Abstract
Background
Peer-assisted learning (PAL) has been widely implemented for many years worldwide. To further enhance the understanding of available data, a scoping review of systematic reviews was conducted to synthesize existing evidence on the effectiveness of PAL in health professional education, aiming to provide more comprehensive outcomes.
Methods
Nine databases were systematically searched. The review process was guided by the five-stage scoping review framework proposed by Arksey and O’Malley. The JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses was used to assess the methodological quality. The results were narratively synthesized and reported following the Context, Input, Process, and Product (CIPP) evaluation model.
Results
24 systematic reviews (including nine meta-analyses) were included. The majority of these reviews were synthesized using narrative analysis. The application of PAL in health professional education was developed. In the context of evaluation, support for the theory, problem-based drivers, and the need to develop teaching and assessment skills for students were the main reasons for the development of PAL. Inputs for PAL predominantly centered on tutor recruitment and tutor training. Common activities within the PAL process encompassed peer teaching, peer tutoring, peer feedback, peer simulation, peer discussion, peer-led debriefing, peer supervision, and curriculum design. Outcomes of PAL were categorized across peer tutees, peer tutors, health professional educators, and challenges of PAL.
Conclusions
Despite certain challenges, the reciprocal benefits of PAL for peer tutees and tutors are evident. It is recommended that relevant institutions should consider incorporating PAL into the curriculum for health professional students. Future research should aim to develop a more rigorous framework to determine the short- and long-term effects, cost-effectiveness, and generalizability of PAL in health professional education.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06434-7.
Keywords: PAL, Peer-assisted learning, Health professional education, Scoping review
Introduction
The goal of health professional education is to prepare the healthcare workforce required to improve social health outcomes [1]. This encompasses a range of disciplines, including medical, nursing, dental, pharmacy, occupational therapy and other-related fields [2]. As healthcare practices evolve with emerging technologies and shift in healthcare models, future health professional students will also need to develop advanced skills and competencies, such as collaborative practice, communication, critical thinking, and problem solving skills [3]. Educators have explored various teaching models to enhance the core competencies of health professional students, with peer-assisted learning being an important approach [4–6].
Peer-assisted learning (PAL) has been described by Topping & Ehly as “People from similar social groupings who are not professional teachers helping each other to learn and learning themselves by teaching” [7]. There are several synonyms and forms of PAL in literature, which could be categorized by three dimensions: distance in stage of education, group size, and formality of the educational setting [8]. We used peer-assisted learning as an umbrella term encompassing a variety of teaching styles and activities used to support learning between tutors and tutees in this review [9].
PAL has been widely implemented among health professional students in medicine, nursing, dentistry, and pharmacy [10]. It is an effective learning method where both tutors and tutees gain knowledge and skills through sharing experiences and learning. Their interactions and support contribute to building friendships, increasing confidence, navigating clinical practice, and socialization [11]. PAL not only increases peer tutees’ self-efficacy, improves academic performance, and clinical skills, and reduces stress and anxiety [12–15], but also fosters intrinsic motivation to learn, develops leadership and improves exam outcomes among peer tutors [9, 16, 17].
Many systematic reviews and meta-analyses have evaluated the effectiveness of PAL in health professional education. However, existing systematic reviews on PAL effectiveness are broad and heterogeneous. For instance, Guraya [18]conducted a meta-analysis of the significant effectiveness of PAL for active learning. Y Zhang [19]focused on PAL’s impact on medical students’ clinical knowledge and skills. Zoraya [17] critically reviewed the impact of PAL programs on peer mentors, and Wong [20] explored nursing students’ perceptions and experiences with peer feedback. Independent systematic reviews may not yield comprehensive insights into the effectiveness and outcomes of PAL in health professional education. Therefore, there is a need to map and synthesize existing systematic reviews to extract as much information as possible from existing data about PAL implementation, identify research gaps and offer recommendations for health professional educators and researchers.
Educators widely recommend teaching skills training for health professional students [21], which is crucial for developing their teaching roles, as well as promoting them as better learners and more effective communicators [22]. PAL, as one of the main programs for developing teaching skills, is essential in the practice of global health professional education [23]. Moreover, researchers highlight that skills in peer teaching, assessment and feedback are documented internationally as required graduate attributes for health professional students [24].
Scientifically structured PAL implementation should be guided by high-quality evidence. A scoping review is useful when dealing with a large, complex, or heterogeneous body of literature. A scoping review of systematic reviews contributes to a comprehensive assessment of the existing literature, systematic integration of evidence and identification of areas requiring future research, a methodology that has gained widespread application in the healthcare field [25–27]. Therefore, following the PICO (Population, Intervention, Comparison, Outcome) framework, we conducted a scoping review of systematic reviews to summarize the evidence derived from systematic reviews systematically.
The review questions were:
• What are the characteristics of PAL in health professional education?
• What are the effects of PAL in health professional education?
Methods
Protocol registration
This review was performed following the five-stages approach of Arksey and O’Malley: (1) identifying the research question, (2) identifying relevant studies, (3) study selection, (4) charting the data, (5) collating, summarizing, and reporting the results [28]. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (number: CRD42023493171).
Search strategy
Nine databases were systematically searched up to November, 2023, including PubMed, Embase, CINAHL, PsycINFO, Web of Science, Cochrane Library, Scopus, Education Resources Information Centre (ERIC), and Wiley Online Library. Search terms included peer teach*, peer educ*, peer led, peer mentor, peer instruction, peer tutor, peer collaboration, student run, student-led, peer-assisted teach*, peer-assisted learn*, peer group teach*, near peer teach*, near peer tutor*, peer tutor*, peer-to-peer tutor*, peer-to-peer teach*, peer assisted learning, PAL, review, systematic review. Studies were sought in English, with an example of the search strings in PubMed provided in Supplementary File 1.
Inclusion and exclusion criteria
Reviews that met the following criteria were included: (1) Population: participants were health professional students, including medical, nursing, dental, pharmacy, and public health, etc.; (2) Intervention: the topic was related to the use of PAL in health professional students; (3) Comparators: no specific comparators are required; (4) Outcomes: the outcomes were the effectiveness of PAL, including the knowledge, academic performance, satisfaction, and participant experience; (5) Context: PAL could occur in academic or clinical settings; (6) Study design: the literature type was systematic reviews of all study designs, with or without meta-analysis; (7) Written in English.
The studies were excluded if they were: (1) systematic review protocols; (2) duplicated publications; (3) dissertations or conference abstracts; (4) not available.
Selection of reviews
All articles retrieved were imported into EndNote software and checked for duplication. Two reviewers (HBF, ZYL) then independently reviewed the titles and abstracts of the remaining studies based on eligibility criteria. The full text of potential publications was retrieved and assessed by two reviewers. Any differences were resolved through discussion or a third reviewer (ZJW).
Quality assessment
The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Systematic Reviews and Research Syntheses was used to appraise the methodological quality [29]. The tool comprises 11 questions designed to assess the risk of bias in systematic reviews and meta-analyses. Two reviewers (HBF, ZJW) independently evaluated the included reviews. Group discussions or consultation with third partners were conducted in case of disagreement during evaluation.
Data extraction
The following data were extracted from the included reviews: first author and year of publication, type of review, aim of the review, number and type of primary studies included in the reviews, participant details, synthesis method, quality assessment tools, and framework.
Data synthesis
A narrative synthesis was conducted to summarize the results. The primary outcome was reported according to the Context, Input, Process, and Product (CIPP) evaluation model [30], developed for decision-making aimed at improving education and commonly utilized in the field of health professional education. The Context component evaluates the conditions leading to PAL implementation. The Input component assesses human resources and training. Process evaluation focuses on the implementation process of PAL, while the Product component assesses the positive and negative effects of PAL [30, 31]. The final summary of evidence tables were presented according to JBI visual stop-light indicator, where green indicates beneficial, amber means that there is no difference in the investigated comparison, and red represents detrimental or less effective [29].
Results
Search results
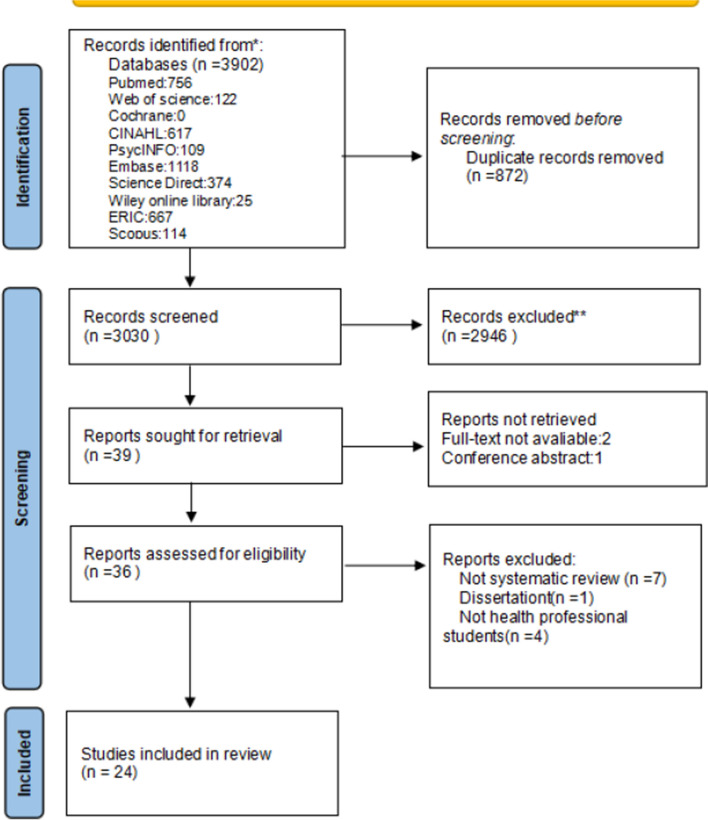
This review identified a total of 3902 articles. After removing duplicates, we screened titles and abstracts of 3030 articles. Among these articles we conducted two rounds of review: the first was based on the title and abstract, and 39 were sought for retrieval. The second aimed to remove articles that did not meet the inclusion criteria by reading the full text. Ultimately, 24 systematic reviews were included in the scoping review. Figure 1 presents the flowchart of the screening process according to PRISMA guidelines. Supplementary file 2 provides the references of excluded papers and the reasons for their exclusion.
Fig. 1.
PRISMA identification and screening process
Characteristics of selected systematic reviews
The main characteristics of the included systematic reviews (SRs) are summarized in Table 1. The 24 included SRs were conducted across twelve countries, namely Australia (n = 6), the UK (n = 5), Singapore (n = 4), the USA (n = 1), Chile (n = 1), India (n = 1), Indonesia (n = 1), Malaysia (n = 1), New Zealand (n = 1), Norway (n = 1), the Republic of Korea (n = 1), and the United Arab Emirates (n = 1). In terms of participants, medical, nursing, dentistry, mental health, physician assistant, and pathology students were included. Meta-analysis was used in nine SRs to calculate the combined effects of PAL in health professional students. 18 SRs summarized the effectiveness of PAL through narrative synthesis, with three using thematic analysis, one meta-synthesis, and one meta-aggregation. The systematic reviews included 423 primary studies published between 1975 and 2021.
Table 1.
Description of included systematic reviews (n = 24)
| First Author (Year) | Country | Type of review | Aim of the review | Range of publication years of primary studies | Number and types of primary studies | Participant details | Quality assessment tools | Synthesis method |
|---|---|---|---|---|---|---|---|---|
| Akinla (2018) [32] | UK | Systematic review | To describe the outcomes of near-peer mentoring schemes for first-year medical students in the transition phase | 2006–2017 |
5 studies Study type is not mentioned |
First-year students as the primary mentees and the mentors must be near-peers | CCAT | Narrative synthesis |
| Brierley (2022) [14] | UK | Systematic review-Meta analysis | To establish the effectiveness of PAL and identify the specific medical education setting | 1997–2021 | 27 RCTs |
2656 students 225 student teachers |
Cochrane Risk of Bias Tool | Meta-analysis |
| Burgess (2014) [33] | Australia | Systematic review | To establish why and how PAL has been implemented | 2002–2012 |
19 studies Study type is not mentioned |
Not mentioned | Not mentioned | Narrative Synthesis according to six review questions |
| Carey (2018) [34] | UK |
Qualitative systematic review |
To explore undergraduate nursing students’ experiences of PAL within the clinical practice environment | 2004–2015 |
6 qualitative 2 mixed-method |
Undergraduate student nurses in acute healthcare settings | JBI Critical Appraisal Checklist | Meta-synthesis |
| Choi (2020) [35] | Republic of Korea | Systematic review-Meta analysis |
To determine the effectiveness of peer learning in nursing students using Meta-Analysis |
1993–2018 | 10 controlled studies |
320 Experimental 316 Control |
RoBANS | Meta-analysis |
| Coli˜nir (2021) [36] | Chile | Systematic review | To analyse the characteristics and impact of PAL programmes implemented in undergraduate health education | 2010–2019 |
47 studies Study type is not mentioned |
Not mentioned | Not mentioned | Narrative synthesis |
| Dalwood (2019) [37] | Australia | Systematic review |
To determine the impact of peer simulation learning outcomes in entry-level health care professional students |
1997–2018 |
10 quantitative 1 qualitative 1 mixed-method |
1385 particpants | MERSQI CASP | Meta-analysis; Narrative synthesis |
| Gazula (2017) [38] | Australia | Systematic review | To examine the role of RPT in health professions education | 2005–2014 |
2 qualitative 1 quantitative 5 mixed methods |
Not mentioned | CASP | Narrative synthesis |
| Guraya (2020) [18] | United Arab Emirates | Systematic review-Meta analysis | To examine the effectiveness of PAL in improving students’ learning | 2008–2017 |
1 mixed-method 10 RCT |
PAL 446 Control 431 |
Not mentioned | Meta-analysis |
| Irvine (2016) [39] | Australia | Systematic review |
To summarize learning outcomes in undergraduate health professional NPT programs |
1997–2015 |
17 experimental 9 observational |
Not mentioned | JBI Critical Appraisal Checklist | Narrative synthesis |
| Khapre (2021) [40] | India | Systematic review-Meta analysis |
To investigate and compare the effectiveness of near-peer tutoring and faculty/expert teaching in health science undergraduates |
2002–2019 |
16 studies Study type is not mentioned |
Not mentioned | MERSQI | Meta-analysis Narrative synthesis |
| Lerchenfeldt (2019) [41] | USA | Systematic review | To determine the role and impact of peer feedback | 1999–2016 |
15 quantitative 3 qualitative 13 mixed-method |
2832 participants |
The Gradings of Strength of Findings of the Paper by Colthart |
Narrative synthesis |
|
Lim (2022) [42] |
Singapore | Systematic review |
To synthesize the best evidence exploring the impacts of peer mentoring programs on nursing students. |
2015–2021 |
31studies Study type is not mentioned |
Not mentioned |
JBI Critical Appraisal Checklist MMAT |
Meta-analysis Meta-aggregation |
|
Nelwati (2018) [43] |
Malaysia | Qualitative systematic review | To synthesize qualitative evidence of peer learning experiences | 2007–2017 | 6 qualitative | Undergraduate nursing students | CASP | Thematic analysis |
|
Rees (2015) [44] |
UK | Systematic review-Meta analysis | To describe the knowledge and skills outcomes for undergraduate medical students taught through peer teaching compared to faculty | 2004–2013 | 10 controlled studies | 1300 participants | MERSQI | Meta-analysis |
| Secomb (2007) [45] | Australia | Systematic review | To make clear the positive and negative aspects of peer teaching | 1987–2003 |
12 studies Study type is not mentioned |
Not mentioned | A specifically adapted appraisal tool | Narrative synthesis |
|
Tai (2016) [46] |
Australia | Narrative systematic review | To synthesize the effects of same-level PAL in undergraduate clinical medical education | 1975–2014 |
43 studies Study type is not mentioned |
Not mentioned | QA |
Qualitative thematic analysis |
| Tanveer (2023) [47] | Norway | Systematic review | To focus on the learning outputs for medical undergraduates acting as student-teachers | 2012–2022 |
30 mixed-method 8 qualitative 7 quantitative |
Student-teachers: 3–481 Student-learners: 5–1053 |
MERSQI | Narrative synthesis |
|
Wong (2022) [20] |
Singapore | Qualitative systematic review | To explore perceptions and experiences of nursing students who have used peer feedback | 1987–2022 |
6 qualitative 8 mixed-method |
728 undergraduates and 251 graduate nursing students | CASP | Thematic analysis |
|
Y Zhang (2022) [10] |
UK | Systematic review-Meta analysis | To analyse the efficacy of PAL on medical students’ learning of clinical knowledge and skills | 2000–2019 |
13 studies Study type is not mentioned |
2003 medical students | Cochrane Collaboration’s tool | Meta-analysis |
|
Yu (2011) [48] |
New Zealand | Systematic review | To summarize and critically appraise evidence presented on peer-teaching effectiveness and its impact on objective learning outcomes of medical students. | 1994–2010 |
19 studies Study type is not mentioned |
Not mentioned | Not mentioned | Narrative synthesis |
| Zhang (2022a)[19] | Singapore | Systematic review-Meta analysis | To determine the overall effect of peer teaching in enhancing students’ theoretical knowledge and practical skills | 1993–2021 | 44 RCTs | 4164 tutees, including medical, nursing, dentistry students. | ROB- 2 | Meta-analysis |
| Zhang (2022b) [49] | Singapore | Systematic review | To focus on the effectiveness of PVF and identify possible effective elements contributing to its best practice. | 1996–2021 |
8 RCTs 14 quasi-experimental |
1687 healthcare students, including nursing, dental, mental, physician assistant, pathology. | MERSQI | Narrative synthesis |
| Zoraya (2020) [17] | Indonesia | Systematic review | To analyse the impact of PAL programs on peer mentors | 2014–2017 |
5 studies Study type is not mentioned |
Not mentioned | JBI critical appraisal tools | Narrative synthesis |
BEME: Best Evidence Medical Education
CASP: The Critical Skills Appraisal Programme tool
CCAT: Crowe Critical Appraisal Tool
ENTREQ: Enhancing Transparency in Reporting the Synthesis of Qualitative Research
MERSQI: Medical Education Research Study Quality Instrument
MMAT: The Mixed Methods Appraisal Tool
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
QA: Quality Appraisal tool
RoBANS: Risk of Bias Assessment Tool for Nonrandomized Studies
Regarding methodological quality, the included reviews ranged from medium to high quality (see Table 2) according to the JBI quality appraisal tool (range 5–11). All reviews clearly stated the research question and had appropriate inclusion-exclusion. However, most reviews lacked methods to minimize errors in data extraction (criterion 7), assessment of publication bias (criterion 9), and recommendations for policy and/or practice supported by the reported data (criterion 10).
Table 2.
The quality assessment of included systematic reviews (n = 24)
| First author (year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Total | % of 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Akinla (2018) [32] | Y | Y | Y | Y | Y | U | U | Y | NA | N | Y | 7 | 63.64 |
| Brierley (2022) [14] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 | 100 |
| Burgess (2014) [33] | Y | Y | Y | Y | U | U | NA | Y | NA | N | Y | 6 | 54.55 |
| Carey (2018) [34] | Y | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 10 | 90.91 |
| Choi (2020) [35] | Y | Y | Y | Y | Y | N | Y | Y | Y | N | Y | 9 | 81.82 |
| Coli˜nir (2021) [36] | Y | Y | Y | N | Y | Y | U | Y | NA | N | Y | 7 | 63.64 |
| Dalwood (2019) [37] | Y | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 10 | 90.91 |
| Gazula (2017) [38] | Y | Y | Y | Y | Y | Y | U | U | NA | Y | Y | 8 | 72.73 |
| Guraya (2020) [18] | Y | Y | Y | Y | U | Y | Y | U | N | N | Y | 7 | 63.64 |
| Irvine (2016) [39] | Y | Y | Y | Y | Y | Y | U | Y | NA | N | Y | 8 | 72.73 |
| Khapre (2021) [40] | Y | Y | Y | Y | Y | U | Y | Y | NA | Y | Y | 9 | 81.82 |
| Lerchenfeldt (2019) [41] | Y | Y | Y | Y | Y | Y | Y | Y | NA | N | Y | 9 | 81.82 |
| Lim (2022) [42] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 | 100 |
| Nelwati (2018) [43] | Y | Y | Y | Y | Y | N | U | Y | NA | Y | N | 7 | 63.64 |
| Rees (2015) [44] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 | 100 |
| Secomb (2006) [45] | Y | Y | Y | Y | Y | U | U | Y | NA | Y | Y | 8 | 72.73 |
| Tai (2016) [46] | Y | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 10 | 90.91 |
| Tanveer (2023) [47] | Y | Y | Y | Y | Y | U | U | Y | NA | Y | Y | 8 | 72.73 |
| Wong (2022) [20] | Y | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 10 | 90.91 |
| Y Zhang(2022) [10] | Y | Y | Y | Y | Y | Y | U | Y | NA | N | Y | 8 | 72.73 |
| Yu (2011) [48] | Y | Y | Y | Y | N | Y | Y | Y | NA | Y | N | 8 | 72.73 |
| Zhang (2022a) [19] | Y | Y | Y | Y | Y | Y | U | Y | Y | N | Y | 9 | 81.82 |
| Zhang (2022b) [49] | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | 10 | 90.91 |
| Zoraya (2020) [17] | Y | Y | N | Y | Y | U | U | Y | NA | N | N | 5 | 45.45 |
Q1 Is the review question clearly and explicitly stated?
Q2 Were the inclusion criteria appropriate for the review question?
Q3 Was the search strategy appropriate?
Q4 Were the sources and resources used to search for studies adequate?
Q5 Were the criteria for appraising studies appropriate?
Q6 Was critical appraisal conducted by two or more reviewers independently?
Q7. Were there methods to minimize errors in data extraction?
Q8 Were the methods used to combine studies appropriate?
Q9 Was the likelihood of publication bias assessed?
Q10 Were recommendations for policy and/or practice supported by the reported data?
Q11 Were the specific directives for new research appropriate?
U: Unclear
NA: Not Applicable
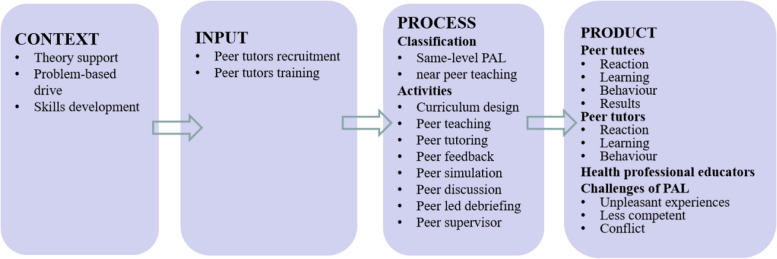
Evaluation of PAL in health professional education
The evaluation of PAL in health professional education was synthesized under the Context, Input, Process, and Product respectively. The PAL implementation context included three aspects.The Input components focused on tutors recruitment and tutors training. The Process evaluation encompassed PAL categories and PAL activities. Outcomes of PAL were summarized from the impact on peer tutors, peer tutees, and health professional educators, as well as the challenges of PAL. (See Fig. 2)
Fig. 2.
Application of PAL in health professional education
Context evaluation of PAL
Only two reviews evaluated the context of PAL implementation [33, 48]. The development of PAL were driven by three main reasons: literature support for the theory, problem-based drivers such as staff resource issues, and the need to enhance the teaching and assessment skills of students.
Input evaluation of PAL
PAL inputs focused on tutors recruitment and tutors training. The selection process for peer tutors considered their experience, motivation, academic level, and leadership qualities [33, 36, 39, 48]. Mentor training included basic principles of teaching, specific content, and practical skills [14, 19, 33, 36, 39, 41, 48, 49].
Process evaluation of PAL
The common features of PAL, such as PAL categories, activities, group size, and frequency, are detailed in Table 3.
Table 3.
Summary of PAL implementation strategies
| Item | Description | Author/year |
|---|---|---|
| PAL categories | Same-level PAL | Tai (2016); [46], Yu (2011); [48], Burgess (2014); [33], Y Zhang (2022); [10], Secomb (2006); [45], Coli˜nir (2021); [36], Zhang (2022b); [49], Zhang (2022a); [19], Choi (2020); [35], Lerchenfeldt (2019); [41], Gazula (2017) [38], |
| Near peer teaching | Yu (2011); [48], Burgess (2014); [33], Zhang (2022a); [19], Secomb (2006); [45], Akinla (2018); [32] Coli˜nir (2021); [36], Zoraya (2020); [17], Brierley (2022); [14] Zhang (2022b); [49], Choi (2020); [35], Khapre (2021); [40], Irvine (2016); [39], Lerchenfeldt (2019); [41], Tanveer (2023); [47], Y Zhang (2022) [10] | |
| PAL activities | Teacher training | Yu (2011); [48], Burgess (2014); [33], Brierley (2022); [14] Zhang (2022b); [49], Coli˜nir (2021); [36], Lerchenfeldt (2019); [41], Irvine (2016); [39], Zhang (2022a) [19] |
| Peer teaching | Tai (2016); [46], Yu (2011); [48], Burgess (2014); [33], Zhang (2022b); [49], Brierley (2022); [14] Rees (2015); [44], Zhang (2022a); [19], Khapre (2021); [40], Choi (2020); [35] Coli˜nir (2021); [36], Y Zhang (2022) [10] | |
| Peer tutoring (mentoring) | Brierley (2022); [14] Choi (2020); [35], Coli˜nir (2021); [36], Akinla (2018); [32] Zoraya (2020); [17], Lim (2022); [42], Yu (2011) [48] | |
| Peer feedback (assessment) | Lerchenfeldt (2019); [41], Burgess (2014); [33], Tai (2016); [46], Zhang (2022b); [49], Zhang (2022a); [19], Wong (2022); [20], Y Zhang (2022) [10] | |
| Peer simulation | Tai (2016); [46], Zhang (2022a); [19], Coli˜nir (2021); [36], Dalwood (2019); [37], Choi (2020); [35], Khapre (2021); [40], Y Zhang (2022) [10] | |
| Peer discussion | Tai (2016); [46], Yu (2011); [48], Zhang (2022a); [19], Khapre (2021); [40], Coli˜nir (2021); [35, ]Y Zhang (2022) [10] | |
| Peer led debriefing | Choi (2020) [35] | |
| Peer supervisor | Choi (2020) Zhang (2022a) [19, 35] | |
| Curriculum design | Yu (2011) [48] | |
| PAL duration per session | 30 min–4 h | Tanveer (2023) [47] |
| 1 h-half-day | Yu (2011) [48] | |
| 15–45 min | Zhang (2022b) [49] | |
| 33 min–6 h | Zhang (2022a) [19] | |
| PAL frequency (sessions) | 1–26 | Tanveer (2023) [47] |
| 1–14 | Yu (2011) [48] | |
| PAL group (students per group) | 4–25 | Tanveer (2023) [47] |
| 4–20 | Yu (2011) [48] | |
| 1–14 | Zhang (2022a) [19] | |
| 1–19 | Akinla (2018) [32] |
Implementation of PAL could be categorized as same-level PAL [10, 19, 33, 35, 36, 38, 41, 45, 46, 48] and near-peer teaching [10, 14, 17, 19, 32, 33, 35, 36, 39–41, 45, 47, 48].
Twenty reviews (83.33%) reflected a wide range of PAL implementation strategies, including curriculum design [48], peer teaching [10, 14, 19, 33, 35, 36, 40, 44, 46, 48], peer tutoring (mentoring) [14, 17, 32, 35, 36, 42, 48], peer feedback [19, 20, 33, 41, 46, 49], peer simulation [19, 35–37, 40, 46], peer discussion [19, 36, 40, 46, 48], peer-led debriefing [35] and peer supervisor [10, 35].
Four reviews [10, 32, 47, 48] reported the group size of PAL, ranging from 1 to 25 students per group. Four reviews [10, 47–49] described the duration of each session of PAL, which ranged from 15 min to 6 h. And two reviews [47, 48] reviewed the frequency of PAL as 1 to 26 sessions.
Product evaluation of PAL
Outcomes of PAL were reported under the following headings based on peer tutees, peer tutors, health professional educators, and challenges of PAL. A summary of evidence was shown in Supplementary file 3.
Outcomes of peer tutees
Twenty-one reviews (87.5%) evaluated the effect of PAL on tutees. Findings were categorized into reaction, learning, and behavior according to Kirkpatrick’s evaluation model.
Regarding their reactions to PAL, participants perceived a more supportive and low-threat learning environment [36, 40, 46], and gained support when connecting with peers [34, 43, 46], which made them feel more comfortable, relaxed, engaged, and prepared for future evaluation [20, 36, 40, 42]. They believed that PAL was a more effective and valuable method [36, 37]. However, mixed effects were found on their satisfaction and team dynamics [40, 41, 45, 49].
The learning outcomes were reported in 20 SRs and were divided into four subthemes: knowledge, attitude, skills, and mental health. Peer tutees reported positive outcomes such as enhanced knowledge, higher scores, and a deeper understanding of the content [14, 18, 34–36, 38, 43, 45]. Higher self-efficacy was found among peer tutees. They increased their motivation to participate, gained confidence, and reported greater learning opportunities, as well as a continued understanding of their development [34, 36, 37, 43, 45, 46, 49]. What’s more, they improved their skills after the PAL program, including communication, empathy, procedural, technical, problem-solving, teaching, clinical, teamwork, leadership, reflection, judgment, and other skills [10, 32, 34, 37, 38, 41, 43, 45, 46]. In the field of mental health, PAL was beneficial in reducing stress and anxiety [32, 34, 36, 42, 45]. However, ambiguous effects were shown on some learning outcomes, such as learning scores, learning opportunities, skill scores, and stress levels [10, 19, 36, 37, 39–42, 44–46, 48, 49].
Two SRs reported positive behavior changes. They showed increased collegial behavior among nursing students [45] and a tendency to use active coping mechanisms after the program [42].
Outcomes of peer tutors
Nine reviews (37.5%) evaluated the effects of PAL on peer tutors. The outcomes were categorized into reaction, learning, and behavior based on Kirkpatrick’s evaluation model.
Peer tutors involved in PAL perceived a more relaxed environment and experienced enjoyment during the process [20, 33].
For the learning outcomes, peer tutors gained a more profound understanding of knowledge, encompassing both subject-specific and pedagogical knowledge [20, 33, 36, 40, 47]. They developed self-confidence and had greater courage, motivation, and autonomy to teach and learn [20, 33, 36, 40, 42, 47]. Peer tutors also improved various skills after the PAL program, such as teaching skills, leadership qualities, communication ability, empathy, ability to admit uncertainty, time management, and teamwork capacity [17, 20, 32, 33, 36, 40, 42, 47]. Conflicting results were presented in two reviews about their learning outcomes and scores [33, 48]. For example, two original studies in the Burgess’ review evaluated peer tutors’ learning scores. The findings of one study showed that peer tutors achieved significantly higher scores, however, the results of the other study showed no benefit to tutors knowledge acquisition.
Finally, positive behavioral changes were reported in one review [32].
Outcomes of health professional educators
Only a few reviews reported the effect of PAL on clinician educators. Tai [46] observed that PAL did not reduce the time of clinical educators but did result in more satisfying educational interaction and contributed to the development of educational skills, such as giving feedback.
Challenges of PAL
Ten reviews (41.67%) assessed the issues and adverse effects associated with PAL, including unpleasant experiences, inadequate competence of peer tutors, and even conflicts.
PAL was perceived as a “significant change” in the learning experience, initially inducing anxiety among students. Some students were unclear about the purpose of PAL and felt that the change was imposed without adequate preparation, leading to anxiety. The lack of training in the peer education program also raised concerns among participants. Additionally, students experienced unpleasant emotions such as stress, fear, and embarrassment when criticized or judged by their friends [20, 33, 34, 38, 40, 41, 49].
The competence of peer tutors was questioned due to the lack of necessary professional knowledge, skills, experience, and authority [38, 40, 46–49]. It was noted that peer feedback and assessment were often inconsistent with the judgments of other experts on performance [20, 33, 46]. In addition, students may refuse to participate in the evaluation or provide overly positive feedback due to fear of facing criticism and a desire to avoid low scores [20, 38, 46].
Moreover, Secomb [45] demonstrated that conflicts arose when students were incompatible due to differences in their knowledge levels, educational backgrounds, or incompatible personalities.
Discussion
This scoping review aimed to map the literature and identify the characteristics, outcomes and effectiveness of PAL in health professional education. To the best of our knowledge, this was the first review specifically aiming to evaluate the implementation of PAL that can be updated and iterated strategically. Findings will help bridge the gap between research and educational practice and guide health professions teachers’ strategies regarding the implementation of PAL.
Main outcomes
There are various activities of PAL in the literature. The findings suggest that PAL can occur in any process of health professional education, including curriculum design, teaching, feedback, discussion, simulation, and supervision. For example, a German study examined the effects of an anatomy revision course on junior students that was designed and implemented by four fourth-year medical students [50]. Kim suggested that peer-led debriefing was an effective strategy for improving undergraduate nursing students’ knowledge and self-confidence [51]. In peer-led groups, students asked debriefing questions while other students shared their experiences and perceptions of each other’s performance using a structured questionnaire. This review showed that peer teaching and peer mentoring were the most common activities in the existing studies, which was consistent with a previous study [16]. Therefore, we encourage the incorporation of peer-led activities in curriculum design, teaching, feedback, and discussions, which may benefit health professional students and address the global trend of faculty resources shortage [37, 52].
Our review also integrated outcomes of PAL in health professional education, including the effects on peer tutees, peer tutors and health professional educators.
Overall, the outcomes for peer tutees were reported to be mostly positive. They recognized PAL as an effective learning method that improved their learning outcomes. A more comfortable and safer learning environment was achieved through peer support and interaction, which increased their self-confidence and satisfaction. These findings confirmed the benefits of PAL for tutees, which can be attributed to the following two key reasons. First, cognitive congruence is widely recognized as a theoretical cornerstone of the efficacy of PAL [53]. Cognitive congruence exists between tutors and tutees who share a common knowledge base due to similar learning context and experiences. Peer tutors may be better positioned to understand the learner’s learning experiences and difficulties. The cognitive and behavioral distance between them is known as the Zone of Proximal Development according to Vygotsky’s Zone of Proximal Development and scaffolding theory [54]. They can form interactive scaffolds with lectures, simulations, interactions, collaborations, discussions, and feedback to facilitate the transformation from the actual development level to a potential level of development. Second, peer tutors and peer tutees share informal communication styles in similar social roles. Peer tutors have a greater likelihood of empathizing with learners’ thoughts and needs. They form learning communities that are beneficial in creating a relaxing, safe, equal, comfortable, and emotionally supportive learning environment in which students are motivated to learn and facilitate their skills development [55].
However, compared with faculty teaching, the findings demonstrated that PAL did not show significant differences in learning outcomes in some studies. On the one hand, this at least suggested that PAL was as effective as traditional faculty teaching. On the other hand, this also reflected some potential problems in PAL implementation. First, peer tutors may lack specialized knowledge and competence [10, 49], which may be related to their insufficient pre-training and a lack of clarity and consensus on PAL. Second, theoretical and clinical teaching in the health professional field requires a high level of expertise, and students need a tutor to explain the connections between concepts, which can be challenging for peer tutors. For example, tutors must have enough knowledge and experience to teach resuscitation skills and make accurate judgments on their cognitive processes [10].
Our review also synthesized the effects of PAL on peer tutors, revealing positive experiences, deeper understanding of knowledge, and skills development. The process of teaching involves preparation, explanation, and feedback [32]. During peer mentoring, peer tutors are required to organize and summarize pertinent knowledge and skills beforehand. Their comprehension is enhanced as they transfer their knowledge to others while interacting with students. The Learning Pyramid Theory [56], which states that 90% of content can be retained by teaching others, also provides a rationale for the benefits of peer tutors. When interacting with the tutees, tutors not only develop teaching skills but also enhance their leadership, communication skills, and empathy, which are essential competencies for healthcare professionals. It is noteworthy that most of the evidence is derived from qualitative data, which suggests the necessity of confirmation in future quantitative studies.
Our review identified some common challenges in PAL programs, such as unpleasant experiences, inadequate competence of peer tutors, and conflicts. We proposed the following suggestions that need attention in future educational practice. First, prepared and explicit training is an important way to enhance the teaching ability of tutors and prevent negative experiences for participants [38, 47]. Peer tutors participating in peer teacher training could learn teaching skills and professional knowledge, which help them to deal with difficulties and problems encountered in teaching, assessment, communication, and feedback. This is an important strategy to avoid the negative effects of PAL [16, 57]. However, in the majority of reviews, training sessions as part of the PAL training program were missing or not specified. A survey revealed that although 67% of health professional students reported having engaged in a peer tutor role, only 32% of the respondents stated that they had received training [58]. In addition, the dominant training approaches were uni-disciplinary, faculty-led, non-mandated programs [24]. Therefore, it is necessary for researchers and health professional educators to train peer tutors on the objectives of the peer mentoring program. The components of the training should consider the basic principles of teaching, the expected qualities of teachers, how to interact and provide constructive feedback, the specific content knowledge or skills required, and issues that may arise during the PAL [34, 38]. The training method can include pre-training readings, formal training tasks, content knowledge, and evaluation of teaching ability [6]. This will help in identifying the best design features, facilitating better replication, communication and comparison among academics, and identifying best practices. Second, in response to biased grading due to the potential for punishment and negative emotional reactions, it is necessary to create a positive environment that could remove students’ perceptions of threat and promote freer participation, as well as to consider the matching of personalities, learning styles, and teaching styles among peers [34, 38]. Third, it is recommended that esoteric and complex content should be taught by specialized instructors and specialists to promote learning and understanding and to avoid an uncomfortable learning experience for both the tutees and tutors. In addition, it was suggested that the introduction of mentors and senior supervisors into the PAL program to provide a safety net for anxious mentors to address difficult issues could be valuable [20, 44].
Strengths and limitations
The strength of this review is twofold. First, it may offer a more comprehensive overview of the effects of PAL because we incorporated data from all types of systematic reviews. Second, the application of PAL in health professional education was developed based on the CIPP evaluation model. We summarized the common activities and evaluation outcomes of PAL, which could serve as a guide for health professional educators and researchers. In addition, we identified some issues associated with students and provided solutions that could enhance PAL practices.
It must be recognized that this review has some limitations. First, there are still wide differences in PAL programs, and there is a lack of descriptions in the included reviews, such as the applied curriculum, details clarifying PAL group, tutor-tutee ratio, frequency, and duration of the interventions. Therefore, we were unable to identify the key design features of PAL and provide a conclusive recommendation for its implementation. Second, this scoping review only included systematic reviews published in English that have been peer-reviewed, which may lead to the possibility of bias.
Conclusions
Health professional education is an ever-evolving field that aims to discover innovative and effective pedagogical methods to help students achieve the necessary competencies. This scoping review integrated the results from 24 SRs to explore the effectiveness of PAL. Despite the existing challenges, the reciprocal benefits of PAL are apparent in the academic performance of student tutees and tutors. Therefore, we suggest PAL as a complementary teaching method to supplement traditional faculty-led activities. Institutions should consider incorporating PAL into the curriculum for health professional students. In addition, we recommend further research to utilize a rigorous framework to determine the short and long-term effects, cost-effectiveness, and generalizability of PAL in health professional education.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
Hanbo Feng: Conceptualization, Methodology, Writing- Original draft, Funding Acquisition, VisualizationZiyi Luo: Resources, SoftwareZijing Wu: Validation, Writing- Reviewing and Editing, Funding AcquisitionXiaohan Li : Supervision, Writing- Reviewing and Editing, Project administration.
Funding
This work was funded by the Teaching Reform Project of China Medical University [grant numbers: YDJG20240063], the Teaching Reform Project of China Medical University[grant numbers: YDJG20230144] and the Project of School of Nursing, China Medical University[grant numbers:2023HL-06]. The funding took no role in the design of study, data interpretation and draft-writing.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zijing Wu, Email: zjwu@cmu.edu.cn.
Xiaohan Li, Email: xhli@cmu.edu.cn.
References
- 1.Hays RB, Ramani S, Hassell A. Healthcare systems and the sciences of health professional education. Adv Health Sci Educ. 2020;25(5):1149–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leadbeatter D, Nanayakkara S, Zhou X, Gao J. Employability in health professional education: a scoping review. BMC Med Educ. 2023;23(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balasooriya C, Lyons K, Tran M, Pather N, Chur-Hansen A, Steketee C. Learning, teaching and assessment in health professional education and scholarship in the next 50 years. FOCUS ON HEALTH PROFESSIONAL EDUCATION; 2024. p. 25. [Google Scholar]
- 4.Stockert B, Silberman N, Rucker J, Bradford J, Gorman SL, Greenwood KC, Macauley K, Nordon-Craft A, Quiben M. Simulation-Based Education in Physical Therapist Professional Education: a scoping review. Phys Ther. 2022;102:1–12. [DOI] [PubMed] [Google Scholar]
- 5.Naing C, Whittaker MA, Aung HH, Chellappan DK, Riegelman A. The effects of flipped classrooms to improve learning outcomes in undergraduate health professional education: a systematic review. Campbell Syst Rev. 2023;19(3):e1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross MT, Cameron HS. Peer assisted learning: a planning and implementation framework: AMEE Guide 30. Med Teach. 2007;29(6):527–45. [DOI] [PubMed] [Google Scholar]
- 7.Topping KJ. The effectiveness of peer tutoring in further and higher education: a typology and review of the literature. High Educ. 1996;32(3):321–45. [Google Scholar]
- 8.Olle TC, Steven D. Dimensions and psychology of peer teaching in medical education. Med Teach. 2007;29(6):546–52. [DOI] [PubMed] [Google Scholar]
- 9.Williams B, Reddy P. Does peer-assisted learning improve academic performance? A scoping review. Nurse Educ Today. 2016;42:23–9. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Liao AWX, Goh SH, Wu XV, Yoong SQ. Effectiveness of peer teaching in health professions education: a systematic review and meta-analysis. Nurse Educ Today. 2022;118:105499. [DOI] [PubMed] [Google Scholar]
- 11.Carey MC, Kent B, Latour JM. Using meta-ethnography to develop a conceptual model of peer-assisted learning of nursing students in clinical practice. NURS OPEN. 2019;6(2):473–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Irvine S, Williams B, McKenna L. Near-peer teaching in undergraduate nurse education: an integrative review. Nurse Educ Today. 2018;70:60–8. [DOI] [PubMed] [Google Scholar]
- 13.Field M, Burke JM, McAllister D, Lloyd DM. Peer-assisted learning: a novel approach to clinical skills learning for medical students. Med Educ. 2007;41(4):411–8. [DOI] [PubMed] [Google Scholar]
- 14.Brierley C, Ellis L, Reid ER. Peer-assisted learning in medical education: a systematic review and meta-analysis. Med Educ. 2022;56(4):365–73. [DOI] [PubMed] [Google Scholar]
- 15.Kachaturoff M, Caboral-Stevens M, Gee M, Lan VM. Effects of peer-mentoring on stress and anxiety levels of undergraduate nursing students: an integrative review. J Prof Nurs. 2020;36(4):223–8. [DOI] [PubMed] [Google Scholar]
- 16.Herrmann-Werner A, Gramer R, Erschens R, Nikendei C, Wosnik A, Griewatz J, Zipfel S, Junne F. Peer-assisted learning (PAL) in undergraduate medical education: an overview. Z fuer Evidenz Fortbild Und Qualitaet Im Gesundheitswesen. 2017;121:74–81. [DOI] [PubMed] [Google Scholar]
- 17.Zoraya SI, Florettira MT, Syakurah RA, Azhar AAB, Okparasta A, Irfani TH. The impact of peer assisted learning on mentors’ academic life and communication skill in medical faculty: a systematic review. Int J Public Health Sci. 2021;10(2):401–10. [Google Scholar]
- 18.Guraya SY, Abdalla ME. Determining the effectiveness of peer-assisted learning in medical education: a systematic review and meta-analysis. J Taibah Univ Med Soc. 2020;15(3):177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Maconochie M. A meta-analysis of peer-assisted learning on examination performance in clinical knowledge and skills education. BMC Med Educ. 2022;22(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong BSH, Shorey S. Nursing students’ experiences and perception of peer feedback: a qualitative systematic review. Nurse Educ Today. 2022;116:105469. [DOI] [PubMed] [Google Scholar]
- 21.Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558–65. [DOI] [PubMed] [Google Scholar]
- 22.Jay EA, Starkman SJ, Pawlina W, Lachman N. Developing medical students as teachers: an anatomy-based student-as-teacher program with emphasis on core teaching competencies. Anat Sci Educ. 2013;6(6):385–92. [DOI] [PubMed] [Google Scholar]
- 23.Marton GE, McCullough B, Ramnanan CJ. A review of teaching skills development programmes for medical students. Med Educ. 2015;49(2):149–60. [DOI] [PubMed] [Google Scholar]
- 24.Annette B, Deborah M. Peer teacher training for health professional students: a systematic review of formal programs. BMC Med Educ. 2018;18(1):263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mcneill J, Lynn F, Alderdice F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health. 2012;12:955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fakoya OA, Mccorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. 2020;20:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Motahari-Nezhad H, Fgaier M, Mahdi Abid M, Péntek M, Gulácsi L, Zrubka Z. Digital Biomarker-Based studies: scoping review of systematic reviews. JMIR Mhealth Uhealth. 2022;10(10):e35722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 29.Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid-Based Healthc. 2015;13(3):132–40. [DOI] [PubMed] [Google Scholar]
- 30.Lee SY, Shin J-S, Lee S-H. How to execute context, input, process, and product evaluation model in medical health education. J Educ Eval Health Prof. 2019;16:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frye AW, Hemmer PA. Program evaluation models and related theories: AMEE guide 67. Med Teach. 2012;34(5):e288–299. [DOI] [PubMed] [Google Scholar]
- 32.Akinla O, Hagan P, Atiomo W. A systematic review of the literature describing the outcomes of near-peer mentoring programs for first year medical students. BMC Med Educ. 2018;18(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burgess A, McGregor D, Mellis C. Medical students as peer tutors: a systematic review. BMC Med Educ. 2014;14:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carey MC, Kent B, Latour JM. Experiences of undergraduate nursing students in peer assisted learning in clinical practice: a qualitative systematic review. JBI Database Syst Reviews Implement Rep. 2018;16(5):1190–219. [DOI] [PubMed] [Google Scholar]
- 35.Choi JA, Kim O, Park S, Lim H, Kim JH. The effectiveness of peer learning in undergraduate nursing students: a Meta-analysis. Clin Simul Nurs. 2020;50:92–101. [Google Scholar]
- 36.Coliñir. JH. Gallardo. LM, Morales. DG, Sanhueza. CI, Yañez. OJ: characteristics and impacts of peer assisted learning in university studies in health science: a systematic review. Rev Clin Esp. 2022;222(1):44–53. [DOI] [PubMed] [Google Scholar]
- 37.Dalwood N, Bowles KA, Williams C, Morgan P, Pritchard S, Blackstock F. Students as patients: a systematic review of peer simulation in health care professional education. Med Educ. 2020;54(5):387–99. [DOI] [PubMed] [Google Scholar]
- 38.Gazula S, McKenna L, Cooper S, Paliadelis P. A systematic review of reciprocal peer tutoring within Tertiary Health Profession Educational Programs. Health Professions Educ. 2017;3(2):64–78. [Google Scholar]
- 39.Irvine S, Williams B, McKenna L. How are we assessing near-peer teaching in undergraduate health professional education? A systematic review. Nurse Educ Today. 2017;50:42–50. [DOI] [PubMed] [Google Scholar]
- 40.Khapre M, Deol R, Sharma A, Badyal D. Near-peer tutor: a solution for Quality Medical Education in Faculty Constraint setting. Cureus. 2021;13(7):e16416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lerchenfeldt S, Mi M, Eng M. The utilization of peer feedback during collaborative learning in undergraduate medical education: a systematic review. BMC Med Educ. 2019;19(1):321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lim S, Min LX, Chan CJW, Dong YH, Mikkonen K, Zhou WT. Peer mentoring programs for nursing students: a mixed methods systematic review. Nurse Educ Today. 2022;119:105577. [DOI] [PubMed]
- 43.Nelwati, Abdullah KL, Chan CM. A systematic review of qualitative studies exploring peer learning experiences of undergraduate nursing students. Nurse Educ Today. 2018;71:185–92. [DOI] [PubMed] [Google Scholar]
- 44.Rees EL, Quinn PJ, Davies B, Fotheringham V. How does peer teaching compare to faculty teaching? A systematic review and meta-analysis. Med Teach. 2016;38(8):829–37. [DOI] [PubMed] [Google Scholar]
- 45.Secomb J. A systematic review of peer teaching and learning in clinical education. J Clin Nurs. 2008;17(6):703–16. [DOI] [PubMed] [Google Scholar]
- 46.Tai J, Molloy E, Haines T, Canny B. Same-level peer-assisted learning in medical clinical placements: a narrative systematic review. Med Educ. 2016;50(4):469–84. [DOI] [PubMed] [Google Scholar]
- 47.Tanveer MA, Mildestvedt T, Skjaerseth IG, Arntzen HH, Kenne E, Bonnevier A, Stenfors T, Kvernenes M. Peer teaching in Undergraduate Medical Education: what are the Learning outputs for the Student-Teachers? A systematic review. Adv Med Educ Pract. 2023;14:723–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011;2:157–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang H, Liao AWX, Goh SHL, Yoong SQ, Lim AXM, Wang WR. Effectiveness and quality of peer video feedback in health professions education: a systematic review. Nurse Educ Today. 2022;109:105203. [DOI] [PubMed] [Google Scholar]
- 50.Rengier F, Rauch PJ, Partovi S, Kirsch J, Nawrotzki R. A three-day anatomy revision course taught by senior peers effectively prepares junior students for their national anatomy exam. Annals Anat = Anatomischer Anzeiger: Official Organ Anatomische Gesellschaft. 2010;192(6):396–9. [DOI] [PubMed] [Google Scholar]
- 51.Kim SS, De Gagne JC. Instructor-led vs. peer-led debriefing in preoperative care simulation using standardized patients. Nurse Educ Today. 2018;71:34–9. [DOI] [PubMed] [Google Scholar]
- 52.Sevenhuysen S, Thorpe J, Molloy E, Keating J, Haines T. Peer-Assisted Learning in Education of Allied Health Professional Students in the clinical setting: a systematic review. J Allied Health. 2017;46(1):26–35. [PubMed] [Google Scholar]
- 53.Loda T, Erschens R, Loenneker H, Keifenheim KE, Nikendei C, Junne F, Zipfel S, Herrmann-Werner A. Cognitive and social congruence in peer-assisted learning-A scoping review. PLoS ONE. 2019;14(9):e0222224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanders D, Welk DS. Strategies to Scaffold Student Learning: applying Vygotskyʼs Zone of Proximal Development. Nurs Educ. 2005;30(30):203–7. [DOI] [PubMed] [Google Scholar]
- 55.Tamachi S, Giles JA, Dornan T, Hill EJR. You understand that whole big situation they’re in: interpretative phenomenological analysis of peer-assisted learning. BMC Med Educ. 2018;18(1):197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Masters K. Edgar Dale’s pyramid of learning in medical education: a literature review. Med Teach. 2013;35(11):e1584–93. [DOI] [PubMed] [Google Scholar]
- 57.Annette B, Christie vD, Chris R, Craig M. Introduction to the peer teacher training in health professional education supplement series. BMC Med Educ. 2020;20(Suppl 2):454–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alexandra C, Yvonne S, Elisa RC. Teaching Medical students to teach:a narrative review and literature-informed recommendations for student-as-teacher curricula. Academic Medicine; 2022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.