Abstract
Background:
Arthroplasty is commonly performed in the management of osteoarthrosis of the hand and wrist by orthopedic or plastic surgeons with a fellowship in hand. The differences between operative outcomes between the 2 groups have not been described. Therefore, we analyzed a national database to determine acute outcomes between orthopedic and plastic surgery when performing arthroplasty for osteoarthrosis of the hand and wrist.
Methods:
A retrospective cross-sectional analysis was performed by including patients with osteoarthrosis of the hand and wrist by International Classification of Diseases codes. Demographic, operative, and outcome variables were collected. Pearson χ2 and Fischer exact tests were used for categorical variables, while a Mann-Whitney U test was performed for continuous variables. Multivariate regression analysis was performed to determine strength of predictors.
Results:
There were 3721 patients who received arthroplasty for osteoarthrosis of the hand and wrist from 2007 to 2020. Most cases were performed by orthopedic surgeons (82.7%); however, there were an increasing number of surgeries performed by plastic surgeons. Most cases were performed on the intercarpal or carpometacarpal joints (81.7%). The incidence of acute complications was low (1.9%) with superficial surgical site infections (SSIs) being the most common complication. Univariate analysis found that plastic surgery may result in higher chances of superficial SSIs, but multivariate analysis indicated that there were no significant differences between the 2 groups.
Conclusion:
There were no significant differences on multivariate regression analysis between plastic and orthopedic surgeons, suggesting that both can perform arthroplasty of the hand and wrist without safety concerns.
Keywords: hand, anatomy, osteoarthritis, arthritis, diagnosis, arthroplasty, wrist, specialty, surgery, acute complications
Introduction
Osteoarthritis (OA) of the hand and wrist is prevalent in up to 56.6% of men and women in the United States. 1 Symptoms vary from patient to patient, from slight tenderness to debilitating pain with joint swelling and instability. While most causes of OA are idiopathic in origin, possible causes of OA include overuse, prior injury, certain metabolic diseases, bone malformations, and genetic predisposition. 2 When conservative measures such as anti-inflammatory medications, physical therapy, steroid injections, or splinting fail to alleviate symptoms, arthroplasty of the hand and wrist is considered 1 of the gold standards for surgical treatment. These procedures are commonly performed by hand surgeons, which is a subspecialization of general, orthopedic, or plastic surgery. Although most surgeons complete a hand fellowship, these procedures can still be performed without additional fellowship training.
There is significant variability in the training of hand surgeons. A hand surgeon can be trained in orthopedic or plastic surgery, which has different levels of training. According to the American College of Graduate Medical Education, orthopedic surgery training is at least 60 months, integrated plastic surgery is at least 72 months, and independent plastic surgery, which subsequently follows after a 5-year or longer surgical residency other than plastic surgery, is at least 36 months.3,4 If surgeons decide to do a hand fellowship, the duration is 12 months after they completed residency. 4 Therefore, the difference in training between orthopedic surgeons and plastic surgeons can vary between 1 and 4 years depending on the path. In addition, their training backgrounds result in different expertise. Studies found that orthopedic surgeons are frequently more experienced in complex and more proximal bone and joint surgeries including elbow and shoulder, whereas plastic surgeons are more familiar with soft tissue reconstruction and microsurgery.5,6
Although there is increasing involvement of various surgical specialties in the treatment of OA, there is a paucity in the literature that examines the differences between orthopedic and plastic surgery. The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) is a surgical database that prospectively collects data on surgical patients from more than 700 hospitals for 30 days after their procedure. 7 This database identifies the specialty of the surgeon performing the procedure and contains patient information including demographic data, perioperative risk factors, and complications. Therefore, we used the ACS NSQIP database from 2007 to 2020 to determine whether there were any differences in acute clinical outcomes between orthopedic and plastic surgery when performing arthroplasty for the treatment of osteoarthrosis of the hand and wrist.
Methods
Study Sample
A retrospective cross-sectional analysis was conducted using data from the ACS NSQIP database from 2007 to 2020. This database collected deidentified patient data undergoing surgery with 30-day postoperative outcomes. Our study included all patients with International Classification of Diseases, Ninth Revision or Tenth Revision codes related to osteoarthrosis of the hand and wrist and whether they received an arthroplasty procedure from an orthopedic, plastic, or general surgeon. The database could not distinguish whether the surgeon received hand fellowship training. Patients were also excluded from analysis if they had any other procedures. Current Procedural Terminology codes that were analyzed included the following: 25442 (arthroplasty with prosthetic replacement, distal ulna), 25445 (arthroplasty with prosthetic replacement, trapezium), 25446 (arthroplasty with prosthetic replacement, distal radius and partial or entire carpus), 25447 (interposition arthroplasty, intercarpal or carpometacarpal joints), 25449 (revision of arthroplasty, including removal of implant, wrist joint), 26530 (arthroplasty, metacarpophalangeal joint; single, each), 26531 (arthroplasty, metacarpophalangeal joint; with prosthetic implant, single, each), 26535 (arthroplasty, interphalangeal joint; single, each), and 26536 (arthroplasty, interphalangeal joint; with prosthetic implant, single, each). Demographic information, comorbidities, perioperative events, and 30-day postoperative complication outcome data were collected.
Study Outcomes
The primary outcomes of interest were operative complications resulting in mortality and/or return to the operating room within 30 days of the procedure. Secondary outcomes included patient readmission, superficial SSIs, deep incisional SSIs, wound dehiscence, unplanned intubation, urinary tract infection, stroke/cerebrovascular accident with neurological deficit, myocardial infarction, and sepsis. Other potential complications listed in the ACS NSQIP database did not occur in the query of the study sample.
Data Collection and Analysis
Univariate analysis was performed to determine differences in patients between orthopedic and plastic surgery. While general surgery was included in the data collection, statistical analysis was not performed due to limited sample size which would violate statistical analysis assumptions. Categorical variables including sex, race, ethnicity, body mass index (BMI), comorbidity factors, elective surgery, patient setting, wound classification, American Society of Anesthesiologists (ASA) classification, and primary and secondary outcomes were analyzed using Pearson χ2 or Fisher exact tests. Continuous variables including age, duration of anesthesia, and duration of operation were not found to have equal variance and normality was not guaranteed. Therefore, a 2-tailed Mann-Whitney U test was performed to determine differences in means. A multivariate regression analysis was performed on significant complication variables to determine the strength of the relationship between the predictor variables and complication. Significance was set at a P value of less than .05 for all analyses. Statistical analysis was performed using SPSS (IBM Corp, Released 2020, IBM SPSS Statistics Version 27.0, Armonk, New York, USA).
Results
A total of 3721 patients who were treated with arthroplasty for osteoarthrosis of the hand and wrist were queried from the 2007 to 2020 ACS NSQIP data set. Most cases were arthroplasty of the intercarpal or carpometacarpal joints (81.7%). In total, orthopedic surgeons (n = 3113, 82.7%) performed many hand arthroplasty procedures than plastic surgeons (n = 608, 16.2%) and general surgery (n = 43, 1.1%). The proportions of procedures on the distal/ulna, carpal bones, metacarpal bones, and phalanges suggest that plastic surgeons were more likely to perform on the distal regions of the hand compared with orthopedic surgeons (Table 1).
Table 1.
Frequency of Procedures Between Orthopedic and Plastic Surgery.
| CPT | Total | Orthopedic surgery (%) | Plastic surgery (%) |
|---|---|---|---|
| Arthroplasty with prosthetic replacement, distal ulna (25442) | 17 | 14 (82.4) | 3 (17.6) |
| Arthroplasty with prosthetic replacement, trapezium (25445) | 90 | 68 (75.6) | 22 (24.4) |
| Arthroplasty with prosthetic replacement; distal radius and partial or entire carpus (25446) | 22 | 20 (90.9) | 2 (9.1) |
| Interposition arthroplasty, intercarpal or carpometacarpal joints (25447) | 3039 | 2584 (85) | 455 (15) |
| Revision of arthroplasty, including removal of implant, wrist joint (25449) | 6 | 5 (83.3) | 1 (16.7) |
| Arthroplasty, metacarpophalangeal joint; single, each (26530) | 89 | 67 (75.3) | 22 (24.7) |
| Arthroplasty, metacarpophalangeal joint; with prosthetic implant, single, each (26531) | 139 | 108 (77.7) | 31 (22.3) |
| Arthroplasty, interphalangeal joint; single, each (26535) | 107 | 77 (72) | 30 (28) |
| Arthroplasty, interphalangeal joint; with prosthetic implant, single, each (26536) | 212 | 170 (80.2) | 42 (19.8) |
Note. CPT = Current Procedural Terminology.
P value significance <.05.
Demographic analysis indicates that orthopedic surgeons treated patients who were similar in age (mean, 63 ± 9.1 vs 63 ± 9.7 years; P = .67), sex (women 72.6% vs 73%, P = .84), race (white 93.5% vs 96.0%, P = .44), ethnicity (non-Hispanic 96.5% vs 95.1%, P = .22), and BMI (P = .73) to patients of plastic surgeons (Table 2).
Table 2.
Demographic Details.
| Variables | Total | Orthopedic surgery | Plastic surgery | P value |
|---|---|---|---|---|
| Cases | 3113 (83.7%) | 608 (16.3%) | ||
| Age, mean, y | 63 ± 9.1 | 63 ± 9.7 | .67 | |
| Sex | .84 | |||
| Female | 2705 | 2261 (72.6%) | 444 (73%) | |
| Male | 1016 | 852 (27.4%) | 164 (27%) | |
| Race | .44 | |||
| American Indian or Alaska Native | 16 | 15 (0.6%) | 1 (0.3%) | |
| Asian | 56 | 53 (2.1%) | 3 (0.9%) | |
| Black or African American | 101 | 92 (3.6%) | 9 (2.8%) | |
| Native Hawaiian or Pacific Islander | 7 | 7 (0.3%) | 0 (0%) | |
| White | 2718 | 2410 (93.5%) | 308 (96%) | |
| Ethnicity | .22 | |||
| Non-Hispanic | 2717 | 2445 (96.5%) | 272 (95.1%) | |
| Hispanic | 102 | 88 (3.5%) | 14 (4.9%) | |
| BMI | .73 | |||
| <18.5 | 34 | 762 (24.8%) | 162 (27.2%) | |
| 18.5-24.9 | 924 | 1008 (32.8%) | 197 (33.1%) | |
| 25-29.9 | 1205 | 712 (23.1%) | 130 (21.8%) | |
| 30-34.9 | 842 | 324 (10.5%) | 63 (10.6%) | |
| 35-39.9 | 387 | 240 (7.8%) | 40 (6.7%) | |
| ≥40 | 280 | 30 (1%) | 4 (0.7%) |
Note. BMI = body mass index.
P value significance <.05.
Comorbidity analysis shows that orthopedic surgeons were more likely to have patients with hypertension (47.4% vs 41.1%, P < .01) and a history of severe chronic obstructive pulmonary disease (COPD) (5.5% vs 3.5%, P = .04). Plastic surgeons were more likely to have patients with a previous percutaneous coronary intervention (PCI) (0.4% vs 1.3%, P < .01). Other risk factors including diabetes (12.7% vs 12%, P = .64) and smoking (12.5% vs 12.7%, P = .91) were similar between the 2 specialties (Table 3).
Table 3.
List of Comorbidities.
| Variables | Total | Orthopedic surgery (%) | Plastic surgery (%) | P value |
|---|---|---|---|---|
| Hypertension | 1725 | 1475 (47.4) | 250 (41.1) | <.01 |
| Diabetes | 468 | 395 (12.7) | 73 (12) | .64 |
| Smoking | 466 | 389 (12.5) | 77 (12.7) | .91 |
| History of severe COPD | 192 | 171 (5.5) | 21 (3.5) | .04 |
| Bleeding disorders | 73 | 65 (2.1) | 8 (1.3) | .21 |
| Congestive heart failure | 6 | 6 (0.2) | 0 (0) | .28 |
| Previous PCI | 22 | 14 (0.4) | 8 (1.3) | <.01 |
| Previous cardiac surgery | 12 | 10 (0.3) | 2 (0.3) | .75 |
| History of angina in 1 mo before surgery | 1 | 1 (0%) | 0 (0) | .61 |
| History of revascularization/amputation for peripheral vascular disease | 2 | 2 (0.1) | 0 (0) | .48 |
| Currently on dialysis (preoperatively) | 10 | 9 (0.3) | 1 (0.2) | .59 |
| History of transient ischemic attacks | 10 | 8 (0.3) | 2 (0.3) | .99 |
| CVA/Stroke with neurological deficit | 3 | 3 (0.1) | 0 (0) | .38 |
| CVA/Stroke with no neurological deficit | 6 | 6 (0.2) | 0 (0) | .21 |
Note. COPD = chronic obstructive pulmonary disease; PCI = percutaneous coronary intervention; CVA = cerebrovascular accident.
P value significance <.05.
Perioperative analysis shows that orthopedic surgeons were more likely to operate on patients with increased ASA classification (P < .01) but have decreased anesthesia (mean, 107 ± 43.7 vs 121 ± 42.7 minutes, P < .01) and operation times (mean, 70 ± 35.3 vs 75 ± 31.8 minutes, P < .01) compared with plastic surgeons (Table 4).
Table 4.
Perioperative Details.
| Variables | Total | Orthopedic surgery | Plastic surgery | P value |
|---|---|---|---|---|
| Elective surgery | .39 | |||
| No | 13 | 12 (0.4%) | 1 (0.2%) | |
| Yes | 3507 | 2927 (99.6%) | 580 (99.8%) | |
| Patient setting | .36 | |||
| Inpatient | 124 | 100 (3.2%) | 24 (3.9%) | |
| Outpatient | 3597 | 3013 (96.8%) | 584 (96.1%) | |
| Wound classification | .07 | |||
| Clean | 3711 | 3107 (99.8%) | 604 (99.3%) | |
| Other than clean | 8 | 6 (0.2%) | 4 (0.7%) | |
| ASA classification | <.01 | |||
| 1—No disturbance | 207 | 152 (4.9%) | 55 (9.1%) | |
| 2—Mild disturbance | 2208 | 1841 (59.3%) | 367 (60.7%) | |
| 3—Severe disturbance | 1253 | 1078 (34.8%) | 175 (28.9%) | |
| 4—Life threat | 39 | 31 (1%) | 8 (1.3%) | |
| Duration of anesthesia, mean, minutes | 107 ± 43.7 | 121 ± 42.7 | <.01 | |
| Duration of operation, mean, minutes | 70 ± 35.3 | 75 ± 31.8 | <.01 |
Note. ASA = American Society of Anesthesiologists.
P value significance <.05
While there were differences in patient comorbidity, orthopedic surgeons had no statistical differences in primary outcome of death (0.1% vs 0%, P = .53) and reoperation within 30 days (0.4% vs 0.3%, P = .84) when compared with plastic surgeons. The 2 patients who died under the orthopedic group had multiple risk factors, including increased age, BMI, and ASA classification. There were no deaths in the plastic surgery group. Superficial incisional SSI was significantly more frequent in plastic surgery than in orthopedic surgery (3.0% vs 0.4%, P < .01). Other secondary outcomes including deep incisional SSI and wound disruption were not significantly different (Table 5). General surgery had 1 case of superficial SSI with no incidence of readmission or reoperation.
Table 5.
Complication List.
| Variables | Total | Orthopedic surgery (%) | Plastic surgery (%) | P value |
|---|---|---|---|---|
| Primary outcomes | ||||
| Death | 2 | 2 (14.3) | 0 (0) | .53 |
| Reoperation | 21 | 12 (85.7) | 2 (100) | .84 |
| Secondary outcomes | ||||
| Readmission | 14 | 15 (34.1) | 6 (17.6) | .14 |
| Superficial incisional SSIs | 30 | 12 (27.3) | 18 (52.9) | <.01 |
| Deep incisional SSIs | 3 | 1 (2.3) | 2 (5.9) | .07 |
| Wound disruption | 1 | 0 (0) | 1 (2.9) | .16 |
| Unplanned intubation | 1 | 0 (0) | 1 (2.9) | .16 |
| Urinary tract infection | 17 | 13 (29.5) | 4 (11.8) | .51 |
| Stroke/CVA with neurological deficit | 2 | 2 (4.5) | 0 (0) | 1.00 |
| Myocardial infarction | 1 | 0 (0) | 1 (2.9) | .16 |
| Sepsis | 2 | 1 (2.3) | 1 (2.9) | .30 |
Note. SSIs = surgical site infections; CVA = cerebrovascular accident.
P value significance <.05.
Multivariate regression analysis was performed on superficial incisional SSIs due to the complication being significant on univariate analysis. Surgical specialty was not a significant independent risk factor for SSIs after adjusting for confounding variables (adjusted odds ratio = 9.01; 95% confidence interval, 0.70-115.72; P = .09). Other risk factors including age, sex, duration of anesthesia, duration of operation, ASA classification, hypertension, and smoking were not significant as well (Table 6).
Table 6.
Multivariate Analysis for Superficial SSIs.
| Variable | Standard error | Adjusted odds ratio | 95% Confidence interval | P value |
|---|---|---|---|---|
| Surgical specialty | ||||
| Orthopedic surgery | 1 (Reference) | |||
| Plastic surgery | 1.3 | 9.01 | 0.70-115.72 | .09 |
| Age | 0.07 | 0.93 | 0.81-1.08 | .33 |
| Sex | ||||
| Female | 1 (Reference) | |||
| Male | 1.36 | 1.77 | 0.12-25.31 | .68 |
| Duration of anesthesia | 0.03 | 1 | 0.94-1.06 | .94 |
| Duration of operation | 0.04 | 0.99 | 0.91-1.07 | .77 |
| ASA classification | ||||
| 1—No disturbance | 3340.71 | 0 | 0-Inf | 1 |
| 2—Mild disturbance | 1 (Reference) | |||
| 3/4—Severe/Life threatening | 1.4 | 1.8 | 0.12-27.8 | .67 |
| Hypertension | 1.41 | 0.52 | 0.03-8.3 | .64 |
| Smoking | 1.44 | 1.71 | 0.10-28.51 | .71 |
Note. SSIs = surgical site infections; ASA = American Society of Anesthesiologists.
P value significance <.05.
Discussion
Hand surgery can be performed by general orthopedic, plastic, and general surgeons as well as those who subspecialize in hand. Most hand surgeons in the United States are orthopedic surgeons. However, the specialty is becoming more heterogeneous as hand fellowships are also available to both general and plastic surgeons. Although the number of fellowship positions is still dominated by orthopedic surgeons (n = 156, 82.5%) when compared with plastic (n = 23, 12.2%) and general (n = 10, 5.3%) surgeons in 2022, training availability allows for surgeons of different backgrounds to share their expertise. 8 With varying surgical specialties involved with hand surgery, it is unclear whether there are differences in complications. Therefore, we analyzed the ACS NSQIP database to show that there are no differences in 30-day postoperative morbidity or mortality of arthroplasty of the hand and wrist for the treatment of osteoarthrosis between plastic and orthopedic surgeons. It should be noted that the ACS NSQIP database does not indicate whether surgeons have completed a hand fellowship.
Most arthroplasty procedures were performed by orthopedic surgeons. This is likely as there are a larger amount of orthopedic-trained hand surgeons than plastic-trained hand surgeons. 9 However, there have been an increasing number of cases performed by plastic surgeons within the last decade (Figure 1). Our analysis showed that most cases were intercarpal or carpometacarpal joint repairs. When comparing the ratio of proximal and distal procedures, plastic surgeons were more likely to perform on the distal aspects of the hand, including interphalangeal and metacarpophalangeal arthroplasty, than orthopedic surgeons. Similarly, studies found that distal hand fractures and trauma were more likely to be treated by plastic surgeons, and proximal hand fractures and trauma were more likely to be treated by orthopedic surgeons.10,11 This is potentially a result of the different residency and fellowship trainings as orthopedic surgeons have been found to be more involved with wrist reconstruction.6,12,13 Therefore, it would be beneficial for hand fellowships to consider diversifying the curriculum, lengthening fellowship programs, or expanding residency training.14,15
Figure 1.
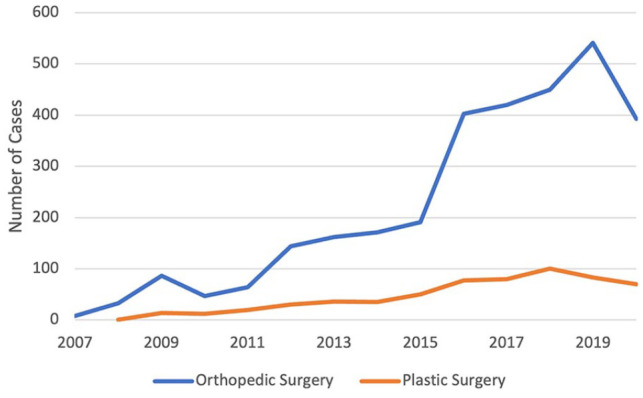
Distribution of arthroplasty cases between orthopedic and plastic surgery from 2007 to 2020.
The patient populations were similar for demographic and comorbidities. Slight differences included increased hypertension (47.4% vs 41.1%) and COPD (5.5% vs 3.5%) for the orthopedic patients and increased previous PCI (1.3% vs 0.4%) for the plastic surgery patients. While operative findings demonstrated that orthopedic surgeons finished their procedures faster than plastic surgeons (mean, 70 ± 35.3 vs 75 ± 31.8 minutes), these differences were not clinically significant. Time difference may be attributed to the increased amount of bone and joint repairs orthopedic surgeons received during residency.16,17
Our analysis demonstrated that the overall incidence of complications was low (1.91%) in hand arthroplasty. There were no significant differences between major complications including mortality, reoperation, or readmission. Surgical site infection was the most prominent complication (0.89%), and is consistent with previous studies.18,19 While plastic surgery was found to be statistically significant for increased superficial SSIs on univariate analysis, multivariate analysis to control for risk factors including age, sex, ASA classification, anesthesia time, and operation time showed no statistical significance. The univariate findings may be associated with the slight differences in operative times. In addition, the heterogeneous training backgrounds as well as surgeon variability in diagnosing, reporting, and treating infections may result in differences. For example, plastic surgery may be more familiar in recognizing skin and soft tissue infections due to their training background and may potentially be more likely to diagnose and treat them. Other studies also showed that plastic and orthopedic surgeons have comparable outcomes in safety and quality when comparing 30-day perioperative complications and reoperation following upper extremity fractures and upper extremity amputations.10,20 Interestingly, 1 study found that insurance status and location of patients increased the odds of acute postoperative visits. 19 This information is not provided in the ACS NSQIP data set and could not be further investigated. Overall, our findings indicate that there are no differences in acute postoperative outcomes in hand arthroplasty patients for the treatment of osteoarthrosis between plastic and orthopedic surgeons.
The ACS NSQIP data set has several limitations due to its inherent structure: (1) the data set collects information for only 30 days after the operation and long-term complications including joint instability, prosthesis fractures, and functional outcomes could not be analyzed; (2) datapoints are limited and certain data that could have influenced complications including antibiotic use, patient location, insurance status, and prosthesis manufacturers could not be collected as well; (3) hospitals voluntarily submit data, which introduces a selection bias and is not inclusive of national data; and (4) The database does not indicate whether the surgeon has completed a hand fellowship or multiple residency training.
Despite these limitations, our study analyzed a large data set to show no complication differences between surgical specialties for hand arthroplasty. To control for confounding variables, we created a specific query to filter out unwanted cases and performed a multivariate analysis. For future studies, it would be beneficial to perform a prospective study that identifies risk factors for long-term complications that could not otherwise be investigated using the ACS NSQIP data set.
Conclusion
Hand surgery is a heterogeneous field that consists of multiple surgical specialties. While there have been a historically larger number of procedures performed by orthopedic surgeons, plastic surgeons are becoming more involved. Our study analyzed the ACS NSQIP data set to determine perioperative complications for hand and wrist arthroplasty between orthopedic and plastic surgeons. There were no significant differences on multivariate regression analysis, suggesting that both surgical specialties can confidently perform hand osteoarthrosis care without safety concerns. As previous studies have shown that residency and fellowship training is associated with the type of hand procedures performed, it will be beneficial for programs to diversify curriculum to ensure well-rounded surgeons.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects. No experiments on animals were performed for this study. No experimental procedures were performed in any human subject for this study.
Statement of Informed Consent: Informed consent was not needed to conduct this study as all information was deidentified.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jason T. Pham  https://orcid.org/0000-0002-6563-1570
https://orcid.org/0000-0002-6563-1570
Data Availability Statement: American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
References
- 1. Haugen IK, Magnusson K, Turkiewicz A, et al. The prevalence, incidence, and progression of hand osteoarthritis in relation to body mass index, smoking, and alcohol consumption. J Rheumatol. 2017;44(9):1402-1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Palazzo C, Nguyen C, Lefevre-Colau MM, et al. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):134-138. [DOI] [PubMed] [Google Scholar]
- 3. Accreditation Council for Graduate Medical Education. ACGME plastic surgery overview. https://www.acgme.org/specialties/plastic-surgery/overview/. Accessed June 7, 2023.
- 4. Accreditation Council for Graduate Medical Education. ACGME orthopaedic surgery overview. https://www.acgme.org/specialties/orthopaedic-surgery/overview/. Accessed June 7, 2023.
- 5. Aliu O, Chung KC. A role delineation study of hand surgery in the USA: assessing variations in fellowship training and clinical practice. Hand (N Y). 2014;9(1):58-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Silvestre J, Upton J, Chang B, et al. The impact of specialty on cases performed during hand surgery fellowship training. J Bone Joint Surg Am. 2018;100(5):e29. [DOI] [PubMed] [Google Scholar]
- 7. American College of Surgeons. ACS NSQIP pediatric participant use data file. https://www.facs.org/quality-programs/childrens-surgery/pediatric/program-specifics/quality-support-tools/puf. Accessed June 7, 2023.
- 8. NRMP. Hand Surgery fellowship match. https://www.nrmp.org/fellowship-applicants/participating-fellowships/hand-surgery-match/. Accessed June 18, 2022.
- 9. Rios-Diaz AJ, Metcalfe D, Singh M, et al. Inequalities in specialist hand surgeon distribution across the United States. Plast Reconstr Surg. 2016;137(5):1516-1522 [DOI] [PubMed] [Google Scholar]
- 10. Wang JH, Du JY, Tu LA, et al. A comparison of 30-day perioperative complications for open operative care of distal upper-extremity fractures treated by orthopedic versus plastic surgeons: a study of the national surgical quality improvement (NSQIP) database. J Hand Surg Glob Online. 2020;2(2):84-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dasari CR, Sandhu M, Wisner DH, et al. Approaches to distal upper-extremity trauma: a comparison of plastic, orthopedic, and hand surgeons in academic practice. Ann Plast Surg. 2016;76(suppl 3):S162-S164 [DOI] [PubMed] [Google Scholar]
- 12. Mehta K, Pierce P, Chiu DTW, et al. The effect of residency and fellowship type on hand surgery clinical practice patterns. Plast Reconstr Surg. 2015;135(1):179-186 [DOI] [PubMed] [Google Scholar]
- 13. Silvestre J, Thomson JG, Thompson TL, et al. Analysis of strengths in exposure to cases during plastic and orthopaedic hand surgery fellowships. J Am Acad Orthop Surg. 2022;30:721-727. doi: 10.5435/JAAOS-D-22-00118. [DOI] [PubMed] [Google Scholar]
- 14. Jupiter J. Hand surgery fellowships: time for reconsideration. Tech Hand Up Extrem Surg. 2011;15(4):197. [DOI] [PubMed] [Google Scholar]
- 15. Kakar S, Bakri K, Shin AY. Survey of hand surgeons regarding their perceived needs for an expanded upper extremity fellowship. J Hand Surg Am. 2012;37(11):2374-2380 [DOI] [PubMed] [Google Scholar]
- 16. Noland SS, Fischer LH, Lee GK, et al. Essential hand surgery procedures for mastery by graduating orthopedic surgery residents: a survey of program directors. J Hand Surg Am. 2013;38(4):760-765 [DOI] [PubMed] [Google Scholar]
- 17. Noland SS, Fischer LH, Lee GK, et al. Essential hand surgery procedures for mastery by graduating plastic surgery residents: a survey of program directors. Plast Reconstr Surg. 2013;132(6):977e-984e [DOI] [PubMed] [Google Scholar]
- 18. Oriel BS, Chen Q, Itani KM. The impact of surgical hand antisepsis technique on surgical site infection. Am J Surg. 2017;213(1):24-29. [DOI] [PubMed] [Google Scholar]
- 19. Menendez ME, Lu N, Unizony S, et al. Surgical site infection in hand surgery. Int Orthop. 2015;39(11):2191-2198. [DOI] [PubMed] [Google Scholar]
- 20. Du JY, Wang JH, Coquillard CL, et al. Comparing plastic surgeon versus orthopedic surgeon outcomes following distal upper extremity amputations: a study of the National Surgical Quality Improvement Program (NSQIP) database. Plast Surg (Oakv). 2021;29(2):110-117. [DOI] [PMC free article] [PubMed] [Google Scholar]


