting Equity in Global Surgery,” Diversity & Equality in Health and Care 14 (2017): 119–121, 10.21767/2049-5471.1000101. [DOI] [Google Scholar]
- 29. Merchant S. Twenty Years of Telesurgery; Improving Healthcare Delivery to Underserved Locations. AM Intercult Mag. 2021, https://www.aimblog.io/2021/01/23/twenty-years-of-telesurgery-improving-healthcare-delivery-to-underserved-locations.
- 30. Wamala D. S. and Augustine K., “A Meta‐Analysis of Telemedicine Success in Africa,” Journal of Pathology Informatics 4, no. 1 (2013): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bali S., “Barriers to Development of Telemedicine in Developing Countries [Internet].” Telehealth (IntechOpen, 2019), 10.5772/intechopen.81723. [DOI] [Google Scholar]
- 32. Aranda‐Jan C. B., Mohutsiwa‐Dibe N., and Loukanova S., “Systematic Review on What Works, What Does Not Work and Why of Implementation of Mobile Health (Mhealth) Projects in Africa,” BMC Public Health 14 (2014): 188, 10.1186/1471-2458-14-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Health Professions Council of South Africa ., General Ethical Guidelines for Good Practice in Telehealth. Revised December 2021 (Pretoria: Health Professions Council of South Africa, 2021). [Google Scholar]
- 34. Mehta A., Awuah W. A., Aborode A. T., et al., “Telesurgery's Potential Role in Improving Surgical Access in Africa,” Annals of Medicine & Surgery 82 (2022): 104511, 10.1016/j.amsu.2022.104511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jafarzadeh F., Rahmani F., Azadmehr F., Falaki M., and Nazari M., “Different Applications of Telemedicine ‐ Assessing the Challenges, Barriers, and Opportunities‐ A Narrative Review,” Journal of Family Medicine and Primary Care 11, no. 3 (2022): 879–886, 10.4103/jfmpc.jfmpc_1638_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mars M., “Telemedicine and Advances in Urban and Rural Healthcare Delivery in Africa,” Progress in Cardiovascular Diseases 56, no. 3 (2013): 326–335, 10.1016/j.pcad.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 37. Wismayer R., “Study on Progress and Challenges Associated With the Use of Telemedicine in Sub‐Saharan Africa.” New Horizons in Medicine and Medical Research Vol. 3 (Book Publisher International (a Part of SCIENCEDOMAIN International), 2022), 44–50, 10.9734/bpi/nhmmr/v3/2794c. [DOI] [Google Scholar]
- 38. Mbunge E., Muchemwa B., and Batani J., “Are We There Yet? Unbundling the Potential Adoption and Integration of Telemedicine to Improve Virtual Healthcare Services in African Health Systems,” Sensors International 3 (2022): 100152, 10.1016/j.sintl.2021.100152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ndwabe H., Basu A., and Mohammed J., “Post Pandemic Analysis on Comprehensive Utilization of Telehealth and Telemedicine,” Clinical eHealth 7 (2024): 5–14, 10.1016/j.ceh.2023.12.002. [DOI] [Google Scholar]
- 40. Akintunde T. Y., Akintunde O. D., Musa T. H., et al., “Expanding Telemedicine to Reduce the Burden on the Healthcare Systems and Poverty in Africa for a Post‐Coronavirus Disease 2019 (COVID‐19) Pandemic Reformation,” Global Health Journal 5, no. 3 (2021): 128–134, 10.1016/j.glohj.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Onyeabor U. S., Okenwa W. O., Onwuasoigwe O., et al., “Telemedicine in the Age of the Pandemics: The Prospects of Web‐Based Remote Patient Monitoring Systems for Orthopaedic Ambulatory Care Management in the Developing Economies,” DIGITAL HEALTH 10 (2024): 1–16, 10.1177/20552076241226964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kokdemir: Are Telemedicine/Telehealth Services Ethical ‐ Google Scholar [Internet]. [cited 2024 Mar 8], https://scholar.google.com/scholar_lookup?journal=Sendrom&title=Are+telemedicine/telehealth+services+ethical?&author=P+Kokdemir&author=S+Gorkey&volume=14&publication_year=2002&pages=86-92&.
- 43. Mars M., “Health Capacity Development Through Telemedicine in Africa,” Yearbook of Medical Informatics 19, no. 01 (2010): 87–93. [PubMed] [Google Scholar]
- 44. Okoroafor I., Chukwuneke F., Ifebunandu N., Onyeka T., Ekwueme C., and Agwuna K., “Telemedicine and Biomedical Care in Africa: Prospects and Challenges,” Nigerian Journal of Clinical Practice 20, no. 1 (2017): 1–5. [DOI] [PubMed] [Google Scholar]
- 45. David K. B., Solomon J. K., Yunusa I., et al., “Telemedicine: An Imperative Concept During COVID‐19 Pandemic in Africa,” Pan African Medical Journal 35, no. Suppl 2 (2020): 129, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7687473/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Labrique A. B., Wadhwani C., Williams K. A., et al., “Bestpractices in Scaling Digital Health in Low and Middle Income Countries,” Globalization and Health 14, no. 1 (2018): 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dodoo J. E., Al‐Samarraie H., and Alzahrani A. I., “Telemedicine Use in Sub‐Saharan Africa: Barriers and Policy Recommendations for Covid‐19 and Beyond,” International Journal of Medical Informatics 151 (2021): 104467, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9761083/. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This review paper does not contain original data. The findings and conclusions presented are based on a synthesis of existing literature. All data and information referenced in this review are derived from previously published studies, which are cited throughout the manuscript. Readers can access the original research data and findings from the sources mentioned in the references. For any queries regarding specific data or to access certain studies, please refer to the respective journals or databases where the original research is published.


