Abstract
Introduction
Humanitarian settings are underserved by HIV self-testing (HIV-ST).
Methods
We conducted a randomized controlled trial to evaluate the effectiveness of HIV-ST (Arm 1), HIV-ST alongside edutainment comics (Arm 2), and edutainment comics (Arm 3), compared with the standard of care (SOC), in increasing HIV testing with refugee youth aged 16–24 in the Bidi Bidi Refugee Settlement, Uganda. Intervention effects on HIV testing at 3-month follow-up (T2) were assessed using generalized estimating equation models alongside open-ended questions.
Results
Retention was 98% (n = 117/120) at T2. In adjusted analyses compared with the SOC, HIV testing changes from baseline to T2 were highest in Arm 2 (adjusted odds ratio [aOR]: 8.46; 95% confidence interval [CI]: 2.87–24.97), followed by Arm 3 (aOR: 4.14; 95% CI: 1.58–10.87), with no significant differences in Arm 1.
Conclusion
HIV self-testing is feasible for refugee youth in Uganda and can be supplemented with edutainment comics to advance HIV prevention efforts.
Keywords: HIV self-testing, Uganda, refugees, youth, edutainment comics, intervention
Plain Language Summary:
Findings from an HIV self-testing and comic intervention with refugee youth in a humanitarian setting in Uganda.
Background
HIV vulnerabilities among refugee youth are shaped by a combination of structural (eg, limited health infrastructure), social (eg, HIV-related stigma), and relational (eg, gender-based violence) factors in humanitarian settings that constrain access to HIV prevention services. 1 An effective HIV response includes facilitating uptake of HIV prevention services, including testing. 2 One such strategy, HIV self-testing, has a rich evidence base3–5 of effectiveness in reducing HIV testing access barriers in low- and middle-income countries. 1 Although HIV self-testing is particularly promising among youth, it is understudied among refugee youth in low- and middle-income humanitarian settings. 6 There are over 103 million forcibly displaced persons worldwide, 7 and Uganda is Africa's largest refugee-hosting nation, with over 1.5 million refugees. 8 While a recent Ugandan study reported the effectiveness of HIV self-testing in improving HIV testing uptake among urban refugees in Kampala, 9 to date, HIV self-testing has not been implemented in rural refugee settlement contexts, where 91% of Uganda's refugees reside. 8
HIV self-testing is a youth-friendly approach10,11 that may be particularly beneficial when offered alongside peer support. A recent systematic review, which included studies conducted in Africa, supported the use of HIV self-testing peer support. 12 Research in Uganda among young women who participated in a peer-delivered HIV self-testing and PrEP intervention reported that the peer-delivered model was confidential, provided social support, increased knowledge about HIV self-testing, and offered benefits such as removal of HIV testing barriers (eg, transportation) in healthcare settings. 13 Youth in Kenya reported the importance of acquiring social support throughout the HIV self-testing process, such as receiving linkages to HIV care and counselling and having support from a mentor. 14 Additionally, youth described the importance of their peers championing HIV self-testing within the community to improve uptake of HIV testing. 14 There is less research on HIV self-testing among refugee youth, who may experience disruptions to social support networks that could potentially mitigate barriers to accessing HIV services.15,16 For example, an HIV self-testing trial among urban refugees in Kampala found that offering HIV self-test kits alongside peer support via text messages was associated with reduced adolescent sexual and reproductive health stigma. 9 Support and stigma reduction are key considerations in developing tailored HIV services for humanitarian settings.15,17–19
Comic books are a form of graphic medicine whereby images are juxtaposed by text reflecting internal (eg, thoughts) and external (eg, dialogue) narratives and are used to share health information, 20 yet they are understudied in the context of HIV self-testing. Using comics for information sharing—also known as “edutainment”—is a youth-friendly approach used to advance knowledge of, and engagement with, sexual and reproductive health issues. For example, comic books were used in Kenya to reduce HIV-related stigma 21 and to share information with youth on contraception, 22 and with adolescents in the United States on HPV vaccination. 23 A comic book post-rape care intervention among refugee youth in Uganda increased post-exposure prophylaxis knowledge and acceptance, increased resilient coping, reduced depression, and reduced sexual violence stigma.24,25 In fact, one youth in the post-rape care study reported the need for comic books to address topics such as HIV testing. 26 There are knowledge gaps regarding the utility of comic books, a low-cost approach, to support self-care approaches such as HIV self-testing and HIV education in humanitarian settings where refugees have constrained access to health workers. 6
To address these knowledge gaps regarding innovative HIV testing strategies in humanitarian settings, we conducted a randomized controlled trial in Bidi Bidi Refugee Settlement, Uganda's second-largest refugee settlement with a population of over 193,000 refugees and asylum seekers, largely from South Sudan. 27 The primary study aim was to compare the effectiveness of HIV self-testing alone, HIV self-testing alongside edutainment comics, and edutainment comics alone, compared to the standard of care in increasing HIV testing uptake among refugee youth in Bidi Bidi Refugee Settlement.
Methods
Study Design
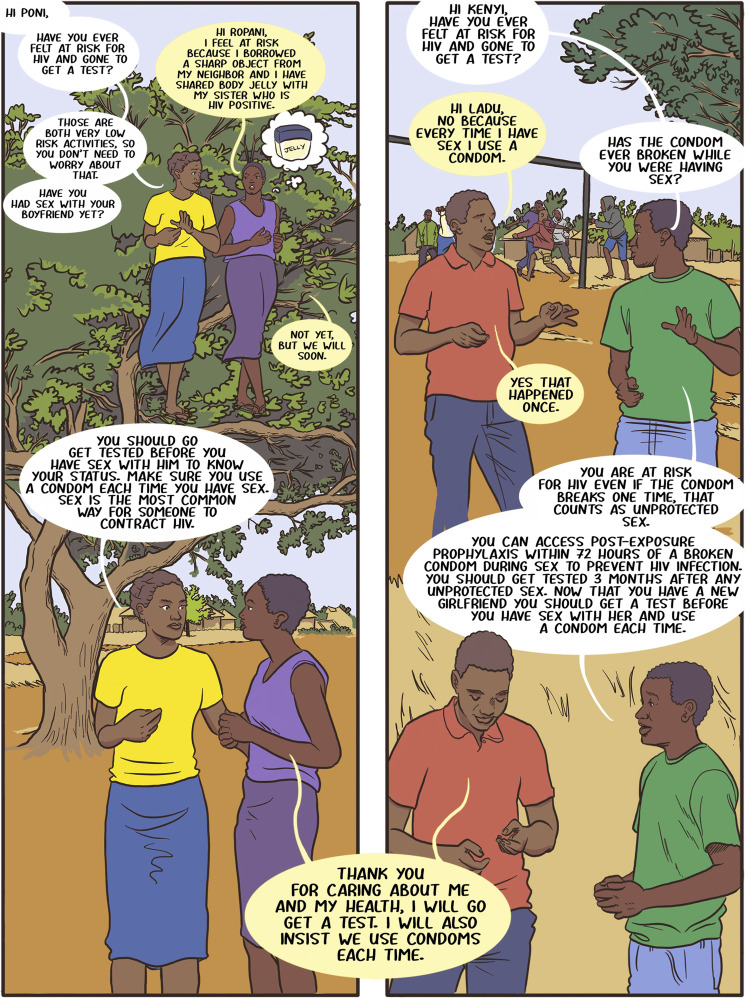
Todurujo na Kadurok (roughly translated to “Empowering Youth” in Bari) was a four-arm randomized controlled trial conducted in Bidi Bidi Refugee Settlement, Uganda. The study design is detailed elsewhere, 28 and the trial is registered at ClinicalTrials.gov (#NCT05213689). In brief, we conducted a qualitative formative phase with focus groups with refugee youth to create a new edutainment comic about HIV testing barriers and facilitators in Bidi Bidi, following detailed processes of qualitative comic book mapping developed in this context. 29 These processes included academics, community-based collaborators, and refugee youth peer researchers working together to develop comic book scenarios based on qualitative data (eg, in our case, focus groups) and aligned with theory (eg, in our case, the HIV prevention cascade 30 dimensions of motivation, access, and effective use). 26 An example page of the comic book is shown in Figure 1.
Figure 1.
Example of the edutainment comic developed for the Todurujo na Kadurok HIV self-testing and edutainment comic randomized controlled trial with refugee youth in Bidi Bidi, Uganda.
We then implemented a randomized controlled trial to test the effectiveness of the following: Arm 1: HIV self-testing and the edutainment comic; Arm 2: HIV self-testing alone; Arm 3: edutainment comic alone; and Arm 4: standard of care. Participants provided informed written consent, and data were collected at baseline (Time 1) directly prior to the intervention and at 3-month follow-up (Time 2). The effectiveness of HIV self-testing and edutainment comics was measured by changes between Times 1 and 2 in HIV testing uptake and HIV status knowledge, and secondary outcomes (HIV-related stigma, HIV knowledge, condom use self-efficacy, condom use experiences, adolescent sexual and reproductive health stigma, and sexual relationship power).
Participants and Recruitment
Four villages from two zones in Bidi Bidi (Zone 3: villages 5 and 14; Zone 4 Annex: villages 5 and 7) were purposively selected for the study, and these villages were geographically separated to avoid contamination. These villages also had established relationships with community health centres through the local community-based collaborators, Uganda Refugee Disaster and Management Council (URDMC). Villages were randomly assigned to a study arm, such that all participants from the same village were enrolled in the same study arm. Participants within each village were conveniently sampled by peer-driven recruitment from eight peer navigators, who were young refugees aged 20–24 years living in Bidi Bidi. Inclusion criteria included the following: living in one of the four villages in Bidi Bidi; identifying as a refugee/displaced person; aged 16–24 years; and able to speak and read at least one study language (English, Bari, Juba Arabic).
Intervention and Control Conditions
Participants in the HIV self-testing arms received two HIV self-test kits (OraQuick Rapid HIV-1/2 Antibody Test, OraSure Technologies) at Time 1, along with verbal, written, and visual instructions. Participants in the edutainment comic arms received a hard copy of the comic book at Time 1 in their preferred language (English, Bari or Juba Arabic); after baseline data collection, a peer navigator met each participant to read the comic together to improve understanding of key messages and provide participants with the opportunity to create their own dialogue on blank comic pages, aligned with a participatory approach to comic-based research. 29 All arms, including the standard of care, received information on accessing support from peer navigators and URDMC as needed to access confirmatory testing and HIV services at local health centers. Participants in the standard of care arm had access to free HIV testing at health centers in Bidi Bidi.
Data Collection
Data were collected in person (or by phone at Time 2 to reduce loss to follow-up) using tablet-based standardized questionnaires administered by trained research assistants in one of the three study languages using SurveyCTO, a secure application (Dobility, Cambridge, USA). 31 All participants were given linkage-to-care cards that had their participant ID and space for the healthcare provider to write the date and circle “+” or “‒” to indicate a positive/negative HIV confirmatory test result. Participants were instructed to bring these cards to participating health centers if they went for confirmatory testing, healthcare providers were instructed to complete the cards, and the cards were collected from health centers at Time 2. Socio-demographic and sexual history data were collected at baseline (Time 1). Data on primary outcomes (HIV testing uptake, HIV status knowledge) and secondary outcomes (HIV self-test kit use, HIV-related stigma, HIV knowledge, safer sex efficacy, condom use, adolescent sexual and reproductive health stigma, and sexual relationship power) were collected at Time 1 and Time 2.
Open-ended questions relevant to each study arm were collected at Time 2 with regards to why confirmatory testing was sought (study arms 1 and 2: “Why did you get a confirmatory test if you tested negative using the self-test kit?,” and study arms 3 and 4: “Why did you get a confirmatory test if you tested negative on the first HIV test?”) and assessed participants’ experiences of the interventions (study arms 1 and 2: “Is there anything else you want to share about the HIV self-test kit?,” and study arms 1 and 3: “Is there anything else you want to share about the comic book?”). Research assistants recorded participants’ responses in free-text fields in the tablet-based questionnaire in English. If the questionnaire was administered in Bari or Juba Arabic, a Peer Navigator would help translate so that the free-text response could be recorded in English.
Primary Outcome Measures
HIV testing uptake was self-reported and assessed by whether the participant had ever had an HIV test at Time 1 compared to Time 2. This was described in two ways: new test and repeat test. A “new test” was defined as those who had never had an HIV test at Time 1 but reported an HIV test between Time 1 and Time 2, compared to participants who had an HIV test at Time I (binary measure). A “repeat test” was defined as those who had an HIV test at Time 1 and reported an HIV test between Time 1 and Time 2, compared to participants who either: (a) had an HIV test at Time 1 but not at Time 2, or (b) had no HIV test at Time 1 regardless of the Time 2 test (binary measure).
HIV status knowledge was a composite variable assessed with two indicators: 1) a comparison between participants’ self-report of receiving a confirmatory HIV test and whether a linkage-to-care card was recorded by the health center, and 2) self-report of HIV serostatus and alignment with the clinic's HIV test result. HIV status knowledge was thus based on Time 2 survey data and linkage to care cards collected from five participating health centers, located in Zone 3 and Zone 4 Annex. HIVST kit use was assessed at Time 2 for the HIVST arms and included self-report of ever using the kit, when and where it was used, and whether they sought support to use the kit.
Secondary Outcome Measures
HIV-related stigma was measured using a questionnaire on public attitudes about people with HIV 32 (Cronbach's alpha = 0.78). HIV knowledge was assessed with the Brief HIV Knowledge Questionnaire 33 (Cronbach's alpha = 0.68). The Condom Use Self-Efficacy scale34,35 was used to assess safer sex efficacy (Cronbach's alpha = 0.86). We assessed condom use at last sex (yes/no) and past 3-month consistent condom use (always vs not always) at Times 1 and 2. The Adolescent Sexual and Reproductive Health Stigma scale, validated in Uganda 36 and adapted from Hall et al., 37 was used to assess adolescent sexual and reproductive health stigma (Cronbach's alpha = 0.74). Sexual relationship power (Cronbach's alpha = 0.78) was measured with the relationship control (Cronbach's alpha = 0.72) and decision-making dominance (Cronbach's alpha = 0.80) 38 subscales.
Some secondary outcomes (linkage to confirmatory testing; HIV care after reporting a positive result; access to other sexual and reproductive health services at health centers) specified in the protocol 28 are not reported as they were no longer relevant due to the results (ie, none of the participants reported a positive HIV test result) or were not reported by participating health centers.
Data Analysis
Descriptive statistics were used to describe socio-demographic characteristics and sexual history at baseline. Means and standard deviation (SD) or median and the interquartile range (IQR) were used for continuous variables and numbers and percentages for categorical variables. Differences in baseline characteristics between arms were assessed using two-sample t-tests for means and chi-square tests for proportions. A flow diagram was used to illustrate participant flow from consent and enrollment to baseline and follow-up visits. A sample size of n = 105 was required for multivariable regression analyses (effect size: 0.2, power: 0.95, tested predictors: n-5, critical F: 2.306) as calculated with G*Power 3.1, 39 and to prepare for 15% attrition, we included a sample size of n = 120.
The primary analysis used intention-to-treat methods (ie, data from participants were analyzed according to their allocation, irrespective of whether they received the intervention) as per the protocol. 28 Test for trend in change in HIV testing from Time 1 to Time 2 was assessed using the Wilcoxon signed-rank test among all participants and by study arm. New HIV test, repeat HIV test, and other outcomes assessed only at Time 2 (HIV status knowledge, HIV self-test kit use and acceptability) were reported using descriptive statistics, and differences between arms were assessed using chi-square tests. Outcomes based on validated scales were included in the primary analysis if the Cronbach's alpha was ≥0.60.40,41 Intervention effects on primary and secondary outcomes at Time 2 were assessed using generalized estimating equation (GEE) models with robust standard errors, accounting for within-subject correlation using an unstructured correlation matrix. Logistic GEE regression models with the logit link were used for binary outcomes, and odds ratios, 95% confidence intervals (CIs), and p-values were reported. Linear GEE regression models with the identity link were used for continuous outcomes, and beta coefficients, 95% CIs, and p-values were reported. Models were analyzed and we report both unadjusted and adjusted findings for the relevant outcome measure at baseline, pre-specified covariates (age, gender, length of stay in Uganda), and covariates that were imbalanced at baseline (p ≤ .05). However, if imbalanced covariates perfectly predicted failures in the outcome, they were not adjusted for in models (ie, education, same-gender sexual practices). All regression analyses were performed among participants who had outcomes measured at Times 1 and 2, and therefore, those who were lost to follow-up were not included in outcome analyses.
Secondary analysis was conducted including all participants together and assessing changes in primary and secondary outcomes due to participating in the study at large between Time 1 and Time 2, using time as the primary exposure. The same modeling procedures were used for the primary analysis, including logistic GEE regression models for categorical outcomes and linear GEE regression models for continuous outcomes with robust standard errors and accounting for within-subject correlation using an unstructured correlation matrix. As a sensitivity analysis, to account for any possible confounding of the treatment effect by study arm, we considered methods appropriate for an observational pre-post design by running a difference-in-difference analysis comparing Time 1 when no participants were treated and Time 2 when three of the study arms were considered as treated (ie, any intervention assessed together) and the standard of care arm as untreated. All statistical analyses were conducted using STATA version 16.1 (StataCorp, College Station, TX, USA).
Qualitative responses from Time 2 were coded by two trained research assistants using Dedoose software (SocioCultural Research Consultants, LA, USA)42–44 with thematic analysis approaches to identify preliminary codes.45,46 Thematic analysis was informed by the Consolidated Framework for Implementation Research (CFIR) to understand the actual implementation process and innovation success of the HIV self-testing and edutainment comic interventions in the Bidi Bidi Refugee Settlement humanitarian setting. 42 The CFIR was chosen because it aims to explain implementation barriers and facilitators to inform the implementation strategies that best address contextual determinants. Quotes were collated into sub-themes and mapped onto two CFIR domains: implementation and innovation outcomes. 43 The actual implementation outcome domain captures strategies and activities used to deliver the innovation, and considers the ways in which implementation outcomes are shaped by antecedent factors such as acceptability and feasibility. 42 The innovation outcome domain includes the impact of the innovation on recipients as well as recipient experiences with the innovation that shape outcomes—recipients are not often included in assessing implementation outcomes but can offer valuable insights. By centering “the human-beings impacted by Innovation Outcomes, the CFIR Outcomes Addendum will help researchers and organizations orient to values of humanism and equity” (7). 42
Ethics
Research ethics board approval was provided by the Mildmay Uganda Research Ethics Committee (REC REF 0802-2021), Uganda National Council for Science and Technology (SS884ES), and the University of Toronto Research Ethics Board (37496). The trial was registered at ClinicalTrials.gov (#NCT05213689). All participants provided written informed consent prior to study enrollment.
Results
Participant Characteristics
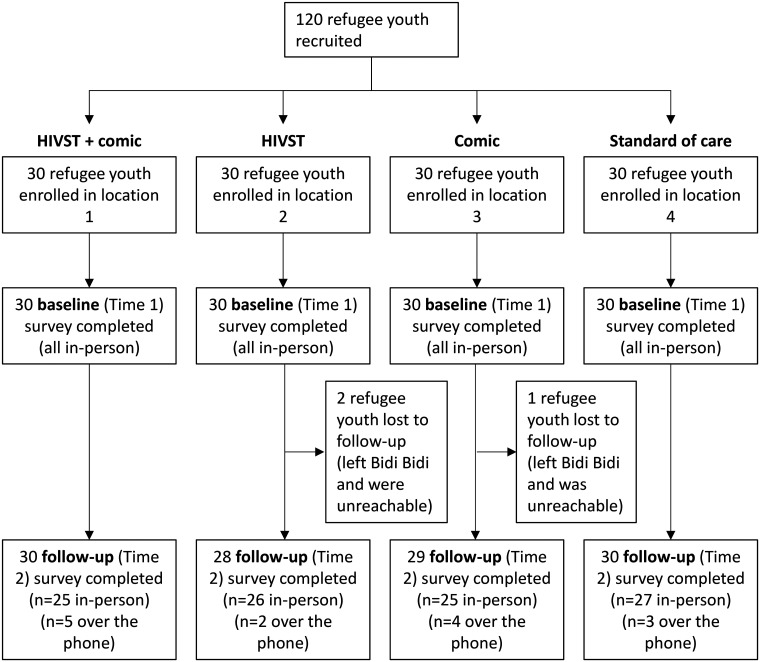
A total of n = 120 refugee youth were enrolled with n = 30 refugee youth randomized to each study arm (Figure 2).
Figure 2.
Flow chart of the participation of refugee youth enrolled in the Todurujo na Kadurok HIV self-testing and edutainment comic randomized controlled trial in Bidi Bidi, Uganda.
Ninety-eight percent (n = 117/120) of youth were followed up at 3 months (Time 2). Participant characteristics (n = 120) are detailed in Table 1; half were cisgender women and half were cisgender men, with a mean age of 20 years (SD = 2.30). Baseline characteristics were similar between study arms apart from the level of education, vaginal sex history, and same-gender sexual practices, which were included in adjusted models.
Table 1.
Baseline Characteristics of Refugee Youth Participants (n = 120) in the Todurujo na Kadurok (Empowering Youth) Randomized Controlled Trial Overall and by Study Arm in Bidi Bidi Refugee Settlement, Uganda.
| All participants | Standard of Care (SOC) | HIV self-testing arm (HIVST) | Comic arm | HIVST + comic arm | p | |
|---|---|---|---|---|---|---|
| Participants | ||||||
| Participants (n) | 120 | 30 | 30 | 30 | 30 | |
| Sociodemographic characteristics | ||||||
| Gender (n, %) | >.999 | |||||
| Women (cisgender) | 60 (50.00) | 15 (50.00) | 15 (50.00) | 15 (50.00) | 15 (50.00) | |
| Men (cisgender) | 60 (50.00) | 15 (50.00) | 15 (50.00) | 15 (50.00) | 15 (50.00) | |
| Age (mean, SD) | 20 (2.30) | 19 (2.42) | 20 (2.50) | 20 (2.53) | 19 (1.59) | .06 |
| Education (n, %) | .01 | |||||
| Less than primary school | 41 (34.17) | 18 (60.00) | 9 (30.00) | 10 (33.33) | 4 (13.33) | |
| Completed primary school | 21 (17.50) | 5 (16.67) | 4 (13.33) | 6 (20.00) | 6 (20.00) | |
| Attended some secondary school | 46 (38.33) | 5 (16.67) | 12 (40.00) | 11 (36.67) | 18 (60.00) | |
| Completed secondary school | 12 (10.00) | 2 (6.67) | 5 (16.67) | 3 (10.00) | 2 (6.67) | |
| Amount of time spent as refugee in Uganda (n, %) | .52 | |||||
| 1–5 years | 32 (26.67) | 6 (20.00) | 11 (36.67) | 5 (16.67) | 10 (33.33) | |
| 6–10 years | 83 (69.17) | 23 (76.67) | 18 (60.00) | 23 (76.67) | 19 (63.33) | |
| >10 years | 5 (4.17) | 1 (3.33) | 1 (3.33) | 2 (6.67) | 1 (3.33) | |
| Employment status (n, %) | .72 | |||||
| Student | 52 (43.33) | 11 (36.67) | 11 (36.67) | 15 (50.00) | 15 (50.00) | |
| Unemployed | 54 (45.00) | 14 (46.67) | 14 (46.67) | 13 (43.33) | 13 (43.33) | |
| Employed | 14 (11.67) | 5 (16.67) | 5 (16.67) | 2 (6.67) | 2 (6.67) | |
| Relationship status (n, %) | .71 | |||||
| No current partner | 10 (8.33) | 1 (3.33) | 4 (13.33) | 2 (6.67) | 3 (10.00) | |
| Married | 24 (20.00) | 6 (20.00) | 8 (26.67) | 6 (20.00) | 4 (13.33) | |
| Dating | 54 (45.00) | 13 (43.33) | 14 (46.67) | 13 (43.33) | 14 (46.67) | |
| Casual dating/ multiple partners | 32 (26.67) | 10 (33.33) | 4 (13.33) | 9 (30.00) | 9 (30.00) | |
| Children (n, %) | .09 | |||||
| No | 81 (67.50) | 19 (63.33) | 16 (53.33) | 21 (70.00) | 25 (83.33) | |
| Yes | 39 (32.50) | 11 (36.67) | 14 (46.67) | 9 (30.00) | 5 (16.67) | |
| Sexual history | ||||||
| Ever had vaginal sex (n, %) | .004 | |||||
| No | 21 (17.50) | 5 (16.67) | 0 (0.00) | 10 (33.33) | 6 (20.00) | |
| Yes | 99 (82.50) | 25 (83.33) | 30 (100.00) | 20 (66.67) | 24 (80.00) | |
| Ever had anal sex (n, %) | .90 | |||||
| No | 116 (96.67) | 30 (100.00) | 29 (96.67) | 29 (96.67) | 28 (93.33) | |
| Yes | 4 (3.33) | 0 (0.00) | 1 (3.33) | 1 (3.33) | 2 (6.67) | |
| Transactional sex (ever had sex in exchange for food, gifts, school fees, money, drugs, and/or alcohol) (n, %) | .96 | |||||
| No | 112 (93.33) | 28 (93.33) | 27 (90.00) | 29 (96.67) | 28 (93.33) | |
| Yes | 8 (6.67) | 2 (6.67) | 3 (10.00) | 1 (3.33) | 2 (6.67) | |
| Number of sex partners in past three months (n, %) | .05 | |||||
| Never had sex or not in the past three months | 49 (40.83) | 14 (46.67) | 7 (23.33) | 14 (46.67) | 14 (46.67) | |
| 1 | 47 (39.17) | 8 (26.67) | 20 (66.67) | 7 (23.33) | 12 (40.00) | |
| 2–3 | 16 (13.33) | 5 (16.67) | 2 (6.67) | 6 (20.00) | 3 (10.00) | |
| 4 or more | 8 (6.67) | 3 (10.00) | 1 (3.33) | 3 (10.00) | 1 (3.33) | |
| Gender of sex partners a (n, %) | .004 | |||||
| Never had sex | 21 (17.65) | 5 (16.67) | 0 (0.00) | 10 (33.33) | 6 (20.69) | |
| Had sex with opposite gender | 97 (81.51) | 25 (83.33) | 29 (96.67) | 20 (66.67) | 23 (79.31) | |
| Had sex with the same gender | 1 (0.84) | 0 (0.00) | 1 (3.33) | 0 (0.00) | 0 (0.00) | |
Note. p-values were estimated from t-test for continuous variables and chi-squared or Fisher's exact test if the cell size <5 for categorical variables.
n = 119 because one participant refused to answer.
Primary Randomized Controlled Trial Quantitative Outcomes
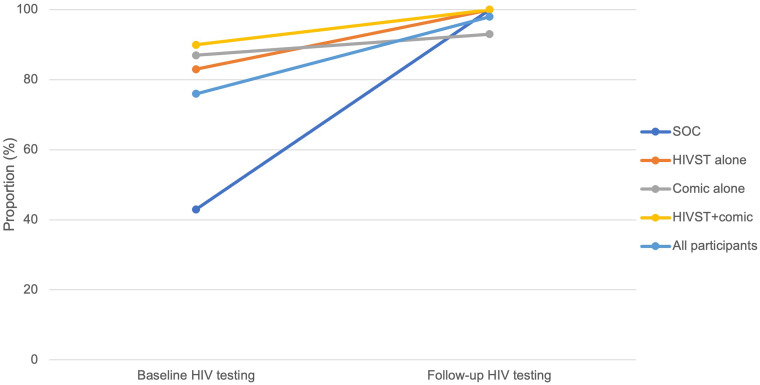
Table 2 describes the distribution of outcomes across time points. Three-quarters (76%) of participants had ever had an HIV test at Time 1, which was statistically different between the study arms, with the standard of care (Arm 4) having the lowest HIV testing rate (Arm 1 [HIV self-test kit + comic]: 90%; Arm 2 [HIV self-test kit alone]: 83%; Arm 3 [comic alone]: 87%; Arm 4 [standard of care]: 43%; p ≤ 0.001) (Table 2, Figure 3). Almost all (98% (n = 115/117)) refugee youth participants had an HIV test between Times 1 and 2, and all self-reported being HIV-negative; of these, 25% (n = 29/117) reported a new HIV test at Time 2 (ie, they had never received an HIV test in their lifetime at Time 1), and 74% (n = 86/117) of youth had a repeat HIV test at Time 2 (ie, they reported having a lifetime HIV test at Time 1) (Table 2, Figure 3). Among those tested between Time 1 and Time 2, 89% (n = 102/115) self-reported that they went to the health centre for confirmatory testing, and all self-reported that the clinic test confirmed the negative HIV self-testing result. Health centres reported n = 104 confirmatory tests, all HIV-negative. Among these, n = 2 participants did not report that they had a confirmatory test, but a linkage to care card was collected from the health centre with a negative HIV test result.
Table 2.
Distribution of HIV Prevention Outcomes Among Refugee Youth Participants (n = 120) in the Todurujo na Kadurok (Empowering Youth) Randomized Controlled Trial with Refugee Youth in a Humanitarian Setting in Uganda.
| All participants | Standard of care (SOC) | HIV self-testing arm (HIVST) | Comic arm | HIVST + comic arm | p | |
|---|---|---|---|---|---|---|
| Primary outcomes | ||||||
| Any HIV test (n, %) | ||||||
| Baseline | 91 (75.83) | 13 (43.33) | 25 (83.33) | 26 (86.67) | 27 (90.00) | <.001 |
| 3-month follow-up | 115 (98.00) | 30 (100.00) | 28 (100.00) | 27 (93.10) | 30 (100.00) | .12 |
| Knowledge of confirmatory testing (n, %) a | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | 102 (98.08) | 30 (100.00) | 20 (90.91) | 25 (100.00) | 27 (100.00) | .04 |
| HIV status knowledge (n, %) b | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | 102 (100.00) | 30 (100.00) | 20 (100.00) | 25 (100.00) | 27 (100.00) | n/a |
| Secondary outcomes | ||||||
| HIVST kit use (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | 58 (100.00) | – | 28 (100.00) | – | 30 (100.00) | n/a |
| Where HIVST kit was used (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | .03 | |||||
| Home | 50 (86.21) | – | 21 (75.00) | – | 29 (96.67) | |
| At site received test | 1 (1.72) | – | 1 (3.57) | – | 0 (0.00) | |
| Health centre | 7 (12.07) | – | 6 (21.43) | – | 1 (3.33) | |
| When HIVST kit was used (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | .001 | |||||
| Immediately | 8 (13.79) | – | 7 (25.00) | – | 1 (3.33) | |
| Within 2 days | 11 (18.97) | – | 9 (32.14) | – | 2 (6.67) | |
| Between 2 days and 1 week | 19 (32.76) | – | 9 (32.14) | – | 10 (33.33) | |
| Between 1 week and 2 weeks | 7 (12.07) | – | 1 (3.57) | – | 6 (20.00) | |
| Over 2 weeks | 13 (22.41) | – | 2 (7.14) | – | 11 (36.67) | |
| Asked for support from peer navigators, family member, friend and/or partner to use HIVST kit (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | 30 (51.72) | – | 9 (32.14) | – | 21 (70.00) | .008 |
| Comfort taking the HIVST (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | .48 | |||||
| Very/somewhat uncomfortable/neutral | 1 (1.72) | – | 1 (3.37) | – | 0 (0.00) | |
| Very/somewhat comfortable | 57 (98.28) | – | 27 (96.43) | – | 30 (100.00) | |
| Comfort asking primary sexual partner to use an HIVST (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up | .48 | |||||
| Very/somewhat uncomfortable/neutral | 1 (1.7) | – | 1 (3.57) | – | 0 (0.00) | |
| Very/somewhat comfortable | 57 (98.28) | – | 27 (96.43) | – | 30 (100.00) | |
| Comfort asking a casual sexual partner to use an HIVST (n, %) | ||||||
| Baseline | – | – | – | – | – | |
| 3-month follow-up (n = 4 answered n/a) | .46 | |||||
| Very/somewhat uncomfortable/neutral | 1 (1.85) | – | 1 (4.00) | – | 0 (0.00) | |
| Very/somewhat comfortable | 53 (98.15) | – | 24 (96.00) | – | 29 (100.00) | |
| HIV-related stigma: public attitudes about people with HIV (mean, SD) | ||||||
| Baseline | 7.85 (2.48) | 8.20 (2.41) | 7.03 (2.86) | 8.27 (2.38) | 7.90 (2.12) | .19 |
| 3-month follow-up | 8.23 (2.22) | 8.30 (2.42) | 7.82 (1.79) | 8.21 (2.57) | 8.57 (2.05) | .65 |
| HIV knowledge (mean, SD) | ||||||
| Baseline | 10.73 (2.22) | 10.80 (2.23) | 10.67 (2.09) | 10.07 (2.53) | 11.37 (1.90) | .16 |
| 3-month follow-up | 12.19 (2.19) | 12.40 (1.98) | 11.50 (2.19) | 12.07 (2.63) | 12.73 (1.82) | .17 |
| Safer sex efficacy (median, IQR) | ||||||
| Baseline | 20 (13.5, 26) | 19 (12, 24) | 20 (16, 23) | 20.5 (16, 24) | 24 (12, 27) | .77 |
| 3-month follow-up | 24.00 (18.5, 28) | 23 (17, 28) | 22 (17, 25) | 24 (19, 28) | 26.5 (20, 28) | .24 |
| Condom use during last sex (n, %) | ||||||
| Baseline | 31 (25.83) | 9 (30.00) | 5 (16.67) | 10 (33.33) | 7 (23.33) | .002 |
| 3-month follow-up | 31 (26.50) | 12 (40.00) | 4 (14.29) | 10 (34.48) | 5 (16.67) | .18 |
| Consistent condom use in last 3 months (n, %) | ||||||
| Baseline | 10 (8.33) | 3 (10.00) | 1 (3.33) | 4 (13.33) | 2 (6.67) | .24 |
| 3-month follow-up | 12 (10.26) | 5 (16.67) | 0 (0.00) | 5 (17.24) | 2 (6.67) | .26 |
| Adolescent sexual and reproductive health stigma (median, IQR) | ||||||
| Baseline | 12 (10, 13) | 12 (11, 13) | 13 (11, 13) | 13 (10, 14) | 12 (10, 14) | .56 |
| 3-month follow-up | 11 (10, 14) | 11 (10, 13) | 11 (9,14) | 12 (10, 14) | 11 (10, 13) | .76 |
| Sexual relationship power: relationship control subscale (mean, SD) | ||||||
| Baseline | 37.73 (6.81) | 38.47 (7.03) | 37.53 (8.41) | 37.00 (5.19) | 37.93 (6.48) | .87 |
| 3-month follow-up | 40.23 (6.69) | 41.00 (7.44) | 40.36 (6.18) | 39.00 (6.77) | 40.53 (6.44) | .70 |
| Sexual relationship power: decision-making dominance subscale (mean, SD) | ||||||
| Baseline | 16.61 (4.33) | 16.83 (4.67) | 16.93 (3.79) | 17.13 (4.61) | 15.53 (4.25) | .47 |
| 3-month follow-up | 16.68 (4.69) | 16.20 (5.37) | 16.46 (4.94) | 17.59 (4.14) | 16.50 (4.31) | .69 |
| Sexual relationship power c overall score (mean, SD) | ||||||
| Baseline | 2.4 (0.55) | 2.5 (0.62) | 2.5 (0.55) | 2.4 (0.51) | 2.3 (0.52) | .76 |
| 3-month follow-up | 2.5 (0.66) | 2.5 (0.79) | 2.5 (0.65) | 2.5 (0.62) | 2.5 (0.57) | .99 |
Notes: N at baseline = 120; N at 3-month follow-up = 117. IQR: interquartile range.
Knowledge of confirmatory testing was defined as a participant reporting that they attended a health center for confirmatory testing and the health center having a record (linkage to care card) for that same participant. The denominator was among those who reported having any HIV test by T2.
HIV status knowledge was defined as a participant reporting the same result of their HIV testing and confirmed by the linkage to care card from the health centre. The denominator was among those who had a confirmatory test at a health centre.
The sexual relationship power scale is a combination of sexual relationship power and decision-making dominance sub-scales.
Figure 3.
Change in HIV testing from baseline (ever tested for HIV before the study) to follow-up by study arm in the Todurujo na Kadurok HIV self-testing and edutainment comic randomized controlled trial with refugee youth in Bidi Bidi, Uganda.
Note: Trend in change in HIV testing over time was tested using Wilcoxon signed-rank test for all participants and by study arm: p-value for all participants < .001, p-value for SOC < .001, p-value for HIVST alone = .03, p-value for comic alone = .41, p-value for HIVST + comic = .08.
Adjusting for age, gender, time in Uganda, vaginal sex history, condom use at last sex, and baseline HIV testing, the odds of HIV testing at Time 2 (i.e., a change in HIV testing from baseline to Time 2) were highest in Arm 1 (HIV self-test kit + comic) compared to the standard of care (aOR: 8.46; 95% CI: 2.87, 24.97), followed by Arm 3 (comic alone) compared to the standard of care (aOR: 4.14; 95% CI: 1.58, 10.87) (Table 3, Figure 3). There was no significant difference in HIV testing from Time 1 to Time 2 between Arm 1 (HIV self-test kit alone) and the standard of care (aOR: 2.81; 95% CI: 0.96, 8.16; p = .058).
Table 3.
HIV Testing and HIV Prevention Outcomes Among Refugee Youth Participants (n = 117 a ) in the Todurujo na Kadurok (Empowering Youth) Randomized Controlled Trial, Bidi Bidi Refugee Settlement, Uganda.
| Odds ratio (OR) or beta coefficient (β) | 95% confidence interval (CI) | p | Adjusted odds ratio (aOR) b or adjusted beta coefficient (aβ) b | 95% CI | p | |||
|---|---|---|---|---|---|---|---|---|
| Primary outcome | ||||||||
| Any HIV test at Time 2 (OR) | ||||||||
| HIV self-test kit alone arm (HIVST) versus standard of care arm (SOC) | 4.16 | 1.57, 11.08 | .004 | 2.81 | 0.96, 8.16 | .058 | ||
| Comic versus SOC | 3.48 | 1.40, 8.65 | .007 | 4.14 | 1.58, 10.87 | .004 | ||
| HIVST + comic versus SOC | 7.51 | 2.23, 25.35 | .001 | 8.46 | 2.87, 24.97 | <.001 | ||
| Secondary outcomes | ||||||||
| HIV-related stigma: Public attitudes about people with HIV (β) | ||||||||
| HIVST versus SOC | −0.84 | −1.67,−0.001 | .05 | −0.95 | −1.88,−0.03 | .04 | ||
| Comic versus SOC | −0.01 | −0.90, 0.87 | .98 | −0.33 | −1.29, 0.63 | .50 | ||
| HIVST + comic versus SOC | −0.02 | −0.85, 0.81 | .97 | −0.22 | −1.17, 0.73 | .64 | ||
| HIV knowledge scale (β) | ||||||||
| HIVST versus SOC | −0.53 | −1.28, 0.22 | .17 | −0.61 | −1.46, 0.25 | .16 | ||
| Comic versus SOC | −0.55 | −1.46, 0.36 | .24 | −0.30 | −1.23, 0.63 | .53 | ||
| HIVST + comic versus SOC | 0.45 | −0.29, 1.19 | .23 | 0.59 | −0.31, 1.48 | .20 | ||
| Safer sex efficacy (β) | ||||||||
| HIVST versus SOC | −0.07 | −3.26, 3.12 | .97 | 0.54 | −2.81, 3.90 | .75 | ||
| Comic versus SOC | 0.68 | −2.62, 3.98 | .69 | −0.62 | −4.20, 2.96 | .73 | ||
| HIVST + comic versus SOC | 1.92 | −1.28, 5.11 | .24 | 1.63 | −1.55, 4.81 | .32 | ||
| Condom use during last sex c (OR) | ||||||||
| HIVST versus SOC | 0.25 | 0.09, 0.69 | .01 | 0.21 | 0.07, 0.65 | .01 | ||
| Comic versus SOC | 1.17 | 0.44, 3.15 | .75 | 0.99 | 0.33, 3.01 | .99 | ||
| HIVST + comic versus SOC | 0.45 | 0.17, 1.17 | .10 | 0.39 | 0.13, 1.20 | .10 | ||
| Consistent condom use in last 3 months c (OR) | ||||||||
| HIVST versus SOC | 0.08 | 0.01, 0.67 | .02 | 0.10 | 0.02, 0.58 | .01 | ||
| Comic versus SOC | 1.26 | 0.40, 3.99 | .70 | 1.07 | 0.29, 3.89 | .92 | ||
| HIVST + comic versus SOC | 0.43 | 0.10, 1.82 | .25 | 0.42 | 0.10, 1.74 | .23 | ||
| Adolescent SRH stigma (β) | ||||||||
| HIVST versus SOC | 0.12 | −0.81, 1.04 | .81 | −0.09 | −1.18, 1.00 | .88 | ||
| Comic versus SOC | 0.11 | −0.98, 1.20 | .84 | −0.20 | −1.57, 1.17 | .76 | ||
| HIVST + comic versus SOC | 0.07 | −0.81, 0.94 | .88 | −0.23 | −1.34, 0.89 | .69 | ||
| Sexual Relationship Power: Relationship control subscale (β) | ||||||||
| HIVST versus SOC | −0.91 | −4.13, 2.31 | .58 | −0.50 | −3.75, 2.75 | .76 | ||
| Comic versus SOC | −1.79 | −4.59, 1.01 | .21 | −2.50 | −5.35, 0.35 | .09 | ||
| HIVST + comic versus SOC | −0.50 | −3.48, 2.48 | .74 | −0.80 | −3.82, 2.23 | .61 | ||
| Sexual relationship power: decision-making dominance subscale (β) | ||||||||
| HIVST versus SOC | 0.24 | −1.87, 2.35 | .82 | 0.43 | −0.65, 1.51 | .44 | ||
| Comic versus SOC | 0.78 | −1.44, 3.00 | .49 | 0.48 | −0.61, 1.57 | .39 | ||
| HIVST + comic versus SOC | −0.50 | −2.68, 1.68 | .65 | −0.62 | −1.74, 0.49 | .27 | ||
| Sexual relationship power scale overall score (β) | ||||||||
| HIVST versus SOC | −0.016 | −0.31, 0.28 | .92 | 0.021 | −0.18, 0.23 | .84 | ||
| Comic versus SOC | −0.0039 | −0.30, 29 | .98 | −0.064 | −0.25, 0.13 | .51 | ||
| HIVST + comic versus SOC | −0.068 | −0.36, 0.22 | .65 | −0.095 | −0.30, 0.11 | .36 | ||
Regression models were conducted among participants who had outcomes measured at Time 1 and Time 2 (n = 117); those who were lost to follow-up at Time 2 (n = 3) were not included.
Adjusted for the baseline measure of the respective outcome, pre-specified covariates (age, gender, length of stay in Uganda) and baseline imbalances (history of vaginal sex, condom use during the last sexual intercourse, and ever HIV test at T1). To note, although education and sexual orientation were imbalanced at baseline, these covariates perfectly predicted failures in the outcomes so they were not adjusted for in the models.
Condom use models were conducted among those who had sex between Time 1 and 2 (n = 86).
The GEE model was not conducted for HIV status knowledge because 98% of participants correctly reported having a confirmatory test, and of those, there was perfect agreement in the HIV test result between the participants and health centres.
Secondary Randomized Controlled Trial Quantitative Outcomes
All participants who received HIV self-test kits used them; however, there were differences in how Arms 1 and 2 used the kits (Table 2). Arm 1 (HIV self-test kit + comic) tended to use HIV self-test kits at home (97%), > 1 week after receiving the kit (57%), and asked for support from a peer navigator, family, friend, and/or partner to use the kit (70%), whereas Arm 2 (HIV self-test kits alone) used them both at home (75%) and at the health centre (21%), within 2 days of receiving the kit (57%), and only one-third asked for support to use the kit. Both arms (Arm 1 and Arm 2) who received the HIV self-test kit reported feeling comfortable taking the HIV self-test kit (Arm 1: 100%, Arm 2: 96%) and asking their primary sexual partner (Arm 1: 100%, Arm 2: 96%) and casual sexual partners (Arm 1: 100%, Arm 2: 96%) to use the kit. At Time 1, there were significantly different condom use practices reported between study arms, whereby 17% of those in Arm 2 (HIV self-test kit alone) used a condom at last sex compared to 23% of Arm 1 (HIV self-test + comic), 33% in Arm 3 (comic alone), and 30% in Arm 4 (standard of care) (Table 2).
In analyses adjusted for pre-specified covariates (age, gender, length of stay in Uganda) and baseline imbalances (history of vaginal sex, condom use during last sex, ever HIV tested), we found that Arm 2 (HIV self-test alone) compared to the standard of care reported significantly lower HIV-related stigma (aβ: −0.95, 95% CI: −1.88, −0.03), lower odds of condom use during last sex (aOR: 0.21, 95% CI: 0.07, 0.65), and lower odds of past 3-month consistent condom use (aOR:0.10, 95% CI:0.02, 0.58) (Table 3).
Secondary and Sensitivity Analyses for Randomized Controlled Trial Quantitative Outcomes
In secondary analyses including all study participants across arms and adjusting for relevant covariates, there were statistically significant increases in HIV testing (aOR: 21.79; 95% CI: 4.57, 103.93), HIV knowledge (aβ: 1.45; 95% CI: 0.93, 1.97), safer sex efficacy (aβ: 3.64; 95% CI: 2.09, 5.19), and relationship control (aβ: 2.39; 95% CI: 1.16, 3.63) at Time 2 compared to Time 1 (Table 4). The sensitivity analysis to estimate any intervention effect compared to standard of care from Time 1 to Time 2 produced the same results as the primary analysis, whereby those who received an intervention had significantly higher odds of a repeat HIV test compared to those who did not receive an intervention, but there were no significant differences in secondary outcomes (Supplementary Table 1).
Table 4.
Effectiveness of Participating in the Todurujo na Kadurok (Empowering Youth) Study Regardless of Study Arm on HIV Prevention Outcomes among Refugee Youth Participants in Bidi Bidi, Uganda Comparing Baseline to 3-Month Follow-up (n = 117).
| Odds ratio (OR) or beta coefficient (β) | 95% confidence interval (CI) | p | Adjusted Odds ratio (aOR a ) or adjusted beta coefficient (aβ) a | 95% CI | p | |
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| HIV testing (OR) | ||||||
| 3-month follow-up versus baseline | 18.95 | 4.24, 84.59 | <.001 | 21.79 | 4.57, 103.93 | <.001 |
| Secondary outcomes | ||||||
| HIV-related stigma: Public attitudes about people with HIV (β) | ||||||
| 3-month follow-up versus baseline | 0.36 | −0.24, 0.96 | .24 | 0.36 | −0.24, 0.96 | .24 |
| HIV knowledge scale (β) | ||||||
| 3-month follow-up versus baseline | 1.45 | 0.93, 1.97 | <.001 | 1.45 | 0.93, 1.97 | <.001 |
| Safer sex efficacy (β) | ||||||
| 3-month follow-up versus baseline | 3.64 | 2.09, 5.19 | <.001 | 3.64 | 2.09, 5.19 | <.001 |
| Condom use during last sex b (OR) | ||||||
| 3-month follow-up versus baseline | 1.86 | 1.06, 3.25 | .03 | 1.69 | 0.91, 3.15 | .10 |
| Consistent condom use in last 3 months b (OR) | ||||||
| 3-month follow-up versus baseline | 1.46 | 0.62, 3.46 | .39 | 1.09 | 0.38, 3.10 | .87 |
| Adolescent SRH stigma (β) | ||||||
| 3-month follow-up versus baseline | −0.38 | −0.80, 0.05 | .08 | −0.38 | −0.80, 0.05 | .08 |
| Sexual Relationship Power: Relationship Control subscale (β) | ||||||
| 3-month follow-up versus baseline | 2.39 | 1.16, 3.63 | <.001 | 2.39 | 1.16, 3.63 | <.001 |
| Sexual Relationship Power: Decision-making dominance subscale (β) | ||||||
| 3-month follow-up versus baseline | 0.08 | −0.59, 0.75 | .82 | 0.08 | −0.59, 0.75 | .82 |
| Sexual Relationship Power scale overall score (β) | ||||||
| 3-month follow-up versus baseline | 0.049 | −0.045, 0.14 | .31 | 0.049 | −0.045, 0.14 | .31 |
Adjusted for pre-specified covariates (age, gender, length of stay in Uganda) and baseline imbalances (history of vaginal sex, condom use during the last sex, and ever HIV test at T1). To note, although education and gender of sex partners were imbalanced at baseline, these covariates perfectly predicted failures in the outcomes, so they were not adjusted for in the models.
Condom use models were conducted among those who had sex between Time 1 and 2 (n = 86).
Qualitative Findings on Study Implementation of HIVST and Edutainment Comic Interventions
Qualitative findings regarding youth experiences and reflections on the intervention (ie, those who received HIV self-testing and/or comics and were followed up to Time 2, n = 87) implementation are presented through two dimensions of the CFIR: implementation outcomes and innovation outcomes. 42
Theme 1: Implementation Outcomes
Findings regarding HIV self-testing implementation comprised three sub-themes relating to mistrust of HIV self-testing that reflect acceptability challenges: mistrust of oral testing for HIV, low HIV self-testing self-efficacy, and mistrust of kit results. Participant narratives also reflected acceptability of HIV self-testing as it offered privacy and convenience.
Mistrust of Oral Testing for HIV: Participants who reported a negative HIV self-testing kit result still engaged with confirmatory testing at the health centers because the test used saliva to detect HIV, instead of blood, which could result in mistrust of the self-test kit. As one youth noted, “I wanted to confirm my results because I wasn’t believing or trusting the test kit since it's my first time and I used my saliva instead of blood” (young man, age 19, HIVST + comic, ID#52), and another reported, “I want to confirm my results because it was the first time testing and I used saliva yet I know [with] HIV testing they take blood” (young woman, age 18, HIVST + comic, ID#44)
Low HIV Self-Testing Self-Efficacy: Participants also reported mistrust in their capacity to correctly administer the HIV self-test kit. A young man's reflection revealed how a lack of self-efficacy could result in concerns regarding the reliability of the HIV self-test result:
Since am not a professional or health worker and being my first time to use this self-test, I thought maybe I could have forgotten or omitted some steps within the procedures which I was told to follow. So, I decided to go to the hospital to see whether I was on the right track and confirm my result. (Young man, age 20, HIVST + comic, ID# 46)
Perceived low self-efficacy using the HIV self-test kits was exacerbated by relational contexts whereby participants (largely young women) did not know their partners’ HIV serostatus. For instance, a young woman described: “I thought maybe I made an error during the process of testing because [I] have been having unprotected sex and I don't know my partner's status.” (young woman, age 18, HIVST alone, ID#18) This was reinforced by another participant who noted both mistrust in her partner as well as testing herself: “I don't trust my husband so I went to confirm if I am really negative, and I am the one testing myself so I wanted doctor to test me also” (young woman, age 17, HIVST alone, ID#11)
Mistrust of HIV Self-Testing Results: Youth narratives revealed other influences on their acceptability of HIV self-testing results that, in turn, prompted them to seek confirmatory testing even with an HIV-negative self-test result. One such factor was information they had previously received regarding the inaccuracy of HIV self-testing: “There was another time these people had told us [HIV] self-test is not 100% accurate, so I had to go and confirm my results” (young man, age 22, HIVST alone, ID#14). Another factor that contributed to mistrusting HIV self-test results was concerns about one's personal risk for HIV acquisition due to having multiple sex partners. This was most noted by young men. For instance, a participant described that his sexual practices increased his perception of his HIV risk:
I was doubting my results, so I had to go to the hospital, [I] am having two girlfriends who I am not sure whether they are not having sex with other people… So, when the results showed negative, I couldn't believe. (Young man, age 18, HIVST + comic, ID #49)
Another participant who reported multiple sex partners went for a confirmatory test as he was worried that he could have acquired HIV after taking the HIV self-test: “I had stayed and had sex with many girls so thought the first results had changed already” (young man, age 20, SA#3, ID#101).
HIV Self-Testing Offers Privacy and Convenience: Participants who received the HIV self-testing kit also provided positive feedback, reporting that they felt the kits were a private, efficient, and reliable method to test which should be encouraged in their community:
HIV self-test kits are private, less time consuming and easy to use. Also [I] learnt that they are reliable because I had same results even after confirmatory test. [I] inquire, is it possible to give HIV self-test kits to friends and family? (young man, age 23, HIVST alone, ID#15)
This sentiment reflecting acceptability was corroborated by another young man who expressed that the kits offered accessibility and privacy:
Encourage the use of self-testing and the good use of it, it's the best method for HIV testing because it's safe to test at home in your time without people seeing you and taking your own time. (young man, age 22, HIVST alone, ID# #5)
Theme 2: Innovation Impact on HIV Self-Testing and Comic Recipients
Both innovations—the HIV self-test kit and edutainment comic—were described as meeting HIV testing and prevention needs among refugee youth participants. Four indicators of innovation success were identified: (1) HIV self-testing and comics increased confidence to engage in HIV testing and learn one's HIV serostatus; (2) comics increased knowledge of HIV testing and prevention; (3) comics increased acceptance and support toward people living with HIV; and (4) participants were motivated to share innovations with others.
HIV Self-Testing and Comics Increased Confidence to Engage in HIV Testing and Learn One's HIV Serostatus: Youth discussed that engaging with testing via HIV self-testing and/or learning about testing via comics resulted in learning their HIV serostatus. For instance, a youth described “HIV self-testing is one of the most convenient methods of HIV testing [I] have ever come across, anywhere and at any time you are able to know your health status” (young man, age 20, HIVST + comic, ID#46]. Others described that engaging with HIV self-testing increased confidence in engaging with additional health services: “It [HIV self-testing] helped me know my status and build confidence in going to the facility to confirm and learn ways to control myself and use of condom so as to be free from HIV” (young woman, age 21, HIVST alone, ID# 3).
Others specifically expressed that the comic encouraged them to use the HIV self-test kit and engage in confirmatory testing with friends:
We read the comic book with my friends, and we were motivated to go and test again. In addition, during the training on how to use the kit, they told us to go back to the health center for confirmatory testing. (young man, age 17, HIVST + comic, ID#17)
Others discussed that health workers and study staff encouraged them to learn their HIV serostatus through confirmatory testing following HIV self-testing: “To be sure of my status and if I am really [HIV] negative, and they told us we should go to health centers to confirm the results we get from self-test” (man, age 23, HIVST + comic, ID# 31).
Comics Increased Knowledge of HIV Testing and Prevention: Participants who received the edutainment comics reported that it increased HIV testing and prevention literacy, including building the capacity to educate others about HIV testing. For instance, a participant reported that the comic taught them how to encourage partners to test together: “It was educative and I learnt about HIV testing and how to engage my girlfriend to go test together” (young man, age 23, HIVST + comic, ID# 31). Comics also provided the opportunity to reflect on relationship dynamics, helped participants assess if HIV testing would be safe or not in a relationship, and shifted perceptions regarding engaging in HIV serodiscordant partnerships. To illustrate, a young man discussed how reading the comics provided insight into healthy and supportive relationships with people living with HIV: “[The comic] helped me learn how to create a relationship with someone that is HIV positive and through the pictures in the comic book [I] learned how to counsel HIV [positive] persons” (young man, age 23, HIVST + comic, ID#32).
Comics Increased Acceptance and Support Toward People Living with HIV: Participants reported that the comic taught them about HIV transmission and prevention which in turn helped to reduce stigma: “[The comic] is so educative; I was able to learn about the various ways of HIV prevention like the use of condoms and how to be good to HIV positive people to fight stigma” (woman, age 18, HIVST + comic, ID# 47). Participants also reported how the comics helped them acquire skills to support others to test for HIV, or when testing positive, to engage with HIV care:
From this comic book here, I learnt how to advise someone to go for HIV testing, to encourage someone who has HIV to go for HIV drugs, and to receive advice from other people. (young woman, age 18, HIVST + comic, ID# 42)
Participants were Motivated to Share Innovations with Others: Youth discussed disseminating the knowledge they acquired through the intervention with others in their community. For instance, a youth discussed sharing the comic with friends:
That comic book is so good, it tells us how to share with our friends, it tells us where we can go for testing, it is really interesting. Thank you so much for the book, I have shared it with my friend to read and they have loved it. (woman, age 19, comic alone, ID#81)
Others shared the knowledge they gained from HIV self-testing with friends: “I got inspired and courage to go have myself tested, and I was able to share with my friends and partners about the importance of having yourself tested and knowing your status” (man, age 20, HIVST + comic, ID#50).
After receiving the HIV self-testing kit and/or comic, participants often requested additional resources for their community. One young woman who received both innovations (comic, HIV self-test kit) suggested that there be “more training to other youths so that they can get to know how to use the self-testing kit” and “more comic books so that they can share with their friends” (woman, age 19, HIVST + comic, ID#38). Another respondent described how the comic could help reduce stigma toward HIV testing in their community, requesting the intervention’s expansion:
I am requesting, if possible, there should be an extension of this program not only to the youth but even the elderly, especially those who can't even move, and also educate and sensitize the community about HIV self-testing to break all the myths people have towards it. (man, age 20, HIVST + comic, ID# 46)
Discussion
Findings indicate the benefits of HIV self-testing and edutainment comics in meeting refugee youth's HIV testing needs in a rural Ugandan refugee settlement. HIV testing uptake was higher in intervention arms who received either the HIV self-test kit alongside the comic, or the comic alone, compared with the standard of care. The benefits of HIV self-testing have not yet been extended to refugee camp humanitarian contexts, 6 and our findings signal the promise of this approach alongside edutainment comics in increasing HIV testing uptake in one of the world's largest refugee settlements. Open-ended participant responses also provided insight into antecedent factors shaping implementation outcomes, including barriers and facilitators to HIV self-testing acceptability, as well as innovation outcomes of increased HIV testing, confidence, acceptance of people with HIV, and interest in sharing the innovation.
Our findings build on past research on HIV self-testing as a feasible, acceptable, and effective approach for increasing HIV testing among non-refugees in Uganda47–50 and other African settings, 51 and among urban refugees in Kampala,9,52 to show its utility in a rural refugee settlement context and the benefits of accompanying HIV self-testing with comics. Notably, receiving an HIV self-test kit on its own was not associated with increased HIV testing in our sample, underscoring the potential importance of peer support that was provided alongside the comic as well as the comic content itself. Our sample of participants had low education, which may amplify the salience of peer support in facilitating clinic-based and HIV self-testing. Indeed, we found that the HIV self-testing and comic arm, compared to the HIV self-testing alone arm, was more likely to ask for social support when using the HIV self-test kit and to use it at home, suggesting that the peer-supported comic may facilitate confidence in using and discussing the HIV self-test kit with others. This important role of peer support in HIV self-testing has been documented with non-refugees in Uganda,53–55 and testing with youth-friendly supportive providers in Zimbabwe was preferred over HIV self-testing alone among youth due to a desire for support. 56 Our findings expand upon these studies to reveal the importance of peer support in HIV testing delivery in humanitarian settings such as Bidi Bidi.
Our findings provide new insight into the role of edutainment comics in increasing HIV testing uptake, building on prior comic book research on their use in sexual and reproductive health areas such as HIV stigma, 21 contraception, 22 HPV vaccination, 23 and post-rape care.24,25 Our application of the HIV prevention cascade dimensions (motivation, access, effective use) 28 to participatory comic 29 development may have helped refugee youth who were provided both the HIV self-test kit and the comic to overcome testing barriers (eg, misinformation) 57 —participants only receiving the HIV self-testing kit did not engage in increased testing between Times 1 and 2. While the HIV self-test kit (alone) arm reported reduced HIV stigma and reduced condom use, with no changes in HIV testing, these findings were not consistent in sensitivity analyses, where we found that any intervention arm was associated with increased HIV testing and no secondary outcome changes. Thus, our sensitivity analyses may help adjust for the baseline imbalances we documented between study arms to better understand intervention effects. 58
Although study arms that received the edutainment comic did not show statistically significant changes in HIV knowledge, HIV-related stigma, or safer sex, the positive qualitative feedback from youth affirmed that wider distribution of the intervention components (HIV self-testing, comics) in the community could reduce stigma. This reflects the potential for innovation impacts to extend beyond the youth participants themselves to the wider community. Youth narratives also indicated that the comic provided knowledge of HIV transmission and prevention, with multiple youth stating that they learned about condom use from the comic. This finding reflects the benefit of HIV testing as a gateway to other HIV prevention services. 59 Feasibility concerns involved both (1) the interaction between low self-efficacy and mistrust of the HIV self-test result due to relational contexts, whereby young women did not know their partner's serostatus; and (2) concerns about trusting HIV self-testing results due to high HIV risk perception when young men reported having multiple sex partners. Participants who received only the HIVST kit without the comic more commonly described this mistrust in the HIV self-test results due to high HIV risk perception from their sexual practices, and this was also reflected in the quantitative finding that the HIVST alone arm was associated with reduced condom use compared to the standard of care.
There are several study limitations. First, the non-random sample does not reflect all youth in Bidi Bidi. Second, baseline differences, adjusted for in analyses, reflect potentially different socio-cultural contexts across refugee villages. While we randomized by village to reduce contamination risks between intervention arms, individual randomization could have reduced heterogeneity between arms. Our analyses adjust for repeated observations within individuals but were not able to adjust for clustering between youth in each village due to the small number of villages included. Third, the effect of peer support and the comic are interlinked, and further disentangling these effects (e.g. comic alone vs. peer-supported comic) could help elucidate the most important facet of the comic (e.g., content or peer support). Yet, in the context of the very low education level of this sample (10% secondary school completion), the team ascertained that peer support was required to ensure comic comprehension. Fourth, no participant was found to have an HIV infection, which may be the result of a relatively low prevalence of HIV among youth in Uganda, 60 and most participants had lived in Uganda since childhood (73% lived in Uganda for 6 or more years). This could also mean that our study was more likely to include youth already connected with URDMC refugee youth services, and we may not have included more marginalized and socially excluded youth with higher HIV vulnerabilities. However, refugee youth participants in Bidi Bidi still believed HIV self-testing was valuable for their community to build self-confidence in their health management and reduce barriers to testing. While we did not find any significant reductions in HIV-related stigma in the quantitative results, participant narratives in the qualitative findings revealed greater acceptance of people with HIV. It is not clear whether this discrepancy is due to the HIV stigma scale used not being relevant or tailored for youth in the refugee settlement context, or whether there were in fact meaningful and lasting differences in stigma attributable to the intervention across multiple stigma dimensions (eg, anticipated, perceived, internalized, enacted). 61 Stigma reduction strategies for youth in Bidi Bidi warrant further attention. Finally, any type of study involvement was associated with improved HIV outcomes among participants, suggesting direct and indirect benefits of clinical trial participation, 62 likely due to all participants being provided information, contact with URDMC, and thus increased knowledge regarding HIV resources in Bidi Bidi and supportive conversations with trained researchers during the surveys.
Qualitative feedback provided insight into how to optimize HIV self-testing implementation in Bidi Bidi. For instance, antecedent factors 42 that reduced acceptability of HIV self-testing in this setting included mistrust of the HIV self-test kit (oral vs blood testing) and low self-efficacy in using the test kit—both factors that could be addressed in future testing interventions. Other factors that shaped the implementation climate were the high perceived risk of HIV acquisition due to mistrust of one's partner among young women, and personal sexual risk practices among young men, which exacerbated mistrust of the HIV self-test kit and one's efficacy in using it. Psychosocial strategies that build peer support, HIV self-testing skills, and risk reduction, such as the TRUST HIV self-testing intervention, 63 may offer promise for addressing these implementation barriers. Innovation success 42 was described qualitatively by participants discussing the role of HIV self-testing and comics in increasing HIV testing uptake, HIV testing and prevention knowledge, and wanting to share the innovations with peers and community members. This points to future opportunities to implement participatory edutainment comic approaches to promote subsequent steps in the HIV prevention and care cascades.
In sum, our HIV self-testing and edutainment comic intervention designed to overcome HIV testing barriers with refugee youth significantly increased HIV testing uptake. With participatory and youth-friendly educational comics accompanying HIV self-testing, HIV self-testing was both feasible and acceptable among this population, and thus could have an impact on the entire community if integrated into healthcare in refugee settlements. This intervention, specifically combining HIV self-testing with edutainment comics, can be considered for youth at elevated exposure to HIV in other humanitarian settings to increase HIV testing uptake and in turn help achieve the 95-95-95 goals of ending the HIV epidemic 64 through increasing HIV serostatus knowledge.
Supplemental Material
Supplemental material, sj-docx-1-jia-10.1177_23259582241307057 for Findings From the Todurujo na Kadurok (Empowering Youth) HIV Self-Testing and Edutainment Comic Randomized Controlled Trial With Refugee Youth in a Humanitarian Setting in Uganda by Carmen H. Logie, Miranda G. Loutet, Moses Okumu, Frannie MacKenzie, Madelaine Coelho, Simon Odong Lukone, Nelson Kisubi, Aiman Malhi, Peter Kyambadde and Lawrence Mbuagbaw in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Acknowledgments
We would like to acknowledge the support and contributions of the Uganda Refugee and Disaster Management Council (URDMC), the Uganda Ministry of Health, the Uganda National AIDS Control Program, Mildmay Uganda, the Uganda Office of the Prime Minister Department of Refugees, the peer navigators, the research assistants who collected the data, and the refugee youth who participated in the study. We would like to acknowledge the support of Ellie Moffatt and Duncan Short at ViiV Healthcare.
Footnotes
Authorship Confirmation: Study design: CHL, MO, MA, PK; Data collection: MGL, MC, FM, SOL, NK, CHL; Data management and analysis: MGL, FM, SOL, NK, LM, CHL, AM; Manuscript writing: MGL, CHL, AM, MO; Manuscript editing and critical review: CHL, MO, MGL, MC, FM, SOL, NK, AM, PK, LM.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval: Research ethics board approval was provided by the Mildmay Uganda Research Ethics Committee (REC REF 0802-2021), the Uganda National Council for Science and Technology (SS884ES), and the University of Toronto Research Ethics Board (37496). The trial was registered at ClinicalTrials.gov (#NCT05213689). All participants provided written informed consent prior to study enrollment.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by ViiV Healthcare (Positive Action for Adolescents Grant), with additional support from: Canada Research Chairs (Tier 2, Logie), Social Sciences and Humanities Research Council of Canada (Insight Grant), Canadian Institutes of Health Research Institute of Gender and Health (Project Grant: Grant#628520-1652450711), and Canada Foundation for Innovation (JELF).
ORCID iD: Carmen H. Logie https://orcid.org/0000-0002-8035-433X
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Vasylyeva TI, Horyniak D, Bojorquez I, Pham MD. Left behind on the path to 90-90-90: Understanding and responding to HIV among displaced people. J Int AIDS Soc. 2022;25(11):e26031. doi: 10.1002/jia2.26031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. The Path That Ends AIDS: 2023 UNAIDS Global Aids Update. UNAIDS; 2023: 196.
- 3.Witzel TC, Eshun-Wilson I, Jamil MS, et al. Comparing the effects of HIV self-testing to standard HIV testing for key populations: A systematic review and meta-analysis. BMC Med. 2020;18(1):381-381. doi: 10.1186/s12916-020-01835-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin Y, Han L, Babbitt A, et al. Experiences using and organizing HIV self-testing. AIDS. 2018;32(3):371-381. doi: 10.1097/QAD.0000000000001705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson CC, Kennedy C, Fonner V, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: A systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1):21594-21594. doi: 10.7448/IAS.20.1.21594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Logie CH, Khoshnood K, Okumu M, et al. Self care interventions could advance sexual and reproductive health in humanitarian settings. Br Med J. 2019;365:l1083-l1083. doi: 10.1136/bmj.l1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Refugees UNHC for. Mid-Year Trends 2022. UNHCR. Accessed October 5, 2023. https://www.unhcr.org/statistics/unhcrstats/635a578f4/mid-year-trends-2022.html
- 8.Uganda - Refugee Statistics May 2023. UNHCR Operational Data Portal (ODP). Accessed November 25, 2023. https://data.unhcr.org/en/documents/details/101196
- 9.Logie CH, Okumu M, Berry I, et al. Findings from the Tushirikiane mobile health (mHealth) HIV self-testing pragmatic trial with refugee adolescents and youth living in informal settlements in Kampala, Uganda. J Int AIDS Soc. 2023;26(10):e26185. doi: 10.1002/jia2.26185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Indravudh PP, Sibanda EL, d’Elbée M, et al. ‘I will choose when to test, where I want to test’: Investigating young people’s preferences for HIV self-testing in Malawi and Zimbabwe. AIDS. 2017;31:S203. doi: 10.1097/QAD.0000000000001516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatzold K, Gudukeya S, Mutseta MN, et al. HIV self-testing: Breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. J Int AIDS Soc. 2019;22(Suppl Suppl 1):e25244. doi: 10.1002/jia2.25244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dawson A, Tappis H, Tran NT. Self-care interventions for sexual and reproductive health in humanitarian and fragile settings: A scoping review. BMC Health Serv Res. 2022;22(1):757-757. doi: 10.1186/s12913-022-07916-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakalega R, Mukiza N, Menge R, et al. Feasibility and acceptability of peer-delivered HIV self-testing and PrEP for young women in Kampala, Uganda. BMC Public Health. 2023;23(1):1163-1163. doi: 10.1186/s12889-023-16081-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lapsley R, Beima-Sofie K, Moraa H, et al. “They have given you the morale and confidence”: Adolescents and young adults want more community-based oral HIV self-testing options in Kenya. AIDS Care. 2023;35(3):392-398. doi: 10.1080/09540121.2022.2067315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Laughlin KN, Rouhani SA, Faustin ZM, Ware NC. Testing experiences of HIV positive refugees in Nakivale Refugee Settlement in Uganda: Informing interventions to encourage priority shifting. Confl Health. 2013;7(1):1-9. doi: 10.1186/1752-1505-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Logie CH, Okumu M, Latif M, et al. Relational Factors and HIV Testing Practices: Qualitative Insights from Urban Refugee Youth in Kampala, Uganda. AIDS Behav. 2022;26(7):2191-2202. doi: 10.1007/s10461-021-03567-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Laughlin KN, Kasozi J, Rabideau DJ, et al. The cascade of HIV care among refugees and nationals in nakivale refugee settlement in Uganda. HIV Med. 2017;18(7):513-518. doi: 10.1111/hiv.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Laughlin KN, Rouhani SA, Kasozi J, et al. A qualitative approach to understand antiretroviral therapy (ART) adherence for refugees living in Nakivale refugee settlement in Uganda. Confl Health. 2018;12(1):1-9. doi: 10.1186/s13031-018-0145-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Logie CH, Okumu M, Kibuuka Musoke D, et al. Intersecting stigma and HIV testing practices among urban refugee adolescents and youth in Kampala. Uganda: qualitative findings . J Intern AIDS Soc. 2021;24(3):e25674. doi: 10.1002/jia2.25674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green MJ, Myers KR. Graphic medicine: Use of comics in medical education and patient care. Br Med J. 2010;340(mar03 2):c863-c863. doi: 10.1136/bmj.c863 [DOI] [PubMed] [Google Scholar]
- 21.Obare F, Birungi H, Deacon B, Burnet R. Effectiveness of using comic books to communicate HIV and AIDS messages to in-school youth: Insights from a pilot intervention study in Nairobi, Kenya . African Population Studies. 2013;27(2):203. doi: 10.11564/27-2-441 [DOI] [Google Scholar]
- 22.Speizer IS, Calhoun LM, Guilkey DK. Reaching urban female adolescents at key points of sexual and reproductive health transitions: Evidence from a longitudinal study from Kenya. Afr J Reprod Health. 2018;22(1):47-59. doi: 10.29063/ajrh2018/v22i1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katz ML, Oldach BR, Goodwin J, Reiter PL, Ruffin MT, Paskett ED. Development and initial feedback about a human papillomavirus (HPV) vaccine comic book for adolescents. J Cancer Educ. 2014;29(2):318-324. doi: 10.1007/s13187-013-0604-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Logie CH, Okumu M, Lukone SO, et al. Ngutulu Kagwero (agents of change): Study design of a participatory comic pilot study on sexual violence prevention and post-rape clinical care with refugee youth in a humanitarian setting in Uganda. Glob Health Action. 2021;14(1):1940763-1940763. doi: 10.1080/16549716.2021.1940763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Logie CH, Okumu M, Loutet M, et al. Mixed-methods findings from the Ngutulu Kagwero (agents of change) participatory comic pilot study on post-rape clinical care and sexual violence prevention with refugee youth in a humanitarian setting in Uganda. Global Public Health. Published Online June. 2022;18(1):1-19. doi: 10.1080/17441692.2022.2092178 [DOI] [PubMed] [Google Scholar]
- 26.Logie CH, Okumu M, McAlpine A, et al. Qualitative comic book mapping: Developing comic books informed by lived experiences of refugee youth to advance sexual and gender-based violence prevention and stigma reduction in a humanitarian setting in Uganda. Int J Qual Methods. 2023;22. doi: 10.1177/16094069231183606 [DOI] [Google Scholar]
- 27.UNHCR. Uganda - Population Dashboard: Overview of Refugees and Asylum-Seekers in Uganda as of 31 July 2023. 2023. https://reliefweb.int/report/uganda/uganda-population-dashboard-overview-refugees-and-asylum-seekers-uganda-31-july-2023
- 28.Logie CH, Okumu M, Loutet MG, et al. Todurujo na Kadurok (empowering youth): Study protocol of an HIV self-testing and edutainment comic cluster randomised trial among refugee youth in a humanitarian setting in Uganda. BMJ Open. 2022;12(11):e065452. doi: 10.1136/bmjopen-2022-065452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Logie CH, Okumu M, McAlpine A, et al. Qualitative comic book mapping: Developing comic books informed by lived experiences of refugee youth to advance sexual and gender-based violence prevention and stigma reduction in a humanitarian setting in Uganda. Int J Qual Methods. 2023;22:16094069231183606. doi: 10.1177/16094069231183606 [DOI] [Google Scholar]
- 30.Moorhouse L, Schaefer R, Thomas R, et al. Application of the HIV prevention cascade to identify, develop and evaluate interventions to improve use of prevention methods: Examples from a study in east Zimbabwe. J Int AIDS Soc. 2019;22(S4):86-92. doi: 10.1002/jia2.25309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.About. SurveyCTO. Published online 2020. https://www.surveycto.com/
- 32.Reinius M, Wettergren L, Wiklander M, Svedhem V, Ekström AM, Eriksson LE. Development of a 12-item short version of the HIV stigma scale. Health Qual Life Outcomes. 2017;15(1):115. doi: 10.1186/s12955-017-0691-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shaweno D, Tekletsadik E. Validation of the condom use self-efficacy scale in Ethiopia. BMC Int Health Hum Rights. 2013;13(1):22. doi: 10.1186/1472-698X-13-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. J Am Coll Health. 1991;39(5):219-225. doi: 10.1080/07448481.1991.9936238 [DOI] [PubMed] [Google Scholar]
- 36.Logie CH, Okumu M, Mwima SP, et al. Exploring associations between adolescent sexual and reproductive health stigma and HIV testing awareness and uptake among urban refugee and displaced youth in Kampala, Uganda. Sexual Reproduct Health Matter. 2019;27(3):86-106. doi: 10.1080/26410397.2019.1695380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hall KS, Manu A, Morhe E, et al. Development and validation of a scale to measure adolescent sexual and reproductive health stigma: Results from young women in Ghana. J Sex Res. 2018;55(1):60-72. doi: 10.1080/00224499.2017.1292493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7):637-660. doi: 10.1023/A:1007051506972 [DOI] [Google Scholar]
- 39.Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. doi: 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- 40.Hinton PR, McMurray I, Brownlow C. SPSS Explained. 2nd ed. Routledge; 2014. [Google Scholar]
- 41.Nunnally J, Bernstein J. Psychometric Theory. 3rd ed. McGraw-Hill; 1994. Published online. [Google Scholar]
- 42.Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery J. Conceptualizing outcomes for use with the consolidated framework for implementation research (CFIR): The CFIR outcomes addendum. Implement Sci. 2022;17(1):1-10. doi: 10.1186/s13012-021-01181-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sween-Cadieux E M, Dagenais C, Somé DT, Ridde V. A health knowledge brokering intervention in a district of Burkina Faso: A qualitative retrospective implementation analysis. PLoS ONE. 2019;14(7):e0220105. doi: 10.1371/journal.pone.0220105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dedoose. Web application for managing, analyzing, and presenting qualitative and mixed method research data. Published online 2016.
- 45.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 46.Attride-Stirling J. Thematic networks: An analytic tool for qualitative research. Qual Res. 2001;1(3):385-405. doi: 10.1177/146879410100100307 [DOI] [Google Scholar]
- 47.Ortblad KF, Kibuuka Musoke D, Ngabirano T, et al. The effect of HIV self-testing delivery models on female sex Workers’ sexual behaviors: A randomized controlled trial in urban Uganda. AIDS Behav. 2019;23(5):1225-1239. doi: 10.1007/s10461-019-02393-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ortblad K, Kibuuka Musoke D, Ngabirano T, et al. Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial. PLoS Med. 2017;14(11):1-24. doi: 10.1371/journal.pmed.1002458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Asiimwe S, Oloya J, Song X, Whalen CC. Accuracy of un-supervised versus provider-supervised self-administered HIV testing in Uganda: A randomized implementation trial. AIDS Behav. 2014;18(12):2477-2484. doi: 10.1007/s10461-014-0765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Okoboi S, Castelnuovo B, Geertruyden J, Pierre V, King R, Mujugira A. Cost-effectiveness of peer-delivered HIV self-tests for MSM in Uganda . Front Public Health 2021;9:1–-8. doi: 10.3389/fpubh.2021.651325 [DOI] [PMC free article] [PubMed]
- 51.Hatzold K, Gudukeya S, Mutseta MN, et al. HIV self-testing: Breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. J Int AIDS Soc. 2019;22(S1):43-52. doi: 10.1002/jia2.25244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Logie C, Okumu M, Hakiza R, et al. Mobile health–supported HIV self-testing strategy among urban refugee and displaced youth in Kampala, Uganda: Protocol for a cluster randomized trial (Tushirikiane, supporting each other). JMIR Res Protoc. 2021;10(2):e26192. doi: 10.2196/26192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Okoboi S, Lazarus O, Castelnuovo B, et al. Peer distribution of HIV self-test kits to men who have sex with men to identify undiagnosed HIV infection in Uganda: A pilot study. Plos One. 2020;15(1):e0227741-e0227741. doi: 10.1371/journal.pone.0227741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McGowan M, Roche SD, Nakitende A, et al. Understanding how social support influences peer-delivered HIV prevention interventions among Ugandan female sex workers: A case study from HIV self-testing. BMC Public Health. 2022;22(1):1-10. doi: 10.1186/s12889-022-12836-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Okoboi S, Twimukye A, Lazarus O, et al. Acceptability, perceived reliability and challenges associated with distributing HIV self-test kits to young MSM in Uganda: A qualitative study. J Int AIDS Soc. 2019;22(3):e25269. doi: 10.1002/jia2.25269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mavodza CV, Mackworth-Young CRS, Bandason T, et al. When healthcare providers are supportive, ‘I’d rather not test alone’: Exploring uptake and acceptability of HIV self-testing for youth in Zimbabwe – A mixed method study. J Int AIDS Soc. 2021;24(9):e25815. doi: 10.1002/jia2.25815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Logie CH, Okumu M, Kibuuka Musoke D, et al. The role of context in shaping HIV testing and prevention engagement among urban refugee and displaced adolescents and youth in Kampala, Uganda: Findings from a qualitative study. Trop Med Int Health. 2021;26(5):1-10. doi: 10.1111/tmi.13560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thabane L, Mbuagbaw L, Zhang S, et al. A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med Res Methodol. 2013;13(1):92. doi: 10.1186/1471-2288-13-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tsoi BW, Parker M, Fine SM, et al. HIV Testing. Johns Hopkins University; 2022. Accessed May 30, 2024. http://www.ncbi.nlm.nih.gov/books/NBK581840/ [PubMed] [Google Scholar]
- 60.Vithalani J, Herreros-Villanueva M. HIV Epidemiology in Uganda: Survey based on age, gender, number of sexual partners and frequency of testing. Afr H Sci. 2018;18(3):523. doi: 10.4314/ahs.v18i3.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stangl AL, Earnshaw VA, Logie CH, et al. The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31-31. doi: 10.1186/s12916-019-1271-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bouzalmate-Hajjaj A, Massó Guijarro P, Khan KS, Bueno-Cavanillas A, Cano-Ibáñez N. Benefits of participation in clinical trials: An Umbrella review. IJERPH. 2022;19(22):15368. doi: 10.3390/ijerph192215368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Frye V, Nandi V, Paige MQ, et al. TRUST: Assessing the efficacy of an intervention to increase HIV self-testing among young black men who have sex with men (MSM) and transwomen. AIDS Behav. 2021;25(4):1219-1235. doi: 10.1007/s10461-020-03091-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.UNAIDS. Fast-Track: Ending the AIDS Epidemic by 2030. World Health Organization; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jia-10.1177_23259582241307057 for Findings From the Todurujo na Kadurok (Empowering Youth) HIV Self-Testing and Edutainment Comic Randomized Controlled Trial With Refugee Youth in a Humanitarian Setting in Uganda by Carmen H. Logie, Miranda G. Loutet, Moses Okumu, Frannie MacKenzie, Madelaine Coelho, Simon Odong Lukone, Nelson Kisubi, Aiman Malhi, Peter Kyambadde and Lawrence Mbuagbaw in Journal of the International Association of Providers of AIDS Care (JIAPAC)