Abstract
Background and aim
The system of family doctor contract services is a crucial component of China's primary healthcare system. Patients enrolled in family doctor contract services typically receive more comprehensive health services. However, it remains uncertain whether the family doctor contract services can fully meet the healthcare needs of patients. Despite extensive research on family doctor contract services, there has been relatively little investigation from the perspective of patients' sense of gain, and there are no specific tools available to measure patients' sense of gain in healthcare. Therefore, this study aims to develop a scale to measure patients' sense of gain in family doctor contract services.
Methods
This study enrolled 600 patients under family doctor contracts. It utilized a review of literature and Delphi expert consultation to form the concept of patients' sense of medical gain in the context of family doctor services, establish an item pool, screen items, and evaluate the scale's reliability and validity. Factor analysis assessed the scale's structural validity, while Cronbach's alpha coefficient evaluated its internal consistency. Test–retest reliability and split-half reliability were used to assess the scale's reliability.
Results
The Patients' Sense of Medical Gain in the context of Family Doctor services(PSMG-FD) scale for assessing sense of medical gain among family doctor contract patients comprises 19 items, categorized into five factors: Medical convenience, continuity, reliability, humanistic care, and experience. Confirmatory factor analysis results indicated satisfactory fit indices: χ2/df = 2.781, RMSEA = 0.077, RMR = 0.031, GFI = 0.875, NFI = 0.918, IFI = 0.946, TLI = 0.934, CFI = 0.945, and RFI = 0.901. The AVE values for different dimensions were 0.544, 0.739, 0.741, 0.755, and 0.654, all surpassing the threshold of 0.5. The CR values for each dimension were 0.820, 0.919, 0.919, 0.925, and 0.850, all exceeding 0.7, indicating satisfactory convergent validity. The interdimensional correlation coefficients were lower than the square roots of the corresponding AVEs, suggesting correlation among latent variables while maintaining sufficient discriminant validity. The PSMG-FD scale demonstrated good reliability and validity, with a Cronbach’s α coefficient of 0.947, test–retest reliability of 0.955, and split-half reliability of 0.895.
Conclusion
The scale exhibits good reliability and validity, making it a suitable instrument for evaluating sense of medical gain among family doctor contract patients in China.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12070-0.
Keywords: Family Doctor's contracting services, Sense of medical gain, Scale, Reliability, Validity
Introduction
Over last 30 years, family doctors have played a crucial role in delivering personalized healthcare within the framework of families and communities. Their impact extends to medical education and has transformed healthcare systems in numerous countries globally [1].To change the healthcare service model in primary health institutions and provide proactive, continuous and comprehensive health accountability management with residents [2],Chinese government agencies jointly released the ‘Guiding Opinions on Promoting Family Doctor Contracted Services’ [3] in 2016, which proposed a model of Family Doctor Contracted Services(FDCS) and established the family doctor as the first person responsible for the contracted service. In China, basic medical care, public health, and health management services are provided by family doctors, which include general practitioners registered with primary health institutions, qualified doctors at township clinics, and village doctors. These services are delivered in the form of teamwork and are based on the principles of full notification, voluntary contract signing, and standardized service [4, 5].Family doctors act as the gatekeeper of residents’ health by assuming six primary roles within the primary care system. These roles encompass triage and treatment, resource allocation, surveillance and monitoring, preventive care, integrated care, and continuity of care [6].In 2022, the National Health Commission issued the "Guiding Opinions on Promoting the High-quality Development of Family Doctor Contracted Services(FDCS)" (National Health and Basic [2022] No. 10), which further emphasized the need to progressively expand the coverage of FDCS while ensuring service quality, residents' satisfaction, and their sense of medical gain from the contract [7]. Residents' sense of medical gain is gradually becoming an important indicator for evaluating the quality of medical services in China.
In the context of Chinese society, the concept of "sense of gain(SG)" aims to depict the living conditions experienced by citizens, reflecting their subjective evaluation of benefits derived during social development [8]. Literally, "sense of gain" refers to the feeling one experiences as a result of obtaining something, encompassing both objective and subjective aspects [9]. Objective gain is not only reflected in material and economic acquisition but also in the attainment of personal rights, self-worth, and participation [10]. From the perspective of evaluative content and standards, "sense of gain" arises within a specific policy context. The evaluators, who are both the recipients and experiencers, assess and perceive the outcomes based on the tangible benefits derived from the relevant policy background [11]. Patient-perceived Sense of Medical Gain(PSMG) refers to the subjective perception of patients regarding the various benefits and experiences gained during the process of receiving healthcare services, reflecting their satisfaction, perspectives, and evaluations of medical services [12, 13].
Similar to PSMG, patient satisfaction (PS) and patient experience(PE) are commonly used metrics to reflect the quality of medical care. Scholar Risser [14] defines patient satisfaction as the consistency between the ideal medical service desired by patients and the actual medical service they receive. Harvey Picker [15] conceptualizes "patient experience" as patients' experiences with healthcare and the feedback received from them about these experiences. Both are evaluation metrics for measuring hospital service quality, aimed at improving the quality of medical care and enhancing patient experience. However, PS surveys are gradually revealing shortcomings in reflecting patient medical experiences and addressing patient needs, as they primarily analyze and judge based on patients' subjective thoughts, focusing only on outcomes while neglecting the process. PE surveys serve as complementary research to patient satisfaction surveys, placing greater emphasis on patients' factual recall of their treatment situations [16].Compared to the aforementioned two indicators, the sense of medical gain is more social and pragmatic. Evaluating the sense of medical gain must be grounded in the societal era and policy context. It requires a comprehensive analysis of how well patients' perceptions align with the medical services, environment, fairness, and participation provided by hospitals under current conditions, as well as their actual treatment outcomes and emotional value fulfillment [17].
In recent years, with the continuous development and reform of the healthcare system, patients have gradually shifted from passive recipients to active participants in the medical process. The "Healthy China 2030" Planning Outline proposes the comprehensive implementation of clinical pathway management to standardize diagnostic and treatment behaviors, optimize treatment processes, and enhance patients' sense of medical gain [18]. Thus, the sense of medical gain is a concrete manifestation of the broader concept of gain within the healthcare sector. It reflects the true experiences of residents with the services provided by medical institutions, from the perspective of China's healthcare development [19].
Against this backdrop, Patient-perceived Sense of Medical Gain (PSMG) has emerged as an increasingly important research area. PSMG not only relates to patients' subjective well-being and health outcomes but also influences their satisfaction with and trust in medical services. Despite its widespread mention in both theory and practice, research on PSMG remains speculative and normative, emphasizing the importance of patients' perceived benefits and calling for more focused studies in this field. As a subjective perception, PSMG requires in-depth investigation at the micro-level. However, theoretical research on PSMG is currently scarce, and there is a lack of effective measurement tools. These issues significantly hinder further exploration in the field, leading to inconsistent and incomparable results across different research and application contexts.
The promotion of the family doctor system is a crucial component of healthcare reform, aimed at enhancing patients' health management and overall medical experience through continuous and personalized medical services. Within this context, understanding and measuring patients' sense of medical gain (PSMG) related to family doctor services presents new challenges. Family doctor services encompass not only patients' actual medical needs but also their expectations and experiences with medical services, all of which must be quantified and assessed using scientific scales.The present study aims to develop a PSMG-FD measurement scale tailored for the context of family doctor services. Specifically, the objectives are to (1) identify the key dimensions of patients' sense of medical gain and (2) create a reliable and valid measurement scale.
Hypotheses: The reliability and validity of the scale will be evaluated through empirical research to ensure its effectiveness in this specific healthcare setting. It is hypothesized that (1) the PSMG-FD scale will demonstrate satisfactory reliability, with a Cronbach’s alpha coefficient exceeding 0.7, and (2) the scale will exhibit strong convergent validity, with average variance extracted (AVE) values surpassing the threshold of 0.5.
Materials and methods
Scale development procedure
In the first phase, relevant articles on sense of gain(SG) are collected to summarize and define the concept of Patients' sense of medical gain(PSMG) in the context of family doctor services. In the second phase, based on the definition of PSMG, a questionnaire bank is developed through literature review and brainstorming sessions. The initial item pool for the questionnaire, comprising 25 items, was developed through a combination of literature review and brainstorming sessions. These items were subsequently refined and selected through group discussions and two rounds of Delphi expert consultation, leading to the creation of a preliminary version of the questionnaire. A small-scale preliminary survey was then conducted with 50 outpatient participants. Based on their feedback regarding the clarity and comprehension of the items, further revisions were made. As a result, the final version of the questionnaire consists of 23 items, with improvements in both clarity and relevance.In the third phase, field surveys are conducted to adjust the content and structure of the questionnaire items using classical measurement theory and factor analysis. The internal consistency (Cronbach’s alpha coefficient), test-retest reliability, and split-half reliability are assessed to evaluate the reliability and validity of the questionnaire, resulting in the final version of the patients' sense of gain scale.The development of the PSMG-FD Scale followed a structured approach. Initially, items were derived from an extensive review of validated literature and existing frameworks. Expert reviews were conducted to ensure the relevance and clarity of the items. However, due to logistical and time constraints, direct patient involvement was not incorporated during the initial stages.This decision was made with the understanding that subsequent validation phases would include direct patient engagement, such as focus groups or interviews, to refine and enhance the scale. While this approach ensured psychometric rigor during the initial development phase, we acknowledge that the lack of patient input may limit the content validity of the scale, particularly its ability to fully capture patient perceptions.
Stage 1: Define the concept of PSMG on Family Doctor Contracting Services
"Sense of Gain (SG)" is a new localized concept based on the Chinese social context, used to describe the life situation of citizens [20].As research on the "sense of gain(SG)" progresses, Chinese researchers have made significant strides in exploring the Patients' sense of medical gain(PSMG) .Studies indicate that the PSMG reflects the actual factors obtained in the process of seeking medical treatment, such as the utilization of service resources required by residents during medical visits, including the availability of registration equipment in hospitals, access to examination and test reports, settlement of medical expenses, and the effectiveness of patient visits. On the subjective perception level, it includes patients' trust in medical staff, their awareness of risk factors during medical service processes, and whether their rights to informed consent and autonomous choice are respected [21].On the other hand, some scholars argue that PSMG reflects the extent to which the public shares in the achievements of healthcare reform, as well as their subjective perceptions and satisfaction with these achievements [22].
In the current research, there is no clear and unified definition of the concept of Patient-perceived Sense of Medical Gain (PSMG) in the context of family doctor services.Based on the analysis and reflection of previous literature, this study defines the Patients' sense of medical gain on family doctor contracting services (PSMG-FD) as follows: Objective cognitive evaluation of the convenience, continuity, reliability, and caring nature of actual medical services obtained to meet their own needs during the process of family doctor services, as well as the subjective perception of their medical experiences.
Stage 2: create a pool of items and form a first draft of the scale
Literature review
A search was conducted within the past three years, with the timeframe set at 2023 as the boundary. Relevant literature was queried in databases such as Pubmed, Web of Science, and CNKI using keywords such as "Family Doctor's contracting services" and "sense of medical gain," with a focus on the field of healthcare science services. The search yielded a total of 860 articles from Pubmed, 911 articles from Web of Science, and 1042 articles from CNKI. Among these articles, particular attention was paid to the definition and dimensions of the questionnaire, and duplicate literature was excluded to establish a literature database.
Establishment of item pool
By analyzing relevant literature in the database, reviewing relevant scales, and using the Perceived Access to Health care model [23] as the theoretical basis, items were classified according to dimensions such as accessibility, reliability, acceptability, empathy, and experience. Based on expert opinions, group discussions , preliminary survey and brainstorming were conducted to establish the item pool for the scale. The final item pool of the scale includes five dimensions: Medical Convenience (5 items), Medical Continuity (4 items), Medical Reliability(4 items), Medical Humanistic Care(4 items), and Medical Experience(6 items), totaling 23 items.
Delphi method
Also known as expert consultation method, the authority coefficient is used to measure the results of expert consultation, which is determined by the experts' familiarity with the subject matter and their judgment criteria. An authority coefficient greater than 0.7 indicates a high level of authority in the expert consultation. The degree of coordination of expert opinions is evaluated using the coefficient of variation and Kendall's W coefficient, where a larger W value indicates better coordination of opinions [24]. Selection criteria for experts include: (1) engagement in public health, family medicine, community nursing, general practice, and related fields; (2) possessing more than 5 years of relevant work experience; (3) voluntary participation in this study and active involvement in multiple rounds of expert consultation. We ultimately invited 20 experts.
Expert consultation
The average working experience of the 20 experts is 19±6.7 years. Among them, there are 3 experts with intermediate professional titles and 16 experts with senior professional titles. Fourteen experts have a postgraduate degree or above and are quite familiar with the contracted family doctor services system and related areas of perceived access. The coefficient for the experts' judgment criteria in the first round is 0.920, familiarity coefficient is 0.730, and authority coefficient is 0.825, indicating a high level of authority in the expert consultation. Based on expert opinions and group discussions, the decision was made to remove the items "You would choose to see a family doctor first when you feel unwell" and "Family doctors are friendly and kind when providing services," and to modify the wording of some items. Subsequently, the modified scale underwent a second round of expert consultation, resulting in an authority coefficient of 0.930 and a Kendall's W coordination coefficient of expert opinions of 0.221 (P<0.05). The importance scores of each item ranged from 3.850 to 4.800, with coefficients of variation (CV) ranging from 0.091 to 0.209 and satisfaction ratios ranging from 0.150 to 0.850. The satisfaction ratios for the items "Family doctors provide health education, health counseling, and guidance on health behaviors (diet, sleep, smoking cessation or reduction, alcohol reduction, exercise, etc.)" and "You are satisfied with the comfort of the medical environment" were 0.200 and 0.250, respectively, which did not reach the threshold value of 0.390. However, their CVs were all below the threshold of 0.167, and they were retained after discussions with experts and the research team. After modifying the wording of some items, a small-scale pre-survey was conducted, and the statistical results of the pre-survey ultimately formed a 5-dimensional, 23-item scale of Patients' sense of medical gain on family doctor contracting services (PSMG-FD).
Stage 3: main survey, completion of the scale
Participants and sample size
The participants in this study were selected from family doctor-contracted patients who visited the outpatient departments of five community health service centers in Jiangmen and Dongguan cities, Guangdong Province. Based on the Kendall rough sample size estimation method, which suggests that the sample size should be at least 5 to 10 times the number of items in the scale, we initially planned to select at least 250 samples for both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). In total, 600 participants were successfully recruited for the study. This sample size met the requirements for both EFA and CFA, ensuring sufficient statistical power for our analyses.
Data collection
Initially, this study used cluster sampling to select 3 community health service centers in Jiangmen and 2 in Dongguan. Using a convenience sampling method, one-on-one questioning was conducted with the signed patients in the outpatient departments of these 5 community health service centers, or patients were asked to fill out the questionnaire themselves for data collection. Simultaneously, interviewers underwent uniform training and used standardized language during questioning to minimize objective interference, maximize the restoration of patients' subjective feelings, and control information bias.
The assignment of scale scores
We ultimately developed a “Sense of Medical Gain Scale”for family doctor signing patients. This scale comprises 5 dimensions and 19 items, with scoring conducted using a summative scoring method. Specifically, we assigned scores to each item based on the 5-point scale levels, where a score of 1 indicated "strongly disagree," 2 indicated "disagree," 3 indicated "neutral," 4 indicated "agree," and 5 indicated "strongly agree." Subsequently, the scores for each item were summed to calculate the total score for each respondent. The score range is from 19 to 95 points, with the patients' sense of medical gain classified into three levels based on the total score: low (19–58 points), moderate (59–77 points), and high (78–95 points). A higher score indicates a higher level of medical gain perception regarding family doctor signing services.
Statistical analysis
Using SPSS 23.0 for correlation analysis, exploratory factor analysis, and reliability evaluation, and AmosGraphics 26.0 for confirmatory factor analysis.
Item selection
Items were selected based on classical measurement theory. Three classical measurement theory methods were employed, and items meeting two or more retention criteria were retained.
①Critical Ratio Method: Scores in the top 27% were defined as the high-score group, while scores in the bottom 27% were defined as the low-score group. Mean and standard deviation were calculated for both groups, and an independent samples t-test was used to compare score differences between the two groups. Items with no statistically significant differences were removed. ②Correlation Coefficient Method: Spearman's correlation coefficient was used to calculate the correlation between item scores and the total score of the scale. Items with correlation coefficients <0.400 were excluded.③Cronbach's Alpha Coefficient Method: If the removal of an item resulted in an increase in the total scale's Cronbach's Alpha coefficient, it indicated low homogeneity for that item, and consideration was given to its removal. Items that, when removed, lowered the Cronbach's Alpha coefficient were retained [25, 26].
Factor analysis
Exploratory factor analysis (EFA) [27] and confirmatory factor analysis (CFA) [28] were used to assess the structural validity of the scale. EFA is typically used to extract a comprehensive factor structure from a set of related data, while CFA is used to evaluate the fit of this factor structure. Principal component analysis and maximum variance rotation were employed to group items in the scale into several factors. EFA utilized principal component analysis and orthogonal maximum variance rotation to extract fixed common factors, deleting items with factor loadings <0.40 and multiple loadings. Generally, factor analysis is considered meaningful only when the Kaiser-Meyer-Olkin (KMO) value is >0.7 and Bartlett's test is <0.05. If each item's corresponding factor loading is >0.5 and the cumulative variance contribution rate is >50%, it indicates good internal structural validity of the scale [29]. Confirmatory factor analysis (CFA) employs model fitting, where a model is considered well-fitted if the model's chi-square degrees of freedom (CMIN/DF) fall within the range of 1–3, root mean square residual (RMR) is <0.05, goodness-of-fit index (GFI) is ≥0.80, Tucker-Lewis index (TLI) is ≥0.90, comparative fit index (CFI) is ≥0.90, and root mean square error of approximation (RMSEA) is <0.08 [30]. Convergent validity is assessed using factor loadings, average variance extracted (AVE), and composite reliability (CR) values for scale items. A scale demonstrates good convergent validity when factor loadings are >0.50, AVE is >0.36, and CR is greater than 0.70.Discriminant validity is evaluated by comparing Pearson correlations with the square root of AVE. Good discriminant validity is indicated when the square root of AVE for each factor exceeds the maximum correlation between that factor and other factors.
Reliability and validity
Test-retest reliability and split-half reliability are commonly used to assess the reliability of a scale, typically represented by the simple correlation coefficient (r). r > 0.7 is generally considered a good level of confidence. Internal consistency is indicated by Cronbach's α coefficient, which is evaluated by calculating the scale's Cronbach's α coefficient. A Cronbach's α coefficient > 0.70 suggests good internal consistency of the scale.
Results
Characteristics of the PSMG-FD population
Sample 1 was obtained using cluster sampling, where 420 community outpatient patients were randomly selected from three communities and health centers in Jiangmen City, Guangdong Province, for a one-on-one questionnaire survey. Subsequently, patients who were not contracted with a family doctor and invalid questionnaires were excluded, resulting in a total of 300 valid questionnaires. This portion of the data was used for item analysis and exploratory factor analysis of the initial questionnaire. Participants in Sample 1 had an average age of 54.16 years (SD = 18.7 years), with 41.67% being men (men, n=125; women, n=175). Among them, 149 had chronic diseases (49.67%).
Additionally, we recruited 341 community outpatient patients from two community health service centers in Dongguan City, Guangdong Province, excluding those not contracted with a family doctor and invalid questionnaires, resulting in 300 valid questionnaires (Sample 2). Participants in Sample 2 had an average age of 53.37 years (SD = 18.34 years), with 44.33% being men (men, n=133; women, n=167). Among them, 159 patients had chronic diseases (53%). This portion of the data was used for confirmatory factor analysis (CFA) of the scale items. Informed consent was obtained from all participants before completing the scale(Table 1).
Table 1.
General demographic characteristics of Contracted patients
| Characteristic | Sample 1 | Sample 2 | ||
|---|---|---|---|---|
| M or N | % or SD | M or N | % or SD | |
| Age (years) | 54.16 | 18.7 | 53.37 | 18.34 |
| Gender | ||||
| Men | 125 | 41.67 | 133 | 44.33 |
| Women | 175 | 58.33 | 167 | 55.67 |
| Marital Status | ||||
| Single | 21 | 7.00 | 17 | 5.67 |
| Married | 241 | 80.33 | 240 | 80.00 |
| Divorced | 3 | 1.00 | 5 | 1.67 |
| Widowed | 28 | 9.33 | 34 | 11.33 |
| Other | 7 | 2.33 | 4 | 1.33 |
| Education Level | ||||
| Junior high school or below | 150 | 50.00 | 142 | 47.33 |
| High school / Vocational school | 46 | 15.33 | 47 | 15.67 |
| University | 37 | 12.33 | 49 | 16.33 |
| Bachelor's degree or higher | 67 | 22.33 | 62 | 20.67 |
| Income | ||||
| ≤ $2000 | 105 | 35.00 | 101 | 33.67 |
| $2001-$4000 | 50 | 16.67 | 50 | 16.67 |
| $4001-$6000 | 53 | 17.67 | 51 | 17.00 |
| $6001-$8000 | 30 | 10.00 | 31 | 10.33 |
| ≥ $8000 | 62 | 20.67 | 67 | 22.33 |
| Residence | ||||
| Rural | 109 | 36.33 | 115 | 38.33 |
| Urban | 64 | 21.33 | 55 | 18.33 |
| City | 127 | 42.33 | 130 | 43.33 |
| Self-Rated Health Condition | ||||
| Poor | 47 | 15.67 | 54 | 18.00 |
| Fair | 135 | 45.00 | 125 | 41.67 |
| Good | 118 | 39.33 | 121 | 40.33 |
| Chronic Disease | ||||
| Yes | 149 | 49.67 | 159 | 53.00 |
| No | 151 | 50.33 | 141 | 47.00 |
M Mean, N Sample size, SD Standard Deviation
Items screening
Through independent sample t-tests, the 23 items obtained after eliminating biased items from the high (top 27%) and low (bottom 27%) scoring groups were examined. Significant differences were found in all 23 items. The correlation coefficient method was used to assess the correlation between items and the total score. The results showed that the correlation coefficient (r) values between items and dimension scores were all >0.4. However, the correlation coefficient (r) value between Item 1 and the total score was <0.4, indicating low representativeness for this item. The remaining items had r values >0.4, ranging from 0.420 to 0.786. Homogeneity was tested using Cronbach's α coefficient, which yielded a Cronbach's α coefficient of 0.950 for the scale. After removing Item 1 and Item 2, the internal consistency coefficient of the new scale increased. Considering this, Item 1 was deleted, while Item 2 showed better results in other analyses and was therefore retained (Table 2).
Table 2.
Summary of items screening results (n1 = 300)
| Item | High-low grouping comparison | Score of each dimension | Total score of the scale | The Cronbach’s αvalue of the deleted item | The Cronbach’s α value changes | Screening results |
|---|---|---|---|---|---|---|
| 1 | P < 0.001 | 0 .544** | 0.384** | 0.952 | ↑* | Delete |
| 2 | P < 0.001 | 0.700** | 0.420** | 0.954 | ↑* | Retain |
| 3 | P < 0.001 | 0.840** | 0.708** | 0.946 | ↓ | Retain |
| 4 | P < 0.001 | 0.818** | 0.669** | 0.947 | ↓ | Retain |
| 5 | P < 0.001 | 0.742** | 0.570** | 0.949 | - | Retain |
| 6 | P < 0.001 | 0.882** | 0.779** | 0.945 | ↓ | Retain |
| 7 | P < 0.001 | 0.899** | 0.759** | 0.946 | ↓ | Retain |
| 8 | P < 0.001 | 0.887** | 0.720** | 0.946 | ↓ | Retain |
| 9 | P < 0.001 | 0.883** | 0.702** | 0.947 | ↓ | Retain |
| 10 | P < 0.001 | 0.878** | 0.760** | 0.946 | ↓ | Retain |
| 11 | P < 0.001 | 0.930** | 0767** | 0.946 | ↓ | Retain |
| 12 | P < 0.001 | 0.928** | 0.778** | 0.946 | ↓ | Retain |
| 13 | P < 0.001 | 0.895** | 0.772** | 0.946 | ↓ | Retain |
| 14 | P < 0.001 | 0.886** | 0.737** | 0.946 | ↓ | Retain |
| 15 | P < 0.001 | 0.935** | 0.786** | 0.945 | ↓ | Retain |
| 16 | P < 0.001 | 0.920** | 0.765** | 0.946 | ↓ | Retain |
| 17 | P < 0.001 | 0.891** | 0.768** | 0.946 | ↓ | Retain |
| 18 | P < 0.001 | 0.655** | 0.701** | 0.946 | ↓ | Retain |
| 19 | P < 0.001 | 0.689** | 0.745** | 0.946 | ↓ | Retain |
| 20 | P < 0.001 | 0.714** | 0.766** | 0.946 | ↓ | Retain |
| 21 | P < 0.001 | 0.781** | 0.784** | 0.946 | ↓ | Retain |
| 22 | P < 0.001 | 0.810** | 0.737** | 0.946 | ↓ | Retain |
| 23 | P < 0.001 | 1.00** | 0.777** | 0.946 | ↓ | Retain |
Exploratory factor analysis
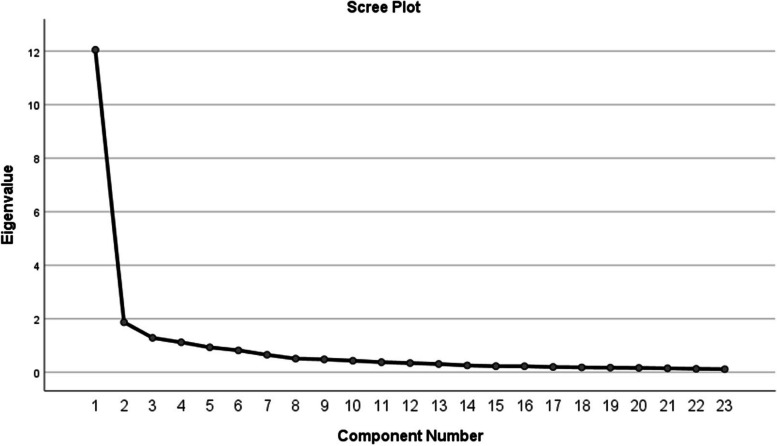
Due to the classification of question dimensions based on expert opinions and practical experience during the preparation of the questionnaire, exploratory factor analysis was conducted using the initial 300 questionnaire data. The validity was assessed through Kaiser-Meyer-Olkin (KMO) and Bartlett's test of sphericity. The KMO value was 0.932, which is greater than 0.60, and Bartlett's test of sphericity showed high significance (χ2 = 6212.342, df = 231, p < 0.01), indicating the presence of common factors among variables, making the data suitable for factor analysis. Principal component analysis was employed to extract factors, and rotation was performed using the varimax method, extracting a fixed number of five factors with a cumulative variance contribution rate of 78.763%. In terms of item inclusion criteria, the structure of the five factors was well preserved, with sufficient loadings and no cross-loadings. The communalities of variables ranged between 0.690 and 0.808. The first four factors each contained four items, with the first factor explaining 20.931% of the variance, labeled as "Medical Convenience" The second factor explained 15.215% of the variance, labeled as "Medical Continuity" The third factor explained 14.991% of the variance, labeled as "Medical Reliability" The fourth factor explained 14.905% of the variance, labeled as "Medical Humanistic Care" The fifth factor contained six items, explaining 14.905% of the variance, labeled as "Medical Experience" (Table 3, Fig. 1) .
Table 3.
Results of factor analysis for the PSMG-FD scale (n1 = 300)
| Sub-dimensions Item number |
Items | Factor loading | Variation explained (%) |
|---|---|---|---|
| Medical Convenience | 20.931 | ||
| 1 | You can conveniently use your smartphone/computer or other smart devices to make appointments, payments, and other services for family doctor visits | 0.748 | |
| 2 | You believe it is more convenient to obtain diagnosis and medication results through family doctor visits | 0.793 | |
| 3 | You believe it is more convenient to receive regular physical examinations through family doctor visits | 0.801 | |
| 4 | You believe that the night clinic services(19:00–23:00)provided by family doctors are more convenient | 0.719 | |
| Medical Continuity | 15.215 | ||
| 5 | When you visit the contracted institution for treatment, the family doctor can provide you with comprehensive and continuous medical services | 0.755 | |
| 6 | The family doctor understands your health issues and establishes a health record (including medication records) | 0.766 | |
| 7 | The family doctor can provide you with assistance in referral services | 0.779 | |
| 8 | The family doctor provides follow-up rehabilitation treatment and conducts tracking visits | 0.795 | |
| Medical Reliability | 14.991 | ||
| 9 | The family doctor can accurately record your information and keep your privacy confidential | 0.709 | |
| 10 | The family doctor's operational skills are proficient, making you feel reassured | 0.808 | |
| 11 | The medical skills of the family doctor make you feel reassured | 0.801 | |
| 12 | After receiving treatment from the family doctor, your condition has improved | 0.723 | |
| Medical Humanistic Care | 14.905 | ||
| 13 | The family doctor patiently listens to your description of your condition | 0.758 | |
| 14 | The family doctor will carefully introduce the treatment plan and costs to you, and solicit opinions | 0.765 | |
| 15 | The family doctor can provide psychological health guidance (such as helping you relieve anxiety, tension, and fear, psychological health knowledge education, etc.) | 0.742 | |
| 16 | The family doctor can provide health education, health consultation, and guidance on health behaviors (diet, sleep, quitting smoking and alcohol, moderate smoking and alcohol, exercise, etc.) | 0.699 | |
| Medical Experience | 12.722 | ||
| 17 | You are satisfied with the timing of your visit | 0.736 | |
| 18 | You are satisfied with the comfort of the medical environment | 0.796 | |
| 19 | You are satisfied with the service attitude of the family doctor | 0.690 | |
| 20 | You are satisfied with the professional technical level of the family doctor | 0.735 | |
| 21 | You are satisfied with the cost of the diagnosis and treatment | 0.753 | |
| 22 | Overall, the entire process of visiting the family doctor's office for treatment makes you satisfied | 0.774 |
Fig. 1.
Scree plot of exploratory factor analysis
Confirmatory factor analysis
The 300 data points from the formal survey were subjected to CFA calculations, revealing suboptimal model fit [χ2/df = 3.294, GFI = 0.830, RMSEA= 0.088]. To enhance model selection, potential modifications were considered, employing some recommended Maximum Likelihood estimation-based corrections (MIs) to reduce cross-loadings. Consequently, three items (19,20, 22) were removed. Through iterative adjustments, the modified model eventually encompassed 19 items across five factors, exhibiting the following fit indices: χ2/df = 2.781, RMSEA=0.077, RMR = 0.031, GFI = 0.875, NFI = 0.918, IFI = 0.946, TLI = 0.934, CFI = 0.945, and RFI = 0.901 (Table 4, Fig. 2) .
Table 4.
Goodness-of-fit of the PSMG-FD model(n2 = 300)
| CMIN/DF | RMSEA | RMR | GFI | TLI | CFI | NFI | IFI | |
|---|---|---|---|---|---|---|---|---|
| Initial Model | 3.294 | 0.088 | 0.031 | 0.830 | 0.907 | 0.920 | 0.890 | 0.920 |
| Adjusted Model | 2.781 | 0.077 | 0.031 | 0.875 | 0.934 | 0.945 | 0.918 | 0.946 |
| Recommended Range | 1–3 | < 0.08 | < 0.05 | ≥ 0.80 | ≥ 0.90 | ≥ 0.90 | ≥ 0.90 | ≥ 0.90 |
Fig. 2.
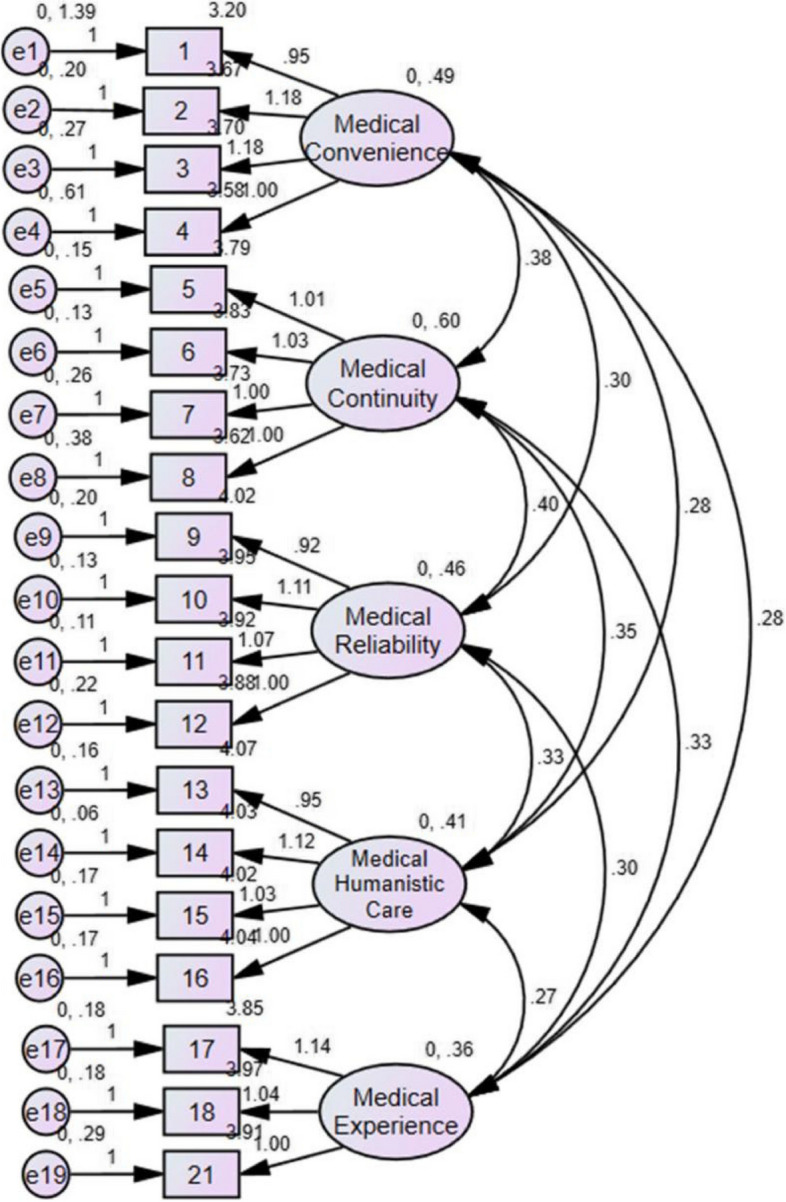
Structural equation model diagram of the PSMG-FD scale
Convergent validity and discriminant validity
The AVE values for different dimensions were 0.544, 0.739, 0.741, 0.755, and 0.654, all surpassing the threshold of 0.5. The CR values for each dimension were 0.820, 0.919, 0.919, 0.925, and 0.850, all exceeding 0.7, indicating satisfactory convergent validity(Table 5). The interdimensional correlation coefficients were lower than the square roots of the corresponding AVEs, suggesting correlation among latent variables while maintaining sufficient discriminant validity(Table 6).
Table 5.
Convergent validity of the PSMG-FD Scale(n2 = 300)
| Path | Factor loading(> 0.50) | AVE(> 0.50) | CR(> 0.7) |
|---|---|---|---|
| 4 < –Medical Convenience | 0.668 | 0.544 | 0.820 |
| 3 < –Medical Convenience | 0.846 | ||
| 2 < –Medical Convenience | 0.879 | ||
| 1 < –Medical Convenience | 0.492 | ||
| 8 < –Medical Continuity | 0.784 | 0.739 | 0.919 |
| 7 < –Medical Continuity | 0.835 | ||
| 6 < –Medical Continuity | 0.913 | ||
| 5 < –Medical Continuity | 0.900 | ||
| 12 < –Medical Reliability | 0.824 | 0.741 | 0.919 |
| 11 < –Medical Reliability | 0.907 | ||
| 10 < –Medical Reliability | 0.899 | ||
| 9 < –Medical Reliability | 0.809 | ||
| 16 < –Medical Humanistic Care | 0.837 | 0.755 | 0.925 |
| 15 < –Medical Humanistic Care | 0.849 | ||
| 14 < –Medical Humanistic Care | 0.949 | ||
| 13 < –Medical Humanistic Care | 0.835 | ||
| 21 < –Medical Experience | 0.745 | 0.654 | 0.850 |
| 18 < –Medical Experience | 0.824 | ||
| 17 < –Medical Experience | 0.854 |
Table 6.
Discriminant validity of the PSMG-FD Scale (n2 = 300)
| F1 | F2 | F3 | F4 | F5 | |
|---|---|---|---|---|---|
| F1 | 0.738 | ||||
| F2 | 0.695 | 0.860 | |||
| F3 | 0.625 | 0.752 | 0.861 | ||
| F4 | 0.616 | 0.706 | 0.752 | 0.869 | |
| F5 | 0.653 | 0.708 | 0.740 | 0.712 | 0.809 |
Reliability analysis
The internal consistency of the scale is typically evaluated through Cronbach's α coefficient for each dimension, with all five dimensions having Cronbach's α coefficients exceeding 0.7. The overall Cronbach's α coefficient for the scale is 0.947. Spearman-Brown correlation coefficients were computed for items divided into two equal parts randomly, showing that the split-half coefficients with dimension scores were all greater than 0.7, with a correlation coefficient of 0.895 with the total scale score. Within two weeks after the formal survey ended, 60 signed patients were randomly selected for a re-survey, resulting in 60 valid questionnaires collected. The intra-group correlation coefficients between each item and the total scale score were calculated for both measurements, indicating that the test-retest reliability coefficients for the seven domains ranged from 0.844 to 0.955, with an overall scale correlation coefficient of 0.955. For most domains, there was no statistically significant difference in total scores between the first and second assessments (p > 0.05) (Table 7).
Table 7.
Reliability coefficients of the total scale and each domain (n1 = 300)
| Dimensions | Items | Cronbach's a | Split-half reliability | Test–retest reliability(n = 60) |
|---|---|---|---|---|
| Medical Convenience | 4 | 0.789 | 0.796 | 0.910 |
| Continuity of Care | 4 | 0.917 | 0.884 | 0.890 |
| Reliability of Care | 4 | 0.917 | 0.912 | 0.954 |
| Caring Atmosphere in Healthcare | 4 | 0.922 | 0.894 | 0.844 |
| Medical Experience | 3 | 0.846 | 0.846 | 0.905 |
| Overall Scale | 19 | 0.947 | 0.895 | 0.955 |
Discussion
Instruments must be validated based on at least two aspects:validity and reliability. Validity is the extent of accuracy by which the instrument measures the target issue [31].This study introduces the concept of "Patients' Sense of Medical Gain (PSMG)" into the field of family doctors and systematically explores important issues such as definition and measurement of this concept. A procedural decision-making process was employed to develop a scale instrument for measuring patients' sense of medical gain in family doctor contracting services. In terms of instrument validity verification, we ensured through extensive literature review, group discussions, and Delphi survey method that the content and indicators of the scale accurately measure patients' sense of medical gain from family doctor contracting services. We also conducted preliminary questionnaire surveys and on-site interviews to capture patients' subjective feelings and feedback on medical services, further validating the effectiveness of the scale. This process ensured good content validity and a sound conceptual structure for the instrument. The final PSMG-FD scale consists of 5 dimensions and 19 items, demonstrating good reliability and validity, making it an effective assessment tool.
In the item analysis, the original item 1 "You can reach the family doctor/community hospital within a walking distance of less than 15 minutes." was removed due to its low dimension correlation (<0.40) and poor internal consistency [32]. 62% of the contracted patients selected 4 points or above for this item, indicating that the majority of contracted patients "basically agree" or "definitely agree" on the influence of medical distance on their sense of medical gain.
Factor analysis revealed that the EFA results showed an explained variance of 78.763% after rotation, which is greater than 50%. The components extracted from the data were consistent with the theoretical structure, confirming the structural validity of the scale and indicating effective extraction of information from the items. Similarly, their factor loadings were >0.50, but the fit indices of the initial patient medical gain model were not ideal [χ2(274) = 3.294, GFI = 0.830, RMSEA= 0.088]. To improve the model fit, we reexamined the items and referred to recommended model modification indices (MIs) [33]. We found that items C20, C21, and C23 had redundant or overlapping information, so they were removed in the model adjustment. The fit indices of the adjusted patient medical gain model significantly improved [χ2/df = 2.781, GFI=0.875, RMSEA = 0.077, RMR=0.031, NFI=0.918, IFI=0.946, TLI=0.934, CFI=0.945, and RFI=0.901] [34].The AVE values are all >0.5 and the CR values are all above 0.7, which meets the convergence validity criteria. The fact that the correlation coefficients between the dimensions of the scale are less than the square root of the respective AVE values indicates the presence of correlation between latent variables, demonstrating the discriminant validity of the scale is ideal [35].
Reliability refers to the consistency or repeatability of item scores from one assessment to another. The reliability of the scale was investigated using measures of internal consistency reliability (Cronbach’s α), split-half reliability, and test-retest reliability. The results indicate that the internal consistency coefficients for each domain of the scale and the total score are all greater than 0.7. The split-half reliability for both the scale domains and the total score is >0.70. Notably, the test-retest reliability coefficient for the total score is 0.955, while the test-retest reliability coefficients for individual domain scores are all >0.80 [36].These results suggest that the instrument demonstrates good reliability.
As "Patients' sense of medical gain(P-SMG) " is a unique concept in China, there is currently no research on patient medical gain-related scales internationally. However, researchers have extensively studied evaluation tools for primary healthcare services, such as the Primary Care Assessment Tools (PCAT) [37]and the Quality and Outcomes Framework (QOF) [38]. These tools have been widely used in evaluating the quality of family doctor services and primary healthcare [39–41]. Each tool has its strengths, but due to multiple indicators, lengthy assessment times, cultural differences, and applicability issues with certain dimensions (such as initial consultations) in the current research on patients' sense of medical gain in China's family doctor visits, their utility is somewhat limited to understanding overall and relative quality levels across dimensions [42].
Our study focuses on the micro perspective of family doctor signing services in primary healthcare, constructing a Patient Medical Gain Scale to address the applicability issues of existing tools in the research on patient medical gain in China's family doctor visits. During the scale construction process, we particularly focused on cultural differences. For example, our team found during visits that signed patients have a strong demand for referral services and prefer community simplification of the process, with referrals handled by family doctors to improve efficiency. Therefore, we paid special attention to this item. Importantly, the research suggests that a doctor's humanistic care can influence patient needs and experiences [43].Thus, our team considered the evaluation of signed patients' attitudes and tone towards family doctors, as well as their need for psychological health guidance, as an important dimension, labeling it as medical humanistic care, a dimension not seen as a separate dimension in other related literature and tools.
Lastly, building upon the review of patient medical experiences and satisfaction studies, we focused on aligning signed medical needs with satisfaction, incorporating satisfaction into the construction of the sense of medical gain index.
A key limitation of this study is the absence of direct patient involvement during the initial stage of scale development. This omission may introduce potential biases in item relevance and scope, thereby affecting the content validity of the scale. For a tool designed to measure patient perceptions, the lack of patient input is a notable constraint.While the psychometric analyses demonstrated satisfactory reliability and validity (e.g., construct validity, reliability, AVE, and CR values), we recognize that these findings should be interpreted with caution. The absence of patient perspectives during item selection may limit the scale’s ability to comprehensively reflect the lived experiences of the target population.Despite this limitation, the scale provides a practical starting point for evaluating patient perceptions and identifying areas for improvement in healthcare delivery. Its psychometric properties confirm its potential utility as an evaluative tool. To address the identified limitations, we commit to incorporating patient engagement in subsequent iterations of the scale. Future phases will involve focus groups and interviews to refine the items, ensuring a more patient-centered approach to scale development.Second, there is the potential for selection bias in the sample and reliance on self-reported measures, which may impact the generalizability of our results. Third, while the factor structure of the scale demonstrates high internal consistency and good validity, we did not assess criterion validity. Finally, our study was conducted in specific regions, which may limit the applicability of the findings to other settings.Future research will include a more diverse sample, assess criterion validity by comparing with established measures, and incorporate patient input through focus groups to refine the scale and enhance its relevance.
Conclusions
We have developed a Patient Medical Gain Scale to assess patients' medical experiences under the family doctor signing environment. Our analysis identified five key factors, totaling 19 items: medical convenience, medical continuity, medical reliability, medical humanistic care, and medical experience. The results of our study indicate that this Patient Medical Gain Scale for family doctor signing patients is a reliable and effective tool. These findings underscore the importance of family doctor signing programs in enhancing patients' sense of well-being and satisfaction in primary healthcare settings. This suggests that policymakers and healthcare administrators should prioritize the implementation and support of family doctor programs to improve patient care and health outcomes.
Supplementary Information
Abbreviations
- SG
Sense of gain
- P-SMG
Patients' sense of medical gain
- PS
Patient satisfaction
- PE
Patient experience
- PSMG-FD
Patients' sense of medical gain on family doctor contracting services
- EFA
Exploratory Factor Analysis
- CFA
Confirmatory Factor Analysis
- PCA
Principal Component Analysis
- RMSEA
Root Mean Square Error of Approximation
- RMR
Root Mean Square Residual
- GFI
Goodness-of-Fit Index
- CFI
Comparative Fit Index
- IFI
Incremental Fit Index
- TLI
Tucker-Lewis Index
- AVE
Average Variance Extracted
Authors’ contributions
JQZ and RML designed the study. CHO, YFC, and TFH conducted data collection. JQZ and CHO performed data analysis and drafted the manuscript. YXL and RML conducted extensive revisions of the manuscript. All authors interpreted the data, read, and approved the final manuscript.
Funding
This work was supported by the 2020 Annual Guangdong Provincial Philosophy and Social Science Planning Project(GD20CGL45 for Ruiming Liu) and the 2022 Annual Routine Project of Guangdong Provincial Philosophy and Social Science Planning(GD22YGL21 for Yuxi Liu).
Data availability
Data availability The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This research was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the IRB (institutional review board) of the affiliated hospital of Guangdong Medical University (YS2022092, YJYS2022092). Informed consent was obtained from all the subjects who participated in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Taylor RB. Family Medicine: Current Issues and Future Practice. In: Taylor RB, David AK, Johnson TA, Phillips DM, Scherger JE, eds. Family Medicine. Springer; 1998:1–20. 10.1007/978-1-4757-2947-4_1
- 2.Shang X, Huang Y, Li B, et al. Residents’ awareness of family doctor contract services, status of contract with a family doctor, and contract service needs in Zhejiang Province, China: a cross-sectional study. Int J Environ Res Public Health. 2019;16:3312. 10.3390/ijerph16183312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medical Reform Office of the State Council of China. Notice on the issuance of guidelines on the promotion of contract services for family doctors. Available at: http://www.gov.cn/xinwen/2016-06/06/content_5079984.htm. Accessed 24 Mar 2024.
- 4.Zhang Z, Zhang R, Peng Y, et al. Barriers and facilitators of family doctor contract services in caring for disabled older adults in Beijing, China: a mixed methods study. BMJ Open. 2023;13(6): e070130. 10.1136/bmjopen-2022-070130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yellamaty V, Ball L, Crossland L, et al. General practitioners with special interests: an integrative review of their role, impact and potential for the future. Aust J Gen Pract. 2019;48:639–43. 10.31128/AJGP-02-19-4849. [DOI] [PubMed] [Google Scholar]
- 6.Lee JQ, Loke W, Ng QX. The role of family physicians in a pandemic: A blueprint. Healthcare. Published online n.d.;8:198. 10.3390/healthcare8030198 [DOI] [PMC free article] [PubMed]
- 7.The State Council Information Office of the People's Republic of China.2022. https://www.gov.cn/zhengce/zhengceku/2022-03/15/content_5679177.htm. Accessed 24 Mar 2024.
- 8.Cao XQ, Li S. The connotation of “Gain” and the foreign experiences. Front. 2017;6:18–28. 10.16619/j.cnki.rmltxsqy.2017.02.002. [Google Scholar]
- 9.Ding YZ. To make residents have a sense of gain, we must open up the last kilometer - the practice path of community governance innovation in the new era. Governance. 2016;3:18–23. 10.16619/j.cnki.cn10-1264/d.2016.02.004. [Google Scholar]
- 10.Liu X. The Connotation and Evaluation Index System Construction of Sense of Gain. Old Area Development. 2019;04:56–60. [Google Scholar]
- 11.Xing Z, Niu Q. Sense of gain: A New Benchmark for Shared Development from the Perspective of Supply and Demand. Theoretical Studies Journal. 2017;05:107–12. 10.14110/j.cnki.cn-37-1059/d.2017.05.015. [Google Scholar]
- 12.Yang W, Wang X, Wang F, et al. Study on the Influencing Factors of Patients’ Sense of Gain of the Medical Treatment from the Perspective of Multiple Subjects. Chinese Hospital Management. 2021;41(1):36–9. [Google Scholar]
- 13.Qiu H, Zou L, Zou Y, et al. Evaluation on Effectiveness of Compensation Mechanism Reform in Foshan from Perspective of Patients’ Sense of Gain. Chinese Journal of Health Quality Management. 2023;30(08):94–7. 10.13912/j.cnki.chqm.2023.30.8.20. [Google Scholar]
- 14.Risser NL. Development of an instrument to measure patient satisfaction with nurses and nursing care in primary care settings. Nurs Res. 1975;24(1):45–52. [PubMed] [Google Scholar]
- 15.Ahmed F, Burt J, Roland M. Measuring patient experience: concepts and methods. Patient. 2014;7(3):235–41. [DOI] [PubMed] [Google Scholar]
- 16.Ye C. Measurement and Analysis of Patient's Sense of Medical Gain Experience and Satisfaction Based on Value Co-creation [Dissertation]. Guangzhou University of Chinese Medicine; 2023. 10.27044/d.cnki.ggzzu.2023.000009.
- 17.Ding S. Research on the Construction of Evaluation Index System for Elderly Patients' Sense of Medical Gain [Dissertation]. Guangzhou University of Chinese Medicine; 2023. 10.27044/d.cnki.ggzzu.2023.000017.
- 18.The Central Committee of the Communist Party of China and the State Council. "Healthy China 2030" Planning Outline [EB/OL]. (2016–10–25) [2023–08–05]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm.
- 19.Wang K, Zhao X, Na W, et al. A study on the sense of gain from primary medical reform among rural residents in Da’an City, Jilin Province—Taking Shaoguo Town of Da’an City as an example[J]. Chinese Rural Health. 2017;21:72–5. [Google Scholar]
- 20.Jiang YM, Zhang XL. The shared development and comprehensively build a well-off society. Leading Journal of Ideological and Theoretical Education. 2016;23:74–8. 10.16580/j.sxlljydk.2016.03.015. [Google Scholar]
- 21.Qian Y, Wang XH, Chen J, et al. Conceptual Connotation, Element Analysis and Research Prospects of Doctor-patient Acquisition in the New Era. Chinese Hospital Management. 2021;41(1):22–6. [Google Scholar]
- 22.Chen H, Li S, Zhao L.Investigation of Sense of Gain in Medical Treatment of Rural Residents in a Town of Jining City Under Background of Healthy China. Medicine and Society. 2018;31(10):54–56+66. 10.13723/j.yxysh.2018.10.018.
- 23.Hoseini-Esfidarjani SS, Negarandeh R, Delavar F, Janani L. Psychometric evaluation of the perceived access to health care questionnaire. BMC Health Serv Res. 2021;21(1):638. 10.1186/s12913-021-06655-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs. 1994;19:1221–5. 10.1111/j.1365-2648.1994.tb01207.x. [DOI] [PubMed] [Google Scholar]
- 25.Yang Z, Wang H, Wang A. Psychometric evaluation of the Chinese version of advance care planning self-efficacy scale among clinical nurses. BMC Palliat Care. 2022;21(1):175. 10.1186/s12904-022-01064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gorsuch RL. Exploratory factor analysis: its role in item analysis. J Pers Assess. 1997;68(3):532–60. 10.1207/s15327752jpa6803_5. [DOI] [PubMed] [Google Scholar]
- 27.Rand S, Towers AM, Allan S, et al. Exploratory factor analysis and Rasch analysis to assess the structural validity of the Adult Social Care Outcomes Toolkit Proxy version (ASCOT-Proxy) completed by care home staff. Qual Life Res. 2024;33(6):1555–67. 10.1007/s11136-024-03631-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zimmerman K, Snyder M, Elkins GR. Confirmatory Factor Analysis of the Elkins Hypnotizability Scale in a Clinical Population. Int J Clin Exp Hypn. 2024;72(1):4–15. 10.1080/00207144.2023.2279680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Courtney M, Gordon R. Determining the number of factors to retain in EFA: using the SPSS R-menu v2 0 to make more judicious estimations. Pract Assess Res Eval. 2013;18:8. [Google Scholar]
- 30.Hu L-T, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3:424–53. [Google Scholar]
- 31.Ma G, Zhong Z, Duan Y, Shen Z, Qin N, Hu D. Development and validation of a self-quantification scale for patients with hypertension. Front Public Health. 2022;10: 849859. 10.3389/fpubh.2022.849859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhuang M, Li CC, Chen SY, et al. Development and validation of a Systemic Sclerosis Health Literacy Scale. Front Public Health. 2023;11:1038019. 10.3389/fpubh.2023.1038019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prinsen CA, Vohra S, Rose MR, Boers M, Tugwell P, Clarke M, et al. How to select outcome measurement instruments for outcomes included in a “Core Outcome Set” - a practical guideline. Trials. 2016;17:449. 10.1186/s13063-016-1555-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–57. 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacCallum R. Specification searches in covariance structure modeling. Psychol Bull. 1986;100(1):107–20. 10.1037/0033-2909.100.1.107. [Google Scholar]
- 36.Higuchi S, Osaki Y, Kinjo A, Mihara S, Maezono M, Kitayuguchi T, et al. Development and validation of a nine-item short screening test for ICD-11 gaming disorder (games test) and estimation of the prevalence in the general young population. J Behav Addict. 2021;10:263–80. 10.1556/2006.2021.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fracolli LA, Gomes MF, Nabão FR, Santos MS, Cappellini VK, de Almeida AC. Primary health care assessment tools: a literature review and metasynthesis. Cien Saude Colet. 2014;19(12):4851–60. 10.1590/1413-812320141912.00572014. [DOI] [PubMed] [Google Scholar]
- 38.Steel N, Willems S. Research learning from the UK Quality and Outcomes Framework: a review of existing research. Qual Prim Care. 2010;18(2):117–25. [PubMed] [Google Scholar]
- 39.Liu S, Meng W, Yu Q, et al. Evaluation and countermeasures of contracted services of Chinese family doctors from demanders’ point of view - a case study of a city. BMC Health Serv Res. 2022;22(1):1534. 10.1186/s12913-022-08891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu R, Shi L, Meng Y, et al. The institutional primary healthcare service quality and patients’ experiences in Chinese community health centres: results from the Greater Bay Area study, China. Int J Equity Health. 2021;20(1):198. 10.1186/s12939-021-01538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berra S, Rocha KB, Rodríguez-Sanz M, et al. Properties of a short questionnaire for assessing primary care experiences for children in a population survey. BMC Public Health. 2011;11:285. 10.1186/1471-2458-11-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu L, Liao X, Zhao Q, et al. Evaluation Common Foreign Quality Evaluation Tools of Primary Health Care and Their Implications for China. Chin Gen Pract. 2024;27(01):27–35. [Google Scholar]
- 43.Wang W, Zhang J, Lu J, Wei X. Patient views of the good doctor in primary care: a qualitative study in six provinces in China. Glob Health Res Policy. 2023;8(1):24. 10.1186/s41256-023-00309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data availability The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.