Abstract
Background:
Proximal phalanx fractures are common, with surgical fixation indicated for unstable fractures. Traditionally, closed reduction percutaneous pinning (CRPP) resulted in decreased stiffness and tendon irritation compared to open reduction internal fixation (ORIF). We hypothesized that more recent studies would have more similar outcomes to CRPP. The purpose of this study was to compare CRPP and ORIF in terms of range of motion, Disabilities of the Arm, Shoulder, and Hand (DASH) scores, and complications.
Methods:
Four electronic databases were queried from 2010 to present. Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, two independent reviewers performed a two-step review process to identify relevant articles. Patient demographics, total active motion (TAM), DASH, and complications were extracted. The methodological quality of each study included was assessed independently. Meta-analysis was performed for comparative trials.
Results:
Fourteen studies met inclusion criteria including four comparative studies: Thirteen studies included TAM. The weighted average TAM was 228 ± 34° for CRPP and 223 ± 32° for ORIF (P = .07 with 95% confidence interval (CI), −0.5 to 10.5). Seven studies evaluated DASH scores; weighted average was 8.2 ± 8.9 for CRPP and 11.7 ± 6.5 for ORIF (P < .01 with 95% CI, 1.8-5.2). Two studies directly compared CRPP to ORIF, favoring ORIF for both TAM with d = 1.07 and DASH with d = 0.23. Rates of tenolysis or hardware removal were higher for ORIF (P < .01).
Conclusions:
New literature suggests more equipoise with regard to treatment of proximal phalanx fracture with CRPP versus ORIF.
Type of study/level of evidence:
Meta-analysis, Level II.
Keywords: hand, surgery, proximal phalangeal fractures
Introduction
Phalanx fractures are common, accounting for 20% to 33% of hand injuries.1-5 The proximal phalanx is the most common phalanx injured and has a worse prognosis compared to other phalanx fractures.1,5,6 Unstable proximal phalanx fractures are indicated for surgical intervention.1-8 Several different methods for surgical treatment of unstable extraarticular proximal phalanx fractures have been reported, the most common of which are open reduction internal fixation (ORIF) with plate and screws versus lag screws alone and closed reduction percutaneous pinning (CRPP).3,7,9,10
Regardless of method, the goal of surgical fixation is to rigidly fix the fracture to promote fracture healing while allowing for early mobilization to prevent stiffness.1-3,11 The use of plate and screws has the benefit of rigid fixation and early mobilization, although complications related to adhesions, flexion contracture, and extension lag have historically been reported.5,6,10 Kirschner wires (K-wires) minimize soft tissue injury and preserve blood supply; however, they do not provide rigid fixation and have problems related to prolonged immobilization, pin tract infection, and malunion.4,10,12,13 Several studies have looked at outcomes of proximal phalanx fixation with CRPP versus ORIF, although a consensus has yet to be reached regarding the best method of proximal phalanx fracture fixation, despite their common occurrence.3,5,10 Previous studies have demonstrated worse outcomes with ORIF including stiffness and extensor tendon irritation, as well as complications such as hardware removal.8,14-16 However, many of these were performed before the advent of newer lower profile plates.2,6
The purpose of this study is to compare CRPP and ORIF for treatment of unstable proximal phalanx fractures through systematic review and meta-analysis. We specifically looked at range of motion (ROM; total active motion [TAM]), functional outcomes (Disabilities of the Arm, Shoulder, and Hand [DASH] score), complications, and need for subsequent surgery. We hypothesized that newer studies with the availability of lower profile plating systems for ORIF would result in outcomes similar to CRPP.
Materials and Methods
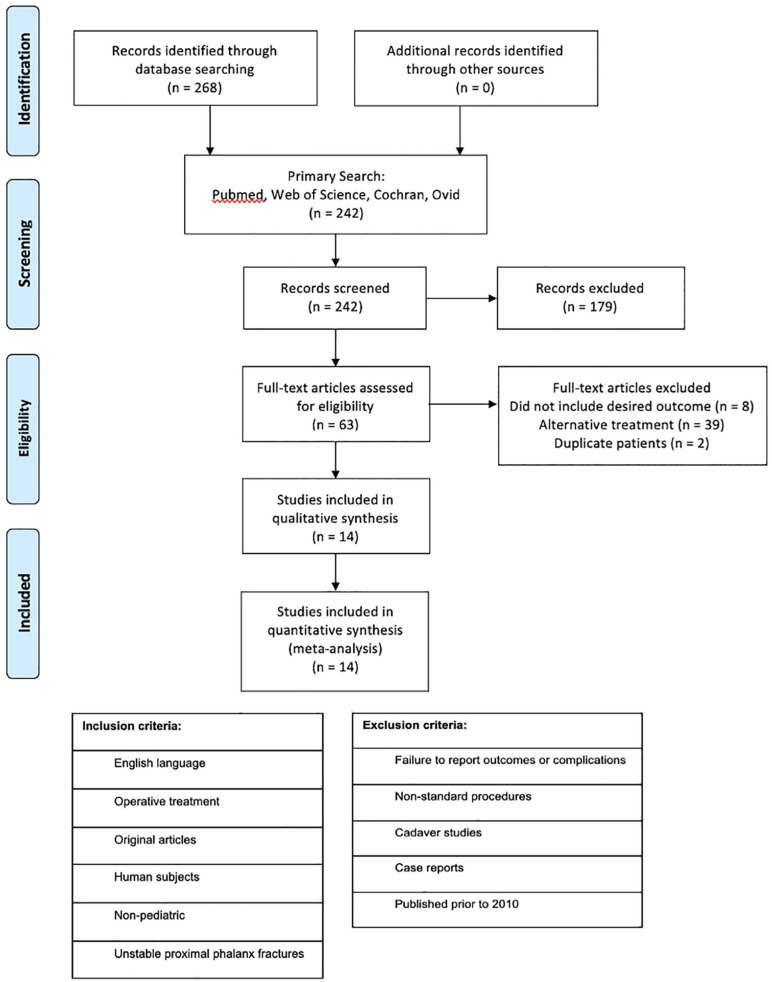
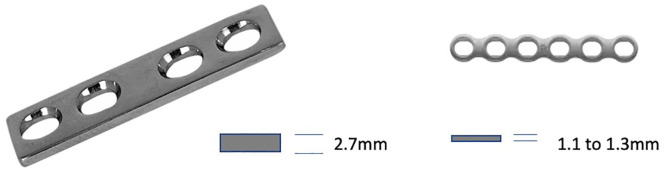
A literature review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Four online databases (PubMed, Ovid Medline, Web of Science, and Cochrane) were queried using search terms “proximal phalanx fracture” or “proximal phalangeal fractures” and “hand” and “surgical.” Two independent reviewers performed a two-step review process (Author 1 and Author 2). Inclusion and exclusion criteria are included in Figure 1. Unstable proximal phalanx fractures were defined as extraarticular fractures with greater than 10° angulation or greater than 2 mm shortening or rotational deformity with fracture patterns including transverse, short oblique, long oblique, and spiral. Articles published prior to 2010 were excluded to include the use of low-profile plate technology. Many of the studies included in our retrospective review did not specify which type of plates was used, so a more recent date range was chosen to increase the probability that the low-profile plates were used. Figure 2 demonstrates the difference between prior plates with 2.7 mm thickness and newer low-profile plates of 1.1 to 1.3 mm in thickness. Articles related to oncology and gunshot wounds were considered outside the scope of this article. Initial search revealed a total of 268 articles (179 from PubMed, 86 from Web of Science, 3 from Cochrane, and 0 from Ovid Medline). Exclusion of duplicates yielded 242 unique articles. On review of titles and abstracts, 179 articles were excluded. This left 63 articles for full text review, 14 of which met final inclusion and exclusion criteria (Figure 1). Study characteristics were recorded including the author, study design, number of fractures included, quality score, and level of evidence (Table 1). Quality score was determined according to the Methodological Index for Non-Randomized Studies (MINORS) criteria, a validated tool to assess the methodological quality of nonrandomized studies. 17 Eight criteria are applied to noncomparative studies for a maximum score of 16, and 12 criteria are applied to comparative studies, for a maximum score of 24. 17 Study demographics were recorded including the intervention analyzed, number of fractures assessed, gender, time to ROM, and follow-up (Table 1). All available data for outcomes of interest were extracted from each article, including finger ROM (TAM, metacarpal phlangeal joint [MCP] motion, proximal interphalangeal joint [PIP] motion, distal interphalangeal joint [DIP] motion, distance to palmar curve, and extension lag), DASH scores (Table 2), and complications (Table 3).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of literature review process including inclusion and exclusion criteria.
Figure 2.
Comparison of 2.7 dynamic compression plating system versus low-profile plate 1.1 to 1.3 mm.
Table 1.
Study Characteristics Including Design, Number of Fractures Assessed, Quality Score as Determined by the MINORS Criteria, Level of Evidence, and Study Demographics.
| Author (year) | Design | N | Quality score | Level of evidence | Treatment: No. of fractures | Follow-up (average) | Gender (female/male) | Time ROM start |
|---|---|---|---|---|---|---|---|---|
| Abubeih et al 12 | Randomized prospective | 50 | 14/24 | II | ORIF: 50 | 8 weeks | 5/16 | 4 days |
| Ataker et al 18 | Prospective | 22 | 11/16 | IV | ORIF: 22 | 15.4 months | 8/14 | 1 week |
| Başar et al 2 | Retrospective | 22 | 16/24 | IV | ORIF: 22 | 19.2 months | 4/18 | 1 week |
| Brei-Thoma et al 6 | Retrospective | 29 | 11/16 | IV | ORIF: 29 | 10 months | 15/17 | 2-4 days |
| Desaldeleer-Le Sant et al 1 | Retrospective multicenter | 35 | 12/16 | III | CRPP: 26 ORIF: 9 |
N/A N/A |
28/59 | 1.7 weeks |
| El-Saeed et al 10 | Prospective randomized | 40 | 21/24 | II | CRPP: 20 ORIF: 20 |
6.5 months 7.2 months |
3/17 4/16 |
1 week |
| Faruqui et al 4 | Retrospective | 50 | 16/24 | III | CRPP: 50 | 8 months | N/A | 1 week |
| Kootstra et al 9 | Retrospective multicenter | 106 | 17/24 | IV | CRPP: 63 ORIF: 43 |
3.2 years 3.5 years |
30/33 19/24 |
4 weeks Variable |
| Köse et al 3 | Retrospective | 40 | 16/24 | IV | CRPP: 18 ORIF: 22 |
16 months 16 months |
8/10 1/21 |
1 week |
| Miller et al 19 | Prospective | 40 | 12/16 | III | ORIF: 40 | 12 weeks | 10/30 | 1 week |
| Robinson et al 5 | Retrospective | 42 | 17/24 | III | ORIF: 42 | 20 weeks | 19/23 | UNK |
| Sadek 11 | Prospective randomized | 26 | 16/24 | II | CRPP: 26 | 22.8 months | 5/21 | 2 days |
| Saied and Sabet Jahromi 13 | Prospective | 61 | 14/24 | III | CRPP: 61 | 6 months | 11/50 | 2 days |
| Shewring et al 20 | Prospective | 113 | 9/16 | IV | CRPP: 113 | 11 weeks | 46/55 | 3 days |
Note. MINORS = Methodological Index for Non-Randomized Studies; ORIF = open reduction internal fixation; CRPP = closed reduction percutaneous pinning; ROM = range of motion; UNK = Unknown.
Table 2.
Weighted Outcome Data.
| Outcomes | ORIF | N | CRPP | N | P value |
|---|---|---|---|---|---|
| TAM | 223 (32) a | 256 | 228 (34) a | 314 | .07 (−0.5-10.5) b |
| DASH score | 11.7 (6.5) a | 188 | 8.2 (8.9) a | 127 | <.01* (1.8-5.2) b |
Note. ORIF = open reduction internal fixation; N = number of patients included; CRPP = closed reduction percutaneous pinning; TAM = total active motion; DASH = Disabilities of the Arm, Shoulder, and Hand.
Weighted mean (SD).
95% Confidence interval for the difference in TAM.
p < .05.
Table 3.
Complications.
| Complication | CRPP total | CRPP assessed | Percent | ORIF total | ORIF assessed | Percent | P value |
|---|---|---|---|---|---|---|---|
| Stiffness | 2 | 38 | 5.26 | 7 | 92 | 7.61 | .63 |
| Delayed/nonunion | 4 | 152 | 2.63 | 1 | 227 | 0.44 | .07 |
| Malunion | 4 | 177 | 2.26 | 12 | 237 | 5.06 | .14 |
| Superficial infection | 4 | 212 | 1.89 | 8 | 299 | 2.68 | .56 |
| Deep infection | 2 | 212 | 0.94 | 1 | 299 | 0.33 | .37 |
| Tenolysis/hardware removal | 13 | 319 | 4.08 | 30 | 299 | 10.03 | <.01 |
| Other reoperation | 3 | 319 | 0.94 | 8 | 299 | 2.68 | .10 |
Note. ORIF = open reduction internal fixation; CRPP = closed reduction percutaneous pinning.
Results
A total of 14 studies were included for analysis. Publication years ranged from 2012 to 2020. Three studies were prospective randomized trials. Four studies were prospective cohort studies, and seven were retrospective in nature. The highest level of evidence included was II (3 studies), and the lowest was IV (6 studies). For the 5 noncomparative studies, quality scores ranged from 9 to 12 out of 16. For the 9 comparative studies, quality scores ranged from 14 to 21 out of 24. All studies included had an N of at least 20, with a maximum of 113 (Table 1). Average reported follow-up ranged from 8 weeks to 3.5 years with an average reported follow-up of 15.3 months. Time from surgery until the start of ROM ranged from 2 days to up to 4 weeks, with an average time to ROM of 7 days. Of those studies that reported gender, females made up 34% of the fractures analyzed and males 66% (Table 1).
Thirteen studies included TAM data, 9 for ORIF and 7 for CRPP. The number of patients totaled 256 for ORIF and 324 for CRPP. The weighted total active ROM can be seen in Table 2 and demonstrated in Figure 3. A total of 7 studies included DASH scores, 7 for ORIF and 4 for CRPP. The number of patients totaled 256 for ORIF and 314 for CRPP. The total weighted DASH scores can be seen in Table 2 and demonstrated in Figure 4. Two of the 14 studies performed a direct comparison of CRPP to ORIF (Table 2). Of these studies, ORIF was favored for TAM (d = 1.07) and DASH (d = 0.23).
Figure 3.
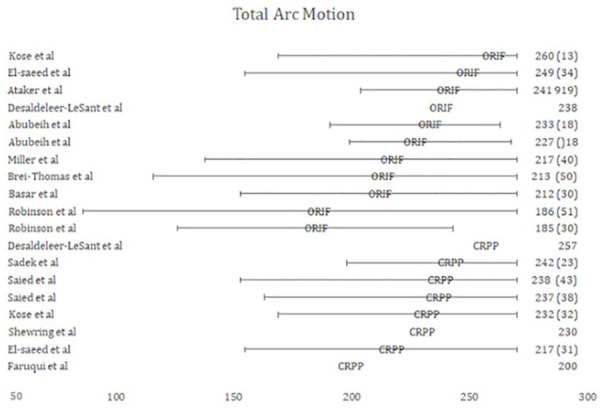
Total arc of motion with 95% confidence interval, right column shows mean (SD).
Note. ORIF = open reduction internal fixation; CRPP = closed reduction percutaneous pinning.
Figure 4.
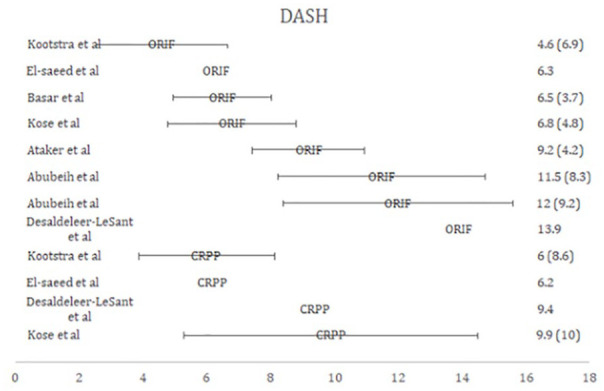
Disabilities of the Arm, Shoulder, and Hand (DASH) with 95% confidence interval, right column shows mean (SD).
Note. ORIF = open reduction internal fixation; CRPP = closed reduction percutaneous pinning.
Complications were also assessed including stiffness, delayed union/nonunion, malunion, superficial or deep infection, tenolysis/hardware removal, and other reoperation. The rate of stiffness was 5.26% for CRPP versus 7.61% for ORIF with a total of 38 versus 92 assessed with a P-value of .63. Closed reduction percutaneous pinning had a higher rate of delayed or nonunion, 2.63% compared to 0.44% for ORIF; however, this difference did not reach significance with a P-value of .07. Open reduction internal fixation had a higher rate of malunion with 5.06% versus 2.26% for CRPP with a total of 237 and 177 assessed, respectively. Again, this did not reach significance with a P-value of .14. Both superficial and deep infection rates were low between both groups. Open reduction internal fixation had a higher rate of tenolysis or hardware removal at a rate of 10.03% compared to 4.08% for CRPP, which was statistically significant with a P-value less than .01, and 2.68% for other reoperations compared to 0.94% for CRPP with a P-value of .10 (Table 3).
Discussion
Several studies have looked at CRPP versus ORIF for proximal phalanx fracture fixation; however, they are largely heterogeneous in inclusion criteria and outcome reporting. Through meta-analysis, this study sought to compare the treatment methods for unstable, extraarticular proximal phalanx fractures. Regarding TAM, there was an absolute difference of 5° between the two methods (228 versus 223), favoring CRPP, though this was not statistically significant. Normal TAM is 270°. Bain et al published on functional range of finger motion, stating that the functionally important ROM is 48%, 59%, and 60% of the MCP, PIP, and DIP joints, respectively; this suggests that the TAM achieved by both procedures is well within functional limits. 21 Prior studies of plate fixation demonstrated stiffness (TAM < 180) in 37% of fractures. 22 Regarding DASH scores, there was an absolute difference of 3.5 points (11.2 versus 8.5) favoring CRPP, which was statistically significant. However, the minimum clinically important difference for DASH score has been published to be 10.81 points. 23 Tenolysis or hardware removal was performed at a higher rate in ORIF (10.4%) versus CRPP (4.1%). However, this rate is much lower than was reported in prior studies with complication rates between 36% and 42%.16,24,25
A recent study by Köse et al published in 2018 compared low-profile plate and screw fixation to Kirschner-wire osteosynthesis for extraarticular proximal phalanx fractures and found that both methods can lead to excellent outcomes and hand function; however, mean TAM was higher and DASH scores were lower in the ORIF group compared to CRPP. 3 Another recent study published by Desaldeleer-Le Sant et al in 2017 compared surgical fixation of proximal phalanx fractures and found that functional results were best in screw fixation alone, followed by plate fixation and finally pinning. 1 Between CRPP and ORIF alone, TAM was again higher and DASH scores were lower in the ORIF group. 1 In contrast, a study published by Kootstra et al in 2020 looked only at patient-reported outcomes of proximal phalanx fractures after surgical fixation and found that patient-reported outcomes were similar among ORIF with plate and screws versus screws alone and CRPP, although unplanned reoperations were higher in plate fixation. 9 Therefore, they concluded that K-wire fixation is usually sufficient for fixation of these fractures and is associated with improved aesthetic outcome. 9 Our results corroborate with these studies, and suggest more equipoise than previous demonstrated with regard to motion and complications between ORIF and CRPP.
Limitations of this study include the limitations inherent to each individual study included. Several of the included studies were retrospective in nature with level IV evidence ratings. Additional limitations include the heterogeneity of individual studies. The exact approach and implants utilized were heterogeneous and not specified. Different postoperative rehabilitation protocols were used among the studies, which has previously been shown to have a large effect on final outcome. 18 There were also different time points at which data were recorded for each study, ranging from several weeks to over 3 years. However, it has been shown that most postoperative motion is gained by 6 weeks, with slower improvements thereafter. 19 Finally, not all articles provided complete data sets for analysis, with standard deviation being the most common value missing. The statistical analysis was therefore limited by available information and most likely would have been stronger with full data sets.
Despite these limitations, this article is the first, to our knowledge, to provide a systematic review and meta-analysis comparing the most common surgical fixation methods used for unstable proximal phalanx fractures. The specific inclusion and exclusion criteria make the results applicable to fixation of these specific fractures. In addition, the narrow date range aims to make results more applicable to new plate technology. Overall, this study shows more similar outcomes in TAM and DASH scores with ORIF and CRPP. Thus more recent data suggest ORIF may have more similar outcomes with respect to CRPP than reported in previous literature.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was not obtained as this study did not involve human subjects.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Lisa M. Kruse  https://orcid.org/0000-0002-0251-625X
https://orcid.org/0000-0002-0251-625X
References
- 1. Desaldeleer-Le Sant AS, Le Sant A, Beauthier-Landauer V, et al. Surgical management of closed, isolated proximal phalanx fractures in the long fingers: functional outcomes and complications of 87 fractures. Hand Surg Rehabil. 2017;36(2):127-135. doi: 10.1016/j.hansur.2016.08.009 [DOI] [PubMed] [Google Scholar]
- 2. Başar H, Başar B, Başçı O, et al. Comparison of treatment of oblique and spiral metacarpal and phalangeal fractures with mini plate plus screw or screw only. Arch Orthop Trauma Surg. 2015;135(4):499-504. doi: 10.1007/s00402-015-2164-3 [DOI] [PubMed] [Google Scholar]
- 3. Köse A, Topal M, Engin MÇ, et al. Comparison of low-profile plate-screw and Kirschner-wire osteosynthesis outcomes in extra-articular unstable proximal phalangeal fractures. Eur J Orthop Surg Traumatol. 2019;29(3):597-604. doi: 10.1007/s00590-018-2342-4 [DOI] [PubMed] [Google Scholar]
- 4. Faruqui S, Stern PJ, Kiefhaber TR. Percutaneous pinning of fractures in the proximal third of the proximal phalanx: complications and outcomes. J Hand Surg Am. 2012;37(7):1342-1348. doi: 10.1016/j.jhsa.2012.04.019 [DOI] [PubMed] [Google Scholar]
- 5. Robinson LP, Gaspar MP, Strohl AB, et al. Dorsal versus lateral plate fixation of finger proximal phalangeal fractures: a retrospective study. Arch Orthop Trauma Surg. 2017;137(4):567-572. doi: 10.1007/s00402-017-2650-x [DOI] [PubMed] [Google Scholar]
- 6. Brei-Thoma P, Vögelin E, Franz T. Plate fixation of extra-articular fractures of the proximal phalanx: do new implants cause less problems? Arch Orthop Trauma Surg. 2015;135(3):439-445. doi: 10.1007/s00402-015-2155-4 [DOI] [PubMed] [Google Scholar]
- 7. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg. 2008;16(10):586-595. doi: 10.5435/00124635-200810000-00004 [DOI] [PubMed] [Google Scholar]
- 8. Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000;8(2):111-121. doi: 10.5435/00124635-200003000-00005 [DOI] [PubMed] [Google Scholar]
- 9. Kootstra TJM, Keizer J, Bhashyam A, et al. Patient-reported outcomes and complications after surgical fixation of 143 proximal phalanx fractures. J Hand Surg Am. 2020;45(4):327-334. doi: 10.1016/j.jhsa.2019.08.010 [DOI] [PubMed] [Google Scholar]
- 10. El-Saeed M, Sallam A, Radwan M, et al. Kirschner wires versus titanium plates and screws in management of unstable phalangeal fractures: a randomized, controlled clinical trial. J Hand Surg Am. 2019;44(12):1091.e1-1091.e9. doi: 10.1016/j.jhsa.2019.01.015 [DOI] [PubMed] [Google Scholar]
- 11. Sadek AF. Joint sparing Kirschner-wire fixation for displaced proximal phalangeal neck fractures: randomized prospective comparative study. J Hand Surg Eur Vol. 2020;45(6):560-566. doi: 10.1177/1753193419894143 [DOI] [PubMed] [Google Scholar]
- 12. Abubeih HMA, Saleh WR, Thabet MA, et al. Extensor tendon splitting versus extensor tendon sparing approach for miniplate fixation of extraarticular proximal phalangeal fractures. Curr Orthop Pract. 2016;27(6):623-632. doi: 10.1097/BCO.0000000000000428 [DOI] [Google Scholar]
- 13. Saied AR, Sabet Jahromi M. Treatment of proximal phalanx fractures: transarticular pinning the metacarpophalangeal joint or cross pinning from the base of the proximal phalanx—a prospective study. Eur J Trauma Emerg Surg. 2019;45(4):737-743. doi: 10.1007/s00068-018-0927-6 [DOI] [PubMed] [Google Scholar]
- 14. Pun WK, Chow SP, So YC, et al. Unstable phalangeal fractures: treatment by A.O. Screw and plate fixation. J Hand Surg Am. 1991;16(1):113-117. doi: 10.1016/S0363-5023(10)80023-1 [DOI] [PubMed] [Google Scholar]
- 15. Chen SH, Wei FC, Chen HC, et al. Miniature plates and screws in acute complex Hand Injury. J Trauma. 1994;37(2):237-242. [DOI] [PubMed] [Google Scholar]
- 16. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827-832. doi: 10.1016/S0363-5023(98)80157-3 [DOI] [PubMed] [Google Scholar]
- 17. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. doi: 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 18. Ataker Y, Uludag S, Ece SC, et al. Early active motion after rigid internal fixation of unstable extra-articular fractures of the proximal phalanx. J Hand Surg Eur Vol. 2017;42(8):803-809. doi: 10.1177/1753193417709949 [DOI] [PubMed] [Google Scholar]
- 19. Miller L, Ada L, Crosbie J, et al. Pattern of recovery after open reduction and internal fixation of proximal phalangeal fractures in the finger: a prospective longitudinal study. J Hand Surg Eur Vol. 2017;42(2):137-143. doi: 10.1177/1753193416670591 [DOI] [PubMed] [Google Scholar]
- 20. Shewring DJ, Trickett RW, Smith A. Fractures at the junction of diaphysis and metaphysis of the proximal phalanges in adults. J Hand Surg Eur Vol. 2018;43(5):506-512. doi: 10.1177/1753193418766973 [DOI] [PubMed] [Google Scholar]
- 21. Bain GI, Polites N, Higgs BG, et al. The functional range of motion of the finger joints. J Hand Surg Eur Vol. 2015;40(4):406-411. doi: 10.1177/1753193414533754 [DOI] [PubMed] [Google Scholar]
- 22. Kurzen P, Fusetti C, Bonaccio M, et al. Complications after plate fixation of phalangeal fractures. J Trauma. 2006;60(4):841-843. doi: 10.1097/01.ta.0000214887.31745 [DOI] [PubMed] [Google Scholar]
- 23. Franchignoni F, Vercelli S, Giordano A, et al. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (quickDASH). J Orthop Sports Phys Ther. 2014;44(1):30-39. doi: 10.2519/jospt.2014.4893 [DOI] [PubMed] [Google Scholar]
- 24. von Kieseritzky J, Nordström J, Arner M. Reoperations and postoperative complications after osteosynthesis of phalangeal fractures: a retrospective cohort study. J Plast Surg Hand Surg. 2017;51(6):458-462. doi: 10.1080/2000656X.2017.1313261 [DOI] [PubMed] [Google Scholar]
- 25. Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res. 1987;214:59-65. [PubMed] [Google Scholar]