Abstract
Background
The payment methodology for diagnosis-related groups (DRG) has implications for both society and medical institutions. Our study aims to analyse the impact of the reform of the payment policy according to the DRG on the operation of a tertiary hospital in Anhui Province.
Methods
Monthly data were collected from April 2020 to September 2023 during the reform period for a tertiary hospital on nine types of operational indicators, including average length of stay (ALOS), number of discharges, number of outpatient visits, percentage of discharged patients undergoing level III or IV surgery, bed turnover rate, inpatient essential drug utilization rate, low-risk group mortality, outpatient subaverage cost and inpatient subaverage cost. The data were divided into two phases according to the time of DRG implementation: pre-reform (April 2020–December 2021) and post-reform (January 2022–September 2023), and the segmented regression model with interrupted time series data was used to analyse the changes in the trend of each type of indicator before and after the reform. Statistical analysis was performed using R software (4.3.1).
Results
After the implementation of the DRG, the number of discharges increased by 112 800 patients (95% confidence interval [CI] 31.125–194.484, P = 0.008), the bed turnover rate rose by 1.403% (95% CI 1.028–1.778, P = 0.022) and the percentage of discharged patients undergoing level III or IV surgery decreased by 0.098% (95% CI −0.181 to −0.015, P = 0.022). The low-risk group mortality decreased by 0.016% (95% CI −0.027 to −0.005, P = 0.007), and the inpatient subaverage cost decreased by 81.514 CNY (95% CI −121.782 to −41.245, P < 0.001). However, there were no significant differences in the trends of average length of stay, outpatient visits, inpatient essential drug utilization rate and outpatient subaverage cost after the DRG implementation.
Conclusions
The findings show that the DRG reform has positively impacted hospital functioning, including quality, safety, efficiency and costs. Although the average length of stay remained unchanged, there was an increase in discharged patients and outpatient visits, indicating hospitals adapted to the new payment model. The reduction in low-risk group mortality suggests improvements in patient safety and care quality. However, challenges remain, as evidenced by decreased surgical complexity and initial drops in bed turnover rates. While the DRG reform holds promise for enhancing healthcare efficiency and controlling costs, potential negative effects such as patient selection bias and coding changes need to be monitored. Future research should focus on the long-term effects of the DRG policy across different healthcare institutions.
Keywords: Interrupted time series analysis, DRG, Policy evaluation, ALOS, Medical cost
Background
Rising healthcare costs not only increase the burden of disease on patients but also have a knock-on effect on the healthcare system [1]. It is particularly important to regulate the payment of health insurance premiums. Diagnosis-related groups (DRG) is a management tool developed by American scholars in the 1970s, which is applied mainly to short-term evaluation of inpatient medical service performance and management of health insurance payments [2]. The DRG payment method is a system for managing cases with similar clinical courses and similar cost consumption in the same group through a case mix analysis method based on big data, taking into account the individual characteristics of the cases, such as age, sex, number of days of hospitalization, clinical diagnosis, diseases, surgeries, disease severity, comorbidities and complications and regressions, etc., and using the groups as the system is based on the group as a unit, and the standardization of medical costs is established for payment [3, 4]. Chinese health insurance payment method reform has been explored for more than a decade. The creation of the Health Care Authority in 2018 made healthcare payment methods one of the key elements of reform. DRG is a type of Medicare payment, and the effectiveness of DRG implementation varies across different levels of medical institutions in different regions [5–9].
Currently, the evaluation of the effect of the implementation of DRG is not consistent due to the idiosyncratic nature of the reform programs in each region in terms of the implementation environment, economic factors, etc. The basic idea of interrupted time series analysis (ITSA) is to assess the impact of an intervention on outcomes by continuously collecting outcome data at multiple time points before and after the intervention and comparing changes in levels and trends in outcomes before and after the intervention. The advantage of ITSA is that by analysing data from multiple observations before and after the intervention, even if no controls are set up, we can control for and exclude the influence of long-term trend changes caused by historical or other unmeasured confounders and, thus, correctly evaluate the true effect of the intervention on the outcome [10]. ITSA is considered to be the strongest quasi-experimental research design to assess the longitudinal effects of policy interventions and is one of the highest-quality research methods in current health policy evaluation [11]. The study population was selected from the largest medical institutions in the northern Anhui region, with the third largest comprehensive strength in Anhui province. The study used the ITSA research design to analyse the impact of the reform on the operation of medical institutions to provide a reference for the decision-making process for the implementation of DRG in different regions of China.
Methods
Data and sample
Convenience sampling was used to select patients from 2020 to 2023 in one of the largest tertiary care facilities in northern Anhui province for the study. The study included 526 887 inpatients and 684 3382 outpatients.
Study variables
We used expert consultation to select nine indicators for the study. Regrading the performance assessment indicators of national tertiary public hospitals, nine indicators were selected through expert consultation to assess the impact of DRG policy implementation on hospital operations, mainly in terms of hospital functional positioning, quality and safety, rational use of the drug, service efficiency and medical cost. The nine indicators were ALOS, the number of discharges, outpatient visits, the percentage of discharged patients undergoing level III or IV surgery, bed turnover rate, inpatient essential drug utilization rate, low-risk group mortality, outpatient subaverage cost and inpatient subaverage cost.
Statistical analysis
The paired t-test was first used to analyse the overall level differences of the nine indicators before and after the reform. The ITSA based segmented regression model was used to test the differences in the trends of the nine indicators before and after the reform, and the regression models were established as follows.
| 1 |
Equation (1), where represents the average level of the relevant indicator in month t; β0 is the estimate of the initial level of the indicator in the observation period, β1 is the slope of the trend of the indicator before the reform, β2 is the estimate of the instantaneous change in the level of the indicator before and after the reform, and β3 is the amount of change in the slope of the trend of the indicator after the reform; timet is the continuous time variable of the representative month of the observation period, taking values in the range of [1, 42], policyt is assigned 0 and 1 before and after the reform, postt is assigned 0 before the reform and postt = timet after the reform; Xt represents a covariate with fixed effects to account for seasonal factors that can affect some of the indicators, and represents the error term.
| 2 |
Equation 2 is based on Eq. 1, we added it as a dummy variable to the model to control for it, considering that the study may be influenced by coronavirus disease (COVID-19). Likewise, we consider seasonal trends in the study variables and fit the seasonality of the model by incorporating paired sine and cosine functions for every 12-month period [12].
A segmented regression model based on ordinary least squares regression (OLS) was fitted and the significance test of the regression coefficients was performed to explain whether the differences in the trends of the relevant operational indicators of medical institutions before and after the DRG reform were statistically significant. R-squared (R2) and adjusted R2 were used to assess the fit of the model. Breusch–Pagan (BP) test and Durbin–Watson (D–W) test were used to assess heteroskedasticity and autocorrelation. P-value in the BP test is greater than the significance level, the model is considered to be free of heteroskedasticity, if heteroskedasticity exists, we used weighted least squares (WLS) to correct for it [13]. Also, no autocorrelation was considered to be present if the D–W value was around 2, and vice versa by iterating the variables through Cochrane–Orcutt to control for the effect of autocorrelation on parameter estimation in the regression model [14]. In addition, to cope with the problem of multiple testing of the nine independent models in the study, correction for multiple comparisons was implemented using the Benjamini–Hochberg procedure to control the false discovery rate (FDR). Statistical analyses were performed using the R package, with P < 0.05 as a condition for significant differences.
Results
The overall level of operational indicators of the medical institution before and after the reform of the DRG
In our study, ALOS in tertiary hospitals was shortened after the reform, and the difference was statistically significant (P < 0.001), the number of discharges and outpatient visits increased (P < 0.05), inpatient essential drug utilization rate decreased (P < 0.001), outpatient subaverage costs increased (P = 0.001) and inpatient subaverage costs decreased (P < 0.001), and the difference in the overall level of change before and after the reform of other indicators was not statistically significant (P > 0.05), as presented in Table 1.
Table 1.
Overall level of operational indicators of the medical institution before and after the reform of the DRG
| Indicators | Before | After | t | P |
|---|---|---|---|---|
| ALOS (day) | 9.050 ± 0.449 | 8.145 ± 0.554 | 6.546 | < 0.001 |
| Number of discharges | 11 939.905 ± 1154.562 | 13 149.952 ± 2133.711 | −2.619 | 0.016 |
| Outpatient visits | 126 891.381 ± 11 938.517 | 140 854.524 ± 19 699.758 | −3.015 | 0.007 |
| Percentage of discharged patients undergoing level III or IV surgery (%) | 88.456 ± 1.144 | 88.568 ± 1.072 | −0.300 | 0.767 |
| Bed turnover rate (%) | 90.729 ± 5.513 | 90.804 ± 10.418 | −0.028 | 0.978 |
| Inpatient essential drug utilization rate (%) | 25.263 ± 1.183 | 21.565 ± 0.950 | 11.295 | < 0.001 |
| Low-risk group mortality (%) | 0.085 ± 0.058 | 0.091 ± 0.067 | −0.243 | 0.811 |
| Outpatient subaverage cost (CNY) | 395.496 ± 19.853 | 428.776 ± 28.192 | −4.042 | 0.001 |
| Inpatient subaverage cost (CNY) | 18 195.388 ± 778.962 | 15 797.062 ± 1505.222 | 7.606 | < 0.001 |
Trends in operational indicators of medical institution before and after the DRG reform
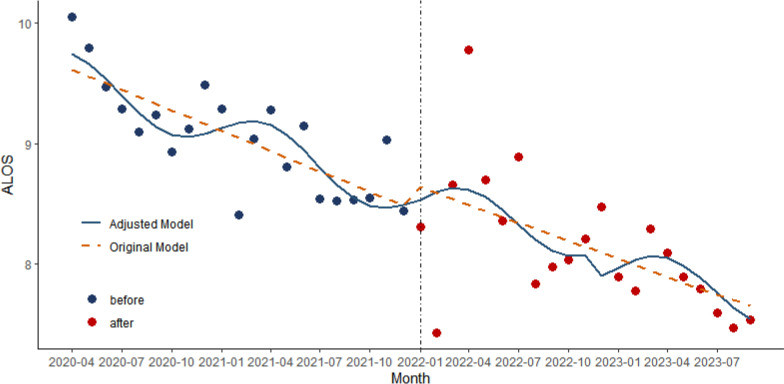
Model 1: ALOS as the dependent variable
As shown in Fig. 1, we fitted the original and adjusted models (considering COVID-19 and seasonal factors), and in the adjusted ALOS model, there was a significant downward trend in ALOS before the DRG policy intervention (β1 = −0.049, 95% CI −0.079 to −0.020, P < 0.01). However, there was no statistically significant difference in the trend of ALOS change at the instant of policy implementation (β2 = −0.442, 95% CI −2.467 to 1.584, P = 0.661) and after implementation (β3 = 0.020, 95% CI −0.058 to 0.098, P = 0.605) (Table 2). With an R2 of 0.717 and an adjusted R2 of 0.669, the model demonstrated strong explanatory power. The P-value in the BP test was 0.092, and the D–W test was 1.884.
Fig. 1.
Trend in ALOS for the medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
Table 2.
Trends in the operational indicators of medical institution before and after the reform of DRG
| Indicators | Trend before implementation | Instantaneous trend after implementation | Trend after implementation | |||
|---|---|---|---|---|---|---|
| β1 (95% CI) | P | β2 (95% CI) | P | β3 (95% CI) | P | |
| ALOS (day) | −0.049 (−0.079 to −0.020) | < 0.01 | −0.442 (−2.467 to 1.584) | 0.661 | 0.020 (−0.058 to 0.098) | 0.605 |
| Number of discharges | 133.790 (105.278–162.295) | < 0.001 | − 5150.940 (−7411.431 to − 2890.459) | < 0.001 | 112.800 (31.125–194.484) | 0.008 |
| Outpatient visits | 1660.560 (643.523–2677.595) | 0.002 | −18 421.560 (−88 070.570–51 227.440) | 0.595 | −85.63 (−2766.918–2595.661) | 0.948 |
| Percentage of discharged patients undergoing level III or IV surgery (%) | 0.127 (0.097–0.158) | < 0.001 | 0.956 (−1.448 to 3.360) | 0.425 | −0.098 (−0.181 to −0.015) | 0.022 |
| Bed turnover rate (%) | 0.354 (0.296–0.411) | < 0.001 | −47.730 (−58.680 to −36.780) | < 0.001 | 1.403 (1.028–1.778) | 0.022 |
| Inpatient essential drug utilization rate (%) | −0.209 (−0.360 to −0.058) | 0.008 | −1.568 (−7.299 to 4.163) | 0.579 | 0.068 (−0.186 to 0.322) | 0.590 |
| Low-risk group mortality (%) | 0.002 (−0.002 to 0.006) | 0.277 | 0.408 (0.120–0.695) | 0.007 | −0.016 (−0.027 to −0.005) | 0.007 |
| Outpatient subaverage cost(CNY) | 0.603 (−1.184 to 2.390) | 0.498 | 32.926 (−89.457 to 155.308) | 0.588 | 0.117 (−4.595 to 4.828) | 0.960 |
| Inpatient subaverage cost (CNY) | −49.945 (−63.375 to −36.514) | < 0.001 | 1457.794 (326.989–2588.599) | 0.013 | −81.514 (−121.782 to −41.245) | < 0.001 |
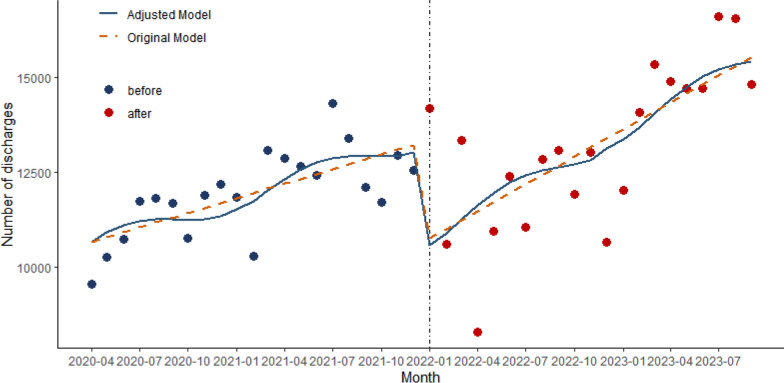
Model 2: number of discharges as the dependent variable
As shown in Fig. 2, in the adjusted modelling of the number of discharges, there was a significant upward trend before the policy intervention (β1 = 133.790, 95% CI 105.278–162.295, P < 0.001). However, there was a significant downward trend in the number of discharges change at the instant of policy implementation (β2 = −5150.940, 95% CI −7411.431 to −2890.459, P < 0.001) but turned to a significant upward trend after policy implementation (β3 = 112.800, 95% CI 31.125–194.484, P = 0.008) (Table 2). With an R2 of 0.987 and an adjusted R2 of 0.985, the model demonstrated strong explanatory power. The P-value in the BP test was 1, and the D–W test was 2.053.
Fig. 2.
Trend in the number of discharges from medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
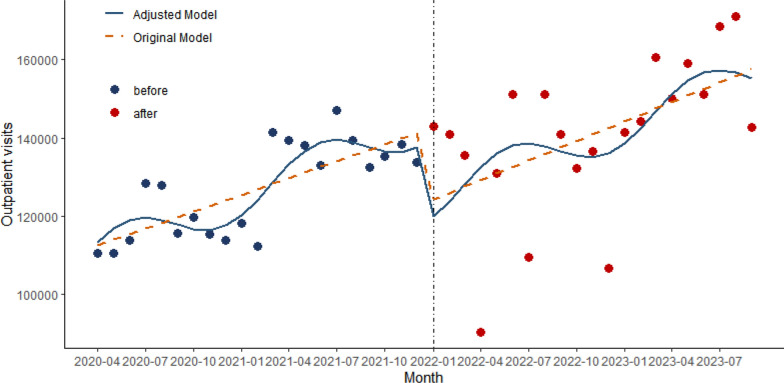
Model 3: outpatient visits as the dependent variable
As shown in Fig. 3, in the adjusted modelling of the outpatient visits, there was a significant upward trend before the policy intervention (β1 = 1660.560, 95% CI 643.523–2677.595, P = 0.002). However, the difference between the instantaneous (β2 = −18 421.560, 95% CI −88 070.570 to 51 227.440, P = 0.595) and postimplementation (β3 = −85.63, 95% CI −2766.918 to 2595.661, P = 0.948) impacts of DRG policy implementation on trends in outpatient visits was not statistically significant (Table 2). The value of R2 and adjusted R2 were 0.505 and 0.420. The P value in the BP test was 0.074, and the D–W test was 2.199.
Fig. 3.
Trend in outpatient visits for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
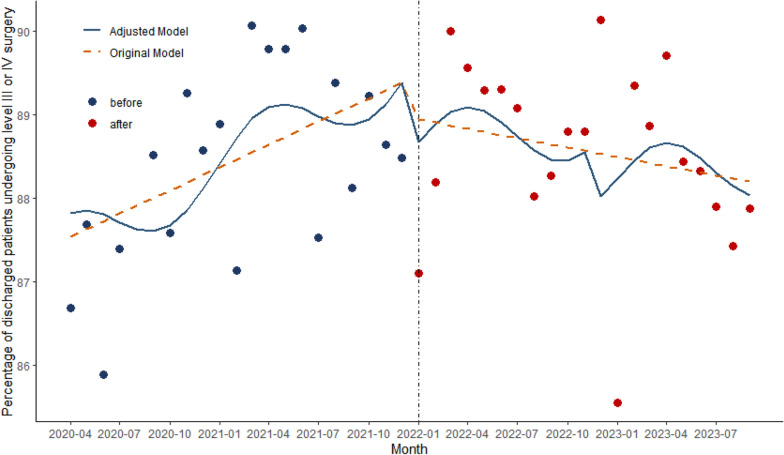
Model 4: percentage of discharged patients undergoing level III or IV surgery as the dependent variable
As shown in Fig. 4, in the adjusted modelling of the percentage of discharged patients undergoing level III or IV surgery, β1 was 0.127 (95% CI 0.097–0.158, P < 0.001), which indicated that there was a significant upward trend before the policy intervention. However, the difference in the trend of change was not statistically significant at the instant of policy implementation (β2 = 0.956, 95% CI −1.448 to 3.360, P = 0.425). After policy implementation, there was a significant downward trend (β3 = −0.098, 95% CI −0.181 to −0.015, P = 0.022) (Table 2). The value of R2 and adjusted R2 were 0.824 and 0.793. The P value in the BP test was less than 0.05, and the D–W test was 2.139.
Fig. 4.
Trend in the percentage of discharged patients undergoing level III or IV surgery for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
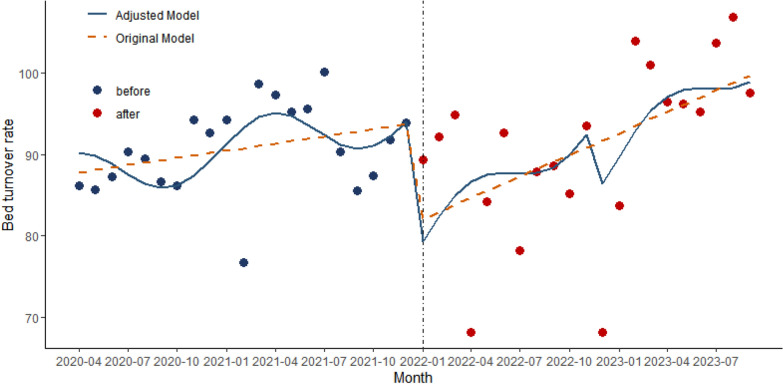
Model 5: bed turnover rate as the dependent variable
As shown in Fig. 5, in the adjusted bed turnover rate model, there was a significant upward trend before the policy intervention (β1 = 0.354, 95% CI 0.296–0.411, P < 0.001). The difference in the trend of change was statistically significant at the instant of policy implementation (β2 = −47.730, 95% CI −58.680 to −36.780, P < 0.001). Nevertheless, after policy implementation, there was a significant downward trend (β3 = 1.403, 95% CI 1.028–1.778, P = 0.022) (Table 2). The value of R2 and adjusted R2 were 0.990 and 0.988. The P value in the BP test was less than 1, and the D–W test was 1.809.
Fig. 5.
Trend in the bed turnover rate for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
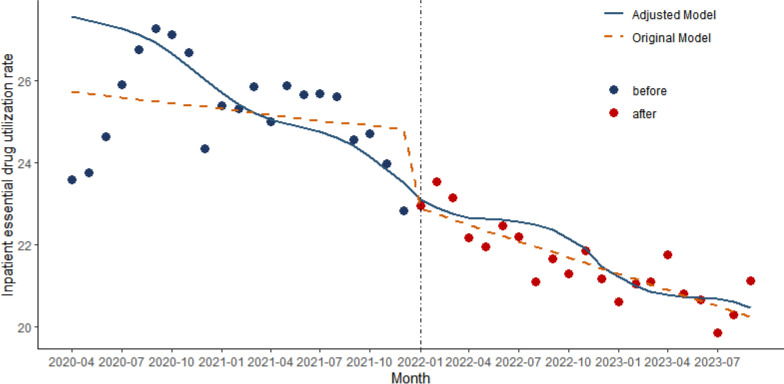
Model 6: inpatient essential drug utilization rate as the dependent variable
As shown in Fig. 6, in the model of inpatient essential drug utilization rate, β1 was −0.209 (95% CI −0.360 to −0.058, P = 0.008), indicating a decreasing trend in inpatient essential drug utilization before the reform. β2 value was −1.568 (95% CI −7.299 to 4.163, P = 0.579), and β3 was 0.068 (95% CI −0.186 to 0.322, P = 0.590), which indicates that the change in the trend of the implementation of the DRG policy on the inpatient essential drug utilization was not significant (Table 2). The value of R2 and adjusted R2 were 0.598 and 0.527. The P value in the BP test was 0.651, the D–W test was 0.893, corrected to 2.084.
Fig. 6.
Trend in inpatient essential drug utilization rate for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
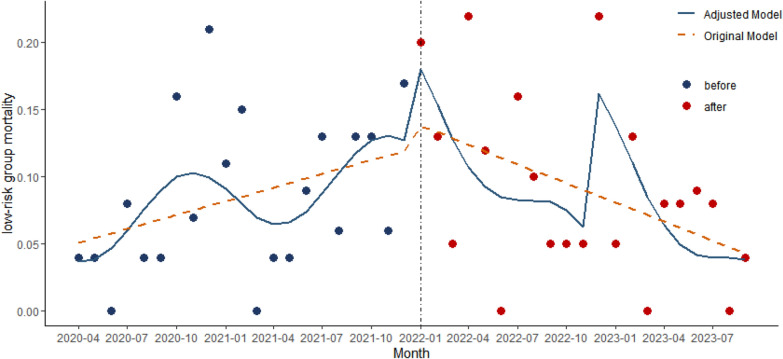
Model 7: low-risk group mortality as the dependent variable
As shown in Fig. 7, in the low-risk group mortality model, β1 was 0.002 (95% CI − 0.002 to 0.006, P = 0.277), which indicated that there was no significant trend before the policy intervention. β2 was 0.408 (95% CI 0.120–0.695, P = 0.007), suggesting an upward trend in low-risk group mortality before and for a short period after the implementation of the policy. β3 was −0.016 (95% CI −0.027 to −0.005, P = 0.007), suggesting that the trend change was significant downward after the DRG policy was launched (Table 2). The value of R2 and adjusted R2 were 0.324 and 0.208. The P-value in the BP test was 0.565. The D–W test was 2.595.
Fig. 7.
Trend in low-risk group mortality for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
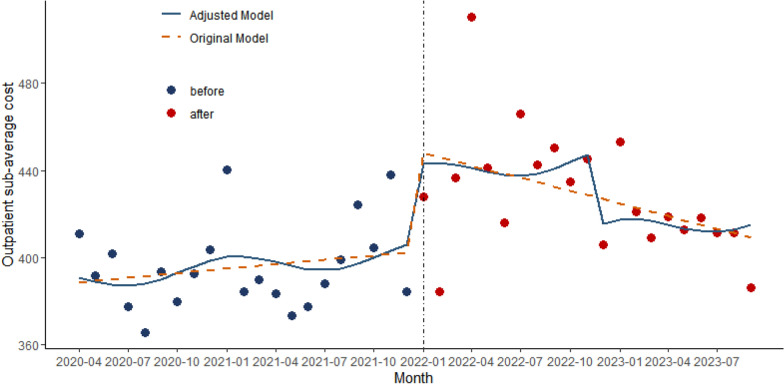
Model 8: outpatient subaverage cost as the dependent variable
As shown in Fig. 8, in the modelling of the outpatient subaverage cost, β1 was 0.603 (95% CI −1.184 to 2.390, P = 0.498), β2 was 32.926 (95% CI −89.457 to 155.308, P = 0.588), and β3 was 0.117 (95% CI −4.595 to 4.828, P = 0.960), indicating that there is no significant difference in the trend of the outpatient subaverage cost before and after the implementation of the DRG policy (Table 2). The value of R2 and adjusted R2 were 0.453 and 0.360. The P value in the BP test was 0.217. The D–W test was 1.850.
Fig. 8.
Trend in outpatient subaverage cost for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
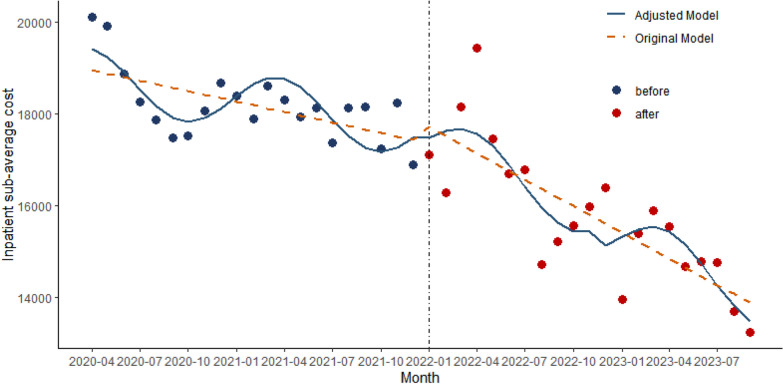
Model 9: inpatient subaverage cost as the dependent variable
As shown in Fig. 9, in the modelling of inpatient subaverage cost, β1 was −49.945 (95% CI −63.375 to −36.514, P < 0.001), indicating that there was a downward trend before the policy was implemented. β2 was 1457.794 (95% CI 326.989–2588.599, P = 0.013), which indicates that there was an upward trend in a short period after the policy was implemented. β3 was −81.514 (95% CI −121.782 to −41.245, P < 0.001), indicating that there was a downward trend after the policy was implemented (Table 2). With an R2 of 0.996 and an adjusted R2 of 0.995, the model demonstrated strong explanatory power. The P value in the BP test was 1, and the D–W test was 1.812.
Fig. 9.
Trend in inpatient subaverage cost for medical institution, from April 2020 to September 2023. The vertical dotted line shows the time when the DRG was implemented
Multiple testing of the nine independent models
Multiple comparisons using the Benjamini–Hochberg procedure for P values of trends in DRG implementation in nine independent models found that the number of discharges model, the percentage of discharged patients undergoing level III or IV model, the bed turnover rate model, the low-risk group mortality model, and the inpatient subaverage cost model all still showed significance after controlling for false discovery rate, i.e., the P value was still less than 0.05.
Discussion
This is the first study to use the ITSA model to evaluate the operational effects of DRG in Anhui Province. Meanwhile, the impact of DRG reform on hospital functional positioning, quality and safety, rational use of drug, service efficiency and medical cost is being systematically studied.
In our study, it was found that the ALOS showed a decreasing trend before the implementation of the DRG, while there was no significant trend in change after the implementation. This is consistent with the previous findings [15–18]. ALOS is primarily a reflection of the efficiency of the service. The lack of statistically significant changes in ALOS following the implementation of the DRG policy, even after controlling for the COVID pandemic and seasonal factors, may be attributed to several interrelated reasons. First, hospitals may require time to adapt to the new payment model, resulting in an initial period where ALOS remains unchanged [19]. Additionally, external factors, particularly the ongoing effects of COVID-19, could continue to influence ALOS despite adjustments in the analysis [16]. Furthermore, insufficient incentives may hinder meaningful changes in ALOS [20]. Patient characteristics, including case complexity and demographics, could also impact the overall trend. Overall, these factors suggest a multifaceted challenge in observing significant changes in ALOS post-policy implementation. Policymakers should consider providing training and resources to assist hospitals in optimizing their operational processes, ensuring that they can effectively manage patient flow and enhance service efficiency.
The number of discharges and outpatient visits is a good reflection of hospital capacity. The rise in inpatient visits before the implementation of the DRG policy suggests an increasing demand for healthcare resources, possibly due to factors such as changing disease patterns, an aging population or improved access to medical services. The significant drop in inpatient visits immediately after the policy implementation may reflect a short-term adjustment period, as hospitals recalibrated their operations to cope with the new payment model and reduce potential financial burdens [21]. However, the subsequent increase in inpatient visits post-implementation indicates that hospitals gradually adapted to the DRG system and began to optimize their management and clinical pathways, allowing them to attract more patients and effectively manage complex cases. Outpatient visits also trended upward before the implementation of the DRG policy but did not show significant changes at the moment of implementation or after, which may be related to the nature and structure of outpatient services. The DRG policy primarily affects the payment and management of inpatient cases, and the patterns of outpatient visits and cost structures may be less directly affected by the policy [22]. As a result, the stability of outpatient services and the increase in patient visits were not significantly disrupted during implementation.
The percentage of discharged patients undergoing level III or IV surgery is indicative of the skill level of the medical institution. Before the implementation of the DRG policy, the percentage of discharged patients undergoing level III or IV surgery was on the rise, indicating that hospitals were increasingly accepting and treating complex cases. This trend reflects improvements in hospital technology, equipment, and the quality of healthcare teams. Additionally, it may also be related to patient demand and market competition, as hospitals might undertake more high-difficulty surgeries to attract patients. However, following the implementation of the DRG policy, there was a decline in the percentage of discharged patients undergoing level III or IV surgery. Patient selection bias that may result from DRG policies. Hospitals may be more inclined to select patients who are at lower surgical risk to ensure that they can effectively control costs and improve economic efficiency under the DRG payment framework [23]. Furthermore, hospitals might aim to enhance patient discharge rates and reduce the length of stay, which could constrain the pursuit of complex surgeries.
The increase in bed turnover rate before the DRG policy implementation suggests that hospitals were actively optimizing their resource utilization. This could reflect a growing demand for inpatient services, driven by factors such as an increasing patient population, changes in disease patterns or improved access to healthcare. Hospitals may have been adapting to these pressures by enhancing their operational efficiencies to accommodate more patients within their existing bed capacity. The immediate decline in bed turnover rate at the moment of DRG implementation indicates that hospitals faced a significant adjustment period as they transitioned to the new payment model. This downturn may have been influenced by several factors, including initial confusion about billing practices, changes in admission and discharge protocols and the need for hospitals to reevaluate their clinical pathways under the new system. Additionally, the short-term financial concerns associated with the new DRG payment system may have led hospitals to adopt more conservative practices regarding patient admissions and discharges, thereby decreasing turnover rates. The subsequent recovery and increase in bed turnover rate post-implementation suggest that hospitals adapted to the DRG policy over time. As institutions became more familiar with the payment model, they likely refined their processes, improving efficiency in patient management and discharge planning. This adjustment may include better utilization of clinical pathways, enhancing case management practices and optimizing staff workflows, which can contribute to shorter lengths of stay and increased bed turnover [24]. Furthermore, the economic incentives inherent in the DRG system might motivate hospitals to maximize their inpatient capacity effectively, thereby leading to an increase in turnover rate. However one has to consider the changes in coding practices that may result from DRG implementation. Hospitals may tend to code cases more aggressively and will select patients who are relatively simple and can be discharged quickly to improve efficiency and reduce costs, which could lead to the exclusion of complex cases, which could affect the overall quality of care.
The inpatient essential drug utilization rate decreased significantly during the early implementation of DRG, but the differences were statistically insignificant at the time of the implementation of the DRG and after the reform. During the initial phase of the implementation of DRG, hospitals and healthcare can adjust treatment protocols and medication usage habits to align with the new healthcare payment system. This adaptation period can lead to noticeable adjustments and reductions in drug utilization rates, which are reflected as statistically significant differences [25]. Over time and with the stable implementation of DRG, hospitals and physicians can further optimize clinical processes and medication management strategies to maximize the utilization of healthcare resources and patient treatment outcomes [19]. These optimizations could lead to further adjustments in basic drug utilization rates, resulting in statistically non-significant changes.
The DRG reform has significant implications for the quality of patient care within the healthcare system. The mortality rate of low-risk patients is an important measure. The decline in the mortality rate of the low-risk group following the implementation of DRG suggests that hospitals may have become more adept at managing cases and prioritizing care strategies that enhance patient safety. This behavior aligns with hospitals’ increased focus on managing operational efficiency, avoiding unnecessary delays in treatment and improving overall care delivery. On the other hand, the DRG reform typically drives hospitals to standardize clinical pathways to enhance treatment protocols, ensuring that patients receive evidence-based care [26]. Additionally, with the economic incentives associated with DRG, hospitals may have placed greater emphasis on patient safety and health outcomes, thereby reducing mortality rates among these patients [20, 27]. Policymakers should prioritize initiatives that promote evidence-based care and patient safety, ensuring that hospitals are incentivized to maintain high-quality standards while managing costs.
The difference in the trend of outpatient subaverage cost during the DRG implementation period is not statistically significant, which is another confirmation that the main body of the DRG policy implementation is the inpatient population. However, the inpatient subaverage cost of hospitalization showed a downward, then upward, then downward trend before the DRG implementation, at the instant of implementation and after the implementation. This shift can be attributed to several factors associated with the adoption of DRG. Initially, hospitals and healthcare providers faced challenges in adapting to the new reimbursement framework, resulting in increased costs as they refined operational processes. However, over time, institutions have streamlined practices to comply with the requirements of the DRG, optimizing resource allocation and enhancing efficiency in patient care [28, 29]. The DRG system incentivizes cost control and data-driven decision-making, requiring hospitals to examine expenditures and implement targeted cost-saving measures. Additionally, policy adjustments and refined reimbursement mechanisms further encouraged cost containment and operational efficiency within healthcare delivery [22, 30]. This evolution highlights the effectiveness of DRG in fostering financial discipline and improving healthcare efficiency post-reform.
Conclusions
The findings indicate that the DRG reform has a systematic impact on various aspects of hospital functioning, including quality and safety, rational drug use, service efficiency and healthcare costs. Although there were no significant changes in the average length of stay post-implementation, the number of discharged inpatients and outpatient visits gradually increased after the policy was enacted, suggesting that hospitals adapted to the new payment model and optimized their management and clinical pathways. Additionally, the decline in the mortality rate among low-risk patients following DRG implementation indicates that hospitals have made progress in enhancing patient safety and care quality. However, the decrease in surgical complexity and the initial drop in bed turnover rate reflect the challenges and adjustments hospitals faced in adapting to the new payment model. Overall, the DRG reform demonstrates positive potential in improving healthcare service efficiency and controlling costs, but attention must also be paid to potential negative effects such as patient selection bias and changes in coding practices. Future research should continue to assess the long-term effects of the DRG policy and differences across various healthcare institutions to further optimize healthcare services.
Limitations
This study has several limitations, particularly the constraints associated with its single-centre design. Since the research was conducted in only one hospital in Anhui Province, the generalizability of the findings may be affected. The sample size and patient characteristics in a single-centre study may not represent a broader population or different types of hospitals. Therefore, while the study provides valuable insights into the implementation of DRG, caution should be exercised when extrapolating these findings. Future research should consider a multi-centre design to enhance the external validity of the results and evaluate the impact of the DRG policy across varying healthcare settings. Additionally, the study could not fully control for all potential confounding variables, such as patients’ socioeconomic status and regional healthcare resource disparities, which may also affect the interpretation of the results. Through a more comprehensive study design, future work could better illuminate the impact of DRG reforms on the healthcare system.
Acknowledgements
Not applicable.
Abbreviations
- DRG
Diagnosis-related groups
- ALOS
Average length of stay
- ITSA
Interrupted time-series analysis
- OLS
Ordinary least squares
- BP
Breusch–Pagan
- WLS
Weighted least squares
- D–W
Durbin–Watson
- FDR
False discovery rate
Author contributions
G.J.M. and E.C.Z.: conceptualization, methodology, data curation and writing – original draft preparation. X.L.F.: data curation. J.B.M. and S.J.K.: methodology and supervision. X.G.: data curation, writing original draft preparation and supervision. Z.L.: conceptualization and writing – review and editing. All authors read and approved the final manuscript.
Funding
This study was conducted without any external funding support.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study does not involve patient information. Data used are anonymized and aggregated, ensuring confidentiality. Ethics approval was obtained from the First Affiliated Hospital of Bengbu Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xuan Guo, Email: 2324387927@qq.com.
Zheng Lu, Email: luzhengdr@163.com.
References
- 1.Meng Z, Hui W, Cai Y, Liu J, Wu H. The effects of DRGs-based payment compared with cost-based payment on inpatient healthcare utilization: a systematic review and meta-analysis. Health Policy. 2020;124(4):359–67. [DOI] [PubMed] [Google Scholar]
- 2.Busse R, Geissler A, Aaviksoo A, Cots F, Häkkinen U, Kobel C, Mateus C, Or Z, O’Reilly J, Serdén L, et al. Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ (Clin Res Ed). 2013;346: f3197. [DOI] [PubMed] [Google Scholar]
- 3.Zhao C, Wang C, Shen C, Wang Q. Diagnosis-related group (DRG)-based case-mix funding system, a promising alternative for fee for service payment in China. Biosci Trends. 2018;12(2):109–15. [DOI] [PubMed] [Google Scholar]
- 4.Meng ZL, Zhu M, Cai YY, Cao XH, Wu HZ. Effect of a typical systemic hospital reform on inpatient expenditure for rural population: the Sanming model in China. BMC Health Serv Res. 2019;19:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zou K, Li HY, Zhou D, Liao ZJ. The effects of diagnosis-related groups payment on hospital healthcare in China: a systematic review. BMC Health Serv Res. 2020;20(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jian W, Lu M, Liu G, Chan KY, Poon AN. Beijing’s diagnosis-related group payment reform pilot: impact on quality of acute myocardial infarction care. Soc Sci Med. 1982;2019(243): 112590. [DOI] [PubMed] [Google Scholar]
- 7.Meng ZL, Ma YN, Song SH, Li Y, Wang D, Si YF, Sun RC, Zhang RC, Xue H, Jing LM, et al. Economic implications of Chinese diagnosis-related group-based payment systems for critically ill patients in ICUs. Crit Care Med. 2020;48(7):E565–73. [DOI] [PubMed] [Google Scholar]
- 8.Hu WY, Yeh CF, Shiao AS, Tu TY. Effects of diagnosis-related group payment on health-care provider behaviors: a consecutive three-period study. J Chin Med Assoc. 2015;78(11):678–85. [DOI] [PubMed] [Google Scholar]
- 9.Vogl M, Schildmann E, Leidl R, Hodiamont F, Kalies H, Maier BO, Schlemmer M, Roller S, Bausewein C. Redefining diagnosis-related groups (DRGs) for palliative care—a cross-sectional study in two German centres. BMC Palliat Care. 2018;17:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernal JL, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–93. [DOI] [PubMed] [Google Scholar]
- 11.Fretheim A, Zhang F, Ross-Degnan D, Oxman AD, Cheyne H, Foy R, Goodacre S, Herrin J, Kerse N, McKinlay RJ, et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. J Clin Epidemiol. 2015;68(3):324–33. [DOI] [PubMed] [Google Scholar]
- 12.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fransiska W, Nugroho S, Rachmawati R. A comparison of weighted least square and quantile regression for solving heteroscedasticity in simple linear regression. J Stat Data Sci. 2022;1(1):19–29. [Google Scholar]
- 14.Piradl S, Shadrokh A, Yarmohammadi M. A robust estimation method for the linear regression model parameters with correlated error terms and outliers. J Appl Stat. 2022;49(7):1663–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen YJ, Zhang XY, Tang X, Yan JQ, Qian MC, Ying XH. How do inpatients’ costs, length of stay, and quality of care vary across age groups after a new case-based payment reform in China? An interrupted time series analysis. BMC Health Serv Res. 2023;23(1):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu T, Chen C, Zhang X, Yang Q, Hu Y, Liu R, Zhang X, Dong Y. Differences in inpatient performance of public general hospitals following implementation of a points-counting payment based on diagnosis-related group: a robust multiple interrupted time series study in Wenzhou, China. BMJ Open. 2024;14(3): e073913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Messerle R, Schreyögg J. Country-level effects of diagnosis-related groups: evidence from Germany’s comprehensive reform of hospital payments. Eur J Health Econ. 2023;25(6):1013–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golinelli D, Sanmarchi F, Toscano F, Bucci A, Nante N. Analyzing the 20-year declining trend of hospital length-of-stay in European countries with different healthcare systems and reimbursement models. Int J Health Econ Manag. 2024;24(3):375–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang T, Lu B, Yan Z, Huang X, Lu W. Impacts of a new episode-based payment scheme on volume, expenditures, and efficiency in public hospitals: a quasi-experimental interrupted time-series study in Jinhua, China. Risk Manag Healthc Policy. 2022;15:1659–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tang X, Zhang X, Chen Y, Yan J, Qian M, Ying X. Variations in the impact of the new case-based payment reform on medical costs, length of stay, and quality across different hospitals in China: an interrupted time series analysis. BMC Health Serv Res. 2023;23(1):568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuan B, Quan L. Comprehensive evaluation of disease coding quality in gastroenterology and its impact on the diagnosis-related group system: a cross-sectional study. BMC Health Serv Res. 2023;23(1):1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu R, Shi J, Yang B, Jin C, Sun P, Wu L, Yu D, Xiong L, Wang Z. Charting a path forward: policy analysis of China’s evolved DRG-based hospital payment system. Int Health. 2017;9(5):317–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shi H, Cheng Z, Liu Z, Zhang Y, Zhang P. Does a new case-based payment system promote the construction of the ordered health delivery system? Evidence from a pilot city in China. Int J Equity Health. 2024;23(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma Y, Wang W. The impact of diagnosis related group payment on the performance of public hospitals. Am J Transl Res. 2021;13(6):6796–801. [PMC free article] [PubMed] [Google Scholar]
- 25.Zeng JQ. The pilot results of 47 148 cases of BJ-DRGs-based payment in China. Int J Health Plan Manag. 2019;34(4):1386–98. [DOI] [PubMed] [Google Scholar]
- 26.Kutz A, Gut L, Ebrahimi F, Wagner U, Schuetz P, Mueller B. Association of the Swiss diagnosis-related group reimbursement system with length of stay, mortality, and readmission rates in hospitalized adult patients. JAMA Netw Open. 2019;2(2): e188332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feng L, Tian Y, He M, Tang J, Peng Y, Dong C, Xu W, Wang T, He J. Impact of DRGs-based inpatient service management on the performance of regional inpatient services in Shanghai, China: an interrupted time series study, 2013–2019. BMC Health Serv Res. 2020;20(1):942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin K, Li Y, Yao Y, Xiong Y, Xiang L. The impact of an innovative payment method on medical expenditure, efficiency, and quality for inpatients with different types of medical insurance: evidence from a pilot city, China. Int J Equity Health. 2024;23(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ding Y, Yin J, Zheng C, Dixon S, Sun Q. The impacts of diagnosis-intervention packet payment on the providers’ behavior of inpatient care-evidence from a national pilot city in China. Front Public Health. 2023;11:1069131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu QJ, Li YL, Yin Q, Lu Y, Li LY, Xu DN, He M, Ma S, Yan W. Evaluation of inpatient services of tertiary comprehensive hospitals based on DRG payment. Front Public Health. 2024;12:1300765. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.